Abstract
Purpose
The use of potentially inappropriate medications (PIMs) in older people is associated with increased risk of adverse drug events and hospitalization. This study aimed to determine the contribution of primary prescribers to variation in PIM use.
Methods
This was a retrospective cohort study using 2008 Medicare Part D event files and claims data for a 100% sample of Texas beneficiaries. PIM use was defined as receiving any of 48 medications on the Beers 2003 list of PIMs. Patient characteristics associated with PIM use were determined using a multivariable model. A multilevel model for the odds of PIM use was constructed to evaluate the amount of variation in PIM use at the level of primary care prescriber, controlling for patient characteristics.
Results
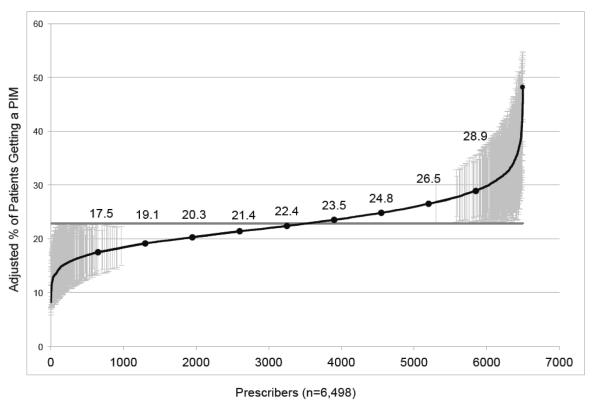
Of 677,580 patients receiving prescriptions through Part D in 2008, 31.9% received a PIM. Sex, ethnicity, low-income subsidy eligibility, and hospitalization in 2007 were associated with PIM use. The strongest associations with higher PIM use were increasing number of prescribers and increasing number of medications. The odds ratio for PIM use was 1.50 (95% CI 1.47-1.53) for ≥4 prescribers versus only 1 prescriber. In the multilevel model, the adjusted average percent of patients prescribed a PIM ranged from 17.5% for the lowest decile to 28.9% for the highest decile of prescribers.
Conclusions
PIM use was prevalent in Part D beneficiaries and varied among individual primary care prescribers. The association of PIM use with increasing numbers of prescribers suggests the need to reduce fragmentation of care to reduce inappropriate prescribing.
Keywords: inappropriate medication, Beers criteria, Medicare Part D, elderly, pharmacotherapy, polypharmacy
INTRODUCTION
Older persons are at high risk for polypharmacy, and particularly for the use of medications that are harmful. Numerous tools have been developed to identify and reduce the use of potentially inappropriate medications (PIMs) in older adults, including the Beers criteria,1,2 a list of medications and drug-disease combinations that should be avoided in older persons due to a high risk to benefit ratio. The use of PIMs in older adults has been linked to an increased risk of adverse drug reactions, falls, hospitalization, and mortality.3-5
The prevalence of PIM use in older outpatients in the United States ranges from 11.5% to 41.9%, with most studies finding rates between 20 and 25%.6 While there are individual situations in which a PIM is a reasonable choice to treat a patient’s condition, reducing rates of PIM use could be beneficial to patients.7 Improving medication appropriateness has been associated with a decreased risk of adverse drug reactions.8
Educational interventions, decision support systems, and academic detailing targeted at prescribers can decrease PIM use.9 However, there are few studies that have evaluated the role of the prescriber in PIM use. PIM use has been associated with health system factors, regional variation, and even prescriber characteristics.10-12 Primary care providers could potentially reduce PIM use through careful medication review and patient education, which is particularly important when patients see multiple providers.13,14 The purpose of our study was to determine the variation among primary care prescribers in the use of PIMs by Medicare Part D beneficiaries in the outpatient setting. We used Medicare Part D data linked with Medicare claims for Texas, allowing for adequate sample size of beneficiaries per prescriber to be able to examine prescriber level characteristics.
