Abstract
Arteriovenous malformations are a rare but important cause of abnormal uterine bleeding in the midlife. Acquired uterine arteriovenous malformations are being increasingly diagnosed by transvaginal ultrasound, color Doppler and magnetic resonance angiography. We present a case where the suspected diagnosis was placental polyp or retained products of conception and hysteroscopy showed typical findings of uterine arteriovenous malformation, which was later, confirmed by magnetic resonance angiography. The patient underwent arterial embolization and recovered satisfactorily with resolution of hemorrhage and resumption of normal menstrual cycles. Abnormal bleeding due to arteriovenous malformations is worsened by curettage and hence its recognition is important in the management of abnormal uterine bleeding in the midlife.
Keywords: Abnormal uterine bleeding, arteriovenous malformation, embolization, hysteroscopy
INTRODUCTION
Arteriovenous malformations are increasingly recognized as a cause of heavy uterine bleeding. These are worsened by curettage and so a high index of suspicion is necessary for diagnosis. Transvaginal ultrasound may point towards diagnosis but the findings are not specific. Hysteroscopy is increasingly being used for diagnosis and management of abnormal uterine bleeding. Only two cases of hysteroscopic findings in arteriovenous malformations have been reported in literature so far. We present a case of acquired uterine arteriovenous malformation, which showed a characteristic pulsatile vascular mass on hysteroscopy.
CASE REPORT
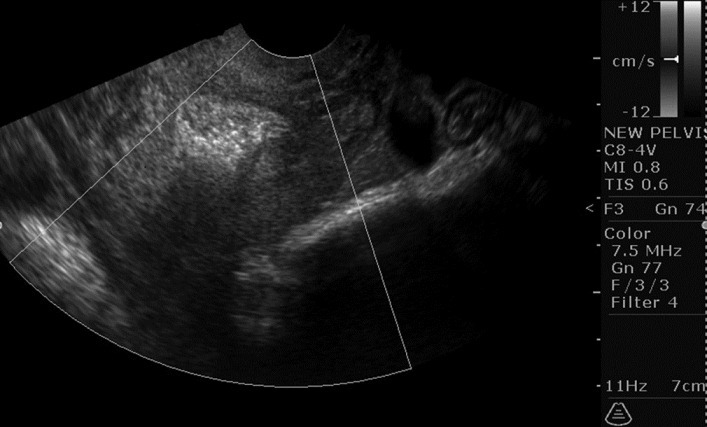
A 36-year-old lady, P2L2 (Para 2, living 2) underwent medical termination of pregnancy one month ago outside for failure of contraception. This was followed by laparoscopic tubal ligation in the same sitting. Subsequently she had profuse bleeding requiring blood transfusion after 15 days. She was admitted at our hospital with heavy bleeding. On admission, she was pale, pulse was 110/min, B.P. was 100/70 mm Hg and vaginal examination revealed a bulky soft uterus with open os and clots in the vagina. A transvaginal ultrasound showed parenchymal inhomogeneity in the uterus in the anterior wall with several interspersed sonolucent spaces of varying size [Figure 1]. The vascularity of uterus was increased on color Doppler [Figure 2]. Her CBC showed a Hb of 7 gm%, serum beta HCG was 50 IU/ml. A provisional diagnosis of uterine arteriovenous malformation or organized retained products of conception was made and hysteroscopy proceed was planned.
Figure 1.
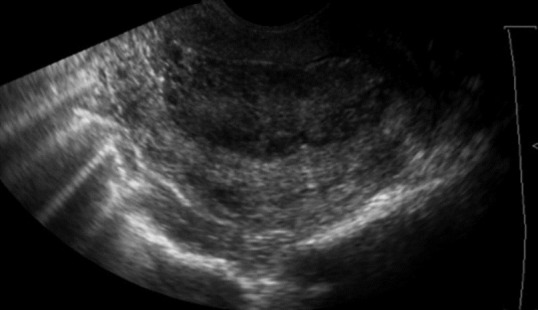
Transvaginal ultrasound showing parenchymal inhomogeneity in the uterus in the anterior wall with several interspersed sonolucent spaces of varying size
Figure 2.
