Abstract
Objective This study was designed to examine whether executive functions and parenting behaviors (acceptance, behavioral control, and psychological control) are associated with medical adherence and autonomy among preadolescents and adolescents with spina bifida (SB). Methods Questionnaire and observational data were collected from a sample of 8–15 year olds with SB (N = 140) and their mothers, fathers, and teachers. Youth also completed neuropsychological testing. Results Youth with SB demonstrated impairment on measures of executive functions, based on questionnaire and test data. Executive functions (questionnaire data only) and parenting behaviors were associated with medical adherence, but only executive functions (test data only) were associated with medical autonomy. Analyses also suggest that maternal and paternal behavioral control and paternal psychological control moderate relations between executive functions and adherence. Conclusions Interventions that target executive functions and parenting behaviors may facilitate positive health care behavior outcomes among youth with SB.
Keywords: adherence, attention, executive functions, medical autonomy, parenting behaviors, spina bifida
Introduction
Health conditions that are both chronic and physically disabling are often challenging to manage and require a combination of physical, mental, and emotional resources. Despite considerable research exploring adherence behaviors among youth with chronic health conditions (see La Greca & Mackey, 2009, for a review), few studies have investigated medical adherence and autonomy among youth with physical disabilities, such as spina bifida (SB; e.g., Stepansky, Roache, Holmbeck, & Schultz, 2010). The purpose of this study is to further understand factors that contribute to higher levels of medical adherence and autonomy among preadolescents and adolescents with SB. The impact of higher order cognitive functions and parenting behaviors on adherence and autonomy among youth with SB will be explored. In this study, adherence refers to the youth’s compliance to their prescribed medical regimen (e.g., bowel program, medications; Haynes, 1979). Medical autonomy, on the other hand, refers to an interpersonal process in which the child begins to develop a greater capacity for independence on health care tasks in the context of continued parental support.
SB is a common congenital neural tube birth defect with an overall prevalence rate of 3.1 cases per 10,000 live births in the United States (Shin et al., 2010). Associated physical complications may include hydrocephalus, neurogenic bladder and bowel dysfunction, weakness and paralysis of the lower extremities, endocrine dysfunction, neurocognitive deficits, and seizure disorders (Fletcher et al., 2004). As a result, children with SB and their families must manage complex medical regimens that include catheterizations, skin checks to avoid pressure sores, bowel programs, use of ambulatory devices (e.g., orthotics, braces, wheelchairs), and monitoring for shunt malfunction or infection.
Prior research has found that youth with less advanced cognitive functioning often have greater difficulty managing their medical regimen (e.g., Dunbar-Jacob et al., 2000). This is noteworthy, as deficits in the area of executive function have been well-established among youth with SB. Specifically, these youth have demonstrated deficits with problem solving, planning and goal-directed behavior, focused attention, ability to shift attention, response inhibition, and working memory (Brown et al., 2008; Mahone, Zabel, Levey, Verda, & Kinsman, 2002; Rose & Holmbeck, 2007). The severity of executive function deficits likely has implications for medical adherence and autonomy outcomes among youth with SB.
Family environmental factors, such as parenting behaviors, have often been the focus of pediatric research investigating health care behaviors of youth with chronic health conditions (e.g., Wysocki & Gavin, 2006). Parenting behaviors during preadolescence and adolescence are important to understand, as transfer of medical responsibilities from the parent to the child often occurs during this developmental period (Williams, Holmbeck, & Greenley, 2002). Prior researchers working with other illness populations have documented the significant effects of parenting behaviors on health care behaviors during this developmental period (Wysocki, & Gavin, 2006; HIV, Naar-King et al., 2009). Parenting behaviors are believed to be particularly influential for adjustment among youth with SB because such youth have less contact with peers and are more dependent on adults (Holmbeck et al., 2003).
This study will investigate the direct and moderating effects of three parenting behaviors on medical adherence and autonomy outcomes: parental acceptance, behavioral control, and psychological control. Parental acceptance refers to affective/emotional aspects of parenting behaviors or the degree to which parents are supportive of and able to adapt to their child’s needs (Steinberg, 1990). Behavioral control describes the extent to which parents set and consistently enforce developmentally appropriate limits on child behavior (Steinberg, 1990). Parental psychological control is defined as intrusive and critical parental behavior that compromises a child’s individuality and inhibits autonomy development (Barber & Harmon, 2001; Steinberg, 1990). These parenting behaviors have been found to have significant implications for the psychosocial adjustment of youth in the areas of academic, social, and emotional functioning (e.g., Holmbeck, Shapera, & Hommeyer, 2002; Steinberg, 1990). Youth tend to be adversely affected by parental psychological control, whereas parental acceptance and behavioral control tend to elicit positive adjustment outcomes among youth.
Several hypotheses will be explored. Consistent with prior research, Hypothesis 1 predicts that youth with SB will exhibit lower levels of executive function ability in comparison with normative samples. Hypothesis 2 predicts that higher levels of executive function ability will be associated with higher levels of medical adherence and autonomy. In addition, higher levels of adaptive parenting behaviors (i.e., acceptance and behavioral control; Hypothesis 3) and lower levels of maladaptive parenting behaviors (i.e., psychological control; Hypothesis 4) are expected to be associated with higher levels of adherence and autonomy. Lastly, this study investigates the moderating role of parenting behaviors on the relation between executive function and medical adherence and autonomy. Parental acceptance and behavioral control are conceptualized as protective factors such that higher levels of these behaviors are expected to buffer against the negative effects of lower levels of executive function on adherence/autonomy (Hypothesis 5). Psychological control is conceptualized as a vulnerability factor such that higher levels of these behaviors are expected to be associated with lower levels of adherence and autonomy, in the context of neurocognitive deficits (Hypothesis 6).
Materials and Methods
Participants
Participants were part of a larger longitudinal investigation that examined psychosocial adjustment, family and peer relationships, and neuropsychological functioning among youth with SB (e.g., Devine, Holbein, Psihogios, Amaro, & Holmbeck, 2012). Data collection for the larger study occurs every 2 years. As data from Time 2 are still being collected, this study only included analyses from the first wave of data collection, when youth were 8–15 years old.
Children with SB were recruited from children’s hospitals, a university-based medical center, and a statewide SB association. Families were included in the study if they met the following inclusionary requirements: (1) diagnosis of SB (types included myelomeningocele, lipomeningocele, myelocystocele); (2) aged 8–15 years at Time 1; (3) ability to speak English or Spanish; (4) at least one primary custodial caregiver; and (5) residence within 300 miles of Chicago. A total of 246 families were approached for participation in this study, and 163 families agreed to participate. Of these 163 families, 21 families were unable to be contacted or later declined, and two families did not meet inclusion criteria. The resulting sample size was 140 families (57% participation rate). A total of 129 mothers and 106 fathers participated. Analyses were conducted to compare the 140 families enrolled in the study with those who declined to participate across several medical variables. Groups did not significantly differ on any of the following: type of SB [myelomeningocele vs. other; χ2(1) = 0.0002, ns], shunt status [χ2(1) = 0.003, ns], or occurrence of shunt infections [χ2(1) = 1.08, ns].