METHODS
Data Sources
We used Medicare claims and Medicare Part D event files for a 100% sample of Texas Medicare beneficiaries for 2007 and 2008. Medicare denominator files were used for demographic factors. Inpatient claims files (MEDPAR) were used to determine hospitalization. The Long Term Care Minimum Data Set was used to identify beneficiaries with a nursing home stay. Diagnosis codes from outpatient visits were obtained from the outpatient statistical analysis files for Part B claims and carrier files for physician claims. Part D event files contained information on prescriptions, including medication name, strength, date of prescription, and de-identified prescriber information. The Prescriber Characteristics File linked to Part D files by a prescriber identifier was used to determine different prescribers and their specialty and sub-specialty.
Study Subjects
We selected beneficiaries 66 years or older on January 1, 2008 (n=2,261,766). We included beneficiaries with 12 months of continuous Part A and B coverage and 12 months of continuous Part D enrollment without HMO enrollment for 2008 (n=760,703). We selected beneficiaries who received at least one prescription from a physician prescriber in 2008 (n=708,838). We further narrowed our study sample only to beneficiaries who received a prescription from a prescriber who wrote prescriptions for at least 10 beneficiaries in 2008 (n=677,580). Of 120,358 total prescribers, this step left 24,561 prescribers. We excluded prescribers who wrote few prescriptions, because we were primarily interested in primary care prescribers who saw adequate numbers of Medicare beneficiaries.
The University of Texas MD Anderson Institutional Review Board approved this study with a waiver of informed consent.
Outcome measures
We defined PIM use by beneficiaries as a beneficiary having received at least one prescription for a PIM in 2008. We used the Beers criteria 2003 list of inappropriate medications to define PIMs. We defined PIMs according to the list of 48 medications or medication classes considered inappropriate, and we did not include the list of 20 inappropriate drug/disease combinations.2
Patient characteristics included age, sex, race/ethnicity, eligibility for low-income subsidy, hospitalization in the year prior to PIM use (2007), nursing home stay in 2008, and comorbidity. We defined comorbidity according to those comorbidities that are included in Elixhauser’s index,15 using claims for the year prior to PIM use (2007). We determined the number of different medications in 2008 from Part D files. We determined the number of different physician prescribers using the unique prescriber identifier from Part D files.
Statistical methods
The primary outcome was whether a patient received a PIM. In univariate analysis, we determined patient characteristics associated with PIM use. We used Chi-square tests to compare the differences in proportion of PIM use across different patient characteristics. We constructed a multivariable logistic regression model including beneficiaries’ characteristics as predictors for the likelihood of receiving a PIM.
Next, we evaluated PIM use according to prescriber specialty. We constructed a cohort of pairs between beneficiaries and prescribers, based on a prescriber writing a prescription for a beneficiary (n=1,890,728). In this analysis, a beneficiary could have multiple prescribers. We then evaluated PIM use for beneficiaries based on prescriptions prescribed by each specialty.
Finally we assigned each patient to a predominant prescriber who wrote the most prescriptions for him/her. In the case of a tie on the number of prescriptions prescribed across multiple prescribers, the beneficiary was assigned to a predominant prescriber who wrote the latest prescription in 2008. In the multilevel analysis, we included only beneficiaries who had a predominant prescriber who was a primary care provider with the specialty of family medicine, general internal medicine, geriatrics, or general practice. Whether or not a patient received a PIM from their primary care prescriber was evaluated by a hierarchical generalized linear model (HGLM) adjusted for the clustering of beneficiaries within primary care prescribers. In the HGLM analysis, we adjusted for all significant beneficiary characteristics. We also estimated the adjusted rate of patients receiving a PIM for each primary care prescriber from the same model. We conducted a sensitivity analysis including beneficiaries with a predominant primary care provider who wrote prescriptions for at least 50 beneficiaries. We used SAS version 9.2 for all analyses (SAS Institute, Cary, NC).
