Abstract
Today’s most basic and important total knee replacement design concepts arose out of an earlier era in which 2 distinct approaches emerged, functional and anatomic. Functional approaches simplified knee kinetics, were easier to implant, and gained widespread popularity, in part, from their inventory control. Anatomic approaches were an attempt to recreate normal knee motion with low prosthetic contact stress. Historically, however, they became impractical to produce because of the cost of maintaining a wide variety of anatomic knee implants. New customized designs may return the anatomic design to favor due to several key features that borrow anatomic principles developed in the past, and improved with new ideas.
Keywords: Total knee, Anatomic, Functional, Customized, Design
Introduction
Current condylar total knee replacements (TKR) are based on design principles originally developed in the late 1960s and early 1970s. During this period, a robust and rapid evolution in design occurred. Generally, 2 different approaches emerged: an anatomic and a functional approach. Either, at any one time, might entail retaining both cruciate ligaments, solely the posterior cruciate ligament, or complete cruciate recession.
The first functional condylar design concepts were taken from Frank Gunston’s unicompartmental knee arthroplasty. Two femoral condylar components, one each for medial and lateral condyles, were connected with a bar at the level of the femoral notch without resurfacing the femoropatellar joint [1]. This first condylar knee, named the Duocondylar, was developed at the Hospital of Special Surgery (HSS) by Peter Walker PhD, John Insall MD, Chitranjan Ranawat MD, and Alan Inglis MD in 1970, and first implanted in 1971 by Ranawat. Both cruciates were retained and there were separate medial and lateral tibial trays. It quickly became evident that it was extremely difficult to balance the knee correctly with intact cruciate ligaments, 2 different tibial trays, and a non-resurfaced femoropatellar joint. These reconstructions were performed free-hand without any specific instrumentation.
The HSS group made significant changes to their design, including 2 symmetric condyles mimicking the individual condylar J-curves, replacement of the femoropatellar joint and resection implant in 1974 by John Insall at HSS. The femoral condylar convexity was matched with a double dished tibial geometry providing sagittal and transverse stability by virtue of the so called “uphill” principle [2]. Joint laxity as a criterion for the design of condylar knee prosthesis was used to provide sufficient contact area and to minimize polyethylene stress. The slightly larger radii of the tibial concavity provided enough stability, but not too much constraint. To decrease the risk of tibial loosening, a single piece tibial tray with a centered peg was later added for better cement fixation [3]. John Insall’s surgical technique of cutting the distal femur and proximal tibia and placing the components perpendicular to their respective mechanical axes was based on conversations he had with his friend, Michael Freeman, MD [4•]. Freeman worked at the London Hospital, UK where he developed the Freeman-Samuelson knee, first implanted in 1968. Insall implanted the first total condylar (TC) knee at HSS 6 years later. Ranawat and Insall differed in their total knee designs. Ranawat would evolve the TC design into the cruciate substituting versions of the PS Press Fit Condylar design (PFC) and later the PS PFC Sigma and a PS rotating platform version. John Insall, however, worked with Al Burstein to improve the PS cam post design, independent of Peter Walker, which evolved into the Insall-Burstein modular PS knee I and II (Zimmer, Warsaw, IN), Optetrak PS (Exactec, Gainesville, FL) and the Advance PS knee (Wright Medical, Arlington, TN). While Peter Walker’s PS design was based on maintaining a more posterior contact point of the condyles on the tibial tray with increased flexion, Al Burstein developed a cam post mechanism, which allowed progressive rollback with flexion replacing the function of the PCL. Walker’s PS designs would later become the PS version of the Kinematic knee (Howmedica) and later into the Kinematic II, Kinemax and Kinemax Plus Knees (Howmedica). Other functional approaches include the work by Averill and Khowayla with Howmedica (Geomedic, Geometric II). Nas Eftekar was the first to implant a non-condylar knee with a metal backed modular total knee in 1969. Later, the design was changed and the knee became a condylar design [1], called Mark II [4•]. David Murray introduced polyethylene modularity in 1974 [5]. Fred Buechel and Michael Pappas introduced, with their LCS bicruciate-retaining knee replacement, 2 meniscal bearings. The bearings were not designed unlike the custom individual iTotal to inversely match the distal femoral offset, but for the purpose of reduced wear, similar to Goodfellow mobile bearing Oxford UKA [6]. Anatomic approaches, with retention of both of the cruciate ligaments, trace their origin to 1968, which was the same year Freeman implanted the first functional knee. In Japan, the Kodama-Yamamoto knee was implanted with a minimally constrained single piece, uncemented polyethylene insert preserving both cruciate ligaments [7].