Among the 140 families of children who participated, the sample was distributed relatively evenly across 8–15 year olds [M(age) = 11.43, SD = 2.46]: 39 were aged 8 or 9 years, 29 were aged 10 or 11 years, 36 were aged 12 or 13 years, and 36 were aged 14 or 15 years. Approximately half of the sample was female (54%). The largest ethnic group was Caucasian (54.0%), followed by Hispanic (27.9%). The sample demonstrated considerable variability in socioeconomic status, based on a mean Hollingshead (1975) four-factor index of 39.70 (SD = 15.90).
Procedure
Trained graduate and undergraduate research assistants collected data during two separate 3-hr in-home sessions, with an average of 45.50 days between sessions. Parental consent and child assent were obtained. Parents were asked to sign release forms for medical chart review, nurse participation, and teacher participation to obtain additional information regarding the family and child. Children completed 1 hr and a half of neuropsychological evaluations at both in-home sessions. Parents and children also completed several questionnaires and were asked to participate in a set of audio and videotaped interaction tasks. Families received gifts (i.e., T-shirts, pens) and monetary compensation ($150) for their participation. Teachers and nurses were also monetarily compensated $25 and $10, respectively.
Measures
Demographics and Illness Severity
Nurses and research assistants conducted medical chart reviews for each participant that provided consent. Medical chart reviews and maternal report provided information regarding the following physical status variables: (1) spinal lesion (medical chart): 19.0% sacral, 62.9% lumbar, 18.1% thoracic; (2) SB type (medical chart): 87.9% myelomeningocele, 8.3% lipomeningocele, 3.8% other; (3) shunt status (maternal report): 80.3% with a shunt; and (4) hydrocephalus status (maternal report): 79.5% with hydrocephalus. The average number of shunt surgeries among children with shunts was 3.40 (SD = 5.27). Similar to prior studies (e.g., Wills, Holmbeck, Dillon, & McLone, 1990), youth with SB typically demonstrated a low average IQ [M = 85.69, SD = 16.58 on the Wechsler Abbreviated Scale of Intelligence (WASI)]. Of the 140 children that participated in this study, 26 children (18.6%) had an IQ score <70. Child questionnaire data were not used for these 26 individuals.
The Gross Motor Function Classification System for SB provided a measurement of limitations in gross motor functioning among individuals with SB (adapted from the Gross Motor Function Classification System for Cerebral Palsy; Palisano et al., 1997). Individuals were categorized across five-levels based on self-initiated movement from Level I (i.e., very minimal limitations; no limitations in walking) to Level V (significant physical impairments and limitations; limited ability to maintain antigravity head and trunk postures). Trained research assistants evaluated medical charts and parent report of the child’s medical history to determine the child’s limitations in gross motor functioning. After coders achieved adequate inter-rater reliability during training (i.e., Kappa ≥ 70), classifications were based on a single coder. Given the severity of disability required for a Level V categorization, youth in this study fell in the Level I to Level IV range only. Seventeen (12.2%) participants were categorized as Level I, 33 (23.7%) as Level II, 30 (21.6%) as Level III, and 52 (37.4%) as Level IV. Disability level could not be determined for eight participants owing to missing data.
Neurocognitive Functioning Measures
General Intellectual Ability
The Vocabulary and Matrix Reasoning subtests of the WASI (Wechsler, 1999) were used in this study as a proxy for general intellectual functioning.
Executive Functions Questionnaire Data
The Behavior Rating Inventory of Executive Functions (BRIEF; Gioia, Isquith, Guy, Kenworthy, 2000) is a parent- and teacher-report questionnaire that measures several domains of executive functions of children. It is composed of the following eight subtests: Inhibit, Shift, Emotional Control, Initiate, Working Memory, Plan/Organize, Organization of Materials, and Monitor subtests. These subtests fall within two broad second-order scales: Behavioral Regulation and Metacognition, which make up the overall Global Executive Composite Score. Mothers, fathers, and teachers completed all 86 items that comprise the BRIEF subtests (e.g., “Makes careless mistakes”). Parents and teachers were instructed to circle whether their child has “never,” “sometimes,” or “often” demonstrated a particular behavior during the past 6 months. Higher scores on the BRIEF subtests represent lower levels of executive function (α = .98 for the total score; .84–.94 for subscales). The BRIEF has demonstrated adequate convergent validity with other self-report measures that assess for similar behavior problems (Gioia et al., 2000). Because the mother-, father-, and teacher reports for the item mean scores were moderately correlated (r = .30–.157), the mean across reporters was used when parent- and teacher reports were available. All scores were first transformed into t-scores.
Executive Functions Test Data
Several neuropsychological measures were utilized as an assessment of executive functions. The Planned Connections subtest of the Cognitive Assessment System (CAS; Naglieri & Das, 1997) was used as an assessment of nonverbal executive function (i.e., planning). The Verbal Fluency Test of the Delis Kaplan Executive Function System (D-KEFS; Delis, Kaplan, & Kramer, 2001) was also utilized as an assessment of verbal executive functions. For these CAS and D-KEFS subtests, higher scores represented higher levels of executive function ability and all scores were transformed into age scaled scores. Because measures of executive function were moderately to strongly correlated (r = .48–.87), a composite score was created based on the mean age scaled scores across these measures (α = .89).
Measure of Parenting Behaviors
Four family interaction tasks were coded using a macro coding system (Holmbeck, Zebracki, Johnson, Belvedere, & Schneider, 2007). Coders viewed an entire family interaction task and rated the family members across several behavioral dimensions on five-point Likert scales (Kaugars et al., 2011). Scales for parental acceptance, psychological control, and behavioral control were formed rationally for separate mother and father scales by selecting items from the complete list of behavioral codes that reflect the definitions of each parenting construct (see Holmbeck, et al., 2002; Kaugars et al., 2011). Scales were created separately for mothers and fathers.
To assess interrater reliability of the observed parenting behavior constructs, intraclass reliability correlations were computed, with ≥.60 considered adequate (Kieffer, Cronin, & Fister, 2004). Adequate interrater reliability was obtained for all six parenting scales (three for mother and three for father; range = 0.68–0.88). In addition, adequate scale reliability was also obtained (range = 0.68–0.91). Skewness analyses, based on guidelines established by Tabachnick and Fidell (2007), demonstrated that the maternal behavioral control was significantly skewed (z-score = −3.35), necessitating use of a square root transformation.