RESULTS
Among 677,580 Texas Medicare beneficiaries age 66 and older who filled a prescription in 2008 through the Part D benefit, 216,364 (31.9%) were prescribed at least one potentially inappropriate medication (PIM) according to the Beers criteria 2003 list. Of all beneficiaries, 24.1% were prescribed one PIM, 6.3% were prescribed 2 different PIMs, and 1.6% were prescribed 3 or more different PIMs. The characteristics of the study population and percent receiving PIMs in each category are shown in Table 1. Higher PIM use was seen in women, in people hospitalized in 2007, in those with an increased number of comorbidities, and those with higher total number of medications. PIM use differed among different ethnic categories. Having increasing numbers of prescribers was also associated with higher PIM use. Table 1 also presents the results from the multivariable model for predictors of whether a beneficiary received a PIM. The multivariable model includes all beneficiaries in the study population and all prescribers. Sex, ethnicity, eligibility for low-income subsidy, and hospitalization in 2007 were significantly associated with increased odds of PIM use. Age was not associated with PIM use. The odds of receiving a PIM increased with increasing number of different prescribers. The strongest independent predictor of PIM use was increasing number of different medications.
Table 1.
Characteristics of 677,580 Texas Medicare Part D Beneficiaries and Adjusted Odds Ratios for PIM Use
| Characteristic | Category | Total Number |
% Getting a PIMa |
Adjusted Odds Ratio for PIM Use (95% CI)b |
|---|---|---|---|---|
| Age | 66-69 70-74 75-79 80-84 85+ |
157,530 171,984 142,225 107,999 97,842 |
29.6 30.9 32.7 33.8 34.4 |
Ref 1.00 (0.99-1.02) 1.00 (0.98-1.02) 0.99 (0.97-1.01) 0.98 (0.96-1.00) |
| Sex | Male Female |
235,923 441,657 |
26.2 35.0 |
Ref 1.33 (1.32-1.35) |
| Race/Ethnicity | White Black Hispanic Asian Other |
465,680 52,611 139,223 16,797 3,269 |
32.2 34.2 31.3 22.9 28.3 |
Ref 1.07 (1.05-1.10) 0.87 (0.86-0.89) 0.60 (0.58-0.63) 0.88 (0.81-0.95) |
| Eligible for Low- Income Subsidy in 2008 |
No Yes |
471,467 206,113 |
30.6 35.0 |
Ref 1.03 (1.02-1.05) |
| Number of Comorbiditiesc |
0 1 2+ |
61,477 110,815 505,288 |
20.0 23.8 35.2 |
Ref 0.99 (0.96-1.01) 0.89 (0.87-0.91) |
| Hospitalized at Least Once in 2007 |
No Yes |
533,839 143,741 |
29.4 41.5 |
Ref 1.10 (1.08-1.11) |
| Nursing Home Stay in 2008 |
No Yes |
608,205 69,375 |
30.7 43.2 |
Ref 0.93 (0.91-0.95) |
| Total Number of Different Medications in 2008 |
1-5 6-8 9-12 13+ |
209,281 158,718 154,913 154,668 |
11.4 25.7 39.3 58.8 |
Ref 2.48 (2.43-2.52) 4.37 (4.29-4.54) 9.11 (8.93-9.29) |
| Number of Different Prescribers in 2008 |
1 2 3 4+ |
182,884 178,487 130,779 185,430 |
19.2 26.6 34.1 48.1 |
Ref 1.18 (1.16-1.20) 1.29 (1.27-1.32) 1.50 (1.47-1.53) |
All proportions of PIM use by category were significantly different with P < 0.001.
Adjusted for all other variables in Table 1 (age, sex, race/ethnicity, eligibility for low income subsidy, number of comorbidities, hospitalization, nursing home stay, number of different medications, and number of different prescribers).
Number of comorbidities that are included in Elixhauser’s index .
Table 2 shows the results for PIM use by prescriber specialty, based on pairs between beneficiaries and prescribers who wrote prescriptions for a beneficiary. Among all 24,561 prescribers, 84.9% prescribed at least one PIM. The beneficiaries with PIM prescriptions written by prescribers varied by specialty, with low rates for subspecialties like ophthalmology and otolaryngology, and higher rates for primary care specialties, surgery, and pain medicine specialists.
Table 2.
