Abstract
Background:
Investigators describe a dramatic increase in the incidence of mood disorder after childbirth, with the largest risk in the 90 days after delivery. This study is designed to develop a relatively simple screening tool and validate it from the significant variables associated with postpartum depression (PPD) to detect delivered women at high risk of having PPD.
Materials and Methods:
In the cross-sectional study, 6,627 from a total of 7,300 delivered women, 2-12 months after delivery were recruited and screened for PPD. Split-half validation was used to develop the risk score. The training data set was used to develop the model, and the validation data set was used to validate the developed the risk factors of postpartum depression risk score using multiple logistic regression analysis to compute the β coefficients and odds ratio (OR) for the dependent variables associated with possible PPD in this study. Calibration was checked using the Hosmer and Lemeshow test. A score for independent variables contributing to PPD was calculated. Cutoff points using a trade-off between the sensitivity and specificity of risk scores derived from PPD model using the Receiver Operating Characteristic (ROC) curve.
Results:
The predicted and observed PPD were not different (P value = 0.885). The aROC with area under the curve (S.E.) of 0.611 (0.008) for predicting PPD using the suggested cut-off point of -0.702, the proportion of participants screening positive for PPD was 70.9% (sensitivity) (CI 95%; 69.5, 72.3) while the proportion screening negative was 60.1% (specificity) (CI 95%; 58.2, 62.1).
Conclusion:
Despite of the relatively low sensitivity and specificity in this study, it could be a simple, practical and useful screening tool to identify individual at high risk for PPD in the target population.
Keywords: Postpartum depression, risk score, validation
INTRODUCTION
Postpartum depression (PPD) is defined in the Diagnostic and Statistical Manual of Mental Disorders- IV[1] as a major depressive episode that occurs within 4 weeks after delivery. However, investigators describe a dramatic increase in the incidence of mood disorder after childbirth, with the largest risk in the 90 days after delivery.[2]
Community studies found the prevalence of PPD to be 13 percent.[3]
A significant number of men become depressed when their wife affected with PPD, further exacerbating the effects of PPD on the mother, marriage, and child development[4,5] Both, antenatal and postpartum depression can interfere with maternal-infant bonding, thereby adversely influencing infant development.[6,7,8,9,10,11] The negative interaction patterns formed during the early critical bonding period may impact on later child development, despite recovery from PPD.[9,10] As an example, conduct disorders,[12] inappropriate aggression,[13] and cognitive and attention deficits[14,15] have been described in children exposed to maternal psychiatric illnesses. However, maternal remission can have a positive effect on offspring.[16] Both, paternal and maternal depression has been associated with behavioral problems in children evaluated at 42 months.[5] Strain in the marital relationship is both a risk factor for and consequence of PPD.[7]
Suicide and infanticide are more likely to occur with postpartum psychosis than with postpartum depression. However, there is an increased risk of suicide, particularly in the most severe cases.[17] Fetal or infant death appears to be a strong risk factor for suicide[18] PPD increases the risk for further episodes of major depression, both puerperal and nonpuerperal.[19]
In summary, postnatal depression is a mental and emotional condition that can affect women during the first postnatal year. Since, the effects of postnatal depression are known to go beyond the mother in that it also affects the partner and the child. Additionally, severe postnatal depression can lead to infanticide, as well as maternal death, often by suicide. The emerging picture is that postnatal depression is indeed a public health problem.
Evidence demonstrates that all countries are faced with the challenge of postnatal depression, but low- to middle-income countries face the greatest burden. However, it also uncovered that not all women are assessed for postnatal depression, nor do all women receive treatment.[20]
These data highlight the need for universal screening of maternal depression during the postpartum period. In this way a tremendous researchers going to establish valid and reliable tools including community based self report scales, biological markers, statistical analysis methods and personality traits or PPD risk factors checklists for early screening and detection of PPD.
This is an active research area in women public health.
The aim of the present study is to develop a relatively simple screening tool from the significant variables associated with PPD to detect delivered women at high risk of having PPD.
