Abstract
Background:
This study aims to determine the prevalence and socio-demographic correlates of caregiver's burden in schizophrenia.
Materials and Methods:
A dyad of 368 schizophrenia patients and their caregivers were interviewed. Caregiver's burden was assessed using the Yoruba-version of the FBIS and GHQ-12.
Results:
Mean age of patients was 29.7 SD (8.6) years. Of the 368 caregivers, 81.5% were parents, mean age was 58.1 years (SD 19.6). Total mean objective FBIS score was 22.69 (6.21), 324 (85.3%) reported total objective burden and 310 (84.2%), subjective burden. There were significant differential demographic associations with caregivers’ burden.
Conclusion:
Caregivers of schizophrenia patients experience enormous burden and are potential “high risk group” for mental disorders. Thus, they require comprehensive intervention in order to reduce the growing incidence of chronic enduring diseases including mental disorders.
Keywords: Caregiver's burden, Yoruba version of family burden interview schedule, schizophrenia
INTRODUCTION
The term “burden of care” emerged after the closure of mental hospitals when patients were followed-up outside of the hospital setting[1] and family members assumed responsibility for these patients, thereby becoming the primary caregivers within the home environment. This construct can be conceptualized as a syndrome of varying clustering affecting the general and mental health of caregivers.[2]
Caregivers burden has two dimensions, “objective burden” (effects on the household including financial loss; effects on health, on children, and family routine; and the abnormal behaviors shown by the patient) and “subjective burden” (the extent to which relatives felt they carried a burden).[3] Some researchers though have erroneously considered subjective burden as same as stress.[4]
Despite reports of substantial social support for mentally ill in developing nations,[5] in Nigeria, with a population of 160 million people,[6] the burden of care of schizophrenia patients on their caregivers is enormous. This could be adduced to a number of reasons including inadequate access to formal mental health service and poor health service profile of the country including serious dearth in number of mental health professionals.[7] Since family burden may be influenced by differences in mental health service provisions, social network, and other cultural factors,[8,9] it is important to recognize that generalizing the concept of family burden based on reports from the western countries which emphasized family burden as fallout of de-institutionalization[1] may be erroneous. A few studies have been carried out in Nigeria on burden of caregivers of schizophrenia patients;[10,11] however, there is no local study on prevalence of family burden using the FBIS.[3]
This study, therefore, set to determine the prevalence of burden of caring among caregivers of schizophrenia patients, and to determine the socio-demographic correlates of caregivers’ burden.
The eventual aims include using the findings in implementing programs to address the needs of the caregivers of schizophrenia patients.
MATERIALS AND METHODS
Patients
Patients were recruited from the Psychiatric Unit of Ring Road State Hospital which is the apex hospital for all hospitals under the management of Oyo State Hospitals Management Board and is situated in Ibadan, the capital city of the state. It is the only psychiatric unit in a general hospital in Oyo state of Nigeria with a population of over 5.5 million people.[12] This unit is the only mental health service within a general hospital setting in Oyo State of Nigeria.
The recruitment period of the study was between January and December 2008. Consecutive outpatients under the care of Ring Road State Hospital, Psychiatric Unit with a principal diagnosis of schizophrenia, and their respective caregivers constituted the sample population. The assessments were conducted by a single rater who was the only attending psychiatrist at the facility throughout the period of study.
Participants provided written informed consent and Ethical approval to conduct the study was obtained from Ethical Review Committee of the Department of Planning, Research and Statistics, Ministry of Health, Oyo State, Nigeria in December 2007.
The diagnoses of the patients were made by the consultant psychiatrist.
All of the patients recruited met the principal diagnosis of schizophrenia according to the Structural Clinical Interview for DSM IV Axis I disorder (SCID)[13] after an initial psychosis screening.[14] Patients with any additional DSM IV axis I, any axis II, or axis III diagnoses were excluded from the study.
