Abstract
Background
The double burden of communicable and noncommunicable diseases (NCD) is an increasing trend in low- and-middle income developing countries. Rural and minority populations are underserved and likely to be affected severely by these burdens. Knowledge among young people could provide immunity to such diseases within a community in the long term. In this study we aimed to assess the knowledge of several highly prevalent NCDs (diabetes, hypertension, and chronic obstructive pulmonary disease [COPD]) and several highly incident communicable diseases (malaria and diarrheal diseases) among Karen high school students in a rural district in far northwest of Thailand. The aim of the study is to explore information for devising life-course health education that will be strategically based in schools.
Method
A cross-sectional survey approved by the ethics committee of Boromarajonani College of Nursing Nakhon Lampang (BCNLP), Lampang, Thailand was conducted in Thasongyang, Tak province, from September 2011 to January 2012. Questionnaires for assessing knowledge regarding diabetes, hypertension, COPD, malaria, and diarrheal diseases were delivered to all 457 Karen high school students attending Thasongyang high school. A total of 371 students returned the questionnaires. Experts’ validation and split-half reliability assessment was applied to the instrument.
Results
Students’ main sources of health information were their teachers (62%), health care workers (60%), television (59%), and parents (54%). Familial risk factors of diabetes and hypertension were not known to more than two thirds of the students. Except obesity and physical inactivity, lifestyle-related risk factors were also not known to the students. Though living in a malaria-endemic area, many of the Karen students had poor knowledge about preventive behaviors. Half of the students could not give a correct answer about the malaria and hygienic practice, which might normally be traditionally relayed messages.
Conclusion
Health education and knowledge about common NCD and communicable diseases are yet to be prompted among the Karen students. A broader and more comprehensive school-based health education strategy for prevention of double burden diseases would benefit the rural minority population at the Thai-Myanmar border.
Keywords: double burden diseases, Thai-Myanmar border, health information, youth, minority, adolescents
Introduction
Ethnic minority groups are prone to health disparity and poor health education.1 The Karen people are an ethnic minority group living along the Thailand and Myanmar border.2 Recent studies in Thasongyang reported poor health education among the middle-aged and old-aged population regarding diabetes and hypertension.3–5
In low- and middle-income countries, the double burden of communicable diseases and noncommunicable diseases (NCDs) is trending upwards.6 Epidemiological transition occurs in such a setting, with the increasing burden of lifestyle-related diseases such as diabetes and hypertension presenting, in addition to the existing burden of infectious diseases such as malaria and diarrheal diseases. Thailand is one such country.7
Minority people are likely to be among those more severely affected because of language barriers, lack of power, and underrepresentation.8–10 Moreover, geographically remote and rural areas are likely to suffer from inequality in many aspects of health care need.11 Situated at the northwestern-most edge of Thailand and populated by a Karen ethnic population, Thasongyang, a rural district and the site of our current study, is a good example of such an area facing inequality.
Diabetes, hypertension, and chronic obstructive pulmonary disease (COPD) are top-ranked causes of morbidity and mortality in Thailand, despite the waning incidence of malaria and diarrheal diseases in recent years, in most urban settings.12–15 In the study site area, diabetes and hypertension are highly prevalent; moreover, malaria is still a high burden disease, as was the case decades ago.15,16 Locally reported data show that the incidence of diarrheal diseases is also very high.17 However, there is limited literature and few research studies on knowledge of such diseases among the Karen minority, particularly among the youth group.
Schools are where health education can be delivered to youth groups, together with educational packages;18 Life-course health education can be launched in schools as part of the curriculum. Thus, it would be beneficial to assess the knowledge that an ethnic minority’s high school students have about nationally and locally high-burden diseases.
In this study, we aimed to assess the knowledge of highly prevalent noncommunicable diseases (NCDs) (diabetes, hypertension, and COPD), as well as highly incident communicable diseases (malaria and diarrheal diseases) among high school students of Karen ethnicity, in a rural district in the northwestern-most edge of Thailand.
Materials and methods
The study was conducted in the Thasongyang district, in Thailand’s Tak province. The district borders Myanmar via the narrow Moei River. The areas along the Thai-Myanmar border are usually populated with Karen ethnic residents, as well as migrants with different immigration statuses.19
A cross-sectional study was conducted to survey the knowledge among Karen minority students who were attending high school in Thasongyang district. The study obtained the approval of the Boromarajonani College of Nursing, Nakhon Lampang (BCNLP)’s institutional review board, Thailand, and permission of the school. The study was conducted from September 2011 to January 2012.