Measures of Health Care Behaviors
Adherence
The SB Self-Management Profile (SBSMP; Wysocki & Gavin, 2006) is a 14-item questionnaire that assesses several dimensions of medical adherence in youth with SB, based on parent report (e.g., bowel control, medication management, catheterization). Parents were instructed to report how well in the past 6 months their child has taken care of each self-care task. For example, to assess the child’s adherence to their bowel program the parent was asked, “In the past 6 months, how often has your child stayed within the diet recommendations that the doctor has given to you?” For this item, parents rated their child’s behavior on a five-point scale from “Always eats according to the recommendations” (100%) to “Rarely or never eats according to the recommendations” (0–10%). Each item score was transformed into standardized z-scores owing to variability across the items’ rating scales (i.e., this measure included four-point, five-point, and six-point scales). A total score was computed using the mean item z-scores across the 14 items. Higher scores represented higher levels of adherence. Because the mother- and father-reported scores on the SBSMP were moderately correlated (r = .49), the mean across reporters was used when mother- and father reports were available. Internal consistency could not be computed owing to a low number of participants that completed all test items (i.e., an item could be left blank if it was “not applicable” to the child’s prescribed medical regimen). Nonetheless, prior studies have demonstrated adequate internal consistency (α = .66; Wysocki & Gavin, 2006). Skewness analyses revealed that the adherence variable was significantly skewed (z-score = −4.26); thus, a square root transformation was used.
Autonomy
The Sharing of SB Management Responsibilities (SOSBMR) scale was adapted from the Diabetes Family Responsibility Questionnaire (Anderson, Auslander, Jung, Miller, & Santiago, 1990). The SOSBMR consists of 34 items regarding SB-related responsibilities (e.g., catheterization, bowel programs), in which the parent and child identify the family member who is responsible for a specified task on a three-point scale: child responsibility, parent responsibility, and shared responsibility. A box marked N/A is provided for tasks that are not relevant for the child’s care. Higher scores indicate greater child responsibility. An item mean score was computed for each reporter. Mother-, father-, and child-report scores were moderately correlated (r = .65–.76). Thus, the mean across reporters was used when parent- and child reports were available. Internal consistency could not be computed owing to a low number of participants that completed all test items (i.e., an item could be left blank if it was “not applicable” to the child’s prescribed medical regimen). Prior studies have demonstrated adequate internal consistency on the Diabetes Family Responsibility Questionnaire (α = .85; Anderson et al., 1990).
Approach to Data Analyses
To test Hypothesis 1, analyses were conducted to determine whether youth with SB demonstrated lower levels of executive function ability as compared with typically developing youth. Specifically, t-test analyses were computed for the executive function measures (i.e., BRIEF, test data subtests) to compare mean executive function ability in comparison with data from a normative population.
To investigate Hypotheses 2 through 6, a series of hierarchical regression analyses were conducted to examine associations between executive functions, parenting behaviors (acceptance, behavioral control, psychological control), and adherence/autonomy. Specifically, analyses were computed to examine the influence of executive functions (based on test data and parent/teacher-report data; Hypothesis 2) and parenting behaviors (Hypotheses 3 and 4) on adherence/autonomy, after controlling for age, IQ, and level of disability. In addition, analyses were also computed to determine whether the nature or magnitude of the association between executive functions and adherence/autonomy varied as a function of parental adaptive (Hypothesis 5) and maladaptive (Hypothesis 6) parenting behaviors. Separate hierarchical regression analyses were run for each of the six parenting behaviors. Analyses were also run separately for each outcome variable. When running these regression analyses, continuous predictor variables were centered, and independent variables and interactions among the independent variables were entered in the following order: (Step 1) covariates—IQ, age, and level of disability; (Step 2) parenting behavior main effect, executive function test data main effect, and executive function questionnaire data main effect; and (Step 3) parenting behavior × executive function test data and parenting behavior × executive function questionnaire data interactions (Aiken & West, 1991; Holmbeck, 2002). If a significant two-way interaction emerged in the regression analyses (i.e., a significant moderation effect), then simple slopes and relevant significance tests were computed for the different levels of the parenting behavior variables (Aiken & West, 1991; Holmbeck, 2002).
Power analyses were conducted based on guidelines established by Cohen (1992). The sample size was sufficient to detect a medium effect size in all regression analyses (N’s = 115–119), except for regression models that included paternal parenting behaviors. For these analyses, the sample size was only sufficient to detect a large effect size (N’s = 91–95).
Results
Preliminary Analyses
Means, standard deviations, and scale ranges for study variables are presented in Table I. The association between the health care behavior outcomes was also investigated. Pearson correlations demonstrated only a weak association between medical adherence and medical autonomy (r = −.17).
Table I.
Means, Standard Deviations, Ranges, and t-Test Analyses for Executive Function Subtests
| Variable | N | Mean | SD | Range | t-test |
|---|---|---|---|---|---|
| Control variables | |||||
| IQ (WASI) | 132 | 85.69 | 17.58 | 82 | |
| Age | 139 | 11.43 | 2.46 | 7 | |
| Level of disability | 132 | 2.89 | 1.08 | 3 | |
| Executive function variables | |||||
| Neuro test data | 126 | 7.00 | 3.15 | 13.60 | |
| Parent/Teacher report (BRIEF) | 136 | 1.70 | 0.32 | 1.67 | |
| Observed parenting variables (macro data) | |||||
| Maternal acceptance | 132 | 3.48 | 0.34 | 1.55 | |
| Paternal acceptance | 104 | 3.33 | 0.37 | 1.84 | |
| Maternal behavioral control | 133 | 3.67 | 0.41 | 2.25 | |
| Paternal behavioral control | 104 | 3.27 | 0.53 | 2.62 | |
| Maternal psychological control | 134 | 2.28 | 0.35 | 1.69 | |
| Paternal psychological control | 105 | 2.30 | 0.34 | 1.54 | |
| Adherence (SBSMP) | 123 | −0.01 | 0.45 | 3.01 | |
| Autonomy (SOSBMR) | 124 | 1.82 | 0.41 | 1.87 | |
| CAS | |||||
| Planned connections | 120 | 6.15 | 3.53 | 13 | −11.95*** |
| D-KEFS | |||||
| Letter fluency | 126 | 7.00 | 3.70 | 17 | −9.11*** |
| Category fluency | 126 | 7.12 | 3.81 | 15 | −8.50*** |
| Switch–Correct | 125 | 7.26 | 3.92 | 18 | −7.82*** |
| Switch–Accuracy | 125 | 7.66 | 3.83 | 18 | −6.83*** |
Note. SD = standard deviation; WASI = Wechsler Abbreviated Scale of Intelligence; SNAP-IV = Swanson, Nolan, and Pelham – Fourth Edition; BRIEF = Behavioral Rating Inventory of Executive Function; SBSMP = Spina Bifida Self-Management Profile; SOSBMR = Sharing of Spina Bifida Management Responsibilities; CAS = Cognitive Assessment System; D-KEFS = Delis Kaplan Executive Function System.
Means for CAS and D-KEFS reflect scaled scores, with higher scores representing higher cognitive ability; t-tests are based on comparisons with published norms (Mean Scaled Score = 10; Standard deviation = 3).
