Abstract
The purpose of this paper is to illustrate the importance of using open source technologies and common standards for interoperability when implementing eHealth systems and illustrate this through case studies, where possible. The sources used to inform this paper draw from the implementation and evaluation of the eHealth Program in the context of the Millennium Villages Project (MVP). As the eHealth Team was tasked to deploy an eHealth architecture, the Millennium Villages Global-Network (MVG-Net), across all fourteen of the MVP sites in Sub-Saharan Africa, the team recognized the need for standards and uniformity but also realized that context would be an important factor. Therefore, the team decided to utilize open source solutions. The MVP implementation of MVG-Net provides a model for those looking to implement informatics solutions across disciplines and countries. Furthermore, there are valuable lessons learned that the eHealth community can benefit from. By sharing lessons learned and developing an accessible, open-source eHealth platform, we believe that we can more efficiently and rapidly achieve the health-related and collaborative Millennium Development Goals (MDGs).
Keywords: eHealth, interoperability, open source, health information technology, standards, Sub-Saharan Africa
Introduction
Background on the Millennium Villages Project
The Center for Global Health and Economic Development (CGHED) is a research unit at the Earth Institute at Columbia University. CGHED develops and coordinates the Earth Institute’s global health programs in low and middle-income countries, with an overall aim to enable and support countries to achieve the Millennium Development Goals (MDGs). CGHED houses the Millennium Villages Project (MVP) which is a community-led initiative that seeks to serve as a model to help and empower rural African communities out of extreme poverty and achieve the MDGs by 2015.
The MVP initiative is supported by a multi-disciplinary team of researchers at Columbia University. The Columbia International eHealth Laboratory (CIEL) links the Department of Biomedical Informatics at the College of Physicians and Surgeons, the Department of Epidemiology at the Mailman School of Public Health and the CGHED at the Earth Institute to help develop innovative electronic health (eHealth) solutions for use by MVP and others around the world. MVP also involves partnerships with Millennium Promise (a Non-Governmental Organization), the United Nations Office for Project Services (UNOPS) and the United Nations Development Programme (UNDP) to support operations and implementation of the program. The Millennium Villages constitute fourteen sites in ten Sub-Saharan African countries with populations of between 5,000 to 85,000 people each in Koraro, Ethiopia; Sauri, Kenya; Dertu, Kenya; Ruhiira, Uganda; Mayange, Rwanda; Mbola, Tanzania; Mwandama, Malawi; Gumulira, Malawi; Potou, Senegal; Tiby, Mali; Toya, Mali; Bonsaaso, Ghana; Pampaida, Nigeria; and Ikaram, Nigeria. MVP interventions are centered on five sectors: agriculture, health, education, enterprise and infrastructure with a strong focus on empowerment of women and girls.
The eHealth Program
To support increased access to health services and information and to improve the quality of care, a broad range of information and communication technology (ICT) systems have been designed, tested, deployed and evaluated as part of the Electronic Health (eHealth) Program within MVP. Systems and initiatives that have been deployed include: 1) the Millennium Villages Global-Network (MVG-Net)—which includes ChildCount+, ODK Clinic, OpenMRS and other applications, 2) an upgrade of network connectivity in MVP sites through a partnership with Ericsson, 3) provision of mobile handsets for all health workers in the fourteen MVP sites through a partnership with Sony Ericsson, 4) the provision of SIM cards for health workers to create a closed user group and 5) the creation of a toll-free emergency lines and toll-free SMS numbers for ChildCount+ and other RapidSMS-based applications through partnerships with AirTel Bharti, MTN, and other mobile operators (Kanter, Negin, et al., 2009; ChildCount+; Open Data Kit; OpenMRS).
To facilitate collaboration across the different countries, languages and governmental systems, the MVP eHealth architecture has been built using a free/libre open source software for health care (FLOSS-HC) platform and has focused on the use of open and international standards, where possible. Open source is a description of both software and the process for using and modifying the software (providing free access to source code and allows for the sense of local “ownership” by developers and programs that use it (see Table 1)). The process of implementing MVG-Net across the MVP sites has highlighted numerous lessons learnt that will be invaluable to health information technology as it relates to implementation and the exchange of information across regions and nations (Kanter, Dick, et al., 2009). Therefore, the purpose of this paper is to illustrate the importance of using open source technologies and common standards for interoperability in the context of an international eHealth project.