Percent of PIM Use among Beneficiaries with Prescriptions Prescribed by Physician Specialty
| Physician Specialty | Number of Beneficiaries Getting Prescriptions from Each Specialty |
Percent Getting a PIM |
|---|---|---|
| Anesthesiology | 7528 | 20.3 |
| Emergency Medicine | 70,906 | 17.5 |
| Family Medicine | 438,185 | 19.3 |
| General Internal Medicine | 355,262 | 19.0 |
| General Practice | 20,730 | 19.7 |
| Geriatrics | 30,767 | 18.7 |
| Gynecology | 27,021 | 11.4 |
| Hospitalist | 1816 | 8.0 |
| Internal Medicine Subspecialties | 364,597 | 8.0 |
| Ophthalmology | 93,036 | 1.4 |
| Otolaryngology | 23,809 | 3.3 |
| Pain Medicine | 5375 | 18.9 |
| Psychiatry and Neurology | 49,743 | 7.1 |
| Surgery | 129,403 | 21.5 |
| All other | 272,550 | 13.0 |
Table 3 shows the most commonly prescribed PIMs according to the number of beneficiaries receiving at least one prescription for the PIM. Propoxyphene, taken off the market in 2010, was the PIM prescribed to the highest number of beneficiaries. The other most commonly prescribed categories among PIMs were tricyclic antidepressants, antihypertensives, and antispasmodics.
Table 3.
The 10 Most Frequently Prescribed PIMs According to Number of Beneficiaries Receiving the PIM
| Medication Name | Number of Beneficiaries Taking PIM |
|---|---|
| Propoxyphene | 83,415 |
| Nitrofurantoin | 37,908 |
| Clonidine | 28,496 |
| Cyclobenzaprine | 27,893 |
| Amitriptyline | 19,390 |
| Doxazosin | 11,941 |
| Amiodarone | 10,906 |
| Dicyclomine | 9753 |
| Carisoprodol | 8475 |
| Methocarbamol | 7958 |
The multilevel analysis included 6,498 primary care providers who were assigned as predominant prescribers to a total of 469,505 patients. Of these patients, 25.5% were prescribed at least one PIM. From the HGLM analysis, the adjusted average percent of patients who received a PIM among all patients assigned to a predominant primary care prescriber was 22.9%, ranging from 17.5% for the lowest 10th percentile to 28.9% for the 90th percentile among primary care prescribers. The prescriber level accounted for 4% of the variation in PIM use among patients. Figure 1 shows the distribution of adjusted percent of PIM use among primary care prescribers. These are cumulative distributions among primary care prescribers, showing the mean value of percent of PIM use among patients assigned to that prescriber, derived from the two-level HGLM model. Red vertical lines indicate primary care prescribers whose patients have a significantly different percent of PIM use from the mean. Compared to all 6,498 primary care prescribers, patients of 391 primary care prescribers (6.0%) had significantly higher PIM use, while the patients of 299 primary care prescribers (4.6%) had significantly lower PIM use.
Figure 1.
Difference among primary care prescribers in adjusted percent of patients getting a PIM, by rank from lowest to highest. These rates were estimated by HGLM, adjusted for patient characteristics. The horizontal line at 22.9% represents the overall mean adjusted percent of patients getting a PIM. The curved line represents the estimated percent of PIM use for individual primary care prescribers. Error bars represent 95% confidence intervals for the primary care prescribers who have significantly higher or lower estimates from the mean. Circles on the curved line and numbers listed above show the values for the adjusted percent of patients getting a PIM for each 10th percentile of prescriber. Primary care prescribers included family medicine, general internal medicine, geriatrics, and general practice. Patients were assigned to a predominant prescriber who wrote the most prescriptions for him/her. In the case of a tie on the number of prescriptions prescribed across multiple prescribers, the patient was assigned to a predominant prescriber who wrote the latest prescription in 2008.
