Abstract
Background:
This study was done to assess the use of traditional/complementary and alternative medicine (TM/CAM) during pregnancy and the reasons behind it from the mother’s perspective.
Materials and Methods:
In a cross-sectional study, 919 pregnant mothers attending at prenatal care units of governmental health centers recruited through a multistage sampling and completed a self-report questionnaire about the use of TM/CAM during pregnancy.
Findings:
TM/CAM was used by 83.7% of women during pregnancy. Diet/nutrition change was applied by 42.3%, herbal preparations by 49.2%, vitamin and mineral by 30.1%, body based practices by 24.7% and spiritual methods by 22.9% of mothers. Most frequently used herbal products were frankincense in 28.6% and date fruit in 26.4% of mothers. The most common indication of diet/nutrition changes and herbal products used related to mothers was gastro-intestinal disorders. Most of the TM/CAM methods used (64.32%) were happening or beginning from the first trimester of pregnancy.
Conclusions:
The use of TM/CAM methods in pregnancy is very common, mainly included the methods suggested by traditional Islamic Iranian medicine. Thus, clinicians should be informed to address CAM methods at each obstetric visit. Safety and efficacy of CAM must be explored and taught in every health education program. Future studies should focus on the safety and efficacy of TM/CAM in pregnancy and clinicians should be educated to address these methods at prenatal visits.
Keywords: Complementary and alternative medicine, traditional medicine, obstetrics, pregnancy, women, diet and nutrition, herbal preparations, spiritual therapy
INTRODUCTION
Recent studies show that complementary and alternative medicine (CAM) is frequently used in the field of obstetrics, worldwide.[1] The medical view holds pregnancy and childbirth as inherently risky, therefore technological interventions are required in order to decrease the risks.[2] Doubts about the well-being of the fetus were found to be especially prominent in women in this period.[3] As complementary and alternative medicine (CAM) is believed safe, pregnant women may consider it to be the best choice for problems during pregnancy as these methods also seem very true to life from the lay standpoint.[4] An overview on earlier studies on CAM during pregnancy showed that there are great variations regarding the use of different CAM methods in different countries.[5] In spite of no known national CAM prevalence studies of pregnant women in the U.S., existing reports of CAM usage in pregnancy range from 7.1% to 73%.[6–10] CAM therapies are also widely used by the U.S. clinical nurse midwives.[11] There are only a few reports that study the safety of CAM methods in pregnancy. A recent study shows that the use of CAM is associated with a 30% lower ongoing pregnancy/live birth rate through 12months of fertility treatment.[12] Considering the fact that pregnant women frequently take these without report to their prenatal care provider, the uncritical CAM usage must be considered a problem.[13] While some CAM methods may be a serious health problem, others are used in spite of proven efficacy.[14,15] CAM usage during pregnancy and during childbirth has primarily been studied in the United States of America, Norway, Canada, Sweden, Italy, Australia and China.[5] Our country has a strong background in use of traditional medicine that seems in recent years is increasing. In spite of that, there is a lack of information about the current use of CAM methods especially during pregnancy in Iran. In order to understand the better use of CAM during pregnancy in our society, we conducted a study to assess the use of CAM and its indications during pregnancy. The results of this study could be a base for safety analyses, so pregnant women could be better counseled on CAM that will finally guide to the use of more effective and safe methods for mother and fetus.