***p < .001.
t-Test Analyses
The t-test analyses were computed to assess Hypothesis 1, which predicted that youth with SB would demonstrate lower levels of executive function, as compared with normative data. Mean scaled scores, standard deviations, and ranges for the executive function test data are presented in Table I. Higher scaled scores represent higher levels of functioning. Consistent with Hypothesis 1, youths’ performance on neuropsychological measures of executive function was statistically lower than normative data across all analyses (i.e., p < .001 for all t-test analyses). In comparison with the normative sample mean scaled score of 10, performance on the CAS and D-KEFS subtests were low average among youth with SB (i.e., scaled scores between 6 and 7).
Mean t-scores, standard deviations, and ranges for the BRIEF subtests and indices are presented in Table II. Lower t-scores represent lower levels of executive function ability. In comparison with a normative sample t-score mean of 50, youth with SB in this sample had t-scores ranging from 50.39 (50th percentile) to 57.29 (77th percentile) based on parent report and t-scores sranging from 53.20 (63rd percentile) to 67.55 (96th percentile) based on teacher report. Consistent with Hypothesis 1, t-test analyses demonstrated that parent- and teacher report of youth executive function were statistically lower among youth with SB, in comparison with normative data (i.e., p < .001), except for parent report on the Organization of Materials subtest. Paired sample t-test analyses were also conducted to compare mean t-scores based on parent report and mean t-scores based on teacher report. Across all analyses, teachers reported lower levels of executive function among youth with SB, as compared with parents’ report of executive function (i.e., p = .00–.03), except for the Inhibit and Emotional Control subtests and the Behavioral Control Index.
Table II.
Means, Standard Deviations, Ranges, and t-Test Analyses for BRIEF Subtests
| Parent report |
Teacher report |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| BRIEF subtest | N | Mean | SD | Range | Parent Normsa | N | Mean | SD | Range | Teacher Normsa | Parent–Teacherb |
| Initiate | 123 | 56.34 | 9.49 | 38.00 | 7.41*** | 119 | 65.69 | 15.57 | 59.00 | 10.99*** | −5.67*** |
| Working memory | 123 | 57.29 | 10.13 | 47.50 | 7.98*** | 119 | 67.44 | 18.28 | 69.00 | 10.40*** | −6.16*** |
| Plan/Organize | 123 | 56.09 | 9.71 | 46.00 | 6.96** | 119 | 65.41 | 14.46 | 56.00 | 11.63*** | −6.21*** |
| Org. of materials | 123 | 50.39 | 8.85 | 36.50 | 0.49 | 118 | 67.51 | 21.65 | 95.00 | 8.78*** | −8.47*** |
| Monitor | 123 | 54.23 | 9.47 | 41.00 | 4.95*** | 120 | 60.57 | 13.57 | 64.00 | 8.53*** | −4.89*** |
| Metacog. index | 123 | 55.82 | 9.35 | 44.50 | 6.91*** | 118 | 67.05 | 16.85 | 67.00 | 11.04*** | −7.03*** |
| Inhibit | 123 | 50.87 | 8.37 | 38.00 | 1.16*** | 118 | 53.20 | 12.49 | 73.00 | 2.79** | −1.80 |
| Shift | 123 | 55.70 | 9.70 | 47.00 | 6.52*** | 119 | 59.52 | 17.22 | 90.00 | 6.03*** | −2.14* |
| Emotional control | 123 | 53.51 | 10.24 | 48.00 | 3.80*** | 118 | 55.04 | 15.56 | 84.00 | 3.52** | −0.68 |
| Beh. Reg. index | 123 | 53.31 | 9.32 | 43.50 | 3.94*** | 118 | 55.98 | 15.17 | 76.00 | 4.28*** | −1.66 |
| Global Exec. Comp. | 123 | 55.26 | 9.28 | 46.00 | 6.29*** | 118 | 63.84 | 16.05 | 76.00 | 9.37*** | −5.53*** |
Note. N’s vary for teacher report owing to missing data. Scores listed are t-scores, with higher scores indicating greater impairment; Mean t-scores based on published norms = 50.
aOne-sample t-test.
bPaired-samples t-test.
*p < .05; ***p < .001.
BRIEF = Behavioral Rating Inventory of Executive Function; SD = standard deviation; Org. = organization; Metacog. = metacognitive; Beh. Reg. = behavioral regulation; Global Exec. Comp. = global executive composite.
Regression Analyses
Adherence
Consistent with Hypothesis 2, higher levels of parent/teacher report of executive function (BRIEF) were associated with higher levels of medical adherence, after controlling for age, IQ, and level of disability [e.g., t(110) = −4.29, p < .001; t(88) = −2.91, p < .01; see Table III]. Yet, contrary to hypotheses, a significant positive main effect emerged for level of disability [t(114) = 2.74, p < .05; t(91) = 3.79, p < .001] such that children with higher levels of gross motor functioning impairment demonstrated higher levels of adherence.
Table III.
Multiple Regression Analyses: Executive Function and Parenting Behaviors as Predictors of Adherence
| Step and variable | R | β | FΔ | Step and variable | R | β | FΔ |
|---|---|---|---|---|---|---|---|
| Maternal acceptance (N = 115) | Paternal acceptance (N = 91) | ||||||
| Step 1 | Step 1 | ||||||
| Disability level | .25 | .25 | 7.49** | Disability level | .37 | .37 | 14.40*** |
| IQ | .26 | −.09 | 0.39 | IQ | .38 | −.06 | 0.40 |
| Age | .26 | .04 | 0.21 | Age | .38 | .04 | 0.13 |
| Step 2 | Step 2 | ||||||
| Acceptance | .46 | .39 | 20.99*** | BRIEF | .47 | −.29 | 8.33** |
| BRIEF | .57 | −.35 | 18.36*** | EF test data | .49 | −.29 | 2.92 |
| EF test data | .59 | −.19 | 22.41 | Acceptance | .50 | .04 | 0.21 |
| Step 3 | Step 3 | ||||||
| Acceptance × BRIEF | .60 | .12 | 2.31 | Acceptance × BRIEF | .50 | .09 | 0.83 |
| Acceptance × EF test data | .60 | .09 | 1.16 | Acceptance × EF test data | .51 | .10 | 0.72 |
| Maternal behavioral control (N = 116) | Paternal behavioral control (N = 91) | ||||||
| Step 1 | Step 1 | ||||||
| Disability level | .26 | .26 | 8.35** | Disability level | .37 | .37 | 14.40*** |
| IQ | .27 | −.08 | 0.67 | IQ | .38 | −.06 | .40 |
| Age | .27 | .05 | 0.25 | Age | .38 | .04 | 0.13 |
| Step 2 | Step 2 | ||||||
| BRIEF | .47 | −.40 | 21.26*** | BRIEF | .47 | −.29 | 8.33** |
| Beh. control | .59 | .36 | 21.85*** | Beh. control | .50 | −.18 | 3.65 |
| EF test data | .61 | −.23 | 3.56 | EF test data | .52 | −.29 | 2.95 |
| Step 3 | Step 3 | ||||||
| Beh. control × EF test data | .63 | .18 | 5.67* | Beh. control × BRIEF | .58 | −.27 | 8.37* |
| Beh. control × BRIEF | .68 | .26 | 11.62** | Beh. control × EF test data | .59 | −.06 | 0.34 |
| Maternal psychological control (N = 116) | Paternal psychological control (N = 92) | ||||||
| Step 1 | Step 1 | ||||||
| Disability level | .26 | .26 | 8.35** | Disability level | .38 | .38 | 15.33*** |
| IQ | .27 | −.08 | 0.67 | IQ | .38 | −.05 | 0.28 |
| Age | .27 | .05 | 0.25 | Age | .38 | .03 | 0.07 |
| Step 2 | Step 2 | ||||||
| BRIEF | .47 | −.40 | 21.26*** | BRIEF | .47 | −.29 | 8.49** |
| EF test data | .50 | −.26 | 3.91* | EF test data | .50 | −.28 | 2.69 |
| Psych. control | .50 | −.06 | 0.46 | Psych. control | .51 | −.11 | 1.26 |
| Step 3 | Step 3 | ||||||
| Psych. control × BRIEF | .51 | −.10 | 1.29 | Psych. control × BRIEF | .55 | −.24 | 6.21* |
| Psych. control × EF test data | .51 | .03 | 0.10 | Psych. control × EF test data | .56 | −.03 | 0.05 |
Note. Transformations for the observed maternal behavioral control (square root) and adherence (square root) variables were used in the aforementioned analyses; IQ based on WASI.