Table 1.
The Open Source Definition (Open Source Initiative)
| 1. Free Redistribution |
| The license shall not restrict any party from selling or giving away the software as a component of an aggregate software distribution containing programs from several different sources. The license shall not require a royalty or other fee for such sale. |
| 2. Source Code |
| The program must include source code, and must allow distribution in source code as well as compiled form. Where some form of a product is not distributed with source code, there must be a well-publicized means of obtaining the source code for no more than a reasonable reproduction cost preferably, downloading via the Internet without charge. The source code must be the preferred form in which a programmer would modify the program. Deliberately obfuscated source code is not allowed. Intermediate forms such as the output of a preprocessor or translator are not allowed. |
| 3. Derived Works |
| The license must allow modifications and derived works, and must allow them to be distributed under the same terms as the license of the original software. |
| 4. Integrity of The Author’s Source Code |
| The license may restrict source-code from being distributed in modified form only if the license allows the distribution of “patch files” with the source code for the purpose of modifying the program at build time. The license must explicitly permit distribution of software built from modified source code. The license may require derived works to carry a different name or version number from the original software. |
| 5. No Discrimination Against Persons or Groups |
| The license must not discriminate against any person or group of persons. |
| 6. No Discrimination Against Fields of Endeavor |
| The license must not restrict anyone from making use of the program in a specific field of endeavor. For example, it may not restrict the program from being used in a business, or from being used for genetic research. |
| 7. Distribution of License |
| The rights attached to the program must apply to all to whom the program is redistributed without the need for execution of an additional license by those parties. |
| 8. License Must Not Be Specific to a Product |
| The rights attached to the program must not depend on the program’s being part of a particular software distribution. If the program is extracted from that distribution and used or distributed within the terms of the program’s license, all parties to whom the program is redistributed should have the same rights as those that are granted in conjunction with the original software distribution. |
| 9. License Must Not Restrict Other Software |
| The license must not place restrictions on other software that is distributed along with the licensed software. For example, the license must not insist that all other programs distributed on the same medium must be open-source software. |
| 10. License Must Be Technology-Neutral |
| No provision of the license may be predicated on any individual technology or style of interface. |
Approach
The sources used to inform this paper draw from the implementation and evaluation of the eHealth Program in the context of the MVP. In order to facilitate collaboration across the different countries, languages, and governmental systems, an eHealth architecture was developed—MVG-Net. MVP took advantage of a process based on an enterprise architecture to show interrelationships between country-specific and more global requirements for information systems and between architectures and solutions (as shown in Figure 1). This was based on work by David Lubinski that describes how country-specific requirements and existing solutions can inform a more generalizable architecture which can then lead to common platforms and tools, which then lead to country-specific technology solutions (Stansfield et al., 2008). Open source tools allowed us full control over the process and permitted iterations on local requirements, creation of the general MVG-Net architecture, and then local adaptation and country specific implementations.
Figure 1.