MATERIALS AND METHODS
This cross-sectional study was conducted from a convenience sampling of 919 pregnant women attending in prenatal unit of 26 health centers in Mashhad, Iran. The study was approved by the research ethics committee of Mashhad University of medical sciences. Subjects were given both verbal and written information regarding the study. Signed informed consent was obtained prior to entry. All participants had Iranian nationality. The pregnant eligible women were selected through a multi stage sampling. A semi-structured questionnaire was applied to assess TM/CAM methods usage during pregnancy designed base on the findings of an earlier study through unstructured in-depth interviews with 40 women of study population; the items related to women experiences of TM/CAM methods were extracted from the context of reviews. Then the items were categorized and categories were completed using scientific references. The questionnaire’s content validity was confirmed by an expert panel from gynecologists, midwives and pharmacologists and its reliability was confirmed by test- retest one week later. It was filled by two bachelor midwives were trained for the purpose of gathering data in the study. It took about 15-40 minutes to be completed. TM/CAM methods were defined in categories of 1) diet and nutrition change, 2) herbs and herbal pharmaceuticals -approved by the Ministry of health and sold through pharmacies. 3) mind-body interventions including spiritual therapies, deep-breathing exercises, relaxation, aromatherapy, music, yoga, etc., 4) body-based practices and manual healing including massage, thermotherapy, light therapy, acupressure, physical exercises, bed rest, therapeutic touch, Chiropractics, etc and 5) supplemental minerals and vitamins. In addition, a comment section was provided to subjects to identify the other forms of TM/CAM usage during pregnancy. Any changes in amounts and types of routine use of 5 food groups’, for example change the type of oils or amounts or types of oils, use of junk food or deleting some foods from the nutritional program, which mothers applied for purposes of meeting a need or solving a health related problem, based on traditional believes or as a complementary method, was considered as diet and nutrition change. Any increase in the use of spices and the use of herbs that are not commonly took as vegetables and fruits were considered as herbal products usage. It was also asked if the methods used for the purpose of promoting the health and preventing or treatment of a health problem. They were asked to report if the usage is suggested by health care providers or self- regulated. Data also gathered about the indication of TM/CAM usage, its form, frequency, the recommendation source and satisfaction from applied TM/CAM methods. Data on demographic factors and obstetric history were collected. Quantitative data was analyzed using SPSS software version 11.0 (SPSS Inc., Chicago, IL) database. Qualitative data analysis used coding of verbatim materials to identify themes that best represented the data. Descriptive results were expressed as mean (standard deviation) and frequency. Statistical differences between two groups of TM/CAM users and non-users were determined by independent sample t-test and between three groups by one-way analysis of variance (ANOVA) and Tukey’s post hoc test. Chi-square test was used to compare the non-continuous data between 2 groups.
FINDINGS
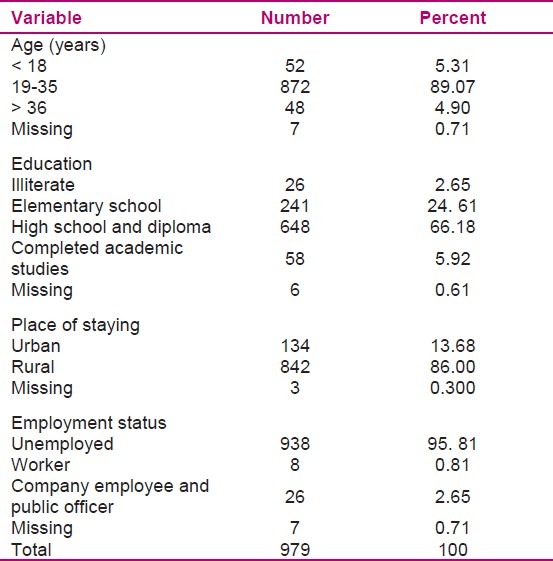
The mean age of participants was 25.7 (5.1) years old. Table 1 demonstrates the demographic characteristics of participants. Some 769 (83.7%) of women used at least one TM/CAM methods during their pregnancy, whereas, 150 (16.3%) did not use any form of it, in total TM/CAM methods have been used 1965 times with mean of 2.56 per user until the time of the study.
Table 1.
Demographic characteristics of participants
Diet/nutrition change had been applied by 42.3%, herbal preparations by 49.2%, mind-body methods by 22.9%, vitamins and minerals by 30.14% and body based practices by 24.7% of mothers. Figure 1 demonstrates the distribution of TM/CAM categories’ in 1965 time use.
Figure 1.