Bahha Seedom PhD, a friend of Peter Walker, worked in Leeds and designed the anatomic Leeds knee. It featured a 2–4 mm femoral shell cast with asymmetric condyles, eliminated the meniscal indentation, and had an anatomic trochlea. In addition, the all-polyethylene tibial tray was asymmetric with preservation of both cruciate ligaments. The knee was first implanted in 1972, but it never received wide market adoption. The concept of asymmetric condyles without the lateral meniscal indentation would later emerge in anatomic designs such as the Cloutier knee (Zimmer, Warsaw, IN).
Charles Townley elucidated several key principles for anatomic knee implant design: a polyethylene insert as thin as possible, a femoral component that should resurface and duplicate the normal polycentric femoral curvature, including a trochlear flange, and a tibial component that allowed rotary and anteroposterior gliding motion on the tibial surface. Furthermore, Townley designed implants to be placed anatomically with accurate sizing to preserve ligament tension, and the anatomic varus-valgus alignment of the joint in the long axis of the extremity in the coronal and sagittal axis restored [8]. Townley’s knee was manufactured by Depuy, and came in 3 sizes. The first knee was implanted in 1972. However, in order to reduce inventory and cost, the anatomic asymmetric condyles and asymmetric patellar flanges were dropped in the final design. The surgical technique focused on accurate alignment and ligament tension to minimize shear and tensile stresses [8]. Contrary to other shell cast implants, such as the Leeds and Ewald knee, he used a saw for the femoral chamfer cut design. Townley also believed that bicruciate retention was a key component to minimize abnormal motion and stress.
Townley reported his 11 year results summarizing 532 knees in 426 patients using a bicruciate retaining implant for degenerative arthritis in 73 %, rheumatoid arthritis in 18 %, and revision arthroplasty in 9 %. Overall, he reported excellent or good results in 89 %, fair in 7 %, and poor or failed in 4 %. Excellent or good results were determined by a range of motion greater than 90 degrees, pain and activity restriction limited to mild or none, and no use of a walking aid [9].
Mallory reported his results utilizing a variant Townley anatomic knee design that included ACL and PCL release. He reviewed 58 patients with degenerative arthritis, and 9 with rheumatoid arthritis in 72 patients with 88 total knee replacements during a 2 to 4 year follow up. Five patients needed revision, 3 for tibial loosening, 1 for patellar loosening, and 1 for infection. 45 patients had mild or no pain, and 82 % had unlimited walking capacity. In addition, 83 % had greater than 80 degrees of flexion [10]. This knee is still sold today as the Total Knee Original (BioPro, Port Huron, MI).
Fred Ewald, working at the Robert Breck Brigham Hospital, Boston, MA took a slightly different approach in the early 1970s. He evolved the concept of the uncemented Smith-Peterson femoral hemiarthroplasty, which was used at the Massachusetts General Hospital, Boston, MA, by adding an anatomic tibial tray. Ewald utilized femoral models of various sized casted bones using plaster of Paris through a range of motion of the knee in 6 degrees of freedom. In the transverse plane he included 6 degrees of rotation to find the optimal shape of polyethylene surface geometry using dental-based plate wax. While this would decrease the constraint, it would increase the contact area. He optimized the ratio between the various radii creating the convex femoral surface with various radii of the concave tibial surface using this simple wax model and filed a patent [11]. The tibial tray looked like 2 tulip cups connected anteriorly (Fig. 1). The posterior cruciate ligament was preserved. After extensive joint simulator testing at the Massachusetts Institute of Technology, the implant was inserted in 24 patients with severe deformities between 1975 and 1977. Each patient had good to excellent outcomes (personal communication, Fred Ewald) at 10 years with only 1 revision for a failed patella. He realized very quickly that 3 sizes were not sufficient to match the range of sizes and geometries he needed during surgery. However, his request to manufacture more than 3 sizes of the implant was uneconomical and not feasible (personal communication, Fred Ewald). He therefore abandoned the anatomic total knee concept and proceeded together with Peter Walker and Clement Sledge at the Brigham and Women’s Hospital in Boston to improve the PCL retaining functional design. One contribution was adding an asymmetric trochlea to the Duopatella concept. This evolved later into the CR Robert Brigham knee which was only briefly implanted due to its relatively flat J-curve in extension. While Walker, Sledge, Ewald, and Robert Poss designed the CR Kinematic knee (Howmedica), Kinematic II and later the CR Kinemax and Kinemax Plus using a symmetric femur, Richard Scott and Tom Thornhill focused on evolving the Robert Brigham Knee by adding more options of different AP and ML sizes and wings to the tibial tray into the design of the CR PFC, CR PFC Modular, CR PFC Sigma, and ultimately a CR rotating platform design of the PFC Sigma family (personal communication, Richard Scott and Thomas Thornhill).
Fig. 1.
