Abstract
Background:
Early diagnosis of tuberculosis (TB) is a major key for effective TB program. Evaluation of delay in diagnosis of smear positive TB is needed to evaluation of TB program situation in each country. The aim of this study was to evaluate of diagnosis delay in smear positive tuberculosis patients in Islamic Republic of Iran.
Materials And Methods:
In this cross sectional study, all smear positive TB registered patients from 20 March 2009 to 20 March 2010 in Iran were assessed. Diagnosis delay is defined as the time interval between the first presentations of TB symptoms to the TB confirmation. Mann-Whitney test, chi-square and logistic regression was used to analysis.
Results:
Diagnosis delay was 58 days in female and 53 days in male (P=0.004), 61 days in non-Iranian and 54 days in Iranian (P<0.001), 59 days in urban and 50 days in rural (P<0.001), 57 days in non-prisoner and 37 days in prisoner (P<0.001), 61 days in patients who chose private outpatients system and 52 days in patients who chose Public health outpatients system (P<0.001). 193 (9.4%) had 1-9 bacilli and 2132 (37.4%) were 3+ in sputum smear examination.
Conclusion:
Non-Iranian, urban, non-prisoner, old patients and the patients who chose private system are in risk of delay diagnosis of TB. Cooperation of private system through public-private mix model is an important key in successful national TB program (NTP).
Keywords: Diagnosis delay, public private mix, tuberculosis
INTRODUCTION
Tuberculosis (TB) kills about two million people annually.[1,2,3] 84% case detection, 87% treatment success rate and reversing TB incidence rate by 2015 are the main goals of World health organization (WHO) and stop TB partnership to control TB.[4,5] TB is one of important infectious diseases in Iran. Immigration from Afghanistan and pilgrims from Pakistan and Iraq are intensifying the problem.
Delay in diagnosis of TB is a major defect in TB program and it can lead to several complications, mortality, and TB contamination in the community.[6,7,8] It may be related to patient (patient delay) or the health system (system delay).[7] Hence, the TB patients are evaluated and reported by some health care sources, identifying the diagnosis delay in these sources is important to planning effective national TB program (NTP). Also, some variable such as age, sex, residency, nationality and HIV may be related to the diagnosis delay.
Evaluation of determinants of delay must be studied and addressed to improve the effectiveness of the NTPs.[7] Also, conducting this study is important for planning Public-Private Mix (PPM) program. This program advised by WHO to improve the collaboration of public and private sectors in the NTP.[9,10]
The aim of this study was evaluation of diagnosis delay in smear positive tuberculosis patients in Islamic Republic of Iran 2009-2010
MATERIALS AND METHODS
In this cross sectional study, all smear positive TB registered patients from 20 march 2009 to 20 march 2010 (one Hijri year) in Iran were assessed. Smear positive TB cases were defined according to WHO and Iran's national TB guideline.[11]
Diagnosis delay (both delays caused by patient and physician) is defined as the time interval between the first presentations of TB symptoms such as cough>2-3 weeks, fever, loss weight, sputum, night sweating to the diagnosis of TB.[11]
The patients were reported from public health outpatient system (PHO), public hospitals (PHs), private outpatient system (PO), private hospitals (PH), social security fund (hospitals or clinics that are belong to social security fund organizations) and other sources (charity and army forced clinic or hospitals).
Sputum smear positivity grade by direct microscopic examination were graded as 1-9 bacilli, 1+, 2+ and 3+.[11]
TB patients data were entered in TB register software via double-entry. After a review, the final data were prepared for analysis using SPSS16 software. Quantitative data were evaluated using Kolmogorow-Smironov statistical test and also via graphical test to assure their normal distribution. Mann-Whitney test were utilized to compare median diagnosis delay between dichotomous variables. Relationship between diagnostic delay group (>median and <=median) and dichotomous variables was evaluated by Chi-square test and odds ratio (95% confidence intervals) was calculated. The significant level of 0.05 was used as a statistical significant value. Logistic regression analysis was used to examine the adjusted odds ratio by SPSS software 16 (Chicago, USA).
RESULTS
The mean age of 5702 TB patients was 47.8 (SD: ±21.6) years. 2855 (50.1%) were female, 852 (14.9%) were Non-Iranian, 183 (3.2%) were prisoner, and 107 (1.9%) were HIV positive.