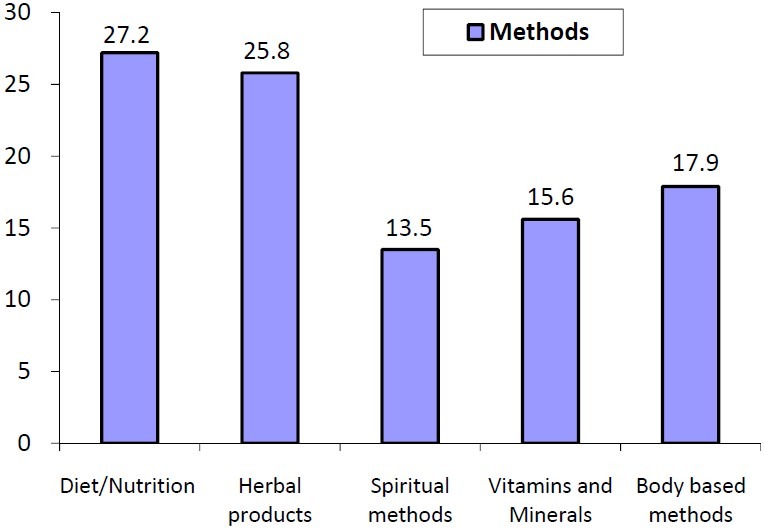
Methods of complementary and alternative medicine used during pregnancy
Until the time of study during their pregnancy, 22.9% of mothers used mind body methods for 266 times that were solely spiritual methods including reading some Quran chapters or other religious texts. The most common religious texts read include complete Quran recitation in 53 (19.9%), Surah of Yusuf (P.B.U.H.) in 88 (33.0%), Surah of Yasin in 27 (10.1%), Surah of Mohammad (P.B.U.H.) in 13 (4.8%), Surah of Maryam (P.B.U.H.) in 10 (3.7%), Surah of Val-Asr in 9 (3.3%) and other forms of religious practices included prayers and etc. were applied 66 (24.8%) times. Other mind- body methods were not reported by our participants.
Spiritual methods were applied for the purpose of mothers’ calming down in 31 (14.7%), anxiety relief in 12 (5.7%) and facilitating delivery in 18 (6.8%) of users. Indications related to baby include baby being safe in 21 (7.9%), clever in 6 (2.3 %), tolerant in 32 (12%), well behaved in 80 (30.1%). The Surah of Yusuf (P.B.U.H.) was read for the purpose of infant’s beauty in 86 (32.3%) of cases. The routine reading of Quran unrelated to purposes of pregnancy and health purposes was not recorded in this study.
A common category was applying herbal preparations that were used for a variety of purposes. Herbal products were used by 452 (%49.2) mothers for 507 times. Each user applied these methods between 1 and 4 times during pregnancy. From 507 cases of herbal methods usage, 73.1% cases were using traditional form of herbal products and 26.83 % cases were related to herbal pharmaceuticals. Table 2 shows the frequency, indications and form of use of 2 categories of herbal preparations by our participants. Among 244 times herbal usage, the most common indications were related to gastro intestinal problems that include 96 times of all herbal uses (39.3%). In our study 15 (3.3%) of mothers who used herbal medicines reported some side effects that included mild or moderate form of nausea, gastric pain, low blood pressure and urticarial that relieved without any intervention. In 57% of cases, herbal pharmacological products and in 11.3% of cases traditional forms of herbs were suggested by health care providers.
Table 2.
