Abstract
Background:
Attempted suicide is a common clinical problem in a general hospital setting. It has a serious clinical and socio-economical impact too.
Aims:
To study the psychosocial, psychiatric, and personality profile of the first suicide attempters in a general hospital.
Settings and Design:
Cross-sectional, hospital-based, descriptive study.
Materials and Methods:
All the consecutive cases of first suicide attempt (n=100) treated in a general hospital were studied to know the clinical profile. Variables related to socio-demographic characteristics, family background, suicide characteristics, psychiatric morbidity, and comorbidity were analyzed. Risk-Rescue rating was applied to know the medical seriousness of the suicide attempt. Presumptive stressful life event scale was utilized to calculate life events score. Structured clinical interview (MINI Plus) and semi-structured clinical interview (IPDE) were used for axis-I and axis-II (personality) diagnoses. The results were analyzed using appropriate statistical measures.
Results:
Family history of psychiatric illnesses (31%) and suicide (11%) were noted. Insecticides and pesticides were the most common agents (71%) employed to attempt suicide. Interpersonal difficulties (46%) were the most frequent stressor. Overall medical seriousness of the suicide attempt was of moderate lethality. 93% of the suicide attempters had at least one axis-I and/or axis-II psychiatric disorder. Most common diagnostic categories were mood disorders, adjustment disorders, and substance-related disorders, with axis-I disorders (89%), personality disorders (52%), and comorbidity of psychiatric disorders (51.6%).
Conclusion:
Individuals who made first suicide attempt were young adults, had lower educational achievement; overall seriousness of the suicide attempt was of moderate lethality, high prevalence of psychiatric morbidity, personality disorders, and comorbidity, and had sought medical help from general practitioners.
Keywords: Attempted suicide, comorbidity, psychiatric disorders, personality disorders, stressful life events
INTRODUCTION
Attempted suicide is a common clinical problem in a general hospital setting. It has a serious clinical and socio-economic impact too. Hence, a study of the psychosocial stressors, psychiatric, and personality profile of suicide attempters is worthwhile.
MATERIALS AND METHODS
The current study is a cross-sectional, hospital-based, descriptive study. 100 consecutive cases of first suicide attempt in a general hospital were the samples. Social class was determined using Modified Prasad's classification of social class.[1] Variables related to socio-demographic characteristics, family background, suicide characteristics were assessed using a self-designed proforma. Risk-rescue rating scale was applied to know the medical seriousness after the suicide attempt.[2] Presumptive stressful life event scale was utilized to calculate life events score.[3] Psychiatric morbidity and comorbidity were analyzed using MINI Plus—a structured clinical interview for axis-I diagnoses, and IPDE—a semi-structured clinical interview for axis-II (personality) diagnoses.[4,5] The results were analyzed with SPSS version 10 for Windows using appropriate statistical measures. Written informed consent was obtained from the sample and informants. Ethical clearance was obtained from the Institutional Ethics Committee.
RESULTS
Socio-demographic characteristics
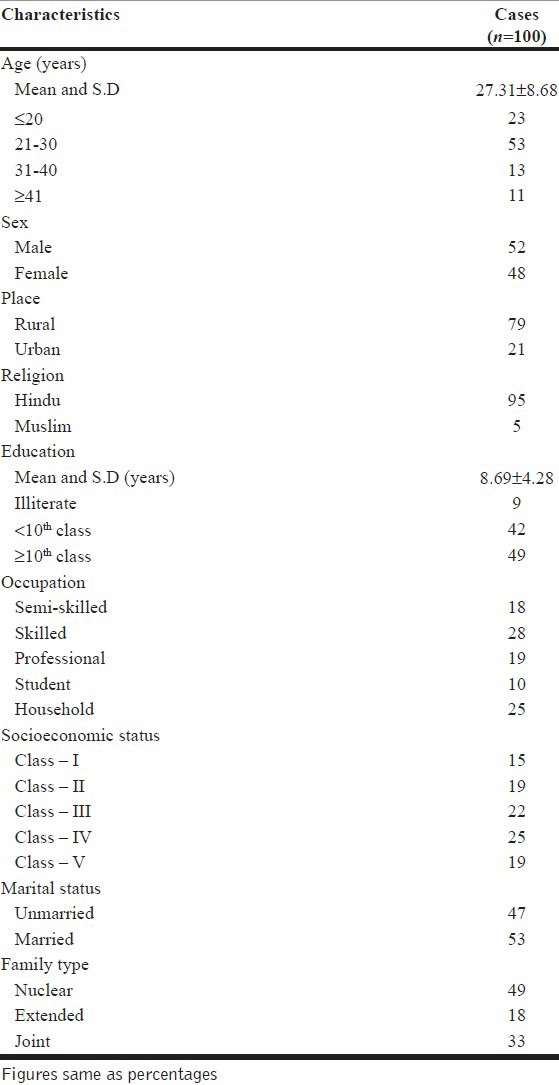
Two thirds of suicide attempters were aged between 21 and 40 years. The mean age was 27.31±8.68 years. There were 52 males and 48 females. A majority (79%) of the subjects were from rural background and were Hindus (95%). Although, literates outnumbered illiterates, mean years of education was 8.69±4.28 years. A majority of the suicide attempters were doing semi-skilled and skilled work. About half of females were housewives and 10% of the samples were students. About half of sample belonged to class-III and -IV on socio-economic status scale and other half were more or less evenly distributed across class-I, -II, and -V. Fifty-three percent were married and 49% were staying in nuclear family [Table 1].