MATERIALS AND METHODS
The study was conducted in rural areas of Isfahan province in central zone of Iran. The health centers in the area are responsible for providing health care services and socio-demographic data is available for all resident families including pregnant and child rearing women.
Participants were all rural women in Isfahan province who had a child ranging from 2 to12 months. Based on primary information from the health system of Isfahan University of Medical Sciences, about 8,000 eligible pregnant women were recruited in this study. Of those, 476 were excluded because of illiteracy and the rest invited to participate. A total of 7,300 agreed to complete the self report questionnaires using a written consent form. From them, 673 were excluded because they were incomplete and our final analysis was carried out on 6,627 participants.
This cross-sectional study (year of study) was carried on 2007, out jointly between the Behavioral Sciences Research Center (BSRC) and The Vice-Chancellor for Health of Isfahan University of Medical Sciences. Mental health professionals from local departments of the Vice-Chancellor for Health of Isfahan University supervised the data collection, as well as training the staff of health centers in all aspects of the study including its objectives and design. The BSRC's ethics committee approved the design of the study.
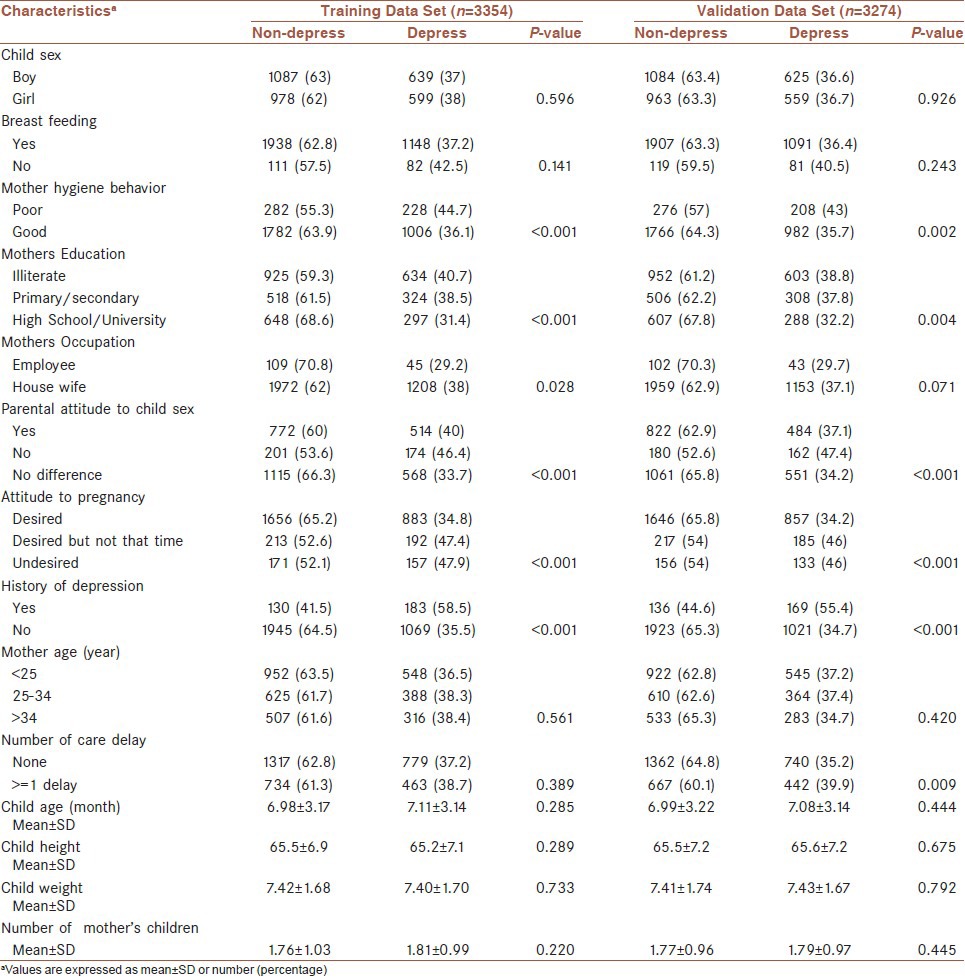
All eligible women were invited to attend the health centers on specified dates so as to complete the self report questionnaires. Participants who were unable to attend the center completed the questionnaires in their homes. The completed questionnaires were collected and then referred to mental health professionals of local departments. These mental health staff followed up women who were found to be severely depressed or suicidal on the questionnaire and evaluated the need for further intervention. The questionnaire included a number of variables to assess the risk of post-partum depression as shown in Table 1.