The targeted population was approached directly because at the time of this study there was only one high school which provided high school education up to grade nine in Thasongyang, Since we wanted to assess the minority Karen high school students’ knowledge, we delivered the questionnaires to all 457 Karen students in grade 7 and 6 purposively. Five sets of paper-based knowledge assessment questionnaires underwent content validation by experts from BCNLP and split-half reliability assessment. Readability and comprehension of questions by the students were confirmed by schoolteachers in Thasongyang. Self-administered questionnaires were returned by the students.
Data was descriptively analyzed by applying STATA 11 (StataCorp LP, College Station, TX, USA). Reliability assessment used SPSS version 11.5 (IBM, Chicago, IL, USA). The reliability coefficients of each set of questions are shown under the knowledge assessment result table (Tables 2–6).
Table 2.
Diabetes knowledge of Karen high school students
| Correct answer
|
Incorrect answer
|
Response rate
|
||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Do you know diabetes? | 312 | 93.13* | 23 | 6.87 | 335 | 90.30 |
| Diabetes is a communicable disease. | 263 | 71.66 | 104 | 28.34 | 367 | 98.92 |
| Diabetes is a curative disease. | 105 | 28.69 | 261 | 71.31 | 366 | 98.65 |
| Elderly persons are more susceptible or more likely to have diabetes than adults. | 201 | 54.92 | 165 | 45.08 | 366 | 98.65 |
| If your blood-related relatives or family members have diabetes, you are also at risk of having diabetes. | 83 | 22.87 | 280 | 77.13 | 363 | 97.84 |
| Obese people are more at risk of diabetes than those who are not obese. | 299 | 81.69 | 67 | 18.31 | 366 | 98.65 |
| Regular exercisers are less likely to have diabetes than those who do not exercise. | 262 | 71.58 | 104 | 28.42 | 366 | 98.65 |
| Suspicious diabetes symptoms are frequent urination and frequent water drinking from thirst. | 188 | 51.51 | 177 | 48.49 | 365 | 98.38 |
| Obese children are at risk of diabetes. | 276 | 75.41 | 90 | 24.59 | 366 | 98.65 |
| Pregnant women are likely to have diabetes. | 67 | 18.36 | 296 | 81.64 | 363 | 97.84 |
| Numbness in one of the limbs is a sign of diabetes. | 130 | 36.01 | 231 | 63.99 | 361 | 97.30 |
| Diabetic people should take special care of their feet by wearing comfortable heel-covered shoes to prevent them from being wounded. | 154 | 42.08 | 212 | 57.92 | 366 | 98.65 |
| Wounds of diabetic people are not easy to heal and likely to get worse. | 196 | 53.41 | 171 | 46.59 | 367 | 98.92 |
| Blindness or kidney failure is a complication of untreated diabetes. | 170 | 46.45 | 196 | 53.55 | 366 | 98.65 |
| Normal level of blood sugar after 8-hour fasting is not more than 100 mg/dL. | 111 | 30.25 | 256 | 69.75 | 367 | 98.92 |
| People who regularly eat sweet, fried, and fatty food are at risk of having diabetes. | 267 | 72.95 | 99 | 27.05 | 366 | 98.65 |
Notes: Reliability coefficient = 0.763;
answer “yes”.
Table 6.
Diarrhea knowledge among Karen high school students
| Correct answer
|
Incorrect answer
|
Response rate
|
||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Do you know diarrhea? | 296 | 92.79* | 23 | 7.21 | 319 | 85.98 |
| Symptom of diarrhea is passing loose or watery stool. | 329 | 92.68 | 26 | 7.32 | 355 | 95.69 |
| Diarrhea is caused by eating unclean food. | 318 | 89.58 | 37 | 10.42 | 355 | 95.69 |
| Eating food landed on by flies can cause diarrhea. | 307 | 86.72 | 47 | 13.28 | 354 | 95.42 |
| Eating hot and cooked food can prevent diarrhea. | 240 | 67.80 | 114 | 32.2 | 354 | 95.42 |
| Using serving spoon when eating with others can prevent diarrhea. | 223 | 63.17 | 130 | 36.83 | 353 | 95.15 |
| Washing hands before eating can prevent diarrhea. | 281 | 79.38 | 73 | 20.62 | 354 | 95.42 |
| Washing hands without soap after going to the toilet is enough in preventing diarrhea. | 155 | 43.66 | 200 | 56.34 | 355 | 95.69 |
| Washing hands with soap before preparing food or cooking can prevent diarrhea. | 255 | 71.83 | 100 | 28.17 | 355 | 95.69 |
| Heating food that has been left unrefrigerated over night until boiling point before eating can prevent diarrhea. | 172 | 48.59 | 182 | 51.41 | 354 | 95.42 |
| One chopping board can be alternately used for raw meat and steamed chicken during cooking. | 138 | 38.98 | 216 | 61.02 | 354 | 95.42 |
| Older persons should avoid eating uncooked food to prevent diarrhea. | 217 | 61.47 | 136 | 38.53 | 353 | 95.15 |
| Adults can eat uncooked food without having diarrhea. | 178 | 50.42 | 175 | 49.58 | 353 | 95.15 |
| Using food cover to keep away cockroaches, flies, or mice can prevent diarrhea. | 246 | 69.30 | 109 | 30.7 | 355 | 95.69 |
| Drinking clean or boiled water can prevent diarrhea. | 269 | 75.77 | 86 | 24.23 | 355 | 95.69 |
| Using landfills for trash disposal can prevent diarrhea. | 72 | 20.34 | 282 | 79.66 | 354 | 95.42 |
| Diarrhea can be fatal. | 213 | 60.17 | 141 | 39.83 | 354 | 95.42 |
Notes: Reliability coefficient = 0.78;
answer “yes”.
