Abstract
Context:
Different risk factors associated with adolescent suicide attempts have been identified including those of socio-demographic and clinical variables. Relatively, little research has been done in the area of their stressors and coping patterns.
Aims:
To study the recent psychosocial stressors and patterns of coping associated with adolescent suicide attempts.
Settings and Design:
Tertiary care hospital, case-control study.
Materials and Methods:
One hundred consecutive cases of adolescent attempted suicide admitted to the hospital and an equal number of controls, matched individually for age and sex, from the relatives and friends of other patients in the ward, were studied. Assessment included details regarding socio-demographic data, psychiatric and physical morbidity, their recent stressors, and patterns of coping. Stressors were assessed using Presumptive Stressful Life Event Scale and coping strategies by Ways of Coping Questionnaire (revised).
Statistical Analysis:
Chi-square test and multivariate logistic regression analysis.
Results:
The number of stressful life events and mean stress scores in the preceding 1 month and certain coping strategies such as confronting, distancing, and escape-avoidance were found to be significant risk factors associated with adolescent suicide attempts. Strategies such as self-control, seeking social support, accepting responsibilities, problem solving, and positive appraisal act as protective factors.
Conclusions:
Recent stressors and strategies such as confronting, distancing, and escape-avoidance are significant risk factors associated with adolescent suicide attempts, whereas certain coping strategies act as protective factors. Teaching adolescents these protective coping patterns may be a promising strategy for prevention of adolescent suicide attempts.
Keywords: Adolescents, coping, psychosocial factors, suicide attempt
INTRODUCTION
According to the World Health Organization, almost 1 million people die from suicide every year. Attempted suicides are about 20 times more. Rates among young people have been increasing to such an extent that they are now the group at highest risk in a third of countries.[1] Suicide ranks as the second cause of death worldwide among 15-19 year olds, with at least one lakh adolescents dying by suicide every year.[2]
The National Crime Records Bureau (India), reports that in 2011, more than one lakh (135,585) persons committed suicide. Around 2.24% of the victims were children up to 14 years, whereas 35.4% suicide victims were youths in the age group of 15-29 years showing that the suicidal behavior increases markedly during adolescence.[3]
Adolescents who attempt suicide, in clinical samples, are a heterogeneous group.[4] Different risk factors associated with adolescent suicide attempts have been identified including those of socio-demographic and clinical variables.[5,6,7,8,9,10] Relatively little research has been done in the area of their stressors and coping patterns.[11,12] and hence this attempt to examine these factors is in more detail.
This study, in particular, aims at identifying the psychosocial risk factors and patterns of coping associated with adolescent attempted suicides so that necessary steps can be implemented to cut down the rates and prevent the family and the society from such a heavy loss.
MATERIALS AND METHODS
The study was conducted in a tertiary care hospital after clearance from the Human Ethical Committee of the Institution. It was designed to be a hospital-based case-control study. One hundred consecutive cases admitted to Medicine and Surgery wards of the hospital were recruited for the study. One hundred age- and sex-matched controls were also recruited for the purpose of the study.
Inclusion criteria
A case of adolescent suicide attempt was defined as “an adolescent (13-19 years of age) who had made deliberate act of self-harm consciously aimed at self-destruction with non-fatal outcome.” Each case was assessed soon after his/her medical condition became stable.
An equal number of controls, “who had never made suicide attempt,” individually matched for each case in respect to age (±2 years) and sex was recruited from the relatives and friends of other patients admitted in the ward. The suicidality subscale of the mini-international neuropsychiatric interview (MINI) devised by Sheehan, et al.[13] was used to screen the control group. Age- and sex-matched controls with a score of zero when assessed by the above subscale were taken as controls.
Methods
Patients were assessed once their medical/surgical condition became stable. The nature of the study was explained to the patient and to the relative and a written informed consent from the patient (aged more than 18 years) and from the relative (if patient is aged less than 18 years) was obtained. Those with mental retardation and those with severe medical complications related to the attempt were excluded from the study.
Assessment of cases included that of socio-demographic data, psychiatric and physical morbidity (if any), details regarding past attempt (if any), details of present attempt, their stressors, and patterns of coping. Controls were also assessed in similar lines except for the attempt.