BRIEF = Behavioral Rating Inventory of Executive Function; EF = executive function; Beh. = behavioral; Psych. = psychological.
*p < .05; **p < .01; ***p < .001.
Maternal Parenting Behaviors
Consistent with Hypothesis 3, significant positive main effects emerged for maternal acceptance [t(111) = 4.58, p < .001; see Table III] and maternal behavioral control [t(111) = 4.68, p < .001] in predicting adherence, after controlling for age, IQ, and level of disability. Specifically, higher levels of maternal acceptance and maternal behavioral control were associated with higher levels of adherence. Contrary to Hypothesis 4, no significant effects emerged for maternal psychological control predicting adherence.
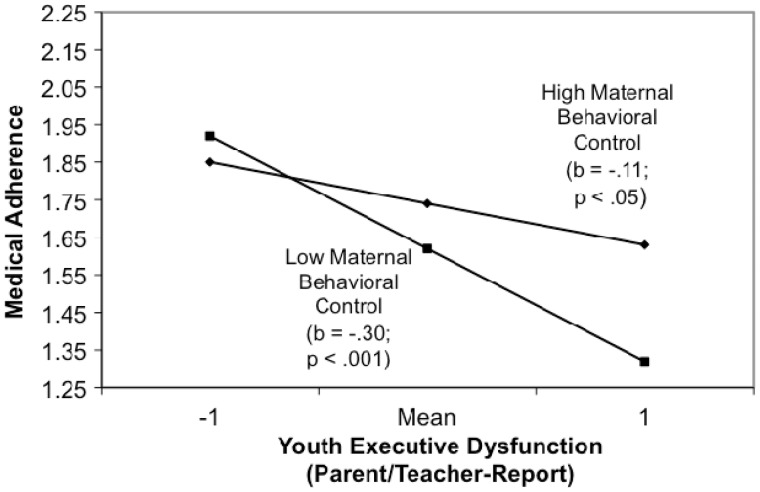
A significant maternal behavioral control × executive function test data interaction emerged, but follow-up simple slope analyses were not significant. In addition, the association between parent/teacher report of executive function (BRIEF), and adherence was qualified by a significant maternal behavioral control × BRIEF interaction [t(109) = 2.38, p < .05; see Figure 1]. Follow-up simple slope analyses demonstrated that the association between lower levels of parent/teacher report of executive function, and lower levels of adherence were enhanced among children with mothers who demonstrated lower levels of behavioral control [t(110) = −5.30, p < .001]. Yet, there was also a significant association between lower levels of parent/teacher report of executive function and lower levels of adherence among children with mothers who demonstrated higher levels of behavioral control [t(110) = −2.01, p < .05]. In other words, consistent with Hypothesis 5, maternal behavioral control partially buffered against the association between lower levels of executive function and lower levels of adherence such that the negative association between executive function based on parent/teacher report and adherence was stronger among children with mothers who demonstrated lower levels of behavioral control. No support was provided for Hypotheses 6, which predicted that maternal psychological control would moderate the relation between lower levels of executive function and lower levels of adherence.
Figure 1.
Parent/Teacher report of youth executive dysfunction by maternal behavioral control two-way interaction for predicting adherence.
Paternal Parenting Behaviors
Contrary to Hypotheses 3 and 4, no support was provided for a significant association between paternal parenting behaviors and adherence. Analyses provided partial support for paternal behavioral control moderating the association between lower levels of parent/teacher report of executive function and lower levels of adherence [t(84) = −2.89, p < .01]. Follow-up simple slope analyses indicated that the relation between lower levels of parent/teacher report of executive function and lower levels of adherence was enhanced among children with fathers who demonstrated higher levels of behavioral control [t(85) = −4.22, p < .001], as compared with children with fathers who demonstrated lower levels of behavioral control [t(85) = −0.69, p = .49]. Thus, in contrast to the finding for maternal behavioral control and contrary to Hypothesis 5, the association between lower levels of executive function based on parent/teacher report and lower levels of adherence was particularly strong among children with fathers who demonstrated higher levels of behavioral control. In other words, lower levels of paternal behavioral control buffered against the significant negative effects of lower levels of executive function and lower levels of adherence.
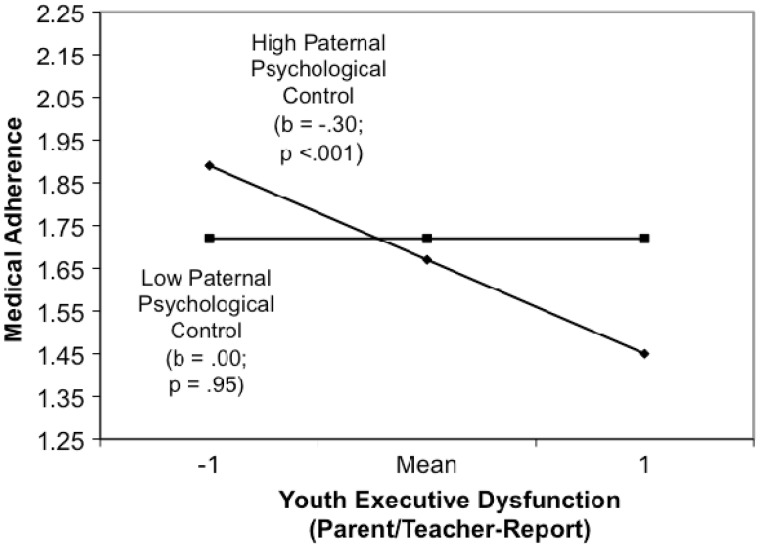
Analyses also provided support for paternal psychological control moderating the association between parent/teacher report of executive function and adherence [see Figure 2; t(85) = −2.49, p < .05]. Follow-up simple slope analyses indicated that the association between lower levels of parent/teacher report of executive function and lower levels of adherence was enhanced among children with fathers who demonstrated higher levels of psychological control [t(86) = −3.73, p < .001], as compared with children with fathers who demonstrated lower levels of psychological control [t(85) = −0.07, p = .95]. In other words, as predicted by Hypothesis 6, the association between lower levels of executive function and lower levels of adherence was only significant among individuals who demonstrated higher levels of psychological control. No significant moderating effects emerged for paternal acceptance (Hypothesis 5).