Results
A total of 371 students filled and returned questionnaires. The response rate was 81%. Two-thirds of students were female. The average age was 17 years. Karen minority students attending four different levels of classes, from level one to level six, were included. Most of their family members’ occupations were farmers and day laborers. Half of the students’ family heads were uneducated. A complete characteristic of the sample is presented in Table 1.
Table 1.
Characteristic of the study sample
| Character | No | % | Response rate |
|---|---|---|---|
| Total | 371 | 100 | |
| Age (years) | 98.38 | ||
| Median (IQR) | 17 (16–18) | ||
| Sex | 99.73 | ||
| Male | 118 | 31.81 | |
| Female | 252 | 67.92 | |
| Class (IQR of age in years) | 99.73 | ||
| Grade 9 high school (15–15) | 77 | 20.75 | |
| Grade 10 high school (16–16) | 127 | 34.23 | |
| Grade 11 high school (17–17) | 84 | 22.64 | |
| Grade 12 high school (18–18) | 82 | 22.1 | |
| Occupation, (IQR of monthly income in Thai bhatt) | 100 | ||
| Farmer (1000–2000) | 179 | 48.25 | |
| Day Laborer (3000–4500) | 108 | 29.11 | |
| Other (3000–5000) | 40 | 10.78 | |
| Government service (8000–12000) | 36 | 9.7 | |
| Housekeeping (4500–5000) | 8 | 2.16 | |
| Education of family head | 98.92 | ||
| No schooling | 173 | 46.63 | |
| Primary school | 97 | 26.15 | |
| Secondary school | 27 | 7.28 | |
| High school | 48 | 15.94 | |
| Bachelor degree | 22 | 5.93 |
Abbreviation: IQR, interquartile range.
Teachers, health care workers, and televisions were the top-ranked source of health information reported by the respondents. Internet use was limited to 26%, and only 18% listened to the radio (see Figure 1).
Figure 1.
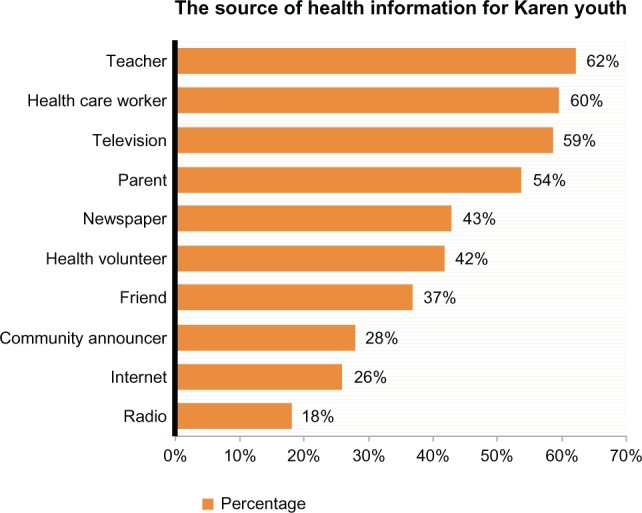
The source of health information for Karen youth.
Note: Categories are not mutually exclusive.
Diabetes
Most of the students in the study sample were familiar with diabetes (93%). About two-thirds of students knew it as an NCD, but only 28.69% realized that it was incurable. The risk factors of diabetes that were well known to students were obesity (81.69%), childhood obesity (75.41%), and lack of exercise (71.58%). Almost two-thirds of students answered that those who ate too much fatty food and sweets could have diabetes. However, 77.13% of the sample did not know that a family history of diabetes is a risk factor for diabetes, and half answered that diabetes was a disease more likely to occur in the elderly. Moreover, half of the students in the study sample had knowledge about well-known symptoms of diabetes such as thirst and frequent urination, and diabetes complications such as slow wound healing (53%), kidney damage (46%), and numbness of the feet (36%). However, seven out of ten students did not have any knowledge of normal blood sugar levels.