Instruments
The mini-international neuropsychiatric interview
The MINI is a short-structured diagnostic interview, developed for DSM-IV and ICD-10 psychiatric disorders. With an administration time of approximately 15 min, it was designed to meet the need for a short but accurate structured psychiatric interview for multicenter clinical trials and epidemiological studies and to be used as a first step in outcome tracking in non-research clinical settings. One of the subscales is suicidality measure. There are six questions with specific scores for each. The total score gives a risk for suicide which may be absent, low, moderate or high. Score of zero in the subscale indicates absent suicidal risk.[13] This group was taken as controls.
ICD-10 classification of mental and behavioral disorders
Based on the clinical assessment, diagnosis was made according to ICD-10 clinical descriptions and diagnostic guidelines.[14]
Presumptive stressful life events scale
This scale was devised by Singh et al.[15] in view of the various limitations and indiscriminate use of the existing life event scales. This standardized scale consists of items which are shown to be relevant to Indian culture and representative of the common life events as experienced by this population. It consists of 51 items and mean stress scores are available for all items. The 51 items are further classified according to (a) whether they are personal or impersonal (not dependent on the individual's action, e.g., death of spouse, change in sleeping habits, etc.), (b) according to whether they are (1) desirable (e.g., outstanding personal achievement) (2) undesirable (e.g., marital conflict, failure in examination), and (3) ambiguous (e.g., change in working conditions, change in eating habits, etc.). The number of life events patient had experienced in the past 1 month was assessed and stress scores were calculated.[15] Certain items such as retirement, wife begins or stops work, pregnancy of wife, and son or daughter leaving home which were not applicable for adolescent population were not considered.
Ways of coping questionnaire (revised)
In this study, the instrument that was chosen to assess the coping strategies which were typically employed by the respondents was the Ways of Coping Questionnaire (revised).[16,17] The ways of coping (revised) is a questionnaire containing a wide range of thoughts and acts that people use to deal with the internal and/or external demands of specific stressful encounters. The revised ways of coping Folkman and Lazarus[17] differs from the original ways of coping checklist Folkman and Lazarus[18] in several ways. The response format in the original version was Yes/No; on the revised version the subject responds on a 4-point Likert Scale (0=does not apply and/or not used; 3=used a great deal). Redundant and unclear items were deleted or reworded, and several items, such as prayer, were added.
For each dimension, the reliability was independently rated. These ratings of reliability coefficients for a group of subjects were confrontive coping 0.70; distancing 0.61; self-controlling, 0.70; seeking social support, 0.76; accepting responsibility, 0.66; escape-avoidance, 0.72; planful problem solving, 0.68; and positive reappraisal, 0.79.
The revised version of the coping scale consists of items arranged in eight scales, by which people generally cope with difficult problems and situations. The eight scales are as follows:
Confrontive coping: This describes aggressive efforts to alter the situation and suggests a degree of hostility and risk taking
Distancing: This describes efforts to detach oneself from the problem, doing nothing about it and also efforts to create a positive outlook by looking at the brighter side of things
Self-control: This describes efforts to regulate one's own feelings and actions
Seeking social support: This describes efforts to seek informational support, tangible support, and emotional support
Accepting responsibilities: This acknowledges one's own role in the problem with a concomitant theme of trying to put things right
Escape-avoidance: This describes wishful thinking and behavioral efforts to escape or avoid. These items, which suggest escape and avoidance, contrast with the items on the distancing scale, which suggest detachment
Planful problem-solving: This describes deliberate problem – focused efforts to alter the situation, coupled with an analytic approach to solve the problem
Positive appraisal: This describes efforts to create positive meaning by focusing on personal growth and has a religious tone.
Statistical analysis
Data were analyzed using computer software, Statistical Package for Social Sciences (SPSS) version 20. Data are expressed in its frequency and percentage. To elucidate the associations and comparisons between different parameters, Chi-square (χ2) test was used as non-parametric test. Multivariate logistic regression analysis was performed to assess the risk factors (odds ratio (OR)) of different factors for each group. For all statistical evaluations, a two-tailed probability value of <0.05 was considered significant.
RESULTS
Majority of the adolescent suicide attempters (68 out of 100) were of the age 17-19 years (68%), whereas 32% belonged to the age group of 14-16 years. None of the cases belonged to 13-14 years of age; therefore, early adolescents were not represented in the study sample. Majority (62%) of the adolescent suicide attempters (62 out of 100) were females, whereas males formed only 38% of the case population. The study population also included age- and sex-matched control group.
Control group and case group did not show any statistical difference when their educational, occupational, marital, religious or socio-economic status, and family type were considered. Majority of the case group was unemployed (55%), less educated (80% high school), and belonged to lower socio-economic status (90%) and nuclear families (84%). Among the 100 attempters, 78 belonged to Hindu religion, 18 were Christians and 4 were Muslims. Among the controls, 70 were Hindus, 22 were Christians and 8 were Muslims.