Table 1.
Socio-demographic characteristics of first suicide attempters
Family history
Thirty-one percent of patients had family history of psychiatric disorders, of which 63% had history of substance abuse or dependence and 37% had other psychiatric disorders. Eleven percent had history of suicidal attempt.
Suicide characteristics
Place of the suicide attempt: Majority (87%) of the suicide attempters had chosen a familiar place during the attempt of suicide
Methods of the suicide attempt: Majority (71%) of the suicide attempters had resorted to consumption of chemical compounds. Of poisons, 51% consumed organophosphorus compounds, 9% took rat poisons (aluminum phosphide, zinc phosphide), and 11% other poisons (DDT, phenol, kerosene, diluted sulfuric acid, potassium cyanide, prallethrin, solvent, seeds, naphthalene). Twenty-seven percent had drug overdose with psychotropics (17), antiepileptics (3), and others (7) like oral hypoglycaemics, antihistamines, gammaxene, and lindane. One case had attempted suicide by drowning and another had cut his throat with knife, both were suffering from psychosis. Fifteen percent of the cases had consumed alcohol during the act or had mixed alcohol with substance used to attempt suicide to minimize the perceived “pain” or bitter taste of the poison or the drug
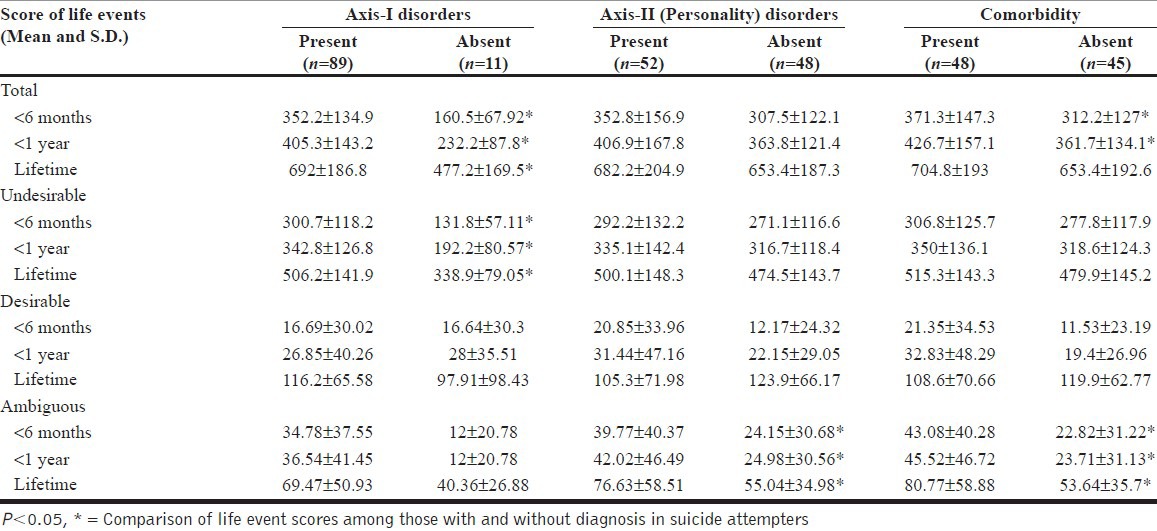
Reasons attributed for the suicide attempt: On repeated confidential interviews with the patient and the informant separately, 97% of patients and 85% of the informants had reported overt stressors. Three percent of cases and 15% of informants reported no overt reason and some of them reported that the consumption of chemical compound was accidental or mistaking it in place of medicines given for symptoms of headache, pain abdomen, common cold, and fever. Forty-six percent of the suicide attempters and 37% of informants reported interpersonal difficulties as the stressor. Other life events such as debts (10%), failure in examination (3%), bereavement (2%), loss of valuables (2%), traumatic facial injury (1%), infertility (1%) were reported from remaining cases. Mean scores of total, undesirable, and ambiguous life events during past 6 months, past 1 year, and lifetime were significantly higher among the suicide attempters who had axis-I and axis-II comorbidity, with lesser desirable life events during the past 6 months [Table 2]
Medical help or advice sought prior to the suicide attempt: 25% of the suicide attempters had already sought medical help from the general practitioners/local doctors but, none had received psychiatric help for their problems
Persistent suicidal ideas: About half of those who reported suicidal ideations (62%) prior to the suicide attempt had persistent suicidal ideas even after being medically stabilized
Hospital stay and events: 31% of the cases suffered from medico-surgical complications related to the mode of suicide attempt, of which 20% (6 cases) needed mechanical ventilator support with mean duration of 9.17±6.43 days. Most common complications were; aspiration pneumonia (13%), respiratory failure (6%), seizures (5%), hypotension (2%), cerebellar toxicity (2%; due to phenytoin, carbamazepine), and others (3%; hemoptysis, dysphonia, hypoglycemia, and hypocalcaemia). The mean total hospitalization duration of suicide attempters was 8.04±4.79 days. The mean duration for medical stabilization was 3.98±4.6 days