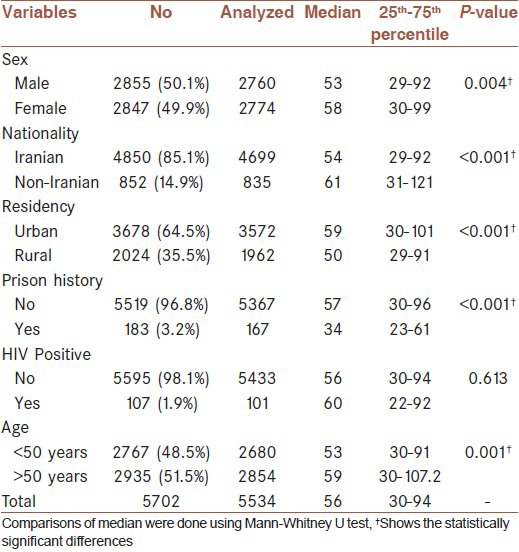
The median of diagnosis delay in all patients was 59 days. Diagnosis delay was longer in female than male (P=0.004), non-Iranian than Iranian (P<0.001), urban than rural (P<0.001), non-prisoner than prisoner (P<0.001) [Table 1]. Significant correlation was seen between age and diagnosis delay (rs=0.05; P<0.001).
Table 1.
Comparison of median diagnosis delay according to some variables
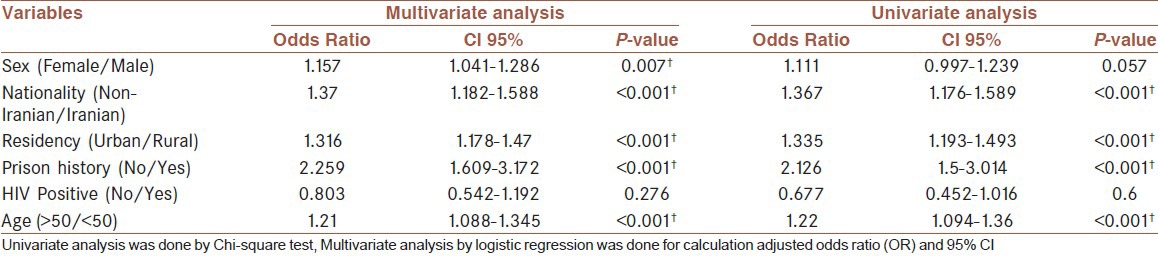
In multivariate analysis, Non-Iranian, urban, Non- prisoner and patients older than 50 years had chance 1.367, 1.335, 2.126 and 1.22 times more likely that their delay in TB diagnosis be longer than>59 days, respectively [Table 2].
Table 2.
Relation of different variables with diagnosis delay (cut-off point, median = 59 days)
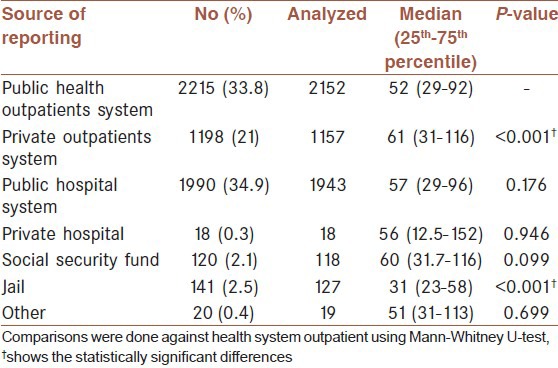
Median diagnosis delay in patients who chose the PO system (private clinics) to be visited were higher than PHO (P<0.001). Prisoners had less diagnosis delay than PHO (P<0.001) [Table 3].
Table 3.
Comparison of median diagnosis delay (day) in registered tuberculosis patients from different source of reporting
One hundred ninety three (3.4%) were 1-9 bacilli, 2053 (36%) were 1+, 1324 (23.2%) were 2+ and 2132 (37.4%) were 3+ in sputum smear examination.
DISCUSSION
Total delay in diagnosis of TB was about 2 months. Prisons had minimum delay in diagnosis of smear positive patients. Diagnosis delay was longer in Non-Iranian, urban, non- prisoner and older than 50 years patients. PO system had higher diagnosis delay than PHO. 37.4% were diagnosed as 3+ in sputum smear examination.