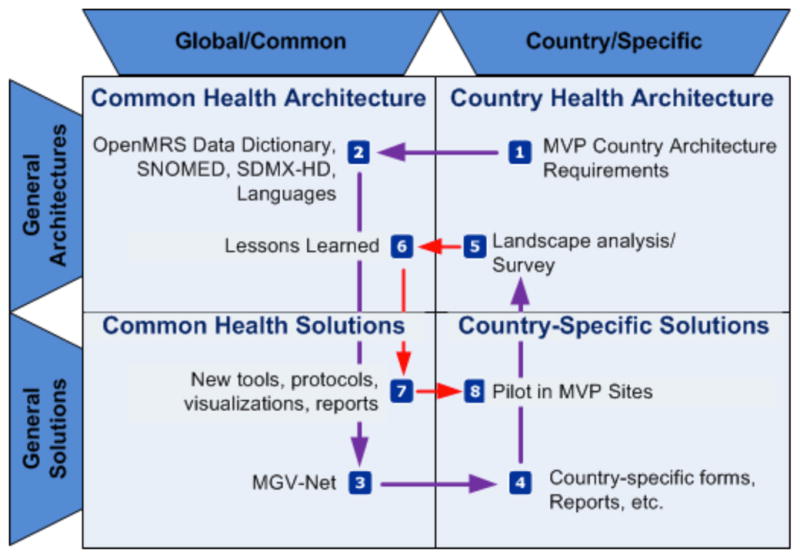
Enterprise architecture model (adapted from Stansfield et al. 2008)
Components of MVG-Net
MVG-Net (see Figure 2) has been deployed across all fourteen MVP sites. The architecture is based on open source platforms. Open source platforms were preferred over proprietary products due to cost and customization. Compared to proprietary products, open source products require no license fees, can be tailored to fit the needs of the project, and have support from the development community contributing to and using the particular product. However, as with any technology—whether open source or proprietary—maintenance costs still must be considered. The following are currently components of MVG-Net: Open Medical Record System (OpenMRS), RapidSMS (ChildCount+) and Open Data Kit (ODK) for Android™ (mClinic). We are also in the process of integrating two other open source technologies: District Health Information System (DHIS2) and CommCare. MVG-Net takes advantage of an open source database (MySQL), interface terminology, a centralized concept dictionary (mapped to standard reference terminologies), and appropriate local technology for data entry.
Figure 2.
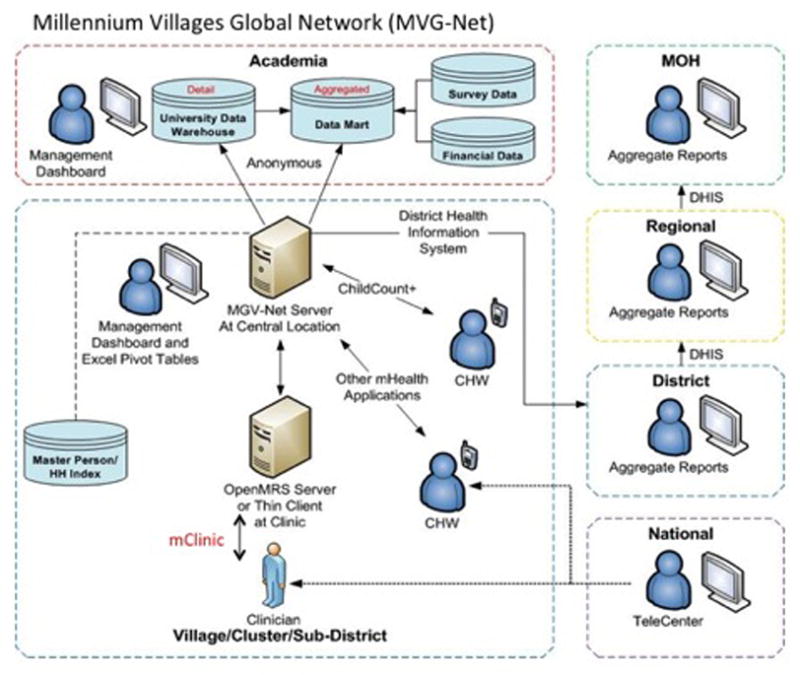
Millennium Villages Global Network (MVG-Net)
OpenMRS
OpenMRS is the core of MVG-Net. It is an open source, web-based electronic medical record platform that functions as the local hub of health information collected from different sources within the Millennium Villages. It has an easily extensible data model, and can aggregate individual, person-level data collected from Community Health Workers (CHWs) as well as clinic-based personnel. In MVP, the platform has been used to automate reports for the Millennium Villages Information System (MVIS) and various Ministries of Health. Currently, OpenMRS has been deployed within each MVP site to serve as the central database. It is also used to support facility-level data collection in several MVP sites where users enter and access the information from desktop computers. There is a substantial OpenMRS developer/implementer community that provides support via listserves, forums, Internet relay chat (IRC) chat rooms and in-person annual meetings (Seebregts et al., 2009). OpenMRS is has been downloaded in nearly 50 countries, is actively deployed around the globe, and is part of national scale-up projects in Rwanda and elsewhere. (OpenMRS)
ChildCount+
ChildCount+ is an SMS-based mobile phone-based CHW point of care support and data collection tool built on the RapidSMS platform (RapidSMS). It is aimed at improving the health outcomes of pregnant women, newborns and children under 5 years of age through ‘real-time’ data collection of household level data to trigger alerts, reminders and health promotion messages via CHWs. The system also enables performance monitoring for more effective supervision and management of community-based health. For example, in Mayange, CHWs receive SMS notifications to conduct follow-up visits and to remind women and children in their catchment area of upcoming clinic visits.