Figure 2.
Parent/Teacher report of youth executive dysfunction by paternal psychological control two-way interaction for predicting adherence.
Autonomy
Consistent with Hypothesis 2, higher levels of executive functioning ability based on test data were associated with higher levels of medical autonomy, after controlling for age, IQ, and level of disability [e.g., t(114) = 2.07, p < .05; t(115) = 2.10, p < .05]. No significant effects emerged for the main effects of parenting behaviors on medical autonomy (Hypothesis 3 and 4) or parenting behaviors moderating the relation between executive functions and medical adherence (Hypothesis 5 and 6). However, positive significant main effects emerged for age [t(117) = 4.89, p < .001; t(92) = 5.23, p < .001] and IQ [t(116) = 5.35, p < .001; t(93) = 4.26, p < .001]. Specifically, older children and children with higher scores on the WASI demonstrated higher levels of medical autonomy. A significant negative main effect also emerged for level of disability [t(91) = −3.00, p < .01] such that children with lower levels of gross motor functioning impairment demonstrated higher levels of medical autonomy.
Discussion
This multisource, multimethod study examined executive function ability and parenting behaviors in association with medical adherence and autonomy in youth with SB. Study findings found support for the direct effects of executive function ability on these health care outcomes and the direct and moderating effects of parenting behaviors on adherence.
Consistent with Hypothesis 1 and prior research among youth with SB (e.g., Mahone et al., 2002; Rose & Holmbeck, 2007), youth in this study demonstrated lower levels of executive function ability, after controlling for age, IQ, and level of disability, on both test and questionnaire data. On test data, mean scores on tests of executive function were low average, with mean scaled scores between 6.53 (around the 13th percentile) and 7.00 (16th percentile), respectively. On the questionnaire data, both parents and teachers reported significantly lower levels of executive function ability in comparison with normative data on all subtests of the BRIEF, except for parent report on the Organization of Materials subtest. It is also noteworthy that teachers tend to report lower levels of executive function in comparison with parents on most subtests of the BRIEF. There are several possible explanations for these findings. Perhaps teachers may more accurately report executive function deficits among youth with SB due, in part, to increased opportunity to observe these children in comparison with other children in an environment that demand such higher-order cognitive function. Of note, deficits in the area of executive function are often first observed in the classroom environment (Dawson & Guare, 2010). These findings highlight the importance of collecting executive function data among youth with SB using multiple methods and multiple sources.
Adherence
Higher levels of executive function based on parent/teacher report (Hypothesis 2) and higher levels of maternal acceptance and behavioral control (Hypothesis 3) were associated with higher levels of adherence, after controlling for age, IQ, and level of disability. In addition, maternal and paternal behavioral control (Hypothesis 5) and paternal psychological control (Hypothesis 6) moderated the relation between executive function and adherence.
The significant association between higher levels of executive function ability and higher levels of adherence was expected, given the complexity of treatment tasks these youth must follow. In addition to managing typical adolescent health care demands (e.g., hygiene behaviors), youth with SB must learn to catheterize, manage a bowel program, identify signs of shunt malfunction, and manage many other health care demands. All of these tasks require planning, organization, attention to detail, and problem-solving ability (i.e., higher-order cognitive ability). These findings are also consistent with prior research demonstrating that youth with less advanced cognitive functioning often have greater difficulty managing their medical regimen (Dunbar-Jacob et al., 2000). Clinically, skills training may be helpful for these youth to manage their executive deficits and ultimately will help them experience greater success with adherence.
The finding that adaptive maternal parenting behaviors were significantly associated with higher levels of adherence is in line with other research documenting the positive effects of these parenting behaviors on psychosocial adjustment outcomes of youth (e.g., Barber & Harmon, 2001; Holmbeck et al., 2002). In other words, the degree that mothers were emotionally supportive, affectionate, approving, and expected and enforced age-appropriate behavior was associated with higher levels of adherence among youth with SB. Moreover, interaction analyses revealed that higher levels of maternal behavioral control buffered against the association between lower levels of executive function on lower levels of adherence.
Paternal behavioral control also emerged as a significant moderating variable. However, interaction analyses revealed that, in contrast to Hypothesis 5 and the maternal parenting behavior findings, lower levels of paternal behavioral control buffered against the association between lower levels of executive function and lower levels of adherence. Given prior studies documenting the positive impact of increased parental involvement and supervision (Naar-King et al., 2009; Wysocki, & Gavin, 2006), these findings are somewhat counterintuitive. However, the majority of prior research investigating the impact of parenting behaviors on adjustment outcomes has only included maternal caretakers (e.g., Barber & Harmon, 2001). Perhaps, the validity of the behavioral control variable varies depending on the parent’s gender. Another explanation may be that lower levels of behavioral control serves as a buffer among fathers, as fathers may be at risk for demonstrating excessive control. Gender biases may also have influenced the coding of this variable. The majority of research assistants involved in coding parenting behaviors was female. There may also be an interaction effect between maternal and paternal parenting behaviors. Future research with larger samples sizes is necessary to explore the simultaneous effects of both maternal and paternal parenting behaviors (e.g., both parents with high levels of behavioral control vs. one parent with high levels and one parent with low levels of behavioral control).
Despite a great deal of research documenting the negative effects of psychological control on adjustment outcomes of youth (e.g., Barber & Harmon, 2001; Steinberg, 1990), including youth with SB (Holmbeck et al., 2002), study findings did not provide support for maladaptive parenting behaviors (i.e., psychological control) predicting adherence (Hypothesis 4). Although no direct effects emerged for psychological control predicting adherence (Hypothesis 4), the association between lower levels of executive function based on parent/teacher report and lower levels of adherence was stronger among children with fathers who demonstrated higher levels of psychological control (Hypothesis 6). Thus, consistent with study hypotheses, fathers who exhibit behaviors characterized by intrusiveness and criticism place youth with lower levels of executive function ability at risk for poor adherence.