Table 1.
Baseline characteristics of 6,628 pregnant women in the training and validation data sets for the development of a risk score to predict postpartum depression (PPD)
The Persian version of Beck Depression Inventory (BDI- II) [21] was used both to screen for possible PPD and provide a measure of severity, since the calibration of the Persian version of Edinburgh Postnatal Depression Scale (EPDS) was not available at that time of data collection. The BDI questionnaire is 21-items with a four-point scale ranging from 0 to 3 score. Depression severity of a respondent is the sum of the score on each item, ranging from 0 to 63 score. The average internal-consistency of the total scores is 0.86 for psychiatric patients and 0.81 for normal adults. The average correlation of the BDI total scores with clinical ratings of depression was greater than 0.90 for the both psychiatric patients and normal adults. Based on the score obtained, the severity of possible depression was assigned as follows: 0-9 (no depression), 10-16 (mild depression), 17-29 (moderate depression) and 30-63 (severe depression).[22,23,24]
Split-half validation was used to develop the risk score. The data set was randomly divided into 2 data set generation the two 50% random sample of cases using SPSS package version 18. The training data set was used to develop the model, and the validation data set was used to validate the developed the risk factors of postpartum depression risk score. In the training data set, predictors at enrollment were examined using multiple logistic regression analysis by STATA version 9.0[25] to compute the β coefficients and odds ratio (OR) for the dependent variables associated with possible PPD in this study. The candidate baseline variables used for model selection included child age (month), breast feeding (0 if Yes and 1 if No), child height, mother hygiene behavior (1 if poor and 2 if good), parental attitude to child gender (1 if Yes, 2 if No and 3 if No difference), attitude to pregnancy (1 if Desired, 2 if Desired but not that time and 3 if undesired), history of depression (0 if No and 1 if Yes), mother age (year), mother education (1 if illiterate, 2 if primary/secondary, 3 if high school/university), mother occupation (1 if employee and 2 if housewife), number of mother's children, and number of care delay (0 if non-delay and 1 if equal or more than 1 time delay). Validation of the risk equation was performed using the test data set. Calibration was checked using the Hosmer and Lemeshow test. The data were divided into deciles of the predicted risk factors of postpartum depression. The chi-square test (8 degrees of freedom) was constructed using the predicted and observed numbers of PPD stratified by deciles of predicted risks. A score for independent variables contributing to PPD was calculated. Cutoff points using a trade-off between the sensitivity and specificity of risk scores derived from PPD model using the ROC curve.
RESULTS
Six thousand six hundred and twenty-seven pregnant women were identified and screened for possible depression using the BDI. Of these, 57.1% were screened possible cases of depression and based on the BDI scores, 20% (1,324) fell within the mild range of scores, 18.3% (1,211) within the moderate range and 18.9% (1,251) within the severe range. The age range of participants was varied between 13 to 50 years with mean (SD) of 26.03 (5.1) years.
Table 1 shows the baseline characteristics of pregnant women in the Training (n = 3354) a nd Validation (n = 3274) Data Sets for the Development of a Risk Score to Predict postpartum depression (PPD).