Hypertension
Most of the respondents knew hypertension, and two-thirds correctly recognized hypertension as an NCD and as a disease which is not curable. However, only one third of them knew about normal and high blood pressure levels. The risk factors of hypertension that are well-known to them were old age (72.63%) and obesity (83.52%). Lifestyle-related risk factors which were not known by students included smoking, which was not known by 64.74% of students, eating a high salt diet (63.54%), stress and strain (40%), drinking alcohol (40%), consuming large amounts of coffee and tea (58.68%), and lack of regular exercise (31.13%). Moreover, two-thirds of the students did not notice family history of hypertension as a risk factor.
COPD
The term COPD was known to only 66.67% of students, but most of them did not realize that COPD was an NCD (56.42%). Only one of five students recognized COPD as an incurable disease. Most of students identified smoking as a risk for COPD (70.42%), but just half answered environmental pollution and inhalation of dust (50.56%) as a risk factor for COPD, and more than one-third (39.61%) thought chewing tobacco might cause COPD. Shortness of breath was recognized as a feature of COPD; reduced functional status was also known to be a consequence of COPD to more than 50% of the students.
Malaria
Almost all respondents knew about malaria. More than two-thirds of students identified malaria as a mosquito-borne disease. Regarding preventive behavior, more than half knew to sleep under an insecticide-impregnated net and that wearing long sleeved shirts and trousers while working in the forest could prevent malaria. Moreover, more than two-thirds identified fever, chills, and headache as symptoms of malaria. A large percentage of students knew it could lead to life threatening disease (74%), but only half of them knew that it could not be treated by over-the-counter drugs (55.2%).
More than half of students answered that general well-being was a protective factor (53.3%); half of them answered that chemical insecticides would be effective to control mosquitoes. However, some were mistaken in their knowledge, answering incorrectly that malaria is a bacterial disease (32%); one-third also thought that malaria was caused by drinking creek water. A third of students also answered that a malaria mosquito would bite only at night.
Despite being familiar with diarrheal disease and its symptoms, only 60% of students realized that diarrhea can be fatal. More than 85% of the students recognized unclean food and fly-landed food as a cause of diarrhea, as well as recognizing hand-washing before meals and after toilet use as preventive practices. However, half of the students chose the option on the questionnaire of washing hands without soap after using the toilet.
Regarding food hygiene, almost two-thirds of students knew to eat freshly cooked food, and to keep food well-covered to avoid mice, flies, and cockroaches. However, half of the students thought that adults could eat uncooked food, without worry of diarrhea.
Discussion
In this study, we assessed Karen high school students’ knowledge of common and burdensome diseases, focusing on a rural setting in Thailand. Health knowledge will prevent adolescent students from establishing unhealthy behavior and risky lifestyles;20 thus, it will consequently contribute to preventing NCDs. Knowledge of malaria and diarrheal diseases will lead to preventive behavior and consequently reduce the transmission and burden of disease. Hence, the information explored by the current school-based survey may benefit the minority health by helping devise strategies and means of school-based health education.
Most of the respondents were from low-income and poorly educated families (Table 1). Most of them were informed by teachers, health care workers, television programs, and parents; traditionally held beliefs, common misbelief, and wrong beliefs may pass from parents to offspring. Based on Figure 1, class-, family- and television-based health education may reach the targeted population.
NCD
The survey findings showed that diabetes was known to more than 80% of students (Table 2). The majority of students also noticed lifestyle-related risk factors such as obesity and physical inactivity;21 some students even knew the complications of diabetes. However, the majority lacked any knowledge about blood glucose levels and did not know that genetic predisposition and family history are strong indicators of diabetes mellitus risk.21,22 A recent study in Thasongyang reported the risk of prediabetes among those with a family history of diabetes (adjusted odds ratio 4.6, 95% confidence interval 1.81–11.71) among the Karen adults.5 Therefore, it is necessary to educate high school students; among those with a family history of diabetes, the knowledge could help lead to a choice of healthy lifestyle and prevention of diabetes by simply alerting students that they are at risk of diabetes.22 Knowledgeable young adults may adopt healthy ways to eat, live, and avoid risky behaviors such as smoking, alcohol, and physical inactivity.