Traditional/complementary and alternative medicine (TM/CAM) methods used in pregnant mothers
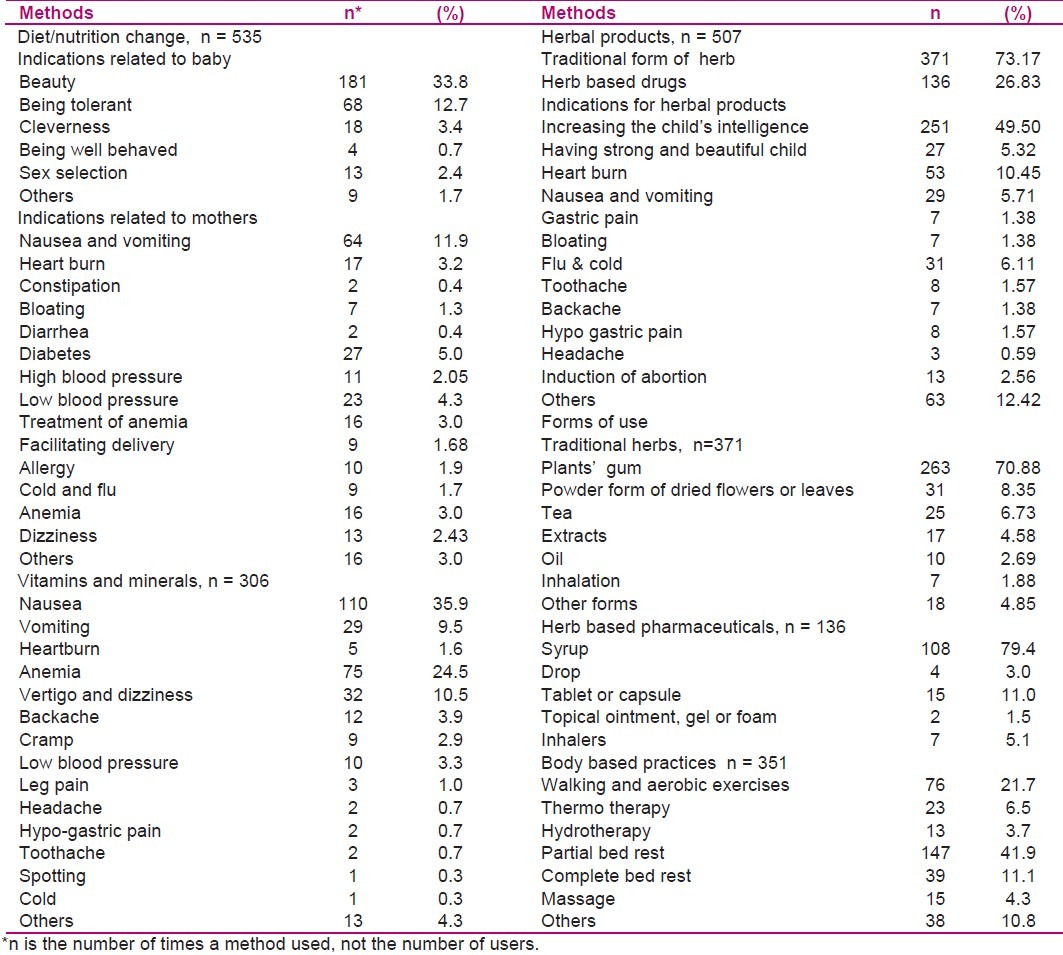
Diet/nutrition change applied 535 times by mothers and was the most common method. They were used for indications related to the babies in 293 cases and for indications related to the mothers in 242 cases. Indications of diet/nutrition change and frequency of its use is shown in Table 2. Most common indications ofdiet/nutrition change related to mothers included gastro- intestinal tract disorders used in 92 (17.2%) cases. Change in the use of fruits was the most common nutrition change applied 339 times by 281 (30.5%) mothers. Date was the most common fruit used by 243 (26.4%) of mothers during pregnancy.
Vitamin and mineral supplements were used 306 times by 277 mothers for treatment or health promotion purposes. The iron and folate supplements were used by 100% of cases, ranged from 6 to 200 days, thus we didanalyze the routine use of them. The other indications of vitamin and mineral supplements usage are mentioned in Table 2.
Table 2, also shows the frequency and indications of body based practices that was used 351 times by 227 participants. In this category, partial bed rest and then walking/aerobic exercises were the most common practices.
Noticeably, the use of TM/CAM methods were most common in the first trimester of pregnancy, as 1264 time (64.3%) of use happened in the first trimester, 568 times (28.9%) in second trimester and 106 times (5.4%) in third trimester of pregnancy. “Hijamat” - a traditional practice of extracting tainted blood from multiple superficial cuts- and also, TM/CAM methods such as chiropractics, biofeedback, homeopathy, yoga etc were not been used by our participants. TM/CAM usage was not in significant relationship with family income, place of residence, the number of pregnancies and parents’ age and education.