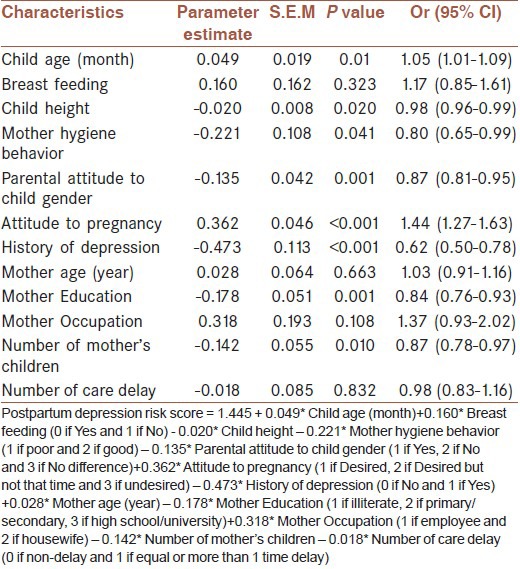
The risk score value was constructed from the estimated β coefficients as follows [Table 2]:
Table 2.
Parameter Estimates of the characteristics postpartum depression Risk Score for pregnant women using Training Data Set (n=3354)
We are going to evaluate the clinical application of this on the following researches.
PPD Risk Score = +1.445
+0.049* Child age (month)
+0.160* Breast feeding (0 if Yes and 1 if No)
-0.020* Child height
-0.221* Mother hygiene behavior (1 if poor and 2 if good)
-0.135* Parental attitude to child gender (1 if Yes, 2 if No and 3 if No difference)
+0.362* Attitude to pregnancy (1 if desired, 2 if desired but not that time and 3 if undesired)
-0.473* History of depression (0 if No and 1 if Yes)
+0.028* Mother age (year)
-0.178* Mother education (1 if illiterate, 2 if primary/secondary, 3 if high school/university)
+0.318* Mother occupation (1 if employee and 2 if housewife)
-0.142* Number of mother's children
-0.018* Number of care delay (0 if non-delay and 1 if equal or more than 1 time delay).
In the validation data set, the predicted and observed PPD were not different (P value = 0.885) [Figure 1]. The ROC for predicting PPD with area under the curve (S.E.) of 0.611 (0.008) using the suggested cutoff point of -0.702 the proportion of participants screening positive for PPD was 70.9% (sensitivity) (CI 95%; 69.5, 72.3) while the proportion screening negative was 60.1% (specificity) (CI 95%; 58.2, 62.1).
Figure 1.
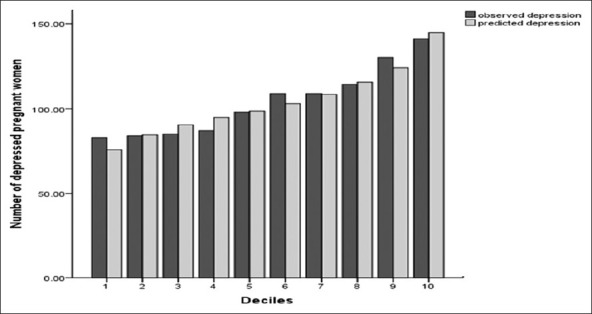
The predicted and observed depression rates by deciles of predicted probability of risk factor in the validation data set (Chi-square = 3.679; df = 8; P = 0.885)
DISCUSSION
Our findings revealed that risk factors for possible PPD in this study were very similar to studies in other countries but the impact of low level of education, unplanned pregnancy and undesired gender of child on risk of PPD seems to be a distinguishing aspect of Iranian women. The details of findings of this study regard to PPD risk factors presented in another article.[26]
While the Edinburgh Postnatal Depression Scale (EPDS) is preferred to others in detecting/screening for a possible PPD, we did not have access to the Persian version of this scale and so compromised by using the Persian version of Beck Depression Inventory BDI-II. The possibility that the BDI scale over-estimated the prevalence of PPD cannot be excluded as it was not specially designed to screen for PPD to identify postnatal depression, although, it has been used as a screener in other studies.[27]
We believe that the public health benefit of this PPD risk score is considerable. Despite of the relatively low sensitivity and specificity in this study, it could be a simple, practical and useful screening tool to identify those at high risk for PPD in the population.