Family history of mental illness forms an important risk factor for attempting suicide. 18% of the cases had family history, whereas 2% had family history in control group which was statistically significant (P=0.001). Family history of suicide/attempt may form an important factor for attempting suicide in adolescents. 12% of the cases had family history, whereas none of the controls had such a history. Past history of suicide attempt is another risk factor for suicide attempts in adolescents which is shown by the above result that eight out of hundred cases (8%) had past history. Controls were selected after excluding an attempt.
Considering the method employed for present attempt, pesticide consumption was the most common (52%) followed by drug overdosage (20%), odollum/nerium consumption (12%), slashed wrist (8%), and hanging (2%). Other methods by attempters (6%) included drowning, burns, and consumption of unknown substance. Most of the attempters had low intent.
Majority (78%) of the suicide attempters had psychiatric disorders, whereas none of the controls had any psychiatric disorders. Among different psychiatric morbidities, adjustment disorder ranked first (48%) followed by depressive disorder (16%), borderline personality in 6%, conduct disorder with alcohol abuse in 4%, alcohol dependence syndrome in 2%, and psychosis in 2%.
In this study, 4 out of 100 cases (4%) and 2 out of 100 controls (2%) had physical illness prior to the attempt. Physical illness was not significantly associated with adolescent suicide attempt (P=0.567).
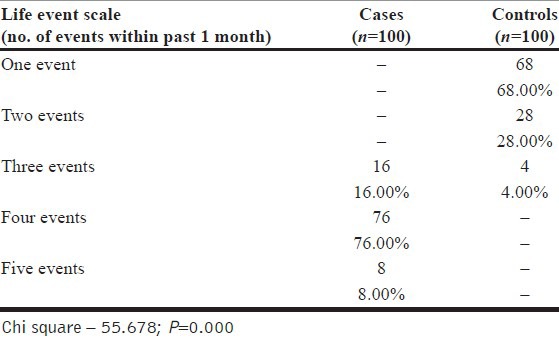
Recent stressful life events
Life event scale (number of events within past 1 month) showed highly significant difference between cases and controls with more life events in cases [Table 1]. All cases in this study had at least three or more events in their life within the past 1 month, whereas controls had maximum three events during this period, of which majority had only one event. Among cases, 16% had one event, 76% four events, and 8% five events.
Table 1.
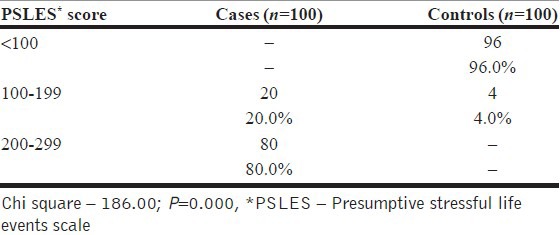
Presumptive stressful life events scale
Presumptive Stressful Life Event Scale (PSLES) showed highly significant difference between cases and controls with more score for cases. All cases in this study had >100 score, whereas controls had relatively low (<100) score. Majority (80%) of the cases had PSLES score ranging from 200 to 299 [Table 2].
Table 2.
Presumptive stressful life events scale
Patterns of coping
Confrontive coping showed significant statistical difference between cases and controls in this study. Confrontive coping was used to a greater extent by cases (86%), whereas fewer controls used them to this extent (16%).
Distancing as a method of coping showed significant statistical difference between cases and controls in this study. This coping strategy was used more by cases (86%), whereas controls used them to a lesser extent (8%).
Self-control as a coping strategy showed significant statistical difference between cases and controls. This strategy was used to a greater extent by controls (76%), whereas cases rarely used them to this extent (4%).
Significant difference was observed between cases and controls in seeking social support as a pattern of coping. Cases showed lesser (5%) social support seeking behavior, whereas controls used this strategy to a greater extent (84%).
Accepting responsibilities as a coping strategy showed significant statistical difference between cases and controls in this study. Controls seemed to accept responsibilities to a greater extent (88%). This pattern of coping seemed to be deficient in cases (6%).
Escape-avoidance coping strategy showed highly significant statistical difference between cases and controls in this study. Cases used this coping strategy to a greater extent (89%); controls rarely used this strategy to this extent (10%).
Planful problem solving as a pattern of coping showed significant statistical difference between cases and controls in this study. Controls used to adopt this strategy more (68%) when compared to cases (12%).