Caregivers
The Family Burden Interview Schedule (FBIS): This scale measures objective and subjective aspects of burden and it contains six general categories of burden, each having two to six individual items for further investigation. Subcategories include: Financial burden, effects on family routine, effects on family leisure, effects on family interaction, effects on physical health of family members, and effects on mental health of other family members. Each item is rated on a three-point scale, where 0 is no burden and 2 is severe burden.[3] The Y-FBIS has been validated among Yoruba speaking Nigerian caregivers. Internal consistency of the Y-FBIS was demonstrated by a significant Cronbach α of between 0.62 and 0.82 for each item. Test retest reliability of individual scales ranged from 0.780 and 0.874 and was 0.830 for total objective scale score.[15]
The General Health Questionnaire (GHQ) is a self-administered instrument used for screening for psychiatric morbidity.[16] It has a good internal consistency (Cronbach alpha 0.82 to 0.93).[17] The GHQ has been validated in Nigeria.[18] The Yoruba version of the GHQ-12 (Y-GHQ-12) which was adopted in this study has been validated in Nigeria.[19] The GHQ had been used by researchers to assess caregiver's distress.[20,21]
Caregivers
A “principal caregiver” was selected and for the purpose of this study defined as “a nonprofessional person in the community who was most involved with the everyday care of the case and would be very likely to respond to any request for special assistance at any time, if such a request was made by the case”.[22] In other words, such a person is not paid. An additional criterion was that all the recruited caregivers must have lived exclusively with the patient for at least 1 year prior to recruitment and was not involved in the care of any other family member with any mental or chronic physical illness. They were also Yoruba Speaking Nigerians of either gender aged 18 and above and were able to understand the exercise.
Setting of the interview
Face-to-face interview was arranged with each patient and the principal caregiver. Caregivers were interviewed separate from the patients, to facilitate free expression of their feelings. The interview took place at the special Clinic of the Ring Road State Hospital. Each interview took between 40 and 50 min to complete.
Statistical analysis
The data analysis was according to the two objectives. An estimate of the prevalence and correlates of family burden were obtained. Mean FBIS scores of two variables were compared using the student t test and ANOVA when the variables were more than two. The level of significant was set at <0.05. All analyses were performed with the SPSS-version 15.0.[23]
RESULTS
Four-hundred and eight patients with the DSM IV diagnosis of schizophrenia according to the SCID were assessed for their eligibility to enter the study. Forty of them were excluded for various reasons including the absence of caregiver, multiple diagnoses, medical co-morbidity, and refusal to give consent. As a result, 368 patient-caregiver dyads were recruited.
Of the 368 patients interviewed, 214 (58.1%) were male [Table 1]. Their age ranged from 14 to 58 years, with a median of 32 years. Only 61 (16.6%) were married, 163 (44.3%) were single, 118 (32.1%) separated, 11 (3.0%) divorced, and 5 (1.4%) were widowed.
Table 1.
Sociodemographic characteristics of patients and caregivers

Seventy-six (20.7%) had no formal education, while the rest, 292 (79.3%) had at least some elementary education. The median year of education was 4 years. The majority, 253 (68.8%) were unemployed. Their mean age was 29.7 (SD=8.6) years, while the median was 27 years. The mean duration of illness was 3.4 years (SD=2.7), while the median was 2 years.
Of the 368 caregivers interviewed, 43 (11.7%) were spouses, 300 (81.5%) were parents, the rest, 57 (6.8%) were non-parent family members. The majority, 266 (77.8%) were female [Table 2]. Sixty-six (17.2%) were married, the rest, 302 (82.9%) were either single, separated, widowed, or divorced. Their age ranged from 18 to 82 with a mean of 58.1 years (SD=19.6), median was 51 years.