In Nasehi et al. study in Iran,[8] 2003 the median of diagnosis delay was reported as 89 days which is fortunately reduced now. A reduction of one month in diagnosis delay is considered as a great success in Iran NTP. However, diagnosis delay in our country is higher than other countries. Smear positivity grade shows 37.4% of the patients diagnosed in advanced stage of TB. In other studies, the median of diagnosis delay was about 50 days in Vietnam,[12] 56 days in Ghana,[13] and 6 days in New York. [14] Generally, the median of delay in diagnosis of smear positive patients varies from 2 days to 4 months in different countries.[6,7,15,16]
The PO services had more delay in diagnosing smear positive cases compared with PHS. Total delay in diagnosis in public sector and private sector are respectively 47.6 and 60.3 days in Egypt, 99.02 and 110.8 days in Pakistan, 79.7 and 84.1 days in Somali, 67 and 86 days in Syria, and 5.05 and 63.1 days in Yemen; in all countries except Somalia and Syria, delay in private sector is significantly higher than public sector[7] which is the same as our study. Participation of private sector in TB program could lead to improved diagnosis and treatment. Furthermore, contribution of private sector is needed to achieve specified targets.[17] It is suggested to implement TB control and reporting system in private sectors in Iran and design and perform a Public-Private Mix program.
The minimum delay was seen in prisons; it is a sign of early TB case finding in Iran prisons. However, it is still higher than some countries.[18]
Median diagnosis of TB in HIV positive did not have different with HIV negative in our study. However, we expected the HIV positives were diagnosed in early stage of TB because of active follow-up of these patients. In Diez et al. study[18] HIV positive diagnosed faster than HIV negative patients. However, diagnosis of TB in HIV patients is difficult but it is likely that TB diagnosis in HIV patients not appropriate in Iran.
Risk factors for diagnosis delay were similar in different area of the world. Characteristics such as lack of specific symptoms (hemoptesia), unemployed, smokers, females, older age, attending private sector as first provider attended, not prescription of CXR, living in Suburban or rural area and low literacy were related with more diagnosis delay.[7,8,19,20,21,22] Some of these factors related to presence of co-morbidity, health seeking behaviors, society culture and health care providers practice and attitude. Family physician system has been implemented in rural area in Iran and it may lead to decrease TB diagnosis delay in rural area. Also, according to the results, it is likely that private care system not familiar with NTP or complicated patients are referred to private system. Therefore, education and cooperation of private system through public-private mix model is an important key in successful NTP.
However, our study had some limitation. First, we just considered the characteristics that recorded in TB register software so we could not evaluate some related characteristics. Second, there may have been some recall bias from patients regarding the onset of symptoms.
CONCLUSION
Non-Iranian, urban, non-prisoner and old patients are in risk of diagnosis delay of TB. Cooperation of private system through public-private mix model is an important key in successful NTP.
ACKNOWLEDGMENTS
We thank all TB coordinators and staffs of NTP. The present article was extracted from the thesis written by Ebrahim Ghaderi and was financially supported by shiraz university of medical sciences grant No 885and WHO grant (APW 2011/128782; title: To develop a plan for the national PPM implementation). We thank stuff of WHO office in Iran and Shiraz University of Medical Sciences for financial support of this study. The authors would like to thank Shahnaz Ahmadi stuff of Iran NTP for editing the data.
Footnotes
Source of Support: This study is funded by Shiraz University of Medical Sciences and World health organization.
Conflict of Interest: None declared.