Likewise, the majority of students knew about hypertension. However, they did not know the exact limits of a healthy blood pressure. Many of them also did not know that family history can be an indication of hypertension risk (Table 3). Moreover, the lifestyle-related risk factors which were common to all cardiovascular diseases were not well known among the students. This situation necessitated health education lessons regarding hypertension and related cardiovascular diseases.
Table 3.
Hypertension knowledge of Karen high school students
| Correct answer
|
Incorrect answer
|
Response rate
|
||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Have you ever heard of the word “hypertension”? | 324 | 92.84* | 25 | 7.16 | 349 | 94.07 |
| Hypertension is a communicable disease. | 283 | 77.32 | 83 | 22.68 | 366 | 98.65 |
| Hypertension is a curative disease. | 68 | 18.73 | 295 | 81.27 | 363 | 97.84 |
| Elderly persons are more susceptible to hypertension than adults. | 268 | 73.63 | 96 | 26.37 | 364 | 98.11 |
| If your blood-related relatives or family members have hypertension, you are also at risk of hypertension. | 84 | 23.20 | 278 | 76.8 | 362 | 97.57 |
| Obese people are more at risk of hypertension than those who are not obese. | 304 | 83.52 | 60 | 16.48 | 364 | 98.11 |
| People with consistent stress and tension are at risk of hypertension. | 222 | 60.99 | 142 | 39.01 | 364 | 98.11 |
| Smoking increases risk for having hypertension. | 128 | 35.26 | 235 | 64.74 | 363 | 97.84 |
| Consuming salty food increases risk for having hypertension. | 132 | 36.46 | 230 | 63.54 | 362 | 97.57 |
| Common symptoms of hypertension are headache, dizziness, blurred vision, nausea, vomiting, and weakness of the limbs. | 197 | 54.42 | 165 | 45.58 | 362 | 97.57 |
| Regular exercisers are less likely to have hypertension than those who do not exercise | 250 | 68.87 | 113 | 31.13 | 363 | 97.84 |
| Alcohol drinkers are at risk of having hypertension. | 220 | 60.61 | 143 | 39.39 | 363 | 97.84 |
| Normal blood pressure is 120/80 mmHg. | 119 | 32.78 | 244 | 67.22 | 363 | 97.84 |
| Blood pressure of 140/90 mmHg is considered high. | 124 | 34.07 | 240 | 65.93 | 364 | 98.11 |
| Drinking coffee or tea is a risk factor for having hypertension. | 150 | 41.32 | 213 | 58.68 | 363 | 97.84 |
Notes: Reliability coefficient = 0.702;
answer “yes”.
Adolescence is the period of life when children develop their behaviors and habits.23 Health education delivered in the classroom would enable students to refuse tobacco, to refuse unhealthy diet choices such as salty food, and to adopt practicing regular physical exercise in the long run.
The number of deaths caused by COPD has increased globally, but it is still less well known to many people compared to other diseases;24,25 this was the case in our study, where COPD was less known to the Karen high school students than diabetes and hypertension. A recently reported smoking rate among Karen adults was as high as 70% among both male and female subjects, indicating a need for tobacco control intervention.4 Meanwhile, students’ knowledge about smoking as a risk factor for COPD was certainly high (67%), even though they did not know that COPD was a NCD (Table 4). Nonsmoking risk factors such as outdoor air pollution were also known to less than half of the students.26 A comprehensive and well introduced health education class regarding COPD is necessary for these adolescents. It might also lead to strong knowledge of the health risk caused by smoking and result in Karen youth groups avoiding tobacco use.
Table 4.
Chronic obstructive pulmonary diseases knowledge among Karen high school students
| Correct answer
|
Incorrect answer
|
Response rate
|
||||
|---|---|---|---|---|---|---|
| n | % | n | % | N | % | |
| Do you know COPD? | 220 | 66.67* | 110 | 33.33 | 330 | 88.95 |
| COPD is a communicable disease. | 156 | 43.58 | 202 | 56.42 | 358 | 96.50 |
| COPD is mostly caused by smoking. | 250 | 70.42 | 105 | 29.58 | 355 | 95.69 |
| COPD can be caused by inhaling dust for several years. | 180 | 50.56 | 176 | 49.44 | 356 | 95.96 |
| COPD can be cured. | 75 | 21.01 | 282 | 78.99 | 357 | 96.23 |
| COPD occurs mostly in elderly. | 148 | 41.46 | 209 | 58.54 | 357 | 96.23 |
| COPD can cause shortness of breath. | 209 | 58.87 | 146 | 41.13 | 355 | 95.69 |
| COPD can decrease individual’s ability to function. | 197 | 55.34 | 159 | 44.66 | 356 | 95.96 |
| COPD can be caused by cold weather. | 92 | 25.92 | 263 | 74.08 | 355 | 95.69 |
| People living in high altitude area are more likely to have COPD. | 62 | 17.42 | 294 | 82.58 | 356 | 95.96 |
| People consuming salty food are likely to have COPD. | 79 | 22.25 | 276 | 77.75 | 355 | 95.69 |
| Regular exercisers are less likely to have COPD. | 188 | 52.96 | 167 | 47.04 | 355 | 95.69 |
| Chewing tobacco or betel nuts can cause COPD. | 141 | 39.61 | 215 | 60.39 | 356 | 95.96 |
Notes: Reliability coefficient = 0.719;
answer “yes”.