Open Data Kit
In the context of MVP, Open Data Kit (ODK) is currently being used for collecting data on vital events (verbal autopsy) and immunization histories of children. ODK is an open source Android™-based application that renders standard forms (Xforms) on mobile devices such as smart phones and tablets. MVP uses ODK to collect data from household interviews done in the collection of verbal autopsy information for each child and maternal death occurring within an MVP site. This information is then used to inform monthly or quarterly morbidity and morality reviews and resulting action of the health team and community to address any pressing concerns (Ohemeng-Dapaah et. al, 2010). Additionally, another ODK tool, mClinic, has been developed to provide a mobile interface to link to OpenMRS. mClinic enables nurses, midwives and other facility-based staff to be able to enter and access electronic patient information and receive clinical decision support at the point-of-care. mClinic provides a mechanism for streamlining data collection for monitoring and reporting and is being used in Tanzania to collect immunization information for children under 2 years old.
Databases
OpenMRS is built on the open source MySQL database. This allows local MVP staff (and other stakeholders) secure, but non-proprietary access to the data collected by MVG-Net. The data can be reported on using any SQL-compliant toolkit. Non-proprietary databases are important for allowing application owners flexibility to update their data collection tools, or move the data whenever necessary.
Interface Terminology Mapped to Reference Terminologies
One major obstacle to adoption of health information technology is the inability of users to locate and enter information using internationally accepted clinical terminology (Kanter et al., 2007), given their familiarity and use of locally accepted clinical terminology. To address this issue within MVP, content has been translated from English into Kinyarwanda in Rwanda; Swahili in Kenya and Tanzania; French in Mali, Senegal and Rwanda and Tigrinya in Ethiopia. Additional localization is occurring on an ongoing basis. The data elements are represented in the languages required at the interface using a multilingual standardized interface terminology mapped to international medical reference standards. By this means the data may be entered and viewed in multiple languages and it is translatable between them. The reference standards (ICD-10, SNOMED CT, RxNORM, LOINC, CVX) allow MVP to report to international agencies, compare between MVP sites, as well as compare with other organizations working in the same domains.
Centralized Concept Dictionary
Data collected across multiple different organizations, countries and languages is rarely interpretable due to differences in design and modeling of the information. OpenMRS ensures that data elements are semantically understood by mapping most elements using a concept dictionary (OpenMRS Concept Dictionary). In MVP, data compatibility is achieved via standardization and mapping at the data element level. The concept dictionary is shared across all users and acts as a central repository for the definitions of all the data collected. CIEL is responsible for maintaining the dictionary that is currently used by over 32 different organizations in as many different countries. The CIEL dictionary includes enhancements to ensure applicability in the context of primary health care across Sub-Saharan Africa. Modifications can be made through the development of site-specific subsets and requests made by the OpenMRS community for new concepts to be added to the platform.
Local Technology for Data Entry
As described above, OpenMRS functions as a central hub for person-level information within the MVP sites. MVP then takes advantage of different data collection tools depending on the requirements of the users and the infrastructure in the sites. Data entry is captured both at the point-of-care, through ChildCount+ (standard cell phones using SMS), mClinic/ODK (smartphones using Android™) and workstations using the web-based OpenMRS XForm interface, and retrospectively by entering data collected on paper forms using the Microsoft Infopath™ application into OpenMRS.
Findings
As noted by Chan et al., “standards in data collection and reporting increase efficiency and encourage collaboration within and between organizations” (Chan et al., 1999). The eHealth Team recognized the need for standards and uniformity but also realized that context would be an important factor. Therefore, the team decided to utilize open source solutions. This next section will outline, in depth, the decisions and outcomes of setting up the open source eHealth Architecture in MVP.