As Figure 2 shows, the mothers’ opinion on the efficacy of applied methods showed that in 42.9% of cases of usage, the mothers were somehow completely satisfied with TM/CAM methods and in 49.1% of times, it was too early to evaluate the effects.
Figure 2.
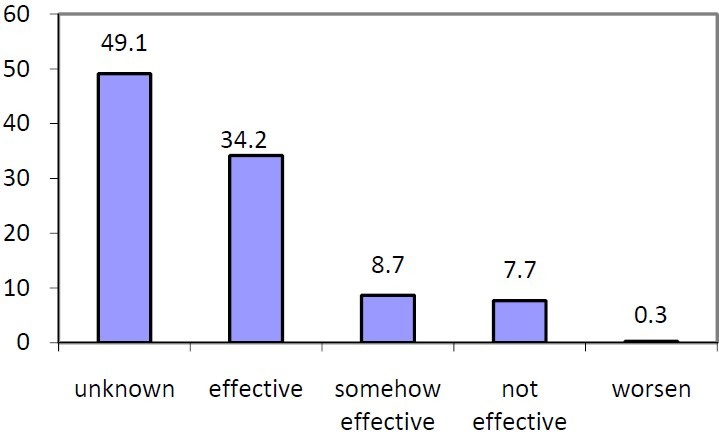
Mothers’ opinion about methods of traditional/complementary and alternative medicine (TM/CAM) in pregnancy
The most important reason reported for using TM/CAM methods was being natural and safe to use especially for fetus at 53%; traditional and cultural belief 11%; having previous successful experience of using these products by themselves and relatives 19% and other reasons 17%. The main sources of information for using CAM/TM methods were listed as: friend, colleague and family members 33.5%; obstetricians and midwives 41.5%; books, journals and magazines 6.7%; traditional healers 3.6%; radio and television 5.1%, internet. 3% and unknown 9.3%.
DISCUSSION
This is the first detailed analysis on the use of TM/CAM methods during pregnancy in Iran. Our findings showed that the use of TM/CAM during pregnancy is very common, and that the commonly used methods often meet with great satisfaction.
Diet/nutrition change (27.2%) was the most common method used in pregnancy. We removed routine increase of milk, egg and meat from diet change analysis as our participants were educated to increase their protein intake and self-reports of them indicated more intakes of such foods, although in some cases, it may not be enough. The most common nutrition change in our study was related to fruits. Date was the first ranked fruit used in pregnancy. In Islamic documentations, it is recommended to be used during pregnancy and postpartum.[16] Our previous research also showed the common use of date for obstetrics purposes.[17] All of our participants used iron and folate supplements during pregnancy that varied from a few days to regular daily usage; because these supplements are widely distributed free of charge to pregnant women in the governmental health centers. Indeed, 15.57% of pregnant mothers used more minerals and vitamins for other purposes. In the Bercaw et al. study (2010), 47% of mothers took vitamin supplements other than prenatal vitamins.[18]
In the study of Holst et al., floradix, ginseng and valerian were the most common used herbal drugs during pregnancy.[19] Other herbal products were also highly applied in our study. Gastro-intestinal disorders were themost common indication related to mothers. In a study, herbal supplement was reported by almost 10% and non-herbal CAM therapies by 13.5% of pregnant mothers.[6] In the Bercaw et al. study, 19% of the mothers took herbs for reason of improving the woman’s general health and energy level or treating specific pregnancy- related problems.[18] Some of the herbal products with their lack of safety and efficacy documentation might constitute a risk for woman as well as fetus.[14,20] Especially because users of herbal products often omit telling their doctor about the use[21,22] and that health care providers have little knowledge about herbs.[23,24]
Our participants also commonly used spiritual methods for health promotion purposes or overcoming their healthy problems during pregnancy. The most common method used was reading some Quran chapters or other religious text that seems very common in Muslim populations. The use of the other forms of mind-body interventions was not reported in our study. The body based practices were reported by 17.9%, mostly included bed rest and walking/aerobic exercises.