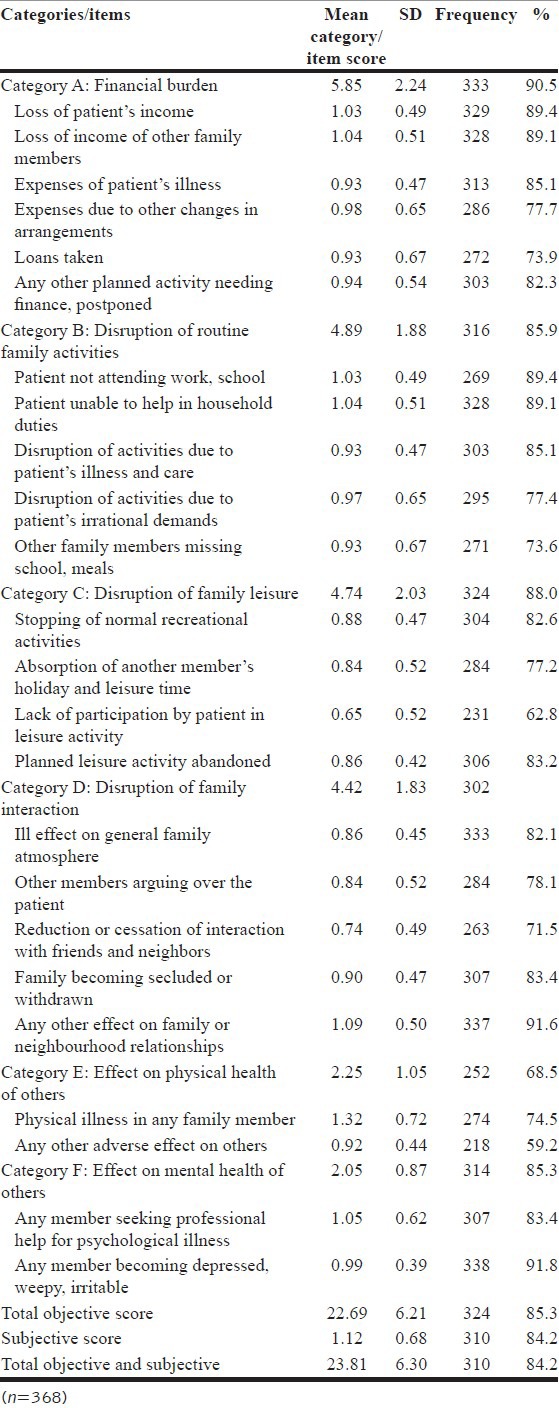
Table 2.
Pattern of objective score at category and item levels
Their mean years of education was 1.8 (SD=0.9); 50.0% of them had no formal education, 35.5% had some elementary education, 8.9% had at least some secondary school education while 5.5% had some post secondary education.
More than half (60.3%) of the caregivers were employed. The mean number of years living with the patient was 11.7 (SD=7.4) and the mean duration of care giving was 2.2 years (SD=1.4). The average number of hours per week in contact with the patient was 73.7 (SD=39.6) while 51.1% of the caregivers scored ≥3 on GHQ [Table 1].
Mean burden score in the domain of financial burden (category A) was 5.85 (2.24), disruption of routine family activities (B) 4.89 (1.88), disruption of family leisure (C) 4.74 (2.03), disruption of family interactions (D) 4.42 (1.83), effect on physical health of others (E) 1.32 (0.72), effect on mental health of others (F) 0.99 (0.39). Total mean objective score was 22.69 (6.21), mean subjective score was 1.12 (0.68). 333 (90.5%) respondents reported burden in the domain of financial burden, 316 (85.9%) in the domain of disruption of routine family activities, 324 (88.0%) in the domain of disruption of family leisure, 302 (82.1) in the domain of disruption of family interactions, 307 (83.5%) in effect on physical health of others, 312 (84.8), in effects on mental health of others 314 (85.3%), global burden, 324 (85.3%), and 310 (84.2) in subjective burden [Table 2].