Abbreviation: COPD, chronic obstructive pulmonary disease.
Communicable diseases
Thasongyang has been one of the districts with the highest malaria incidence in Thailand.16 Personal protection is one of the key elements in prevention of malaria, while vector control and human vector interface were less successfully controlled. The majority of the participants knew malaria and recognized it as a vector-borne disease caused by mosquito bites (Table 5). However, knowledge of personal protection was confined to not more than half of the sample. Moreover, many of them had wrong knowledge or held incorrect beliefs; for example, the belief that general wellbeing would prevent malaria, and that malaria was caused by drinking creek water. These could be traditional beliefs relayed by parents. Even though these students were residents of a malaria-endemic area, their knowledge on personal protective behavior was less than satisfactory. It is worth to educate these students with health informations.
Table 5.
Malaria knowledge among Karen high school students
| Correct answer
|
Incorrect answer
|
Response rate
|
||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Do you know malaria? | 320 | 96.10* | 13 | 3.9 | 333 | 89.76 |
| Malaria is caused by mosquito bite. | 260 | 73.03 | 96 | 26.97 | 356 | 95.96 |
| Drinking creek water in the forest can cause malaria. | 125 | 35.11 | 231 | 64.89 | 356 | 95.96 |
| Malaria-carrying mosquitoes normally bite at night. | 104 | 29.13 | 253 | 70.87 | 357 | 96.23 |
| Malaria-carrying mosquitoes breed only in clear and low flow creeks. | 142 | 39.89 | 214 | 60.11 | 356 | 95.96 |
| Malaria is caused by the bacteria. | 45 | 12.75 | 308 | 87.25 | 353 | 95.15 |
| People infected with malaria have high fever, chills, and headache. | 298 | 83.47 | 59 | 16.53 | 357 | 96.23 |
| There are several types of malaria but all are treated by the same kind of medicine. | 119 | 33.43 | 237 | 66.57 | 356 | 95.96 |
| Without treatment, malaria can be life threatening. | 277 | 77.59 | 80 | 22.41 | 357 | 96.23 |
| Malaria can be cured by over the counter medicine. | 204 | 57.30 | 152 | 42.7 | 356 | 95.96 |
| If you are sick from malaria you can stop taking medicine when you feel better. | 199 | 55.74 | 158 | 44.26 | 357 | 96.23 |
| Sleeping in mosquito net from twilight can protect from mosquito bites. | 280 | 78.43 | 77 | 21.57 | 357 | 96.23 |
| Spraying the room with chemical insecticide is effective in killing malaria-carrying mosquitoes. | 187 | 52.68 | 168 | 47.32 | 355 | 95.69 |
| Mosquito nets impregnated with insecticide can protect you from mosquito bites and can kill mosquitoes. | 235 | 66.01 | 121 | 33.99 | 356 | 95.96 |
| Wearing long-sleeved shirts and long trousers while working in the forest or the rice field can prevent malaria. | 233 | 65.27 | 124 | 34.73 | 357 | 96.23 |
| Healthy people are less likely to be sick from malaria. | 30 | 8.40 | 327 | 91.6 | 357 | 96.23 |
Notes: Reliability coefficient = 0.717;
answer “yes”.
Diarrheal diseases were leading causes of illness in the areas along the Thai-Myanmar border.17 Diarrhea is a hygiene-related disease and hand washing is a basic and critical personal behavior which can cut down on infections, prevent illness, and save lives.27 Three quarters of the students in the study knew to wash their hands before every meal and after using the toilet. However, half of them thought washing hands without soap after using the toilet was acceptable (Table 6).