In a sensitivity analysis, we conducted the multilevel HGLM analysis using primary care prescribers who wrote prescriptions for at least 50 beneficiaries. This analysis included 386,839 patients and 3259 primary care prescribers. The adjusted mean percent of patients who received a PIM was 23.8%, ranging from 17.2% for the 10th percentile to 30.7% for the 90th percentile; 10.0% of prescribers were significantly below the mean adjusted percent of PIMs, and 9.6% of prescribers were significantly above the mean. The odds ratios for patient-level predictors of PIM use were similar in this population compared to the results obtained for the 469,505 patients and 6498 prescribers included in the original analysis.
DISCUSSION
We found a high prevalence of PIM use among fee-for-service Medicare beneficiaries who received prescriptions through the Medicare Part D program in Texas in 2008. Increased numbers of prescribers and higher number of medications were independently and strongly associated with increased odds of PIM use. PIM prescribing varied by prescriber specialty and among individual primary care prescribers.
The relatively high prevalence of PIM use in our study is partly due to our sample selection. We evaluated PIM use among Medicare beneficiaries who actually received a prescription, rather than among all Medicare beneficiaries. The number of Texas Medicare beneficiaries in 2008 who had Parts A, B, and D enrollment without HMO enrollment was 765,398, giving a rate of PIM use of 28.3% among those eligible to receive prescriptions in the Part D plan. Among Medicare beneficiaries in the Medical Expenditures Panel Survey in 2006, an adjusted 16% received a PIM.16 However, only 45% of the sample study was enrolled in Part D.
The high prevalence of PIM use could also be due to real differences in prescribing quality across different regions of the United States. In a study by Zhang, et al, of a 5% national sample of Medicare Part D beneficiaries, PIM rates varied substantially by geographic region.17 The overall mean prevalence of high risk medication use according to measures from the Healthcare Effectiveness Data and Information Set in 2007 was 25.8%, with rates as high as 44%. The highest rates were seen in the southern United States, including Texas. Another study in the Veteran’s Administration system found that average PIM use ranged from 13.3 to 18.9%, and was 54% higher in the South relative to the Northeast, adjusted for age and sex.18
Another reason for the high PIM rate in our study could be that we included beneficiaries residing in nursing homes. A high proportion of persons residing in long-term care are enrolled in Part D,19 and long-term care patients may have higher rates of medication and PIM use.20 Variation in PIM use across nursing homes has also been described,21 although a study of PIM use in Scotland showed no difference in rates between patients residing at home or in nursing homes.22
Increasing numbers of different prescribers strongly predicted PIM use, suggesting a lack of continuity of care and increased fragmentation in care.23 Higher continuity of care was associated with a 56% lower odds use of PIM use in elderly outpatients in Taiwan, although provider specialty was not included in their analysis.24 In a study of PIM use among hospitalized elderly patients, prescriber specialty was a significant factor increasing the likelihood of PIMs, with cardiologists having higher PIM rates.12 The fact that increasing medication number was the strongest predictor of PIM use suggests the importance of the primary care provider in reconciling all medications and reducing medication-related problems.
A strength of this study is the use of Texas Medicare Part D data, allowing for adequate sample size to include the prescriber level in our analysis. However, this limits generalizability to the Part D population and to the Medicare population as a whole. We evaluated only the primary care prescribers in our multilevel analysis, based on assumptions that primary care providers would have the most ability to detect and reduce PIM use. This may have resulted in attributing PIM us by patients to prescribers who were unaware of their patient’s PIM use. Another limitation is the fact that we could not link prescriber characteristics files with other files, such as Medicare A and B and American Medical Association provider files. We thus could not determine whether additional prescriber characteristics like academic affiliation or patient volume were related to PIM use. This limitation also prevented us from further comparing the 6% of primary care prescribers whose patients had the highest PIM use and the 4.6% of primary care prescribers whose patients had the lowest PIM use with other prescribers. Because we were unable to determine the true indication for each medication, we were unable to evaluate whether medications on the Beers list may have been prescribed for appropriate reasons. Since Medicare Part D does not cover over-the-counter medications, we were unable to include PIMs sold without a prescription.