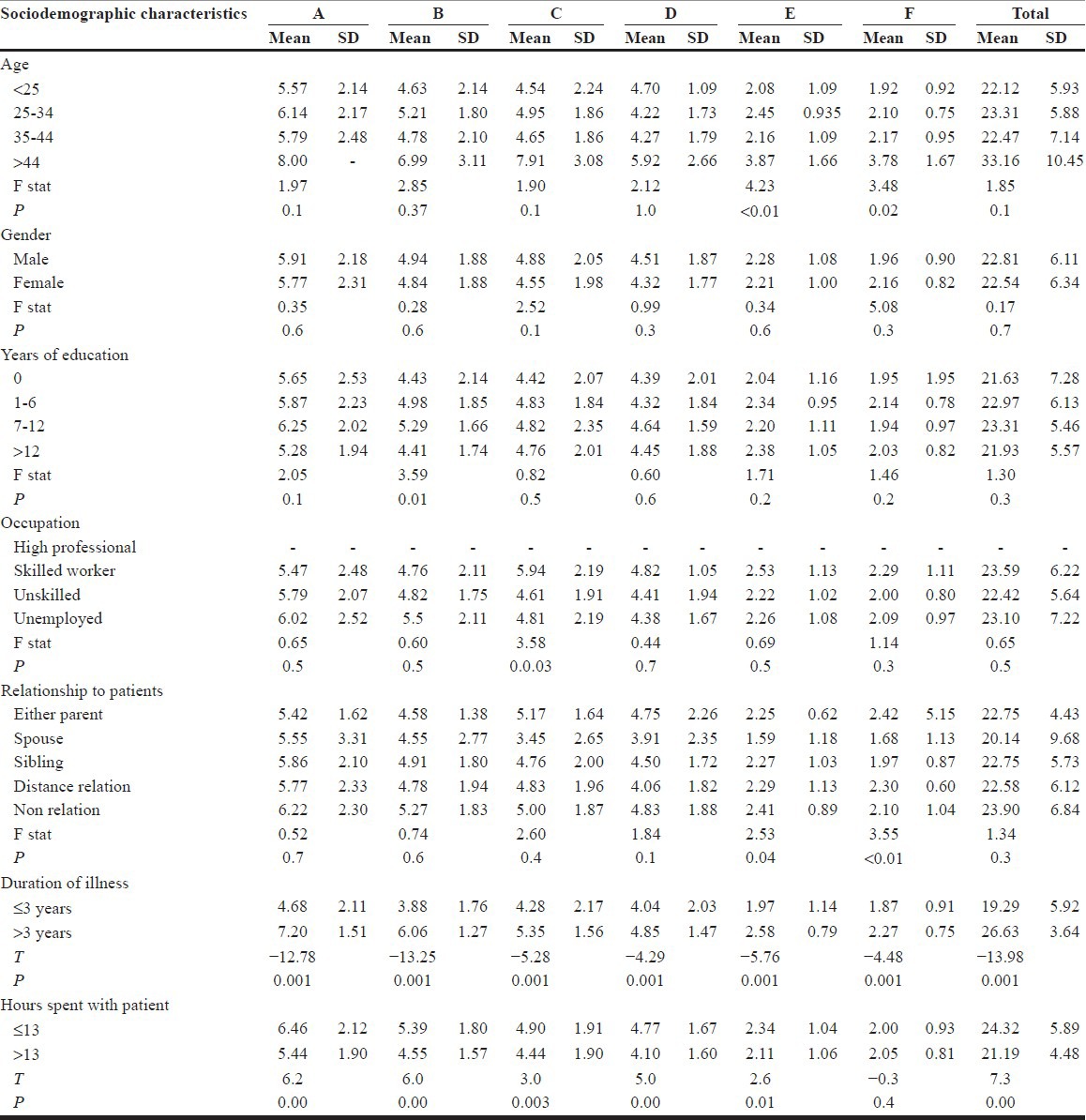
Significant factors that were associated with caregivers’ burden were: Age in the domains of effect on physical health of others and effect on mental health of others F, P<0.01, P=0.02 respectively; years of education, P=0.01 in the domain of disruption of routine family activities; occupation of caregiver P=0.03 in the domain of disruption of family leisure, and relationship of caregiver to patient on items domain of effect on physical health of others and effect on mental health of others, P=0.04, P<0.01, respectively [Table 3].