Given the significant effect of both mother and father parenting behaviors on adherence, this study provides support for including both parents in treatment. Observing how families interact (e.g., playing a game, engaging in a problem solving task) can provide a baseline assessment of specific behaviors to target. In addition, mothers of children with physical disabilities, such as SB, would benefit from increased psychoeducation regarding the positive impact of maternal acceptance and behavioral control on adherence. Fathers of youth with SB who exhibit lower levels of executive function ability would benefit from psychoeducation regarding the negative effects of higher levels of behavioral control and psychological control.
Interestingly, youth with higher levels of disability also demonstrated higher levels of adherence in this study. Of note, the SBSMP measure does not address who takes care of medical tasks. Perhaps youth with higher levels of disability and, in turn, more severe cognitive impairment receive increased support from family members and health care providers to complete treatment tasks. As a result, these youth are reported to be more adherent. This speculation is in line with prior studies that highlight the importance of parental involvement on adherence among adolescents (e.g., Wysocki & Gavin, 2006). Moreover, youth with more severe disabilities likely warrant stricter adherence to treatment regimens owing to higher risks associated with non-compliance. More generally, these findings suggest that interventions should target youth who demonstrate only mild-to-moderate disability, as these youth tend to be at risk for adherence difficulties.
Autonomy
Lower levels of executive function based on test data were associated with lower levels of autonomy, after controlling for age, IQ, and level of disability (Hypothesis 2). Given prior research that documents that rates of autonomy skill acquisition among youth with SB tend to be 2–5 years behind typically developing peers (Davis, Shurtleff, Walker, Seidel, & Duguay, 2006; Devine, Wasserman, Gershenson, Holmbeck, & Essner, 2011), it is not surprising that youth who exhibit more profound deficits would have more difficulty on autonomy tasks.
It is noteworthy that the questionnaire measure was associated with adherence, whereas the performance-based measure was associated with autonomy. One reason for this finding may be that these different instruments are measuring different aspects of executive function ability. Although the test data measures the youth’s ability to rapidly plan and execute problem-solving strategies (Delis et al., 2001; Naglieri & Das, 1992), the BRIEF measures social and behavioral manifestations of executive function abilities (Gioia et al., 2000). In other words, social and behavioral manifestations of these neurocognitive deficits have greater implications for adherence outcomes, and medical autonomy relies more heavily on youth’s performance on tasks. Another explanation for this discrepancy may be that the adherence outcome is heavily influenced by caregiver bias, and the medical autonomy outcome is more objective. For example, parents who perceive their child to have greater difficulty adhering with medical tasks may over-report executive dysfunction (or vice versa). Nonetheless, teacher report of executive function was also part of the executive function composite, which reduces the likelihood of single-source bias.
Study findings did not provide support for the prediction that parenting behaviors would be associated with medical autonomy. However, other factors seem to be more salient predictors of autonomy among youth in this population including being older, having a higher level of disability, higher general cognitive functioning (i.e., IQ), as well as higher executive function ability. This is noteworthy, as autonomy taped into factors related to child functioning, whereas adherence taped into factors related to family functioning (i.e., parenting behaviors). Clinically, interventions for autonomy that are geared toward individual factors would likely be more beneficial. Yet, given that the majority of these factors cannot be changed (e.g., age), establishing realistic expectations with families is important.
Limitation and Future Research
There are several limitations of this study that will be important to address in future research. First, a small sample size, particularly among fathers (N’s = 88–95), reduced the statistical power of the regression analyses, and thus, the likelihood of detecting small and medium effects. Second, this study sampled youth within a single illness group (i.e., SB). There are several advantages to conducting research within a single illness group (Holmbeck et al., 2003); yet, this methodology limits the degree to which study findings can be generalized to groups with other chronic health conditions, as well as youth without chronic health conditions. Third, study findings were based on cross-sectional data only. As such, the temporal ordering of the variables cannot be determined. For example, parents might adapt their parenting style to a child who struggles with adherence by increasing structure. Fourth, the parenting measures do not account for the simultaneous impact of mother and father parenting behaviors and possible factors that contribute to certain parenting behaviors (e.g., cultural considerations). Lastly, future research is necessary to determine factors that impact health care behaviors across the life span among individuals with SB.
Relevant to this special issue, there were some limitations regarding the measurement of adherence that should be addressed in future research. This measure did not take into account the amount of assistance youth are receiving from their families to complete their treatment tasks. In addition, given the complexity of health care needs of children with SB, a questionnaire is not sufficient to fully assess adherence within this population and is susceptible to reporter bias. Moreover, the retrospective nature of this measure across a long interval (i.e., 6 months) may impact the temporal reliability of this measure. Nonetheless, this questionnaire allowed for the measurement of a complex array of medical adherence behaviors and for data to be collected from multiple individuals, reducing the likelihood of bias.
Acknowledgments
The authors wish to thank the Spina Bifida Association of Illinois, the staff of the spina bifida clinics at Children’s Memorial Hospital, Chicago, IL; Shriners Hospitals for Children, Chicago, IL; and Riley Children’s Hospital, Indianapolis, IN. They also thank numerous undergraduate and graduate research assistants for help with data collection and data entry. Most importantly, they gratefully acknowledge the contributions to this study by the parents, children, friends, teachers, and health professionals who participated for many years.
Funding
Completion of this manuscript was supported in part by research grants from the March of Dimes Birth Defects Foundation (12-FY01-0098) and the National Institute of Child Health and Human Development (RO1 HD048629).
Conflicts of interest: None declared.