Our results suggest that PIM use is high in the Part D population. Given the recent release of updated Beers criteria for inappropriate prescribing,7 the policy implications of our study are that the Part D program may benefit from regular medication therapy management targeted specifically at PIM use. Further study is needed to determine whether PIM use is associated with increased healthcare utilization or negative outcomes such as adverse drug reactions.
Increasing medication use and increasing numbers of prescribers are strongly associated with increased use of PIMs in Medicare Part D beneficiaries. We found a high prevalence of PIM use, with variation among primary care prescribers. Interventions could be directed to reduce variation in care and to reduce the overall level of PIM use in Part D beneficiaries.
Key Points.
Inappropriate medication use continues to be a common problem in older persons.
Multiple patient-level factors are associated with inappropriate medication use, including having higher numbers of different prescribers.
While PIM use by patients varied among physicians, this study suggests the need to improve fragmentation of care to improve PIM use.
Acknowledgments
Sponsor: Dr. Holmes is supported by K23AG038476 from the National Institute on Aging. Dr. Goodwin is supported by K05CA134923 from the National Cancer Institute. The sponsor had no role in any elements of this study.
Footnotes
Conflict of Interest: All authors report no conflicts of interest in relation to the work presented in this manuscript.
Prior Presentation: The research in this manuscript was presented in part at the CMS Symposium in Hunt Valley Maryland in March 2012.
References
- 1.Beers MH, Ouslander JG, Rollingher I, Reuben DB, Brooks J, Beck JC. Explicit criteria for determining inappropriate medication use in nursing home residents. Arch Intern Med. 1991;151:1825–1832. [PubMed] [Google Scholar]
- 2.Fick DM, Cooper JW, Wade WE, Waller JL, Maclean JR, Beers MH. Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts. Arch Intern Med. 2003;163:2716–2724. doi: 10.1001/archinte.163.22.2716. [DOI] [PubMed] [Google Scholar]
- 3.Aparasu RR, Mort JR. Inappropriate prescribing for the elderly: Beers criteria-based review. Ann Pharmacother. 2000;34:338–346. doi: 10.1345/aph.19006. [DOI] [PubMed] [Google Scholar]
- 4.Dedhiya SD, Hancock E, Craig BA, Doebbeling CC, Thomas J., 3rd Incident use and outcomes associated with potentially inappropriate medication use in older adults. Am J Geriatr Pharmacother. 2010;8:562–570. doi: 10.1016/S1543-5946(10)80005-4. 10.1016/s1543-5946(10)80005-4. [DOI] [PubMed] [Google Scholar]
- 5.Akazawa M, Imai H, Igarashi A, Tsutani K. Potentially inappropriate medication use in elderly Japanese patients. Am J Geriatr Pharmacother. 2010;8:146–160. doi: 10.1016/j.amjopharm.2010.03.005. 10.1016/j.amjopharm.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 6.Guaraldo L, Cano FG, Damasceno GS, Rozenfeld S. Inappropriate medication use among the elderly: a systematic review of administrative databases. BMC Geriatr. 2011;11:79. doi: 10.1186/1471-2318-11-79. 10.1186/1471-2318-11-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2012;60:616–631. doi: 10.1111/j.1532-5415.2012.03923.x. 10.1111/j.1532- 5415.2012.03923.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patterson SM, Hughes C, Kerse N, Cardwell CR, Bradley MC. Interventions to improve the appropriate use of polypharmacy for older people. Cochrane Database Syst Rev. 2012;5:CD008165. doi: 10.1002/14651858.CD008165.pub2. 10.1002/14651858.CD008165.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Topinkova E, Baeyens JP, Michel JP, Lang PO. Evidence-based strategies for the optimization of pharmacotherapy in older people. Drugs Aging. 2012;29:477–494. doi: 10.2165/11632400-000000000-00000. 