Positive appraisal coping strategy showed highly significant statistical difference between cases and controls in this study. Controls (82%) used this strategy to greater extent than cases (10%).
Logistic regression analysis [Table 3] of various parameters with suicide attempters revealed that several factors and coping strategies act as significant risk factors, whereas certain coping strategies do not act as risk factors. A higher number of life events within past 1 month increase the risk of attempting suicide by seven times. The most important factor found from this study was escape-avoidance as a coping strategy shown by suicide attempters, which gave an OR of 22.98. Similarly confronting coping strategy had six times (OR=6.86) risk in making suicide attempts. PSLES score (OR=2.126) and distancing coping (OR=2.784) strategy had double risk in making suicide attempts.
Table 3.
Multivariate logistic regression analysis to assess risk factors
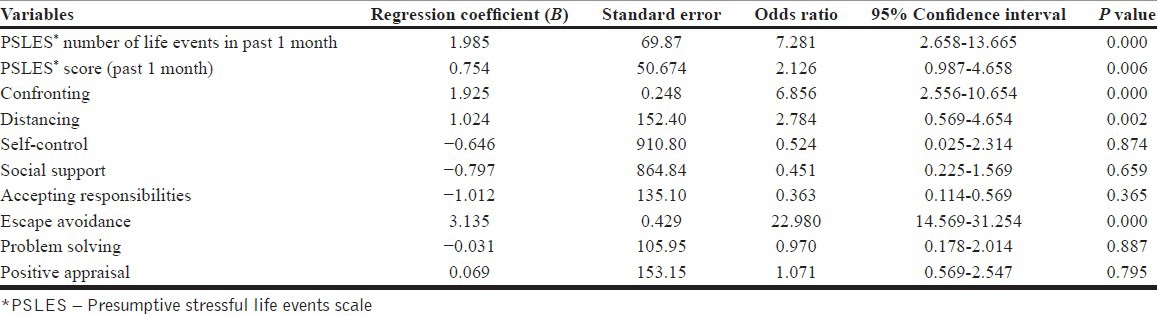
Certain strategies such as self-control, social support, accepting responsibilities, problem solving, and positive appraisal act as protective factors for suicide attempters. Logistic regression analysis gave protective factor value or risk factor (OR) value in not attempting suicide as high value for positive appraisal followed by accepting responsibilities, seeking social support, and self-control.
DISCUSSION
This study was necessitated by the need to evaluate the psychosocial risk factors and patterns of coping associated with adolescent suicide attempts. Only very few studies of similar nature were done in the past. During the assessment, two of the adolescent suicide attempters were excluded due to mental retardation and five of them were excluded due to severe medical complications related to the attempt.
Socio-demographic variables
The mean age of cases was found to be 17.10±1.53 which is similar to earlier Indian studies. Study by Sudhirkumar[7] had reported mean age of the sample as 17.58±1.26 when 74 adolescent suicide attempters were studied. This increase in rate in later adolescence may be due to greater psychopathology, more cognitive ability to plan and act, more autonomy, and less supervision.[4] Majority (62%) of attempters were females, whereas males formed only 38% of case population. Nearly, all studies on adolescent suicide attempts have reported more representation of females.[4,6,19] Though in the traditional Indian culture, women enjoy a more protected role, the changing expectations, and work force participation, the female sex also experience a concurrent rise in role conflicts and psychosocial stressors. Females are reported to make less lethal attempts than males which were observed in this study also. This study had 12% of cases and 8% controls who were married. In India, the minimum age for marriage for males is 21 years and for females, 18 years. This means that none of the males were married. There had been very few Indian studies which had analyzed the marital status of the adolescent suicide attempters. Sudhirkumar[7] had reported that in their sample of 74 adolescents, 8% were married and 3% separated or divorced. The hostile environment in families, pre-existing personality problems, and mental illness could precipitate suicidal behavior.[8]
In this study, 55% of cases were unemployed and 36% were students. Among students, high school students (especially 10th standard) made more suicide attempts than higher educational group. In this study, however, there was no statistically significant difference between cases and controls when education and socio-economic status were considered. Since age for controls had been matched with cases, educational status need not show much difference in this age group. Higher socio-economic factors are less represented in this study sample probably due to this group preferring private hospitals (especially among cases to avoid legal issues).