Table 3.
Sociodemographic characteristics and mean subcategory score for categories A to E of the Y-family burden interview schedule
DISCUSSION
To the best of the researchers’ knowledge, this is the first study evaluating caregivers’ burden in Nigeria using the validated version of the FBIS. In brief, the key findings in this study were that 85.3% of caregivers of schizophrenia patients experienced at least some amount of objective burden; 84.2% experienced at least some subjective burden. The mean total score of the Y-FBIS was 22.69 (SD=6.21).
This result highlights the diverse areas of caregivers’ burden in a developing nation with little or no resources for the care of mentally ill. The area rated to have created the highest level of burden was “financial burden” (90.5%), while “effect on physical health of others” was rated least burdensome (68.4%). This study has reported some socio-demographic correlates of caregivers’ burden such as age, education, occupation, relationship to patient, duration of illness, and hours spent with patients in some categories of caregivers’ burden. In total objective scale, this study has identified only duration of illness and hours spent with patients to be associated with caregivers’ burden.
When the socio-demographic profiles of the caregivers in this study were compared with an earlier study in China that utilized same caregivers’ assessment instrument,[25] results from this study showed that caregivers were generally older, had fewer years of education, fewer proportions were married but a larger proportions were either unskilled workers or unemployed. The mean FBIS scores reported were also generally lower than the baseline figures in that study. These generally low mean FBIS figures may be potentially ascribed to the effect of social network and effective support system in Nigeria.[5]
Results from this study showed that older caregivers significantly reported burden in the areas of “effect of illness on physical health of others” and “effect of illness on mental health of others.” This finding corroborates reports that general medical conditions are very prevalent within the older age groups.[26] It also suggests that older caregivers are more “at risk” of mental health problems as a result of care giving.
The salience of caregiver education which is one of the most replicated findings in this field of study[27,28] was only reported in the domain of “disruption of routine family activities.” However, contrary to reported association between low level of education and caregivers’ burden, the present study found a significant association between high level of education (secondary school education) and caregiver's burden. It is possible that higher level education was responsible for greater perception of the complexities involved in care giving.
In this study, when spouses were compared with other caregivers, spouses were found to have the lowest mean FBIS score in the areas of “effect of illness on physical health of others” and “effect of illness on the mental health of others.” This is contrary to previous studies that reported high level of burden among the spouses.[28,29] A potential explanation for low level of burden in the aforementioned areas is that spouses would be more tolerant of the behaviors of their partners compared with any other caregiver. This may be an example of the concept of “dissonance” in the experience of burden.[30] In a German study, it was noted that many spouses reported low level of burden when their partners had mentally illnesses.[31]
The category where the largest proportion of caregivers reported burden is “financial Burden” (90.6%). This is not unexpected considering the continuing salience of family out-of-pocket expenses for the care of patients in a country such as Nigeria where National health profile is still poor.[7]
The present study also found support for the notion that long duration of schizophrenia could affect objective burden, including the physical deterioration of family caregivers and financial difficulties.[32]
The finding that over 80% of caregivers reported moderate to high level of subjective burden is notable. Moreover, subjective burden mediates stress reaction in caregivers to the burden of care and some researchers have erroneously considered subjective burden as equal to stress.[33] This finding is consistent with stress-process models,[34] which posit that caregivers’ burden mediate the association between stressors and psychological distress. This is further exemplified by the finding that the item on which the highest number of caregivers reported burden is “Any member becoming depressed, weepy, irritable” (91.6%). This may further suggest an interaction between caregivers’ burden and emotional problems.