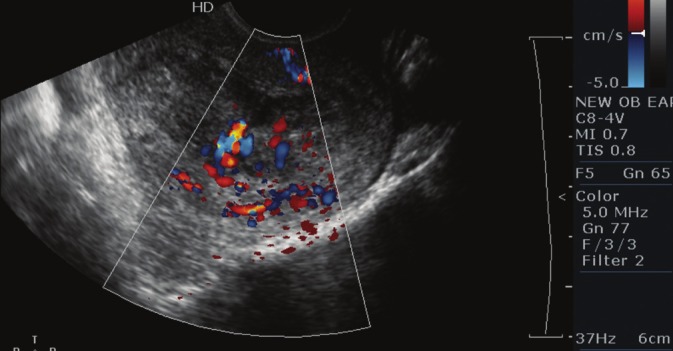
Transvaginal ultrasound color Doppler showing increased vascularity
Hysteroscopy revealed a clot in the uterine cavity. There was a pulsatile bluish vascular mass in the fundus extending to anterior wall of uterus. A diagnosis of acquired arteriovenous malformation was made [Figure 3]. MR angiography confirmed an arteriovenous malformation at the fundus and anterior wall of uterus being fed by mainly by left uterine artery [Figure 4]. Patient was taken for percutaneous arterial embolization and bilateral uterine artery embolization was done with polyvinyl alcohol particles. Patient had cessation of bleeding after the embolization and she resumed menstrual cycle 5 weeks after the procedure with scanty menstrual flow. Transvaginal scan revealed reduced vascularity with embolic particles seen in uterine myometrium [Figure 5].
Figure 3.
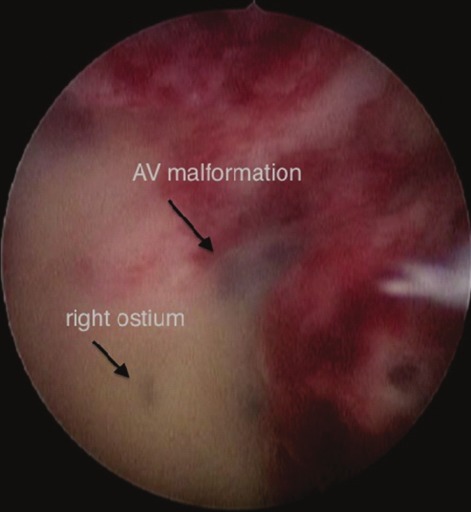
Hysteroscopy showing bluish vascular mass in anterior and right lateral wall of uterus
Figure 4.
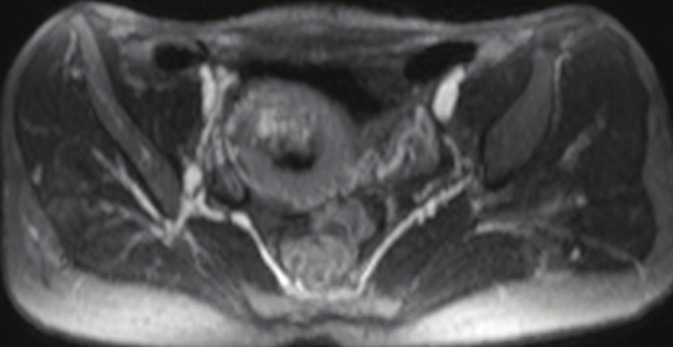
MR angiography showing arteriovenous malformation at the fundus and anterior wall of uterus being fed by mainly by left uterine artery
Figure 5.
Transvaginal scan revealed reduced vascularity with embolic particles seen in uterine myometrium
Six months later, patient continues to have cyclic menstrual bleeding with moderate flow.
DISCUSSION
Acquired arteriovenous malformations are known to occur after uterine curettage, medical abortion, gestational trophoblastic disease, cesarean section and endometrial carcinoma.[1] They usually present with torrential bleeding requiring blood transfusion and this bleeding is worsened by uterine curettage. The differential diagnosis is retained products of conception, polyps, adenomyosis, endometrial carcinoma and gestational trophoblastic disease.[2] Abnormal uterine bleeding is an important cause of morbidity in the midlife and uterine arteriovenous malformations are a rare albeit important cause of such bleeding.