Earlier studies have reported that suicide attempts in youth were linked to educational disadvantage.[20] An Indian study identified 41.9% of adolescent suicide attempters to be from lower socio-economic status and 58.1% to be unemployed.[7] Socio-economic factors and unemployment in the etiology of suicide have been recognized as important. It is not suggested that unemployment causes suicide per se, but creates a feeling of hopelessness, which adds further stress to the economically and psychologically vulnerable.
In this study, 84% of cases and 82% of controls belonged to nuclear families. No statistically significant difference was observed between cases and controls. Earlier studies have also reported higher representation of nuclear family setting among adolescent suicide attempters.[7] This over representation could also be due to the disintegration of joint family system within the society which has led to change in family environment and added burden on the family members.[21]
Family history
18% of cases as compared to 2% of controls (P=0.001; statistically significant) had family history of mental illness in this study. Brent and colleagues have looked into the familial factors earlier stating that familial loading of depression and substance use disorders are important risk factors for attempted suicide.[22]
In our study, 12% of cases had family history of suicide or attempt. None of the controls had family history of suicide or attempt. Earlier observations show that suicidal behavior is familial and that liability to suicidal behavior is transmitted in families independent of psychiatric disorder per se.[23]
Repeated suicide attempts
In this study, 8% of cases had a previous history of suicide attempt. Controls were selected on the basis of not having made an attempt in the past. Previous suicide attempt appears to be an important risk factor associated with another attempt in adolescents, as in earlier studies.[7,10,24] Among the eight cases who had attempted suicide earlier, four had slashed their wrists and four had taken a drug overdosage in the previous attempt. The risk factors for making an attempt again include psychopathology such as borderline personality disorder, poorer coping skills, and family history of a psychiatric disorder.
Present attempt
Studies conducted earlier in different parts of India have reported poisoning by insecticides as the commonest method followed by drug overdosage. Our results were comparable to these earlier studies, when mode, nature, intent, and lethality of attempts were studied.[6,7] Usage of organophosphorous compounds as insecticides and easy availability are the contributing factors for its rampant use in suicide attempts. Areas where vegetable poisons like odollum and nerium are commonly available provide an easy source for the attempters. World Health Organization has suggested restricting access to pesticides as a means to reduce suicide attempts.[1] Practice of over the counter issue of drugs should also be curtailed.
Adolescent suicide attempters, in general, are a heterogeneous group though majority of their attempts were impulsive in nature, a cry for help to reduce personal distress. The intent of their act is often found to be low unless associated with severe psychopathology like depressive disorder which was found to be true in our study also.
Psychiatric morbidity
In our study population, 78% of cases had a psychiatric disorder; most common was adjustment disorder (48%) followed by depressive disorder (16%); borderline personality disorder (6%); conduct disorder with alcohol abuse (4%); alcohol dependence syndrome (2%); and psychoses (which included psychotic disorders and mood disorder with psychotic features) in 2%. High rates of psychiatric comorbidity (80%) among adolescent suicide attempters had been observed by earlier researchers.[6,19,23] Study by Sudhirkumar[7] reported that 65% of the sample (n=74) had diagnosable psychiatric disorder. The results obtained in this study were comparable to the above study when psychiatric morbidity was considered. These findings point to the possibility that psychiatric disorders and psychological disturbances are important risk factors for attempted suicide. This is of importance to the professional care givers who provide services to these people so that they can be identified early and necessary interventions can be done before it precipitates an attempt.
Physical illness
In this study, 4% of cases and 2% of controls had chronic physical illness prior to the attempt. Physical illness was not found to be significantly associated with adolescent suicide attempt (P=0.567). Few earlier studies including those of Brent, et al. had postulated poor physical health and disability to be associated with suicidal behavior.
Recent stressful life events
Presumptive Stressful Life Events Scale was used to assess the psychosocial stressor in the study population. The mean number of life events for the cases in the past 1 month was 3.79±0.672 as compared to 1.36±0.559 among controls. The mean stress score of the cases in this study during that time was 229.5±39.89 as compared to 61.12±15.48 among controls. The number of stressful life events (P=0.000; OR 7.28) as well as mean stress scores (P=0.006; OR 2.13) in the past 1 month prior to the attempt was found to be an important risk factor associated with adolescent suicide attempts. The events that preceded an attempt were mostly undesirable events (failure in examination, break up with friend, family conflict, illness or death of family member, excessive alcohol, or drug usage by family member); one of them resorted to an attempt to end his life following death of his pet (puppy). None of the attempts were closely following an exposure to suicide. Majority of the attempters (63%) had reported interpersonal problems as the main precipitating factor for attempt, be it with parents, spouse, in-laws, or friends. The results are comparable to those of earlier researchers including Kar et al.,[6] Sudhirkumar,[7] Beautrais et al.,[20] Marttunen et al.,[25] Brent et al.,[26] and Vijaykumar et al.[27] Factors like being a single child or being brought up by a single parent were not found to be significant factors associated with adolescent suicide attempts.