REFERENCES
- 1.Organization WH. Geneva: World Health Organization; 2010. Global Tuberculosis Control: WHO Report2010. [Google Scholar]
- 2.Kochi A. The global tuberculosis situation and the new control strategy of the World Health Organization. Tubercle. 1991;72:1–6. doi: 10.1016/0041-3879(91)90017-m. [DOI] [PubMed] [Google Scholar]
- 3.Raviglione MC, Snider DE, Jr, Kochi A. Global epidemiology of tuberculosis. Morbidity and mortality of a worldwide epidemic. JAMA. 1995;273:220–6. [PubMed] [Google Scholar]
- 4.Organization WH. Geneva: STOPTB department WHO; 2007. WHO report 2007, Global tuberculosis Control, Surveillance, Planning and Financing. [Google Scholar]
- 5.Geneva: World Health Organization; 2010. The global plan to stop TB 2011-2015: Transforming the fight towards elimination of tuberculosis. [Google Scholar]
- 6.Sreeramareddy CT, Panduru KV, Menten J, Van den Ende J. Time delays in diagnosis of pulmonary tuberculosis: A systematic review of literature. BMC Infect Dis. 2009;9:91. doi: 10.1186/1471-2334-9-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bassili A, Seita A, Baghdadi S, AlAbsi A, Abdilai I, Agboatwalla M, et al. Diagnostic and treatment delay in tuberculosis in 7 countries of the eastern mediterranean region. Infect Dis Clin Pract. 2008;16:23–35. [Google Scholar]
- 8.Nasehi M, Mohammad K, Gouya MM, Madjdzadeh R, Zamani G, Holakoii K, et al. Health care system delay in diagnosis and treatment of contagious tuberculosis in I.R. Iran. Tanaffos. 2003;(2):55–64. [Google Scholar]
- 9.Organization WH. Geneva: World Health Organization; 2010. Public-Private Mix for TB Care and Control: A Toolkit. [Google Scholar]
- 10.WHO. Available from: http://www.emro.who.int/tdr/TDR-Tuberculosis-Researchhtm 2011 .
- 11.The World Health Organization. Geneva: World Health Organization; 2003. Treatment of tuberculosis guideline for national programmes. [Google Scholar]
- 12.Lonnroth K, Thuong LM, Linh PD, Diwan VK. Delay and discontinuity--a survey of TB patients’ search of a diagnosis in a diversified health care system. Int J Tuberc Lung Dis. 1999;3:992–1000. [PubMed] [Google Scholar]
- 13.Lawn SD, Afful B, Acheampong JW. Pulmonary tuberculosis: Diagnostic delay in Ghanaian adults. Int J Tuberc Lung Dis. 1998;2:635–40. [PubMed] [Google Scholar]
- 14.Sherman LF, Fujiwara PI, Cook SV, Bazerman LB, Frieden TR. Patient and health care system delays in the diagnosis and treatment of tuberculosis. Int J Tuberc Lung Dis. 1999;3:1088–95. [PubMed] [Google Scholar]
- 15.Odusanya OO, Babafemi JO. Patterns of delays amongst pulmonary tuberculosis patients in Lagos, Nigeria. BMC Public Health. 2004;4:18. doi: 10.1186/1471-2458-4-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ngadaya ES, Mfinanga GS, Wandwalo ER, Morkve O. Delay in tuberculosis case detection in Pwani region, Tanzania. A cross sectional study. BMC Health Serv Res. 2009;9:196. doi: 10.1186/1472-6963-9-196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lal SS, Uplekar M, Katz I, Lonnroth K, Komatsu R, Yesudian Dias HM, et al. Global Fund financing of public-private mix approaches for delivery of tuberculosis care. Trop Med Int Health. 2011;16:685–92. doi: 10.1111/j.1365-3156.2011.02749.x. [DOI] [PubMed] [Google Scholar]
- 18.Diez M, Bleda MJ, Alcaide J, Caloto T, Castells C, Cardenal JI, et al. Determinants of patient delay among tuberculosis cases in Spain. Eur J Public Health. 2004;14:151–5. doi: 10.1093/eurpub/14.2.151. [DOI] [PubMed] [Google Scholar]
- 19.Leung EC, Leung CC, Tam CM. Delayed presentation and treatment of newly diagnosed pulmonary tuberculosis patients in Hong Kong. Hong Kong Med J. 2007;13:221–7. [PubMed] [Google Scholar]
- 20.Chan-Yeung M, Noertjojo K, Tan J, Chan SL, Tam CM. Tuberculosis in the elderly in Hong Kong. Int J Tuberc Lung Dis. 2002;6:771–9. [PubMed] [Google Scholar]
- 21.Lin HP, Deng CY, Chou P. Diagnosis and treatment delay among pulmonary tuberculosis patients identified using the Taiwan reporting enquiry system, 2002-2006. BMC Public Health. 2009;9:55. doi: 10.1186/1471-2458-9-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Huong NT, Vree M, Duong BD, Khanh VT, Loan VT, CoNV , et al. Delays in the diagnosis and treatment of tuberculosis patients in Vietnam: A cross-sectional study. BMC Public Health. 2007;7:110. doi: 10.1186/1471-2458-7-110. [DOI] [PMC free article] [PubMed] [Google Scholar]