In conclusion, this simple, inexpensive screening instrument can be easily used by staff of health centers instead of psychiatrist experts. This study show that the PPD risks score is a useful screening tool, which can be applied to demographically similar populations in different parts of the world where there may be a scarcity of mental health professionals.
Limitations: More studies are required to replicate these findings or to adjust the cutoff scores so as to achieve greater sensitivity and specificity.
ACKNOWLEDGMENTS
We are grateful to the health workers and mental health professionals of local departments who helped in conducting this study. We thank Mrs. Mahnaz Kelishadi for help with on time and precise refer of collected data to us, Dr Gholamhossein Sadri head of The Vice-Chancellor for Health of Isfahan University of medical sciences for his co-operations.
This study was supported by a research grant from the fluid research fund of Vice-Chancellor for Research of Isfahan University of medical sciences.
Footnotes
Source of Support: This work was supported by Vice-Chancellor for Research of Isfahan University of medical sciences. Grant number: 83136
Conflict of Interest: None declared.
REFERENCES
- 1.American Psychiatric Association (APA) Diagnostic and Statistical Manual of Mental Disorder: DSM-IV. 1996:422–3. [Google Scholar]
- 2.O’Hara MW. Postpartum depression: What we know. J Clin Psychol. 2009;65:1258–69. doi: 10.1002/jclp.20644. [DOI] [PubMed] [Google Scholar]
- 3.Horowitz JA, Murphy CA, Gregory KE, Wojcik J. A community based screening initiative to identify mothers at risk for postpartum depression. J Obstet Gynecol Neonatal Nurs. 2011;40:52–61. doi: 10.1111/j.1552-6909.2010.01199.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Paulson JF, Dauber S, Leiferman JA. Individual and combined effects of postpartum depression in mothers and fathers on parenting behavior. Pediatrics. 2006;118:659–68. doi: 10.1542/peds.2005-2948. [DOI] [PubMed] [Google Scholar]
- 5.Ramchandani P, Stein A, Evans J, O’Connor TG. Paternal depression in the postnatal period and child development: A prospective population study. Lancet. 2005;365:2201–5. doi: 10.1016/S0140-6736(05)66778-5. [DOI] [PubMed] [Google Scholar]
- 6.Halbreich U. The association between pregnancy processes, preterm delivery, low birth weight, and postpartum depressions-The need for interdisciplinary integration. Am J Obstet Gynecol. 2005;193:1312–22. doi: 10.1016/j.ajog.2005.02.103. [DOI] [PubMed] [Google Scholar]
- 7.Bagner DM, Pettit JD, Lewinsohn PM, Seeley JR. Effect of maternal depression on child behavior: A sensitive period? J Am Acad Child Adolesc Psychiatry. 2010;49:669–707. doi: 10.1016/j.jaac.2010.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Field T. Postpartum depression effects on early interactions, parenting, and safety practices: A review. Infant Behav Dev. 2010;33:1–6. doi: 10.1016/j.infbeh.2009.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sutter-Dallay AL, Murray L, Dequae-Merchadou L, Glatigny-Dallay E, Bourgeois ML, Verdoux H. A prospective longitudinal study of the impact of early postnatal vs. chronic maternal depressive symptoms on child development. Eur Psychiatry. 2011;26:484–9. doi: 10.1016/j.eurpsy.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 10.Lilja G, Edhborg M, Nissen E. Depressive mood in women at childbirth predicts their mood and relationship with infant and partner during the first year postpartum. Scand J Caring Sci. 2012;26:245–53. doi: 10.1111/j.1471-6712.2011.00925.x. [DOI] [PubMed] [Google Scholar]