Paykel et al. had observed that the patients who attempt suicide show as much as four times an incidence of an upsetting life event in the preceding month compared to general population.[28] Elevated levels of undesirable events and exit events in the previous year were observed by Adams et al.[29] The impact of stress is tempered by the mitigating effect of primary (in the family), secondary (among friends, relatives, and neighbors) and tertiary (at social service organizations, religious, and charitable services) factors. But when the person is faced with the issues in the context of interpersonal and family breakdowns, the stressed adolescent who is already in an age of emotional turmoil due to physiological and psychological changes stands in a high-risk position. Therefore, it is imperative that this section of the population needs more psychological and social support, especially during periods of stress.
Patterns of coping
The revised Ways of Coping Questionnaire was used in both cases and controls to find how the groups employed different strategies. In this study, it was found that the controls employed coping mechanisms of self-control, seeking social support, accepting responsibilities, planful problem solving, and positive appraisal to a greater extent when compared to cases. The negative strategies of escape-avoidance (OR 22.98) and confronting (OR 6.86) were used more by the attempters when compared to controls and were acting as significant risk factors associated with adolescent suicide attempts. The above results are comparable to Arulmani's study of competent and disturbed adolescents in the Indian setting.[30] Distancing was used as a coping style to a greater extent by cases in this study. The subscale of distancing has both positive and negative aspects; positive in that persons view their difficulties in a more positive fashion. In this study, it was observed that the cases tend to cope by distancing using the negative aspect, that is, by insulating themselves from active consideration of their problems. The above-mentioned earlier study had observed that competent and disturbed adolescents used to employ distancing, competent trying to make light of their situation, and disturbed trying to insulate from their problems and do nothing about it.
The controls in the study population were found to use self-control as a coping strategy more often than the suicide attempters. They sought social support more frequently. This implied that they actively attempt to gain information regarding possible solutions to their problems, elicit help from others or seek emotional support from others. The attempters on the other hand, manifest this behavior to a lesser extent and thereby tend to suffer the adverse effects of stressors they experience. In the event of stressful situations, the controls were able to accept personal responsibility to a greater extent and acknowledge their personal role in finding solutions. Similar trends were found in the area of planful problem solving, with the controls manifesting deliberate problem-solving efforts to alter the stressfulness of a situation. Those who had resorted to an attempt to end their life, on the other hand, seemed to be less able to perceive their own role in solving their problems and were thereby less able to take a problem-solving approach to stressful situations. In addition, the controls were able to positively reappraise difficulties that they experienced. In spite of being exposed to adverse circumstances, they were able to attribute positive meanings to them by focusing on personal growth. Earlier researchers had also observed similar findings that the competent had positive attitudes, ability to analyze problems and problem-solving skills. Escape-avoidance as a coping mechanism was used to a greater extent by the attempters. They tend to cope using cognitive avoidance such as wishful thinking and fantasy and behavioral avoidance such as resorting to substance use or avoid being with people in general. This has been observed in earlier studies.[31] In summary, the attempters manifest an external locus of control and poor task orientation. Their coping behavior is predominantly characterized by escape-avoidance and confronting. In contrast, the controls demonstrate an internal locus of control and a high level of task orientation. They have a positive attitude toward their problems and manifest coping behavior that is characterized by a problem-solving approach.
When logistic regression was done (using data from this study), it was found that positive strategies such as self-control, positive appraisal, accepting responsibilities, seeking social support, and problem solving were acting as protective factors against adolescent suicide attempts. Hence, it becomes important to teach adolescents proper social skills and healthier and protective patterns of coping so that they will be able to face both normative and non-normative stressors during this period of life. A study evaluating the impact of empowering adolescents with life skills education as part of school mental health program observed that those adolescents in the program had significantly better self-esteem and perceived adequate coping, better adjustment, and prosocial behavior.[32] Steps to incorporate appropriate life-skill training into the curriculum can also be considered. Masten et al. have also observed that among adolescents, better parenting resources were associated with good outcomes across competence domains, even in the context of severe, chronic adversity.[33] Parents and teachers can also be trained so that the healthier and positive behavioral patterns may be taught in the early childhood itself.