10.2165/11632400-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 10.Gellad WF, Good CB, Amuan ME, Marcum ZA, Hanlon JT, Pugh MJ. Facility-level variation in potentially inappropriate prescribing for older veterans. J Am Geriatr Soc. 2012;60:1222–1229. doi: 10.1111/j.1532-5415.2012.04042.x. 10.1111/j.1532-5415.2012.04042.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pugh MJ, Rosen AK, Montez-Rath M, et al. Potentially inappropriate prescribing for the elderly: effects of geriatric care at the patient and health care system level. Med Care. 2008;46:167–173. doi: 10.1097/MLR.0b013e318158aec2. 10.1097/MLR.0b013e318158aec2. [DOI] [PubMed] [Google Scholar]
- 12.Rothberg MB, Pekow PS, Liu F, et al. Potentially inappropriate medication use in hospitalized elders. J Hosp Med. 2008;3:91–102. doi: 10.1002/jhm.290. [DOI] [PubMed] [Google Scholar]
- 13.Tulner LR, Kuper IM, Frankfort SV, et al. Discrepancies in reported drug use in geriatric outpatients: relevance to adverse events and drug-drug interactions. Am J Geriatr Pharmacother. 2009;7:93–104. doi: 10.1016/j.amjopharm.2009.04.006. 10.1016/j.amjopharm.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 14.Garcia RM. Five ways you can reduce inappropriate prescribing in the elderly: a systematic review. J Fam Prac. 2006;55:305–312. [PubMed] [Google Scholar]
- 15.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Fu AZ, Tang AS, Wang N, Du DT, Jiang JZ. Effect of Medicare Part D on potentially inappropriate medication use by older adults. J Am Geriatr Soc. 2010;58:944–949. doi: 10.1111/j.1532-5415.2010.02809.x. 10.1111/j.1532-5415.2010.02809.x. [DOI] [PubMed] [Google Scholar]
- 17.Zhang Y, Baicker K, Newhouse JP. Geographic variation in the quality of prescribing. The New England journal of medicine. 2010;363:1985–1988. doi: 10.1056/NEJMp1010220. 10.1056/NEJMp1010220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lund BC, Charlton ME, Steinman MA, Kaboli PJ. Regional differences in prescribing quality among elder veterans and the impact of rural residence. J Rural Health. 2012 doi: 10.1111/j.1748-0361.2012.00428.x. 10.1111/j.1748-0361.2012.00428.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaiser Family Foundation [Accessed August, 2012];Medicare prescription drug coverage for residents of nursing homes and assisted living facilities: special problems and concerns. http://www.kff.org.
- 20.Forsetlund L, Eike MC, Gjerberg E, Vist GE. Effect of interventions to reduce potentially inappropriate use of drugs in nursing homes: a systematic review of randomised controlled trials. BMC Geriatr. 2011;11:16. doi: 10.1186/1471-2318-11-16. 10.1186/1471-2318-11-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bronskill SE, Gill SS, Paterson JM, Bell CM, Anderson GM, Rochon PA. Exploring variation in rates of polypharmacy across long term care homes. J Am Med Dir Assoc. 2012;13:309, e315–321. doi: 10.1016/j.jamda.2011.07.001. 10.1016/j.jamda.2011.07.001. [DOI] [PubMed] [Google Scholar]
- 22.Barnett K, McCowan C, Evans JM, Gillespie ND, Davey PG, Fahey T. Prevalence and outcomes of use of potentially inappropriate medicines in older people: cohort study stratified by residence in nursing home or in the community. BMJ Qual Saf. 2011;20:275–281. doi: 10.1136/bmjqs.2009.039818. 10.1136/bmjqs.2009.039818. [DOI] [PubMed] [Google Scholar]
- 23.Liu CW, Einstadter D, Cebul RD. Care fragmentation and emergency department use among complex patients with diabetes. Am J Managed Care. 2010;16:413–420. [PubMed] [Google Scholar]
- 24.Chu HY, Chen CC, Cheng SH. Continuity of care, potentially inappropriate medication, and health care outcomes among the elderly: evidence from a longitudinal analysis in taiwan. Med Care. 2012;50:1002–1009. doi: 10.1097/MLR.0b013e31826c870f. 10.1097/MLR.0b013e31826c870f. [DOI] [PubMed] [Google Scholar]