Making the Decision to Go Open Source
As described above, there are many reasons to favor open source over proprietary software solutions. This includes cost, flexibility, ownership, and the benefit of a large passionate, and involved developer and implementer community (Karopka et al., 2011). However, there are tradeoffs that have to be taken into account:
-
Resources
Although FLOSS applications do not require licensing fees, they do often require higher levels of developer support. Service and support may be available for free for FLOSS applications from a volunteer community, but organizations frequently must build in such support if they want to ensure reliable availability of assistance. MVP has implemented a structure which includes separate, development team and support staff. The team of three developers responds to new development requests and maintenance issues. The implementation and operation of MVG-Net is supported by an eHealth Specialist in each country. The eHealth Specialists do not develop any of the software but do help to localize and ensure that the applications are in good working order. They also assist the MVP Health Team in acquiring the data and analyzing the results generated by the tools.
-
Innovation and Collaboration
FLOSS promotes collaboration through the reuse of code that translates to time and money savings for clients. The resultant culture of sharing and proper attribution promotes open innovation. MVP partners with other FLOSS organizations such as Dimagi in the US, Jembi Health Systems in South Africa, Mindflow in Kenya and Baobab Health in Malawi.
-
Transparency
FLOSS applications are not developed as a “black box” meaning that organizations can see and modify code as necessary to ensure that it serves their purposes.
-
Independence
FLOSS avoids vendor lock-in, reducing the risk of negative unilateral actions by the software provider.
FLOSS offers freedom by allowing applications to be adapted and modified locally.
-
Localization/Customization
FLOSS applications provide a significant advantage in flexibility when customizing or localizing the software for use in the different settings. In particular, many proprietary health care software solutions are designed for resource-available environments and not for resource-limited ones.
Localization also promotes and builds development capacity in the local software industry. This capacity is critical for ongoing support and customization which will be required over time. Since a greater proportion of the resources stay in the country, the sustainability of local support is also improved.
-
Types of technologies, infrastructure
The OpenMRS platform was chosen for MVP due to its extensible data base design and central concept dictionary. This was a key factor in being able to provide sufficient flexibility to address each country’s local data collection requirements, while still being capable of maintaining the database over time and retaining semantic interoperability of the data elements.
Mobile devices played a key role in overcoming the limitations of power and computer connectivity in the field. Having several different mobile solutions all linked into a central information system allowed MVP to take advantage of different infrastructure and user contexts. These mobile solutions include the use of basic/feature phones by CHWs during their household visits and the use of smartphones for verbal autopsies and point-of-care support in the clinics.
-
Lessons learned
Developing and deploying software solutions maintained by a single organization is resource intensive and risky. Developing tools based on a common platform developed by partnering organizations allows the sharing of development (and required resources) and reduces the reliance on individual software engineers. The loss of a key developer in any software project represents a large potential risk to the ongoing sustainability of that system, especially if it is being maintained by a single or small set of organizations. Working with partners in a collaborative manner to create the underlying platform in which tools are built helps greatly to reduce risk and costs.
Implementation and Evaluation
MVP implemented various components of MVG-Net in different sites during the pilot phase. Rapid rollout to the whole MVP network put significant strain on the team and prevented more rapid iteration of releases that would have increased acceptability of the applications. MVP has focused on four sites for a mixed methods evaluation under the Open Architectures, Standards and Information Systems for Healthcare in Africa project (OASIS II), funded by the International Development Research Centre (IDRC) in Canada. OASIS II specifically evaluates the impact of MVG-Net on qualitative and quantitative outcomes in the Millennium Village sites. The results of OASIS II should be available by mid-2012 (OASIS II-IDRC).
-
Lessons learned
It is important to fine tune applications and solutions in a few sites then implement, or implement in stepwise fashion.
It is imperative to have adequate human resources (programmers, support staff, etc.).
It is not easy to set up a bridge between two information systems, and interoperability as well as resources are required.
Having development teams in multiple locations is very difficult. Do not overly mix software development with implementation support.
Cost-benefit analyses should be incorporated into evaluations. While keeping track of expenses is useful, it does not fully capture the potential costs or savings that result from implementation and use of eHealth tools within a health system. Where possible, work should be done with an health economist to incorporate such analyses into a monitoring and evaluation framework for eHealth projects.