These findings are mainly in accordance with our study on intra-partum and postpartum use of CAM methods that showed the dominant role of the methods prescribed by traditional Islamic-Iranian medicine.[17] Hijamat (cupping), that is relatively common for health purposes among Iranian Muslims as a traditional form of medicine, was not reported in our study, perhaps it did not appeal to them or many of providers did not perform this procedure in pregnancy.[17] Other types of CAM therapies such as homeopathy, osteopathy, reflexology and acupuncture, etc., were not used by our subjects that are different from studies in other countries,[19] probably due to low access and low familiarity with these methods in Iran. Studies in Europe showed that massage, acupuncture, vitamins and herbs are the most frequently applied methods during pregnancy.[14,25,26]
The frequencies of various CAM methods’ usage vary greatly between different countries.[27,5]
In this study CAM/TM usage was not in relation to couple’s age, education and the number of pregnancies. It seems traditional medicine is highly popular and accepted among all groups of Iranians. Our participants have reported satisfactory results with CAM usage. Our study showed that women used CAM/TM during pregnancy, mostly because they belief in safety of natural products especially for fetus. These findings are in accordance with previous studies.[19,13,28] The use of CAM/TM methods were most common in the first trimester of pregnancy and mostly applied for treatment of common problems of pregnancy such as nausea, heart burn, etc. The mothers may be unaware about the sensitivity of this period for fetus’ health and development or be unaware about beingpregnant. Safety concerns emphasize the need for data collection on applying the methods during pregnancy and the importance of pregnancy databases in revealing potential useful and therapeutic effects, side effects and teratogenic/embryo-fetotoxic signals. In our study it showed that a few mothers had unsuccessful abortion trial with the herbs. The unsuccessful use of abortifacients is a particular cause for concern as it may have toxic effects for mother or fetus.[29]
In our study herbal based pharmaceuticals were mainly prescribed by physicians and midwives, whereas traditional forms of herbs were often used by themselves or suggested by relatives.
These finding indicates the need for informing pregnant mothers about the maternal fetal risk of herbal products’ usage. Therefore, health care providers, especially those offering prenatal care should be aware of potential benefits or risks associated with especially self-prescribed herbal remedies in pregnancy.[30]
Study limitations included gathering and analyzing information from a group of pregnant women that were under cover of governmental health system, thus the findings cannot be generalized to whom received antenatal cares from private health systems and offices. The health system offered total maternity and antenatal care in order to motivate women to be adherence to healthy behaviors (e.g. less illicit drug use). Thus these mothers may have more desire to non chemical drugs and methods for solving their healthy problems. Participants received health education especially on vitamin and mineral use, diet and nutritional needs, illicit drug risks in pregnancy and other important educational materials for maternal-child health. However, this information usually ignores the education of mothers regarding TM/CAM use especially herbs in pregnancy. Other study limitation is related to participants’ inability to recall all previous information. It is noteworthy that researchers aimed to describe findings without intention to confirm or disconfirm any of the used TM/CAM methods.
CONCLUSION
This study shows wide spread TM/CAM usage, mainly self-prescribed herbal-based methods among pregnant women. Our findings about the prevalence of TM/CAM use in pregnancy benefit midwives and obstetricians and alert the importance of their familiarity with the advantages and disadvantages of TM/CAM methods for obstetric patients. Self-administered and prescribed TM/CAM methods for pregnant women should be carefully monitored to provide supportive scientific evidences to assure its safety and efficacy. Mothers should be informed regarding the effects of applying TM/CAM methods especially herb based products on pregnancy outcome. The evidences on efficacy and safety of TM/CAM methods should be further explored through well designed studies. Evidence based TM/CAM therapy should be considered as a part of the medical and midwifery education programs.
ACKNOWLEDGMENT
This study was supported by a grant award from Mashhad University of Medical Sciences. Special thanks to the midwives at various health centers, research associate [interviewer] and mothers who participated in the study.