Hygienic practices are influenced not only by acquired knowledge but also by the sanitation facilities in the local community and civil structures such as the municipal water supply system. In this study setting, most of the houses had a periodically accessible tap water supply. The use of sanitation facilities in Thailand has improved in the last decade.28 However, in rural areas, piped-into-premises coverage is only 31%.28 Many rural areas still rely on community water resources, which might lead to inconvenience if washing one’s hands with soap frequently. However a recent observational study in Bangladesh reported that washing hands with water alone, before preparing food, could reduce the incidence of diarrhea, given that both hands were washed; on the other hand, washing with water only and without soap after defecation could not significantly prevent diarrhea.29 Moreover, the responses relating to the food hygiene questions was poor. Some students thought adults could eat uncooked food; only six out of ten students answered that they needed to avoid uncooked food to prevent diarrhea. This response reveals the need for health education to improve the students’ knowledge of diarrhea prevention and hygienic practices.
Limitation
Because of access difficulties, we approached high school students directly and purposively sampled the Karen minority students. This approach might have an impact on the generalizability of this study, since there could be minority youths who did not have the opportunity to attend school. Likewise, difficult access did not allow us to run a test-retest reliability assessment of questionnaires. Nonetheless, the split-half assessment showed sound reliability indicators for the questionnaires.
Conclusion
Despite the limitations cited, this survey’s findings may provide a spotlight on the health knowledge of Karen youth along the rural Thai-Myanmar border area. We also identified the entry points for promoting students’ health education in the future. These might lead us to achieve our ultimate objective of finding ways to start life-course health education of ethnic minorities in rural communities.
Health inequalities and disparities in knowledge are common in minority populations.11 The current study’s findings clearly disclosed the need for promoting health knowledge among high school students of Karen ethnicity. Based on these findings, we recommend broader and more comprehensive health education in high schools classes to prevent the double burden of NCD and communicable diseases in minority populations.
Author contributions
TL and MNA were lead authors. TL designed the study. All authors contributed to the research process, data management and drafting. TL and PN developed the questionnaires. PJ translated the questionnaires into English and MNA edited those. MNA designed and performed analysis. TL, MNA and all authors interpreted the results. All authors have seen and confirmed the final draft and discussions written by MNA.
Acknowledgments
The authors acknowledged Saiyud Moolphate, Department of Tropical Hygeine, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand and Janthila Srikrajang, Department of Research and Community Engagement, BCNLP, Lampang, Thailand for their important suggestions for data analysis and data presentation.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Disease Burden and Risk Factors [webpage on the Internet] Atlanta: Centers for Disease Control and Prevention; 2007Available from: http://www.cdc.gov/omhd/amh/dbrf.htmAccessed February 18, 2013 [Google Scholar]
- 2.Rajah A.Remaining Karen: a Study of Cultural Reproduction and the Maintenance of Identity Canberra: ANU E Press; 2008Available from: http://www.burmalibrary.org/docs6/Remaining_Karen.pdfAccessed February 18, 2013 [Google Scholar]
- 3.Lorga T, Srithong K, Manokulanan P, Aung TNN, Aung MN. Public knowledge of diabetes in Karen Ethnic rural residents: a community-based questionnaires study in the far north-west of Thailand. Int J Gen Med. 2012;5:799–804. doi: 10.2147/IJGM.S33177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aung MN, Lorga T, Srikrajang J, et al. Assessing awareness and knowledge of hypertension in an at-risk population in the Karen ethnic rural community, Thasongyang, Thailand. Int J Gen Med. 2012;5:553–561. doi: 10.2147/IJGM.S29406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lorga T, Aung MN, Naunboonruang P, et al. Predicting prediabetes in a rural community: a survey among the Karen ethnic community, Thasongyang, Thailand. Int J Gen Med. 2012;5:219–225. doi: 10.2147/IJGM.S27876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bygbjerg IC. Double burden of noncommunicable and infectious diseases in developing countries. Science. 2012;337(6101):1499–1501. doi: 10.1126/science.1223466. [DOI] [PubMed] [Google Scholar]