Practical Implications
When using an open source model there are many factors that must be taken into consideration. This includes the types of applications used, how many organizations are involved, and buy-in and capacity of stakeholders and end-users to adopt the tools for their use.
With a large project like MVP, there will be many different applications used for multiple purposes, both programmatic and organizational. There is not always an open source application available for each use case, so the advantages and disadvantages of proprietary versus open source must be considered when selecting the appropriate software for each situation. In this case, an advantage for MVP is that it is a large multi-disciplinary project, but under one organizational structure. Though MVP has partners in many areas, all operational matters are unified so interoperability is easier to enforce than may be true in other organizations/projects attempting similar initiatives. The MVP eHealth team consists of several different project groups working in multiple countries under the larger heading of MVP. This means that using a common set of indicators and a centralized concept dictionary required considerable communication and coordination between the project teams.
In terms of external stakeholders, there is another set of factors to consider. Traditionally, governments provide paper books/forms to be used by health care givers at the point of care which are thereafter summarized to generate monthly reports to the relevant Ministry of Health (MoH). There is limited implementation of eHealth Care platforms by governments and very few have standards for setting up such platforms. Because of the absence of standards, many projects have come up implementing health management information systems (HMIS) in silos with limited consideration on interoperability. With limited HMIS implementations in the countries with MVP sites, it means that there is limited technical support at implementation sites. The use of FLOSS-HC with community support under the MVG-net has leveraged on the community support to address technical issues that would otherwise not be possible to solve.
Overall, the MVP implementations provide a model and valuable lessons learned for those looking to implement informatics solutions across disciplines and countries due to the range of topics covered and the geographical and situational diversity in which these solutions are applied.
Social Implications
The MVP implementation of MVG-Net using FLOSS-HC applications and common standards provides for widespread interoperability of health information systems within and between countries, regardless of their technological and economic environments. This not only reduces the cost of designing and implementation of the systems, but the ability to share data and lessons learned between organizations and countries should allow for more rapid, evidence-based decision-making and program planning. Sharing what works and what does not work between countries and projects will allow us to be more efficient and more rapidly reach the goals of achieving the MDGs by 2015.
Originality/Value of Paper
The process has highlighted numerous lessons learned that will be invaluable to health information technology as it relates to implementation and the exchange of information across regions and nations.
Acknowledgments
The authors wish to acknowledge the contributions of in each of the Millennium Villages Project sites. In particular, we would like to thank the eHealth specialists, without whose support, MVG-Net would not have been possible: In Ghana, Seth Ohemeng-Dapaah; in Nigeria, Innocent Olamiposi, in Tanzania, Killian Mahembe and Athanas Alois; in Rwanda, Benjamin Rukundo and Teddy Kaberuka; in Kenya, Dickson U’kanga and in Uganda, Emmanuel Toko and Henry Corrigan-Gibbs. This work has been funded by the generous support of the Rockefeller Foundation, the International Development Research Centre and the Novartis Fund for Sustainable Development.
Contributor Information
Andrew S. Kanter, Email: Andrew.kanter@dbmi.columbia.edu, Director of Health Information Systems/Medical Informatics, Millennium Villages Project, Earth Institute at Columbia University; Assistant Professor of Clinical Biomedical Informatics, College of Physicians and Surgeons, Columbia University; Clinical Epidemiology, Mailman School of Public Health, Columbia University; 622 W. 168th Street, VC5, New York, NY, USA 10032; Tel: +1.212.305.4842
Rob Borland, Email: rborland.mvp@gmail.com, Development Coordinator, eHealth Program, Millennium Villages Project, Earth Institute at Columbia University c/o The Millennium Villages Project, 475 Riverside Drive, Suite 401, New York, NY, USA 10115; Tel: +263.712.347.911.
Mourice Barasa, Email: barazam@gmail.com, Regional eHealth Specialist, Millennium Villages Project, Earth Institute at Columbia University, c/o The Millennium Villages Project, 475 Riverside Drive, Suite 401, New York, NY, USA 10115; Tel: +254.722.853.117.
Casey Iiams-Hauser, Email: ciiamshauser@ei.columbia.edu, eHealth Solutions Coordinator, eHealth Program, Millennium Villages Project, Earth Institute at Columbia University; MDG Centre West & Central Africa, BP 320, Hyppodrome Rue 287, Porte 341, Bamako, Mali; Tel: +223.20.219.133.