Risk-rescue rate: 41% of cases had mild lethality, 33% had moderate lethality, 18% had severe lethality, and 8% had very severe lethality of the suicidal attempt. As the lethality of the suicide attempt increased, the incidence of complications also increased. The mean risk score of 2.09±0.9 suggest low moderate lethality and mean rescue score of 3.62±1.29 suggest that majority of cases had high moderate rescuability (low intentionality). The mean risk-rescue rate of 37.35±16.05 suggests that the overall seriousness of the suicide attempt was of moderate lethality (low risk, high rescue).
Table 2.
Stressful life events in first suicide attempters
Psychiatric morbidity and comorbidity
93% of the suicide attempters had at least one axis-I and/or axis-II diagnosis. Very few (7%) cases had no diagnosable axis-I or axis-II diagnoses. Mood disorders (47%), neurotic, stress-related and somatoform disorders (33%), and substance-related disorders (25%) were the most common axis-I disorders. Among mood disorders, major depression was predominant (35%) and among neurotic-stress-related disorders, adjustment disorder was predominant (27%). Psychotic disorders were diagnosed in 11% of cases. Alcohol dependence was noted exclusively among males (14%). Forty-eight percent cases had comorbid axis-I and axis-II (personality disorder) diagnosis.
Personality disorder morbidity
Nearly half of the cases had at least one personality disorder comorbid with at least one axis-I disorder. Very few cases (4%) had axis-II personality disorder alone. Most common cluster of personality disorder was cluster-B (impulsive, borderline, anankastic) followed by cluster-A (schizoid, paranoid) and cluster-C (anxious). Emotionally unstable-impulsive type, schizoid, paranoid, and anankastic personality disorders were most frequent personality disorders.
DISCUSSION
The mean age of the sample being 27.31±8.68 years may mean that in a general hospital, suicide is a problem of young adults. Equal representations of gender, religion, education, economic, and rural background have been found to be in accordance with socio-demographic profile of the country. This finding has also been supported by a prospective Western study that the socio-demographic factors in suicide attempters did not differ from general population.[6] The mean years of education of 8.69±4.28 years reflect that low literacy rate is a factor of importance in suicide attempt. Low representation of unemployment in the sample study in contrast to Western study[6] may be due to difficulty in its identification in agrarian than in industrialized countries and also that lower need of employment in most females who were housewives and students. Socio-economic status of the sample is in concurrence with Indian studies[7] and Western studies.[8,9] However, in general this finding calls for an improvement of access to medical care for middle and lower socio-economic groups.[10]
High preponderance of family history of psychiatric disorders in the sample (31%) is in variance with other studies that have quoted figures as low as 1.5% and as high as 71%.[11,12] The difference may be due to place of sample selection and method of obtaining family history.
As with the present study, most of the Indian studies report that consumption of organophosphorus compound as a common mode of suicidal attempt.[7,11,13,14,15,16] This may be due to its easy availability especially in rural population. This may call for some restrictions on availability of these compounds.
Higher risk-rescue rate in the sample (26%) signifying medically serious suicide attempt in the sample is in contrast with other Indian studies of 15% and 6%.[13,17] This may be due to the sample selection from a tertiary care center. Nevertheless, the overall mild to moderate risk-rescue rate in three-fourth cases signifying low intentionality may mean that suicidal attempt is more a cry for help rather than an attempt at annihilation.