Transvaginal sonography with color Doppler may point to the diagnosis but the condition may be confused with retained products of conception.[3] In our case, the serum beta HCG was 50 IU/ml, which was suggestive of retained products of conception or placental polyp. Hysteroscopic picture of arteriovenous malformation has been described in literature as a pulsatile vascular mass in the uterine cavity.[4,5] In this case there was a clot in the uterine cavity and typical vascular mass, which showed pulsations on reducing the intrauterine pressure. Recognition of this rare hysteroscopic picture is important, as arteriovenous malformations are being increasingly diagnosed and treated. Hysteroscopy if often the investigation of choice for abnormal uterine bleeding and arteriovenous malformations are a rare but potentially treatable cause of abnormal uterine bleeding. Transcatheter embolization of feeding vessels is an established treatment of arteriovenous malformations other being hysterectomy.[6,7] There are reports of failed angiographic embolization in which definitive treatment i.e., hysterectomy was offered.[4,8] Treatment with GnRH analogues, methylergonovine maleate etc., have also been described.[9,10] Acquired arteriovenous malformations arise mostly after pregnancy or pregnancy related complications and they may coexist with conditions like retained placental tissue, retained products of conception and gestational trophoblastic disease.[11] While the treatment of retained products of conception is curettage, in arteriovenous malformations it can lead to torrential hemorrhage. Hysteroscopy has an important potential role in the diagnosis of arteriovenous malformation in selected patients.[2,4,5] Recognition of typical hysteroscopic picture can aid in diagnosis and the coexisting confounding problems like polyps, retained products of conception can also be tackled at the same sitting. However, sometimes even putting in a small hysteroscope can cause torrential hemorrhage in cases with A_V malformations and this should be kept in mind while tacking a suspected case. Transcatheter embolization of feeding vessels is a minimally invasive treatment for such lesions and affords an opportunity to manage these cases and salvage the uterus as well.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Burrows PE. Vascular malformations involving the female pelvis. Semin Intervent Radiol. 2008;25:347–60. doi: 10.1055/s-0028-1102993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Timmerman D, Van den Bosch T, Peeraer K, Debrouwere E, Van Schoubroeck D, Stockx L, et al. Vascular malformations in the uterus: Ultrasonographic diagnosis and conservative management. Eur J Obstet Gynecol Reprod Biol. 2000;92:171–8. doi: 10.1016/s0301-2115(00)00443-7. [DOI] [PubMed] [Google Scholar]
- 3.Kido A, Togashi K, Koyama T, Ito H, Tatsumi K, Fujii S, et al. Retained products of conception masquerading as acquired arteriovenous malformation. J Comput Assist Tomogr. 2003;27:88–92. doi: 10.1097/00004728-200301000-00016. [DOI] [PubMed] [Google Scholar]
- 4.Taylor E, Hitkari J. Hysteroscopic identification of a uterine arteriovenous malformation. J Obstet Gynaecol Can. 2009;31:1117–8. doi: 10.1016/s1701-2163(16)34367-5. [DOI] [PubMed] [Google Scholar]
- 5.Manolitsas T, Hurley V, Gilford E. Uterine arteriovenous malformation-a rare cause of uterine haemorrhage. Aust N Z J Obstet Gynaecol. 1994;34:197–9. doi: 10.1111/j.1479-828x.1994.tb02691.x. [DOI] [PubMed] [Google Scholar]
- 6.Halperin R, Schneider D, Maymon R, Peer A, Pansky M, Herman A. Arteriovenous malformation after uterine curettage: A report of 3 cases. J Reprod Med. 2007;52:445–9. [PubMed] [Google Scholar]
- 7.Lin A-C, Hung Y-C, Huang L-C, Chiu T-H, Ho M. Successful treatment of uterine arteriovenous malformation with percutaneous embolization. Taiwan J Obstet Gynecol. 2007;46:60–3. doi: 10.1016/S1028-4559(08)60109-6. [DOI] [PubMed] [Google Scholar]
- 8.Bagga R, Verma P, Aggarwal N, Suri V, Bapuraj JR, Kalra N. Failed angiographic embolization in uterine arteriovenous malformation: A case report and review of the literature. Medscape J Med. 2008;10:12. [PMC free article] [PubMed] [Google Scholar]
- 9.Nonaka T, Yahata T, Kashima K, Tanaka K. Resolution of uterine arteriovenous malformation and successful pregnancy after treatment with a gonadotropin-releasing hormone agonist. Obstet Gynecol. 2011;117:452–5. doi: 10.1097/AOG.0b013e3181f7381f. [DOI] [PubMed] [Google Scholar]
- 10.Flynn MK, Levine D. The noninvasive diagnosis and management of a uterine arteriovenous malformation. Obstet Gynecol. 1996;88:650–2. doi: 10.1016/0029-7844(96)00122-6. [DOI] [PubMed] [Google Scholar]
- 11.Kratz KG, Green IC. Coincident acquired ateriovenous malformation and retained products of conception following surgical termination of pregnancy. J Minim Invasive Gynecol. 2011;18:S155. [Google Scholar]