In contrast to reports indicating that higher burden was associated with more hours of contact with the patient,[2,29] the present study found an inverse relationship. This was so in four categories: Financial burden, disruption of routine family activities, disruption of family leisure, and disruption of family interaction and also in the total subjective burden. As for financial burden, the potential explanation is that caregivers who spent shorter hours incur extra on expenditure on transportation, more so, findings from this study indicated that those in employment reported greater burden than the unemployed. As for disruption of routine family activities, disruption of family leisure and disruption of family interaction, this inverse relationship could be ascribed to the large extended family system in Nigeria, whereby other family members absorb part of the burden, which is later transferred to the main caregiver by their critical comments. There is also the tendency for main caregiver to aspire to impress other family members to his own detriment. This and the extra expenditure on transportation may be a postulation for the higher total objective burden among those who spent shorter hours with their patients.
In support of Montero's finding that over 55% of caregivers of schizophrenia had high GHQ score,[35] the present study found that 51.1% of caregivers scored above the GHQ cut off point indicating psychological distress, although no attempt was made in allocating psychiatric diagnoses to the caregivers despite this. However, this finding suggests that caregivers are potential “high risk group” for mental disorders. Thus, they constitute a group of individuals who require medical, psychological, and social intervention in order to reduce the growing incidence of chronic non-communicable diseases including mental health problems. This therefore calls for policies that focus on provision and funding of programmes that are targetted at social and occupational rehabilitation for patients, as well as psychoeducational programmes and psychosocial support for families and care givers of patients with schizophrenia. Collaborative efforts involving government agencies, non-government organisations and other stakeholders have a better chance of success.
This study was limited by a number of factors. The Y-FBIS like the English version does not have cut-off points that may serve as focus of clinical intervention. It is rated over only 3 points, no burden, moderate burden, and severe burden. Thus, it requires more anchor points for the response to give a more meaningful interpretation.
A structured personality and IQ assessments were not carried out, to determine whether the patients had intellectual impairment or personality disorder, these could have created additional burden to the care of the patients. Caregivers IQ and personality could also mediate their perception of and reaction to caregiver burden.
Although we assessed patients’ severity of symptoms and other related measures, these will be addressed in subsequent paper from the parent study.
The impact of patient's socio-demographic variables on burden was not assessed. There is a need for more research on this to determine whether they have equivalent effects with clinical variables on burden or rather have a differential effect.
Risk factor analysis was not carried out and this has greatly limited the interpretation of various bivariate relationships.
Footnotes
Source of Support: The Invaluable contributions of Dr. Kazeem Adebayo, Dr. Yomi Esan, Dr. Laolu Aremu, Dr. George Lasebikan, CNO Biola Lasebikan, PNO Kemi Oke, NO Yinka Olawale, NO Muyiwa Lasisi, Mr. Sola Ogundeji, Christy Alabi is appreciated. We also acknowledge the patients and caregivers who kindly consented to participate in this study. The funding support of New World Psychiatric Hospital, Ibadan, Nigeria is also acknowledged
Conflict of Interest: None.
REFERENCES
- 1.Awad AG, Voruganti LN. The burden of schizophrenia on caregivers: A review. Pharmacoeconomics. 2008;26:149–62. doi: 10.2165/00019053-200826020-00005. [DOI] [PubMed] [Google Scholar]
- 2.Schene AH, van Wijngaarden B, Koeter MW. Family caregiving in schizophrenia: Domains and distress. Schizophr Bull. 1998;24:609–18. doi: 10.1093/oxfordjournals.schbul.a033352. [DOI] [PubMed] [Google Scholar]
- 3.Pai S, Kapur RL. The burden on the family of a psychiatric patient: Development of an interview schedule. Br J Psychiatry. 1981;138:332–5. doi: 10.1192/bjp.138.4.332. [DOI] [PubMed] [Google Scholar]
- 4.Stull DE, Kosloski K, Kercher K. Caregiver burden and generic well-being: Opposite sides of the same coin? Gerontologist. 1994;34:88–94. doi: 10.1093/geront/34.1.88. [DOI] [PubMed] [Google Scholar]
- 5.Lasebikan V, Asuzu M, Owoaje E. Social network as a determinant of pathway to mental health service utilization among psychotic patients in a Nigerian hospital. Ann Afr Med. 2012;11:12–20. doi: 10.4103/1596-3519.91010. [DOI] [PubMed] [Google Scholar]
- 6.Population Reference Bureau. 2011 World population data sheet. [Last accessed on 2011]. Available from: http://www.prb.org/pdf11/2011population-data-sheet_eng.pdf .