Olivia Velez, Email: ov2111@columbia.edu, Postdoctoral Research Fellow, Department of Biomedical Informatics, College of Physicians and Surgeons, Columbia University; 622 W. 168thStreet, VC5, New York, NY, USA 10032; Tel: +1.646.685.7351.
Nadi Nina Kaonga, Email: nnk2108@columbia.edu, Research and Evaluation Coordinator, eHealth Program, Millennium Villages Project, Earth Institute at Columbia University; 475 Riverside Drive, Suite 401, New York, NY, USA 10115; Tel: +1.603.969.4883.
Matt Berg, Email: mlb2178@columbia.edu, Director of Emerging Applications, Modi Research Group, Columbia University; 134F SW Mudd, MC: 4703, New York, NY, USA 10027; Tel: +1.212.854.3239.
References
- Chan W, Centiu C, Morris J. Uniform Data Standards for Capturing Patient Medical Record Information at the Point of Care. Journal of Healthcare Information Management. 1999;13(3):85–95. [PubMed] [Google Scholar]
- [accessed 11/10/2011];ChildCount+: Every Child Counts. from http://www.childcount.org/
- Kanter A, Dick J, Bukachi F, Johnson E, Borland C, Dusabe S, et al. Update on the Millennium Global Village-Net: Status and Lessons Learned. HELINA 2009, Abidjan, Cote d’Ivoire. Paper presented at the HELINA; Abidjan, Cote d’Ivoire. 2009. [Google Scholar]
- Kanter A, Negin J, Olayo B, Bukachi F, Johnson E, Sachs S. Millennium Global Village-Net: Bringing together Millennium Villages throughout sub-Saharan Africa. International Journal of Medical Informatics. 2009;78(12):802–807. doi: 10.1016/j.ijmedinf.2009.08.002. [DOI] [PubMed] [Google Scholar]
- Kanter A, Wang A, Naeymi-Rad F, Safran C. Interface Terminologies Bridge the Gap between Theory and Reality for Africa. Paper presented at the HELINA; 2007. [PubMed] [Google Scholar]
- Karopka T, Schmuhl H, Marcelo A, Molin J, Wright G. Towards Open Collaborative Health Informatics - The Role of Free/Libre Open Source Principles. Yearbook of Medical Informatics. 2011;6(1):63–72. [PubMed] [Google Scholar]
- OASIS II-IDRC. [accessed 11/10/2011]; From http://web.idrc.ca/es/ev-151413-201-1-DO_TOPIC.html.
- Ohemeng-Dapaah S, Pronyk P, Akosah E, Nemser B, Kanter A. Combining Vital Events Registration, Verbal Autopsy and Electronic Medical Records in Rural Ghana for Improved Health Services Delivery. Paper presented at the MedINFO; 2010; Cape Town, South Africa. 2010. [PubMed] [Google Scholar]
- [accessed 11/10/2011];Open Data Kit: Magnifying human resources through technology. from http://www.opendatakit.org.
- OpenMRS. [accessed 11/10/2011]; from http://www.openmrs.org.
- OpenMRS. [accessed 11/10/2011];Concept Dictionary. from https://wiki.openmrs.org/display/docs/Concept+Dictionary.
- Open Source Initiative. [accessed 11/10/2011];The Open Source Definition. from http://opensource.org/docs/osd.
- RapidSMS. [accessed 11/10/2011]; from http://www.rapidsms.org.
- Seebregts C, Mamlin B, Biondich P, Fraser H, Wolfe B, Jazaveri D, et al. The OpenMRS Implementers Network. International Journal of Medical Informatics. 2009 doi: 10.1016/j.ijmedinf.2008.09.005. [DOI] [PubMed] [Google Scholar]
- Stansfield SN, Orobaton N, Lubinski D, Uggowitzer S, Mwanyika H. The Case for a National Health information System Architecture; a Missing Link to Guiding National Development and Implementation. 2008 from http://www.who.int/healthmetrics/tools/1HMN_Architecture_for_National_HIS_20080620.pdf.