Footnotes
Research Article of Mashhad University of Medical Sciences, No: 84052
Source of Support: Mashhad University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.Hrgovic I, Hrgovic Z, Habek D, Oreskovic S, Hofmann J, Munstedt K. Use of complementary and alternative medicine in departments of obstetrics in croatia and a comparison to Germany. Forsch Komplementmed. 2010;17(3):144–6. doi: 10.1159/000314902. [DOI] [PubMed] [Google Scholar]
- 2.Mitchell M. Risk, pregnancy and complementary and alternative medicine. Complement Ther Clin Pract. 2010;16(2):109–13. doi: 10.1016/j.ctcp.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 3.Hammarberg K, Fisher JR, Wynter KH. Psychological and social aspects of pregnancy, childbirth and early parenting after assisted conception: a systematic review. Hum Reprod Update. 2008;14(5):395–414. doi: 10.1093/humupd/dmn030. [DOI] [PubMed] [Google Scholar]
- 4.Low DT. The use of botanicals during pregnancy and lactation. Altern Ther Health Med. 2009;15(1):54–8. [PubMed] [Google Scholar]
- 5.Adams J, Lui CW, Sibbritt D, Broom A, Wardle J, Homer C, et al. Women’s use of complementary and alternative medicine during pregnancy: a critical review of the literature. Birth. 2009;36(3):237–45. doi: 10.1111/j.1523-536X.2009.00328.x. [DOI] [PubMed] [Google Scholar]
- 6.Gibson PS, Powrie R, Star J. Herbal and alternative medicine use during pregnancy: a cross-sectional survey. Obstetrics & Gynecology. 2001;97(4, Supplement 1):S44–S45. [Google Scholar]
- 7.Hepner DL, Harnett M, Segal S, Camann W, Bader AM, Tsen LC. Herbal medicine use in parturients. Anesth Analg. 2002;94(3):690–3. doi: 10.1097/00000539-200203000-00039. [DOI] [PubMed] [Google Scholar]
- 8.Refuerzo JS, Blackwell SC, Sokol RJ, Lajeunesse L, Firchau K, Kruger M, et al. Use of over-the-counter medications and herbal remedies in pregnancy. Am J Perinatol. 2005;22(6):321–4. doi: 10.1055/s-2005-873235. [DOI] [PubMed] [Google Scholar]
- 9.Tsui B, Dennehy CE, Tsourounis C. A survey of dietary supplement use during pregnancy at an academic medical center. Am J Obstet Gynecol. 2001;185(2):433–7. doi: 10.1067/mob.2001.116688. [DOI] [PubMed] [Google Scholar]
- 10.Westfall RE. Herbal healing in pregnancy: women’s experiences. J Herb Pharmacother. 2003;3(4):17–39. [PubMed] [Google Scholar]
- 11.Hastings-Tolsma M, Terada M. Complementary medicine use by nurse midwives in the U.S. Complement Ther Clin Pract. 2009;15(4):212–9. doi: 10.1016/j.ctcp.2009.06.016. [DOI] [PubMed] [Google Scholar]
- 12.Boivin J, Schmidt L. Use of complementary and alternative medicines associated with a 30% lower ongoing pregnancy/live birth rate during 12 months of fertility treatment. Hum Reprod. 2009;24(7):1626–31. doi: 10.1093/humrep/dep077. [DOI] [PubMed] [Google Scholar]
- 13.Holst L, Wright D, Haavik S, Nordeng H. The use and the user of herbal remedies during pregnancy. J Altern Complement Med. 2009;15(7):787–92. doi: 10.1089/acm.2008.0467. [DOI] [PubMed] [Google Scholar]
- 14.Nordeng H, Havnen GC. Use of herbal drugs in pregnancy: a survey among 400 Norwegian women. Pharmacoepidemiol Drug Saf. 2004;13(6):371–80. doi: 10.1002/pds.945. [DOI] [PubMed] [Google Scholar]
- 15.Smith CA, Cochrane S. Does acupuncture have a place as an adjunct treatment during pregnancy. A review of randomized controlled trials and systematic reviews? Birth. 2009;36(3):246–53. doi: 10.1111/j.1523-536X.2009.00329.x. [DOI] [PubMed] [Google Scholar]