Limitations
Limitations of this study are that it is a hospital-based study and that the timing of assessment includes a selection bias as only those medically stable were included as cases.
FUTURE IMPLICATIONS
The outcome of this study has implications in both clinical and public health approaches to the reduction in rates of adolescent suicide attempts. It helps a professional to identify high-risk cases and intervene before the crisis occurs. Promising prevention strategies include school-based skills training for students, screening for at-risk youths, education of primary care physicians, media education, and lethal means restriction. There is a great need for well-designed prospective multicenter longitudinal studies, keeping in view the heterogeneity of adolescent suicidal attempters. Future research should adopt a practice-based approach to examine suitable techniques and skills for counseling adolescent suicide attempters, their needs after recovery and evaluate suicide prevention.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.World Health Organization. Suicide prevention (SUPRE) 2003. [Last accessed on 2012 Aug 31; cited 2012 Sep 9]. Available from: http://www.who.int/mental_health/prevention/suicide/suicideprevent/en .
- 2.International Association of Suicide Prevention. IASP. World Suicide Prevention Day: September 10, 2012. [Last accessed on 2012 Sep 9; cited 2012 Oct 13]. Available from http://www.iasp.info/wspd .
- 3.Accidental Deaths and Suicides in India 2011. New Delhi: Ministry of Home Affairs, Government of India; 2011. National Crime Records Bureau. Suicides in India; pp. 179–89. [Google Scholar]
- 4.Bridge JA, Goldstein TR, Brent DA. Adolescent suicide and suicidal behavior. J Child Psychol Psychiatry. 2006;47:372–94. doi: 10.1111/j.1469-7610.2006.01615.x. [DOI] [PubMed] [Google Scholar]
- 5.Gould MS, Greenberg T, Velting DM, Shaffer D. Youth suicide risk and preventive interventions: A review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 2003;42:386–405. doi: 10.1097/01.CHI.0000046821.95464.CF. [DOI] [PubMed] [Google Scholar]
- 6.Kar N. Profile of risk factors associated with suicide attempts: A study from Orissa, India. Indian J Psychiatry. 2010;52:48–56. doi: 10.4103/0019-5545.58895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sudhirkumar CT. A study of psychosocial and clinical factors associated with adolescent suicide attempts. Indian J Psychiatry. 2000;42:231–42. [PMC free article] [PubMed] [Google Scholar]
- 8.Vijaykumar L. Suicide and its prevention: The urgent need in India. Indian J Psychiatry. 2007;49:81–4. doi: 10.4103/0019-5545.33252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vijayakumar L, John S, Pirkis J, Whiteford H. Suicide in developing countries (2): Risk factors. Crisis. 2005;26:112–9. doi: 10.1027/0227-5910.26.3.112. [DOI] [PubMed] [Google Scholar]
- 10.Spirito A, Esposito-Smythers C. Attempted and completed suicide in adolescence. Annu Rev Clin Psychol. 2006;2:237–66. doi: 10.1146/annurev.clinpsy.2.022305.095323. [DOI] [PubMed] [Google Scholar]
- 11.Wilson KG, Stelzer J, Bergman JN, Kral MJ, Inayatullah M, Elliott CA. Problem solving, stress, and coping in adolescent suicide attempts. Suicide Life Threat Behav. 1995;25:241–52. [PubMed] [Google Scholar]
- 12.Piquet ML, Wagner BM. Coping responses of adolescent suicide attempters and their relation to suicidal ideation across a 2-year follow-up: A preliminary study. Suicide Life Threat Behav. 2003;33:288–301. doi: 10.1521/suli.33.3.288.23212. [DOI] [PubMed] [Google Scholar]
- 13.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- 14.World Health Organization. The ICD-10 Classification of Mental and Behavioral Disorders: Clinical Descriptions and Diagnostic Guidelines, A.I.T.B.S. Delhi (Authorized reprint): Publishers and Distributors; Mental and Behavioral Disorders; pp. 22–291. [Google Scholar]
- 15.Singh G, Kaur D, Kaur H. Agra: National Psychological Corporation; 1983. Handbook for Presumptive Stressful Life Events Scale; pp. 10–20. [Google Scholar]