- 7.Kaufman ND, Chasombat S, Tanomsingh S, Rajataramya B, Potempa K. Public health in Thailand: emerging focus on non-communicable diseases. Int J Health Plann Manage. 2011;26(3):e197–e212. doi: 10.1002/hpm.1078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Egede LE, Dagogo-Jack S. Epidemiology of type 2 diabetes: focus on ethnic minorities. Med Clin North Am. 2005 Sep;89(5):949–975. doi: 10.1016/j.mcna.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 9.Kurian AK, Cardarelli KM. Racial and ethnic differences in cardiovascular disease risk factors: a systematic review. Ethn Dis. 2007;17(1):143–152. [PubMed] [Google Scholar]
- 10.World Health Organization global atlas on cardiovascular disease prevention and control 2011http://www.who.int/cardiovascular_diseases/publications/atlas_cvd/en/index.htmlAccessed 04.04.2012
- 11.Thammatacharee N, Tisayaticom K, Suphanchaimat R, et al. Prevalence and profiles of unmet healthcare need in Thailand. BMC Public Health. 2012;12(1):923. doi: 10.1186/1471-2458-12-923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217–223. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 13.Tiptaradol S, Aekplakorn W. Prevalence, awareness, treatment and control of coexistence of diabetes and hypertension in Thai population. Int J Hypertens. 2012;2012:386453. doi: 10.1155/2012/386453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Malaria Report 2012: Country profiles: Thailand 2012 [webpage on the internet] Geneva: World Health Organization; 2010Available from: http://www.who.int/malaria/publications/country-profiles/profile_tha_en.pdfAccessed February 19, 2013 [Google Scholar]
- 15.Sriwattanapongse W, Prasitwattanaseree S, Khanabsakdi S. Mortality Rate due to Malaria in Thailand. Walailak Journal of Science and Technology (WJST) 2012;9(2):135–139. http://wjst.wu.ac.th/index.php/wjst/article/view/296 [Google Scholar]
- 16.Thimasarn K, Jatapadma S, Vijaykadga S, Sirichaisinthop J, Wongsrichanalai C. Epidemiology of malaria in Thailand. J Travel MEd. 1995;2(2):59–65. doi: 10.1111/j.1708-8305.1995.tb00627.x. [DOI] [PubMed] [Google Scholar]
- 17.International Organization for Migration Thailand Migration Report 2011 Geneva: IOM: International Organization for Migration; 2013Available from: http://publications.iom.int/bookstore/free/TMR_2011.pdfAccessed February 15, 2012 [Google Scholar]
- 18.World Health Organization School health and youth health pro motion 2013 http://www.who.int/school_youth_health/en/Accessed June 6, 20132013
- 19.2013 UNHCR country operations profile – Thailand [webpage on the internet] Geneva: United Nations High Commissioner for Refugees; 2012Available from: http://www.unhcr.org/pages/49e489646.htmlAccessed February 15, 2012 [Google Scholar]
- 20.Abelson PH. Great transitions. Science. 1995;270(5238):895. doi: 10.1126/science.270.5238.895. [DOI] [PubMed] [Google Scholar]
- 21.Aekplakorn W, Bunnag P, Woodward M, et al. A risk score for predicting incident diabetes in the Thai population. Diabetes Care. 2006;29(8):1872–1877. doi: 10.2337/dc05-2141. [DOI] [PubMed] [Google Scholar]
- 22.Alberti KG, Zimmet P, Shaw J. International Diabetes Federation: a consensus on type 2 diabetes prevention. Diabet Med. 2007;24(5):451–463. doi: 10.1111/j.1464-5491.2007.02157.x. [DOI] [PubMed] [Google Scholar]
- 23.Alderman EM, Rieder J, Cohen MI. The history of adolescent medicine. Pediatr Res. 2003;54(1):137–147. doi: 10.1203/01.PDR.0000069697.17980.7C. [DOI] [PubMed] [Google Scholar]
- 24.COPD predicted to be third leading cause of death in 2030 [webpage on the internet] Geneva: World Health Organiztion; 2008Available from: http://www.who.int/respiratory/copd/World_Health_Statistics_2008/en/index.htmlAccessed February 18, 2013 [Google Scholar]
- 25.Tan WC. Trends in chronic obstructive pulmonary disease in the Asia-Pacific regions. Curr Opin Pulm Med. 2011;17(2):56–61. doi: 10.1097/MCP.0b013e32834316cd. [DOI] [PubMed] [Google Scholar]
- 26.Mannino DM, Buist AS. Global burden of COPD: risk factors, prevalence, and future trends. Lancet. 2007;370(9589):765–773. doi: 10.1016/S0140-6736(07)61380-4. [DOI] [PubMed] [Google Scholar]
- 27.Centers for Disease Control and Prevention Handwashing: Clean hands save lives. [webpage on the internet] Atlanta: Centers for Disease Control and Prevention; 2013Available from: http://www.cdc.gov/handwashing/Accessed February 22, 2013 [Google Scholar]
- 28.WHO/UNICEF Joint Monitoring Programme (JMP) for Water Supply and Sanitation [webpage on the internet] Geneva: World Health Organization; 2010Available from: http://www.wssinfo.org/data-estimates/table/Accessed February 27, 2013 [Google Scholar]
- 29.Luby SP, Halder AK, Huda T, Unicomb L, Johnston RB. The effect of handwashing at recommended times with water alone and with soap on child diarrhea in rural Bangladesh: an observational study. PLoS Med. doi: 10.1371/journal.pmed.1001052. [Epub June 28, 2011] [DOI] [PMC free article] [PubMed] [Google Scholar]