- 16.Majlisi MB. Bahar ol-Anvar. Beyrut: Darorreza; [Google Scholar]
- 17.Khadivzadeh T, Fooladi M. Complementary and Alternative Medicine use in Childbirth and Postpartum in Mashhad, Iran in 2008. Proceedings of the International Congress of Obstetrics and Reproductive Health; 2011 May 3-5; Mashhad, Iran. 2011. [Google Scholar]
- 18.Bercaw J, Maheshwari B, Sangi-Haghpeykar H. The use during pregnancy of prescription, over-the-counter, and alternative medications among Hispanic women. Birth. 2010;37(3):211–8. doi: 10.1111/j.1523-536X.2010.00408.x. [DOI] [PubMed] [Google Scholar]
- 19.Holst L, Nordeng H, Haavik S. Use of herbal drugs during early pregnancy in relation to maternal characteristics and pregnancy outcome. Pharmacoepidemiol Drug Saf. 2008;17(2):151–9. doi: 10.1002/pds.1527. [DOI] [PubMed] [Google Scholar]
- 20.Ernst E. Herbal medicinal products during pregnancy: are they safe? BJOG. 2002;109(3):227–35. doi: 10.1111/j.1471-0528.2002.t01-1-01009.x. [DOI] [PubMed] [Google Scholar]
- 21.Kennedy J. Herb and supplement use in the US adult population. Clin Ther. 2005;27(11):1847–58. doi: 10.1016/j.clinthera.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 22.Thomas K, Coleman P. Use of complementary or alternative medicine in a general population in Great Britain. Results from the National Omnibus survey. J Public Health (Oxf) 2004;26(2):152–7. doi: 10.1093/pubmed/fdh139. [DOI] [PubMed] [Google Scholar]
- 23.Suchard JR, Suchard MA, Steinfeldt JL. Physician knowledge of herbal toxicities and adverse herb-drug interactions. Eur J Emerg Med. 2004;11(4):193–7. doi: 10.1097/01.mej.0000134721.72356.f7. [DOI] [PubMed] [Google Scholar]
- 24.Giveon SM, Liberman N, Klang S, Kahan E. A survey of primary care physicians’ perceptions of their patients’ use of complementary medicine. Complement Ther Med. 2003;11(4):254–60. doi: 10.1016/s0965-2299(03)00114-6. [DOI] [PubMed] [Google Scholar]
- 25.Skouteris H, Wertheim EH, Rallis S, Paxton SJ, Kelly L, Milgrom J. Use of complementary and alternative medicines by a sample of Australian women during pregnancy. Aust N Z J Obstet Gynaecol. 2008;48(4):384–90. doi: 10.1111/j.1479-828X.2008.00865.x. [DOI] [PubMed] [Google Scholar]
- 26.Wang SM, DeZinno P, Fermo L, William K, Caldwell-Andrews AA, Bravemen F, et al. Complementary and alternative medicine for low-back pain in pregnancy: a cross-sectional survey. J Altern Complement Med. 2005;11(3):459–64. doi: 10.1089/acm.2005.11.459. [DOI] [PubMed] [Google Scholar]
- 27.Munstedt K, Kirsch K, Milch W, Sachsse S, Vahrson H. Unconventional cancer therapy--survey of patients with gynaecological malignancy. Arch Gynecol Obstet. 1996;258(2):81–8. doi: 10.1007/BF00626028. [DOI] [PubMed] [Google Scholar]
- 28.Fakeye TO, Adisa R, Musa IE. Attitude and use of herbal medicines among pregnant women in Nigeria. BMC Complement Altern Med. 2009;9:53. doi: 10.1186/1472-6882-9-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pinn G, Pallett L. Herbal medicine in pregnancy. Complement Ther Nurs Midwifery. 2002;8(2):77–80. doi: 10.1054/ctnm.2001.0620. [DOI] [PubMed] [Google Scholar]
- 30.Tiran D. The use of herbs by pregnant and childbearing women: a risk-benefit assessment. Complement Ther Nurs Midwifery. 2003;9(4):176–81. doi: 10.1016/S1353-6117(03)00045-3. [DOI] [PubMed] [Google Scholar]