- 7.Gureje O. Psychiatry in Africa: The myths, the exotic, and the realities. Afr J Psychiatry (Johannesbg) 2007;10:11–4. [Google Scholar]
- 8.Roick C, Heider D, Bebbington PE, Angermeyer MC, Azorin J-M, Brugha TS, et al. Burden on caregivers of people with schizophrenia: Comparison between Germany and Britain. Br J Psychiatry. 2007;190:333–8. doi: 10.1192/bjp.bp.106.025353. [DOI] [PubMed] [Google Scholar]
- 9.van Wijngaarden B, Schene A, Koeter M, Becker T, Knapp M, Knudsen HC, et al. People with schizophrenia in five countries: Conceptual similarities and intercultural differences in family caregiving. Schizophr Bull. 2003;29:573–86. doi: 10.1093/oxfordjournals.schbul.a007029. [DOI] [PubMed] [Google Scholar]
- 10.Ohaeri JU. Caregiver burden and psychotic patients’ perception of social support in a Nigerian setting. Soc Psychiatry Psychiatr Epidemiol. 2001;36:86–93. doi: 10.1007/s001270050294. [DOI] [PubMed] [Google Scholar]
- 11.Ukpong D. Burden and psychological distress among Nigerian family caregivers of schizophrenic patients: The role of positive and negative symptoms. Turk Psikiyatri Derg. 2012;23:40–5. [PubMed] [Google Scholar]
- 12.National Population commission of Nigeria. National results: Population by state and sex. 2007. [Last accessed on 2012 Jun 29]. Available from: http://web.archive.org/web/20110519235026/http://www.population.gov.ng/files/nationafinal.pdf .
- 13.First MB, Spitzer RL, Gibbon M, Williams JB. Washington, DC: American Psychiatric Press, Inc; 1996. Structured clinical Interview for DSM-IV axis I disorders, clinical version, (SCID-CV) [Google Scholar]
- 14.Bebbington P, Nayani T. The psychosis screening questionnaire. Int J Methods Psychiatr Res. [Internet] 1995. [Last accessed on 2012 Jun 28]. Available from: http://psycnet.apa.org/psycinfo/1995-39335-001 .