- 16.Folkman S, Lazarus RS, Dunkel-Schetter C, DeLongis A, Gruen RJ. Dynamics of a stressful encounter: Cognitive appraisal, coping, and encounter outcomes. J Pers Soc Psychol. 1986;50:992–1003. doi: 10.1037//0022-3514.50.5.992. [DOI] [PubMed] [Google Scholar]
- 17.Folkman S, Lazarus RS. If it changes it must be a process: Study of emotion and coping during three stages of a college examination. J Pers Soc Psychol. 1985;48:150–70. doi: 10.1037//0022-3514.48.1.150. [DOI] [PubMed] [Google Scholar]
- 18.Folkman S, Lazarus RS. An analysis of coping in a middle-aged community sample. J Health Soc Behav. 1980;21:219–39. [PubMed] [Google Scholar]
- 19.Bhugra D, Desai A. Attempted suicide in South Asian women. Adv Psychiatr Treat. 2002;8:418–23. [Google Scholar]
- 20.Beautrais AL. Suicide and serious suicide attempts in youth: A multiple-group comparison study. Am J Psychiatry. 2003;160:1093–9. doi: 10.1176/appi.ajp.160.6.1093. [DOI] [PubMed] [Google Scholar]
- 21.Gehlot PS, Nathawat SS. Suicide and family constellation in India. Am J Psychother. 1983;37:273–8. doi: 10.1176/appi.psychotherapy.1983.37.2.273. [DOI] [PubMed] [Google Scholar]
- 22.Brent DA, Perper JA, Moritz G, Liotus L, Schweers J, Balach L, et al. Familial risk factors for adolescent suicide: A case-control study. Acta Psychiatr Scand. 1994;89:52–8. doi: 10.1111/j.1600-0447.1994.tb01485.x. [DOI] [PubMed] [Google Scholar]
- 23.Brent DA, Mann JJ. Family genetic studies of suicide and suicidal behavior. Am J Med Genetics. 2005;133C:13–24. doi: 10.1002/ajmg.c.30042. [DOI] [PubMed] [Google Scholar]
- 24.Miranda R, Scott M, Hicks R, Wilcox HC, Harris Munfakh JL, Shaffer D. Suicide attempt characteristics, diagnoses, and future attempts: Comparing multiple attempters to single attempters and ideators. J Am Acad Child Adolesc Psychiatry. 2008;47:32–40. doi: 10.1097/chi.0b013e31815a56cb. [DOI] [PubMed] [Google Scholar]
- 25.Marttunen MJ, Aro HM, Lönnqvist JK. Precipitant stressors in adolescent suicide. J Am Acad Child Adolesc Psychiatry. 1993;32:1178–83. doi: 10.1097/00004583-199311000-00010. [DOI] [PubMed] [Google Scholar]
- 26.Brent DA, Perper JA, Moritz G, Baugher M, Roth C, Balach L, et al. Stressful life events, psychopathology, and adolescent suicide: A case control study. Suicide Life Threat Behav. 1993;23:179–87. [PubMed] [Google Scholar]
- 27.Vijayakumar L. Indian research on suicide. Indian J Psychiatry. 2010;52:S291–6. doi: 10.4103/0019-5545.69255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Paykel ES, Prusoff BA, Myers JK. Suicide attempts and recent life events. A controlled comparison. Arch Gen Psychiatry. 1975;32:327–33. doi: 10.1001/archpsyc.1975.01760210061003. [DOI] [PubMed] [Google Scholar]
- 29.Adams DM, Overholser JC, Spirito A. Stressful life events associated with adolescent suicide attempts. Can J Psychiatry. 1994;39:43–8. doi: 10.1177/070674379403900109. [DOI] [PubMed] [Google Scholar]
- 30.Arulmani G. M.Phil Dissertation, 1991 (unpublished) Bangalore: University of Bangalore, National Institute of Mental Health and Neurosciences; Patterns of coping with psychosocial stressors amongst Indian adolescents. [Google Scholar]
- 31.Spirito A, Overholser J, Stark LJ. Common problems and coping strategies. II: Findings with adolescent suicide attempters. J Abnorm Child Psychol. 1989;17:213–21. doi: 10.1007/BF00913795. [DOI] [PubMed] [Google Scholar]
- 32.Srikala B, Kishore KK. Empowering adolescents with life skills education in schools-School mental health program: Does it work? Indian J Psychiatry. 2010;52:344–9. doi: 10.4103/0019-5545.74310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Masten AS, Hubbard JJ, Gest SD, Tellegen A, Garmezy N, Ramirez M. Competence in the context of adversity: Pathways to resilience and maladaptation from childhood to late adolescence. Dev Psychopathol. 1999;11:143–69. doi: 10.1017/s0954579499001996. [DOI] [PubMed] [Google Scholar]