Concurring with other Indian[11,13,18,19,20] and Western studies,[21,22,23,24,25] higher prevalence of (97%) stressors prior to the suicidal attempt may be due to poor problem solving skills that leads to cognitive constriction and an easy way out approach through annihilation. The “psychic pain” could be too much to bear for the attempters such that suicide is looked upon as “one and the only solution” to solve their problems.[18] However, the stressors may serve only as a precipitating factor and may not be a causal one. Among the stressor nearly half of the cases reported interpersonal conflicts with significant persons. This may suggest that such persons are highly sensitive to interpersonal rejection. This factor may have to be focused in counseling sessions of such persons. Among students, 30% were related to academic and 70% to non-academic reasons as predisposing factor to attempt suicide. Thus, it is important to find not only the quantity and type of the stressors but also the patients’ perception of the stressors and their coping style.
As reflected in Indian study, the current study concurs that mental disorders occupy a premier position in the matrix of causation of suicide, with affective disorders being the most important diagnosis related to suicide.[26] Robins et al. opined suicide practically does not occur without the presence of mental illness, most commonly depression and thereafter alcoholism.[27]
The presence of personality disorders in nearly half of the sample may mean that it could be a determinant of suicidal behavior. It acts in many ways: by predisposing to major psychiatric disorders such as depression or alcoholism, by leading to difficulties in relationship and social adjustment, by precipitating undesirable life events, by impairing the ability to cope with a psychiatric or physical disorder, and by drawing a person into conflicts with family members and others. However, prevalence of personality disorders may vary in studies due to different diagnostic criteria and screening tools used.
As substantial number of suicidal attempters seek help from general practitioners, as also observed by another Indian study,[13] there is an imminent need to sensitize this section of medical professionals with regarding to suicide prevention and assessment of psychiatric morbidity.
In conclusion, individuals who made first suicide attempt were young adults, had lower educational achievement; high family history of psychiatric illnesses; more undesirable and ambiguous life events; moderate lethality and low intentionality of suicide attempt; more psychiatric morbidity, personality disorders, and comorbidity; and had sought medical help from general practitioners.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Prasad BG. Social classification of Indian families. J Indian Med Assoc. 1961;37:250–1. [PubMed] [Google Scholar]
- 2.Weisman AD, Worden JW. Risk-rescue rating in suicide assessment. Arch Gen Psychiatry. 1972;26:553–61. doi: 10.1001/archpsyc.1972.01750240065010. [DOI] [PubMed] [Google Scholar]
- 3.Singh G, Kaur D, Kaur H. Presumptive stressful life events scale (PSLES) – A new stressful life events scale for use in India. Indian J Psychiatry. 1984;26:107–14. [PMC free article] [PubMed] [Google Scholar]
- 4.Sheehan DV, Lecrubier Y, Harnett-Sheehan K, Amorim P, Janavs J, Weiller E, et al. The Mini International Neuropsychiatric Interview (M.I.N.I): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- 5.Loranger AW, Sartorius N, Andreoli A, Berger P, Buchheim P, Channabasavanna SM, et al. The international personality disorder examination: The World Health Organization/Alcohol Drug Abuse and Mental Health Administration international pilot study of personality disorders. Arch Gen Psychiatry. 1994;51:215–24. doi: 10.1001/archpsyc.1994.03950030051005. [DOI] [PubMed] [Google Scholar]
- 6.Nordentoft M, Rubin P. Mental illness and social integration among suicide attempters in Copenhagen: Comparison with the general population and a four year follow-up study of 100 patients. Acta Psychiatr Scand. 1993;88:278–85. doi: 10.1111/j.1600-0447.1993.tb03457.x. [DOI] [PubMed] [Google Scholar]