- 15.Lasebikan V. Validation of Yoruba Version of Family Burden Interview Schedule (Y-FBIS) on Caregivers of Schizophrenia Patients. International Scholarly Research Network (Psychiatry) 2012. 2012:1–8. doi: 10.5402/2012/165179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goldberg DP. London: Oxford university press; 1972. The detection of psychiatric illness by questionnaire. [Google Scholar]
- 17.Goldberg D, Williams P. Windsor. UK: NFER-Nelson; 1988. A user's guide to the GHQ. [Google Scholar]
- 18.Gureje O, Obikoya B. The GHQ-12 as a screening tool in a primary care setting. Soc Psychiatry Psychiatr Epidemiol. 1990;25:276–80. doi: 10.1007/BF00788650. [DOI] [PubMed] [Google Scholar]
- 19.Gureje O. Reliability and the factor structure of the Yoruba version of the 12-item General Health Questionnaire. Acta Psychiatr Scand. 1991;84:125–9. doi: 10.1111/j.1600-0447.1991.tb03115.x. [DOI] [PubMed] [Google Scholar]
- 20.Chien WT, Norman I. The validity and reliability of a Chinese version of the family burden interview schedule. Nurs Res. 2004;53:314–22. doi: 10.1097/00006199-200409000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Kumari S, Singh AR, Verma AN, Verma PK, Chaudhury S. Subjective burden on spouses of schizophrenia patients. Ind Psychiatry J. 2009;18:97–100. doi: 10.4103/0972-6748.62268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Falloon RH, Graham-Hole V, Woodroffe R. Stress and health of informal carers of people with chronic mental disorders. J Ment Health. 1993;2:165–73. [Google Scholar]
- 23.Illinois, Chicago: IBM; 2006. IBM. Statistical Package for Social Studies. [Google Scholar]
- 24.Pineo P, Porter J, McRoberts H. The 1971 census and the socio-economic classification of occupations. Can Rev Sociol Anthropol. 1977;14:91–102. [Google Scholar]
- 25.Chien WT, Chan SW, Morrissey J. The perceived burden among Chinese family caregivers of people with schizophrenia. J Clin Nurs. 2007;16:1151–61. doi: 10.1111/j.1365-2702.2007.01501.x. [DOI] [PubMed] [Google Scholar]
- 26.Naughton C, Bennett K, Feely J. Prevalence of chronic disease in the elderly based on a national pharmacy claims database. Age Ageing. 2006;35:633–6. doi: 10.1093/ageing/afl106. [DOI] [PubMed] [Google Scholar]
- 27.Magaña SM, Ramírez García JI, Hernández MG, Cortez R. Psychological distress among latino family caregivers of adults with schizophrenia: The roles of burden and stigma. Psychiatr Serv. 2007;58:378–84. doi: 10.1176/appi.ps.58.3.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zahid MA, Ohaeri JU. Relationship of family caregiver burden with quality of care and psychopathology in a sample of Arab subjects with schizophrenia. BMC Psychiatry. 2010;10:71. doi: 10.1186/1471-244X-10-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Winefield HR, Harvey EJ. Needs of family caregivers in chronic schizophrenia. Schizophr Bull. 1994;20:557–66. doi: 10.1093/schbul/20.3.557. [DOI] [PubMed] [Google Scholar]
- 30.Veltman A, Cameron J, Stewart DE. The experience of providing care to relatives with chronic mental illness. J Nerv Ment Dis. 2002;190:108–14. doi: 10.1097/00005053-200202000-00008. [DOI] [PubMed] [Google Scholar]
- 31.Jungbauer J, Wittmund B, Dietrich S, Angermeyer MC. The disregarded caregivers: Subjective burden in spouses of schizophrenia patients. Schizophr Bull. 2004;30:665–75. doi: 10.1093/oxfordjournals.schbul.a007114. [DOI] [PubMed] [Google Scholar]
- 32.Lim YM, Ahn YH. Burden of family caregivers with schizophrenic patients in Korea. Appl Nurs Res. 2003;16:110–7. doi: 10.1016/s0897-1897(03)00007-7. [DOI] [PubMed] [Google Scholar]
- 33.Reine G, Lancon C, Simeoni MC, Duplan S, Auquier P. Caregiver burden in relatives of persons with schizophrenia: An overview of measure instruments. Encephale. 2003;29:137–47. [PubMed] [Google Scholar]
- 34.Pearlin LI, Mullan JT, Semple SJ, Skaff MM. Caregiving and the stress process: An overview of concepts and their measures. Gerontologist. 1990;30:583–94. doi: 10.1093/geront/30.5.583. [DOI] [PubMed] [Google Scholar]
- 35.Montero I, Masanet MJ, Lacruz M, Bellver F, Asencio A, García E. Family intervention in schizophrenia: Long-term effect on main caregivers. Actas Esp Psiquiatr. 2006;34:169–74. [PubMed] [Google Scholar]