References
- Aiken L S, West S G. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Anderson B J, Auslander W F, Jung K C, Miller J P, Santiago J V. Assessing family sharing of diabetes responsibilities. Journal of Pediatric Psychology. 1990;15:477–492. doi: 10.1093/jpepsy/15.4.477. [DOI] [PubMed] [Google Scholar]
- Barber B K, Harmon E L. Violating the self: Parental psychological control of children and adolescents. In: Barber B K, editor. Intrusive parenting: How psychological control affects children and adolescents. Washington, DC: American Psychological Association; 2001. pp. 15–52. [Google Scholar]
- Brown T M, Ris M D, Beebe D, Ammerman R T, Oppenheimer S G, Yeates K O, Enrile B G. Factors of biological risk and reserve associated with executive behavior in children and adolescents with spina bifida myelomeningocele. Child Neuropsychology. 2008;14:118–134. doi: 10.1080/09297040601147605. [DOI] [PubMed] [Google Scholar]
- Cohen J. A power primer. Psychological Bulletin. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Davis B E, Shurtleff D B, Walker W O, Seidel K D, Duguay S. Acquisition of autonomy skills in adolescents with myelomeningocele. Developmental Medicine and Child Neurology. 2006;48:253–258. doi: 10.1017/S0012162206000569. [DOI] [PubMed] [Google Scholar]
- Dawson P, Guare R. Executive skills in children and adolescents. New York, NY: Guilford Press; 2010. [Google Scholar]
- Delis D C, Kaplan E, Kramer J H. Delis Kaplan Executive Function System: Examiner’s manual. San Antonio, TX: Psychological Corporation; 2001. [Google Scholar]
- Devine K A, Holbein C E, Psihogios A M, Amaro C M, Holmbeck G N. Individual adjustment, parental functioning, and perceived social support in Hispanic and non-Hispanic white mothers and fathers of children with spina bifida. Journal of Pediatric Psychology. 2012;37:769–778. doi: 10.1093/jpepsy/jsr083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devine K A, Wasserman R M, Gershenson L S, Holmbeck G N, Essner B. Mother-child agreement regarding decision-making autonomy: A longitudinal comparison study of families of adolescents with and without spina bifida. Journal of Pediatric Psychology. 2011;36:277–288. doi: 10.1093/jpepsy/jsq093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunbar-Jakob J, Erlen J A, Schlenk E A, Ryan C M, Sereika S, Doswell W M. Adherence in chronic disease. Annual Review of Nursing Research. 2000;18:48–90. [PubMed] [Google Scholar]
- Fletcher J M, Dennis M, Northrup H, Barnes M A, Hannay H J, Landry S, Copeland K, Blaser SE, Kramer LA, Brandt ME, Francis DJ. Spina bifida: Genes, brain, and development. In: Glidden L, editor. International Review of Research in Mental Retardation. San Diego, CA: Academic Press; 2004. [Google Scholar]
- Gioia G A, Isquith P K, Guy S C, Kenworthy L. BRIEF Behavior Rating Inventory of Executive Function. Odessa, FL: Psychological Assessment Resources; 2000. [Google Scholar]
- Haynes R B. Introduction. In: Haynes R B, Taylor D W, Sackett D L, editors. Compliance in healthcare. Baltimore, MD: Johns Hopkins University Press; 1979. pp. 1–7. [Google Scholar]
- Hollingshead A A. Four factor index of social status. New Haven, CT: Yale University; 1975. [Google Scholar]
- Holmbeck G N. Post-hoc probing of significant moderational and meditational effects in studies of pediatric populations. Journal of Pediatric Psychology. 2002;27:87–96. doi: 10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- Holmbeck G N, Shapera W, Hommeyer J S. Observed and perceived parenting behaviors and psychosocial adjustment in pre-adolescents with spina bifida. In: Barber B K, editor. Intrusive parenting: How psychological control affects children and adolescents. Washington, DC: American Psychological Association; 2002. pp. 191–234. [Google Scholar]
- Holmbeck G N, Westhoven V C, Phillips W S, Bowers R, Gruse C, Nikolopoulos T, Totura C M, Davison K. A multimethod, multi-informant, and multidimensional perspective on psychosocial adjustment in preadolescents with spina bifida. Journal of Consulting and Clinical Psychology. 2003;71:782–796. doi: 10.1037/0022-006x.71.4.782. [DOI] [PubMed] [Google Scholar]
- Holmbeck G N, Zebracki K, Johnson S Z, Belvedere M, Schneider J. Parent-child interaction macro-coding manual (unpublished manual) Loyola University of Chicago, IL: 2007. [Google Scholar]
- Kaugars A S, Zebracki K, Kichler J C, Fitzgerald C J, Greenley R N, Alemzadeh R, et al. Use of the family interaction macro-coding system. Journal of Pediatric Psychology. 2011;36:539–551. doi: 10.1093/jpepsy/jsq106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kieffer K M, Cronin C, Fister M C. Exploring variability and sources of measurement error in alcohol expectancy questionnaire reliability coefficients: A meta-analytic reliability generalization study. Journal in Studies in Alcohol. 2004;65:663–671. doi: 10.15288/jsa.2004.65.663. [DOI] [PubMed] [Google Scholar]
- La Greca A M, Mackey E R. Adherence to pediatric treatment regimens. In: Roberts M C, Steele R G, editors. Handbook of pediatric psychology. 4th ed. New York, NY: Guilford Press; 2009. pp. 130–152. [Google Scholar]
- Mahone E M, Zabel T A, Levey E, Verda M, Kinsman S. Parent and self-report ratings of executive function in adolescents with myelomeningocele and hydrocephalus. Child Neuropsychology. 2002;8:258–270. doi: 10.1076/chin.8.4.258.13510. [DOI] [PubMed] [Google Scholar]
- Naar-King S, Montpiedra G, Nichols S, Farley J, Gravie P A, Kammerer B, et al. Allocation of family responsibility for illness management in pediatric HIV. Journal of Pediatric Psychology. 2009;34:187–194. doi: 10.1093/jpepsy/jsn065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naglieri J A, Das J P. Cognitive Assessment System administration and scoring manual. Itasca, IL: Riverside Publishing; 1997. [Google Scholar]
- Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Developmental Medicine and Child Neurology. 1997;39:214–223. doi: 10.1111/j.1469-8749.1997.tb07414.x. [DOI] [PubMed] [Google Scholar]
- Rose B M, Holmbeck G N. Attention and executive functions in adolescents with spina bifida. Journal of Pediatric Psychology. 2007;32:983–994. doi: 10.1093/jpepsy/jsm042. [DOI] [PubMed] [Google Scholar]
- Shin M, Besser L M, Siffel C, Kucik J, Shaw G M, Lu C, et al. Prevalence of spina bifida among children and adolescents in 10 regions in the United States. Pediatrics. 2010;126:273–279. doi: 10.1542/peds.2009-2084. [DOI] [PubMed] [Google Scholar]
- Steinberg L. Autonomy, conflict, and harmony in the family relationship. In: Feldman S S, Elliott G R, editors. At the threshold: The developing adolescent. Cambridge, MA: Harvard University Press; 1990. pp. 255–276. [Google Scholar]
- Stepansky M A, Roache C R, Holmbeck G N, Schultz K. Medical adherence in young adolescents with spina bifida: Longitudinal associations with family functioning. Journal of Pediatric Psychology. 2010;35:167–176. doi: 10.1093/jpepsy/jsp054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnick B G, Fidell L S. Using multivariate statistics. 5th ed. Boston, MA: Pearson Education; 2007. [Google Scholar]
- Wechsler D. Manual for the Wechsler Abbreviated Scale of Intelligence (WASI) San Antonio, TX: Psychological Corporation; 1999. [Google Scholar]
- Williams G, Holmbeck G N, Greenley R N. Adolescent health psychology. Journal of Consulting and Clinical Psychology. 2002;70:828–842. [PubMed] [Google Scholar]
- Wills K E, Holmbeck G N, Dillon K, McLone D G. Intelligence and achievement in children with myelomeningocele. Journal of Pediatric Psychology. 1990;15:161–176. doi: 10.1093/jpepsy/15.2.161. [DOI] [PubMed] [Google Scholar]
- Wysocki T, Gavin L. Parental involvement in the management of pediatric chronic diseases: Associations with adherence, quality of life, and health status. Journal of Pediatric Psychology. 2006;31:501–511. doi: 10.1093/jpepsy/jsj042. [DOI] [PubMed] [Google Scholar]