- 7.Kumar NS. Age and gender related analysis of psychosocial factors in attempted suicide. Indian J Psychiatry. 1998;40:338–45. [PMC free article] [PubMed] [Google Scholar]
- 8.Johnson BA, Brent DA, Bridge J, Connolly J. The familial aggregation of adolescent suicide attempts. Acta Psychiatr Scand. 1998;97:18–24. doi: 10.1111/j.1600-0447.1998.tb09957.x. [DOI] [PubMed] [Google Scholar]
- 9.Haw C, Hawton K, Houston K, Townsend E. Psychiatric and personality disorders in deliberate self-harm patients. Br J Psychiatry. 2001;178:48–54. doi: 10.1192/bjp.178.1.48. [DOI] [PubMed] [Google Scholar]
- 10.Lorant V, Kunst AE, Huisman M, Costa G, Mackenbach J. Socio-economic inequalities in suicide: A European comparative study. Br J Psychiatry. 2005;187:49–54. doi: 10.1192/bjp.187.1.49. [DOI] [PubMed] [Google Scholar]
- 11.Srivastava MK, Sahoo RN, Ghotekar LH, Dutta S, Danabalan M, Dutta TK, et al. Risk factors associated with attempted suicide: A case control study. Indian J Psychiatry. 2004;46:33–8. [PMC free article] [PubMed] [Google Scholar]
- 12.Runeson B. Mental disorder in youth suicide. Acta Psychiatr Scand. 1989;79:490–7. doi: 10.1111/j.1600-0447.1989.tb10292.x. [DOI] [PubMed] [Google Scholar]
- 13.Latha KS, Bhat SM, D’souza P. Suicide attempters in a general hospital unit in India: Their socio-demographic and clinical profile - emphasis on cross-cultural aspects. Acta Psychiatr Scand. 1996;94:26–30. doi: 10.1111/j.1600-0447.1996.tb09820.x. [DOI] [PubMed] [Google Scholar]
- 14.Chandrasekaran R, Gnanaseelan J, Sahai A, Swaminathan RP, Perme B. Psychiatric and personality disorders in survivors following their first suicide attempt. Indian J Psychiatry. 2003;45:45–8. [PMC free article] [PubMed] [Google Scholar]
- 15.Narang RL, Mishra BP, Mohan N. Attempted suicide in Ludhiana. Indian J Psychiatry. 2000;42:83–7. [PMC free article] [PubMed] [Google Scholar]
- 16.Singh SP, Santosh PJ, Avasthi A, Kulhara P. A psychosocial study of ‘self-immolation’ in India. Acta Psychiatr Scand. 1998;97:71–5. doi: 10.1111/j.1600-0447.1998.tb09966.x. [DOI] [PubMed] [Google Scholar]
- 17.Bagadia VN, Abhyankar RR, Shroff P, Mehta P, Doshi J, Chawla R, et al. Suicidal behavior: A clinical study. Indian J Psychiatry. 1979;21:370–5. [Google Scholar]
- 18.Joseph Raj MA, Kumaraiah V, Bhide AV. Social and clinical factors related to deliberate self-harm. NIMHANS J. 2000;18:3–18. [Google Scholar]
- 19.Badrinarayana A. Suicidal attempt in Gulbarga. Indian J Psychiatry. 1977;19:69–70. [Google Scholar]
- 20.Ponnudurai R, Jeyakar J, Saraswathy M. Attempted suicides in Madras. Indian J Psychiatry. 1986;28:59–62. [PMC free article] [PubMed] [Google Scholar]
- 21.Morgan HG, Burns-Cox CJ, Pocock H, Pottle S. Deliberate self-harm: Clinical and socio-economic characteristics of 368 patients. Br J Psychiatr. 1975;127:564–74. doi: 10.1192/bjp.127.6.564. [DOI] [PubMed] [Google Scholar]
- 22.Heikkinen M, Aro H, Lonnqvist J. The partners’ view on precipitant stressors in suicide. Acta Psychiatr Scand. 1992;85:380–4. doi: 10.1111/j.1600-0447.1992.tb10323.x. [DOI] [PubMed] [Google Scholar]
- 23.Lesage AD, Boyer R, Grunberg F, Vanier C, Morissette R, Menard-Buteau C, et al. Suicide and mental disorders: A case-control study of young men. Am J Psychiatry. 1994;151:1063–8. doi: 10.1176/ajp.151.7.1063. [DOI] [PubMed] [Google Scholar]
- 24.Hawton K, Fagg J, Simkin S, Bale E, Bond A. Trends in deliberate self-harm in Oxford, 1985-1995: Implications for clinical services and the prevention of suicide. Br J Psychiatry. 1997;171:556–60. doi: 10.1192/bjp.171.6.556. [DOI] [PubMed] [Google Scholar]
- 25.Paykel ES, Dowlatshahi D. Life events and mental disorder. In: Fisher S, Reason J, editors. Handbook of life stress, cognition and health. Chichester: John Wiley and Sons; 1988. pp. 241–63. [Google Scholar]
- 26.Vijaykumar L. Suicide and its prevention: The urgent need in India. Indian J Psychiatry. 2007;49:81–3. doi: 10.4103/0019-5545.33252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Robins E, Murphy GE, Wilkinson RH, Gassner S, Kayes J. Some clinical considerations in the prevention of suicide based on a study of 134 successful suicides. Am J Publ Health. 1959;49:888–99. doi: 10.2105/ajph.49.7.888. [DOI] [PMC free article] [PubMed] [Google Scholar]