- 11.Hanington L, Ramchandani P, Stein A. Parental depression and child temperament: Assessing child to parent effects in a longitudinal population study. Infant Behav Dev. 2010;33:88–95. doi: 10.1016/j.infbeh.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Matthew CM, Jeffrey CA, Judy G. A prospective study of the cognitive-stress model of depressive symptoms in adolescents. J Abnorm Psychol. 2008;117:719–34. doi: 10.1037/a0013741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Muralidharan A, Yoo D, Ritschel LA, Simeonova DI. Development of emotion regulation in children of bipolar parents: Putative contributions of socioemotional and familial risk factors. Clin Psychol Sci Prac. 2010;17:169–86. [Google Scholar]
- 14.Zahn-Waxler C, Chapman M, Cummings EM. Cognitive and social development in infants and toddlers with a bipolar parent. Child Psychiatry Hum Dev. 1984;15:75–82. doi: 10.1007/BF00706165. [DOI] [PubMed] [Google Scholar]
- 15.Beck CT. The effects of postpartum depression on child development: A meta-analysis. Arch Psychiatr Nurs. 1998;12:12–20. doi: 10.1016/s0883-9417(98)80004-6. [DOI] [PubMed] [Google Scholar]
- 16.Weissman MM, Pilowsky DJ, Wickramaratne PJ, Talati A, Wisniewski SR, Fava M, et al. Remissions in maternal depression and child psychopathology: A STAR* D-child report. JAMA. 2006;295:1389–98. doi: 10.1001/jama.295.12.1389. [DOI] [PubMed] [Google Scholar]
- 17.Lindahl V, Pearson JL, Colpe L. Prevalence of suicidality during pregnancy and the postpartum. Arch Womens Ment Health. 2005;8:77–87. doi: 10.1007/s00737-005-0080-1. [DOI] [PubMed] [Google Scholar]
- 18.Schiff MA, Grossman DC. Adverse perinatal outcomes and risk for postpartum suicide attempt in Washington state, 1987-2001. Pediatrics. 2006;118:669–75. doi: 10.1542/peds.2006-0116. [DOI] [PubMed] [Google Scholar]
- 19.Nonacs R, Cohen LS. Postpartum mood disorders: Diagnosis and treatment guidelines. J Clin Psychiatry. 1998;59(Suppl 2):34–40. [PubMed] [Google Scholar]
- 20.Almond P. Postnatal depression: A global public health persprcive. Perspect Public Health. 2009;129:221–7. doi: 10.1177/1757913909343882. [DOI] [PubMed] [Google Scholar]
- 21.Ghassemzadeh H, Mojtabai R, Karamghadiri N, Ebrahimkhani N. Psychometric properties of a Persian-language version of the Beck Depression Inventory-Second edition: BDI-II Persian. Depress Anxiety. 2005;21:185–92. doi: 10.1002/da.20070. [DOI] [PubMed] [Google Scholar]
- 22.Beck AT, Steer RA. Internal consistencies of the original and revised Beck Depression Inventory. J Clin Psychol. 1984;40:1365–7. doi: 10.1002/1097-4679(198411)40:6<1365::aid-jclp2270400615>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 23.Beck AT, Rush AJ, Shaw BF, Emery G. New York: Cuiford Press; 1979. Cognitive therapy of depression. [Google Scholar]
- 24.Beck AT, Steer RA, Carbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin Psychol Rev. 1988;8:77–100. [Google Scholar]
- 25.Schumm LP. Review of data analysis using stata by Kohler and Kreuter. Stata J. 2005;5:594–600. [Google Scholar]
- 26.Kheirabadi GR, Maracy MR, Barekatain M, Salehi M, Sadri GH, Kelishadi M, et al. Risk factors of postpartum depression in rural areas of Isfahan Province, Iran. Arch Iran Med. 2009;12:461–7. [PubMed] [Google Scholar]
- 27.Harris B, Huckle P, Thomas R, Johns S, Fung H. The use of rating scales to identify post-natal depression. Br J Psychiatry. 1989;154:813–7. doi: 10.1192/bjp.154.6.813. [DOI] [PubMed] [Google Scholar]