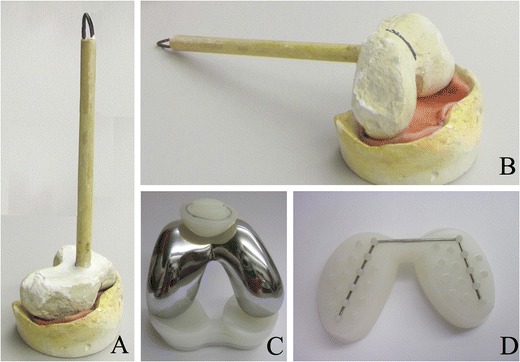
Fred Ewald’s anatomic knee designed in Boston and first implanted in 1975
In 1971, Ted Waugh and Richard Smith designed an anatomic articular surface arthroplasty without a patella flange, but with rotational freedom between the femur and the tibia. This implant permitted unrestricted rotational freedom [12] and was manufactured by Wright Medical (Memphis, TN). Later, it would evolve into the Gustillo and Ram knee. Its features were also influential for the design of the Genesis I and II (Smith & Nephew, Memphis TN). All these designs required chamfer cuts [4•].
The early advantage of a functional approach was the inventory needed. There was only 1 size for the TC and IB I design, which had a femoral AP distance of 42 mm. A second size was added in the IB II series (personal communication, Norman Scott). In order to make the implant fit, additional bone usually had to be resected. While this required a more extensive bone removal, it reduced the number of manufactured sizes. Alternatively, anatomic implants were impractical and uneconomic because of the large range of different sizes and geometries needed to conform to individual anatomy. Some anatomic designs, including the Townley knee, used chamfer cuts, while others, such as the Ewald knee, did not.
The development of functional designs over the last few decades reveals the addition of more implant size options to accommodate the large range of knee sizes and geometries. While left and right trochlear flanges were added early to the duocondylar design, gender specific features, such as narrower femoral components and more AP femoral sizes, were added later in the 1980s and 1990s. In the past decade alone, narrower trochlear flanges were marketed as gender specific and subsequently added. However, inferior clinical outcome with implant overhang [13] will likely drive the orthopedic device manufacturers in the next years to introduce even more sizes and geometries, such as a larger range of femoral ML and AP options. It remains unclear whether the increasing number of implant size options is cost effective. Hospitals are facing higher implant costs and will force industry to decrease the relatively high cost of knee implants to accommodate upcoming health care changes. If surgical outcome is the same with different implants hospitals will chose the less expensive [14]. With these economic considerations, it is unlikely that manufacturers would invest in, and produce, the implant inventory needed for anatomic knee replacement.
Functional approaches are a compromise regarding knee kinetics. While current traditional PS designs achieve femoral roll-back in knee flexion due to the cam-post mechanism, some newer designs, such as the revised PS Journey (Smith and Nephew, Memphis, TN) add asymmetric features into the cam design to create tibial internal rotation with flexion.
An anatomic approach restores the joint surfaces anatomically but functional approaches do not. Functional approaches create even flexion and extension gaps. PS designs resect more off the distal femur to compensate for flexion gap opening of 4–5 mm after the posterior cruciate ligament is resected [15]. This inherently elevates the joint line by 4–5 mm. The anatomic approach seeks to recreate the pre-arthritic femoral condylar surface of the knee by only supplementing the exact amount of cartilage and/or bone loss with femoral prosthesis. In this manner, bone resection is minimized, the offset of the distal femur, particularly the medial femoral condyle is restored, and the posterior femoral condylar offset is recreated to its pre-disease state. In doing so, the anatomic knee joint line is restored, and flexion gap laxity is minimized. This can be accomplished to some degree with standard, off the shelf implants, using a modified gap balancing technique [16] where the distal and posterior medial femur is restored and more bone is resected off the tibia using a CR functional approach without changing the joint line relying on the mechanical axis. By reestablishing the correct joint line, the center of rotation of the medial and lateral ligaments is properly restored, allowing for more normal kinematic motion after soft tissue balancing. Another technique restores the joint surfaces with standard implants, but coronal cuts are not perpendicular to the mechanical axes of femur and tibia [17]. Also, patellofemoral kinematics are more normal as a byproduct of the recreation of the femoral offset and joint line restoration. Recreating the joint surfaces restores the distance between ligament origin and insertion to restore ligament tension. It is important to know however, that ligaments of arthritic knee have changed their mechanical properties. The elongation is reduced requiring more bone resection to alleviate the increase in stiffness of an arthritic knee [18], which can be done on the tibial side.
Achieving the ideal scenario in total knee design of a large contact area without too much constraint is a paramount concern that was recognized by early innovators. Increased contact area leads to reduced polyethylene stress. Polyeythlene stress is also reduced by minimizing shear forces which, in the TC and Duopatellar designs, was addressed by adding a tibial stem. This also was thought to decrease the chance of implant loosening.
Fred Ewald addressed contact area and knee constraint concerns by modifying his tibial tray design to find the ideal male and female geometry of the femoral and tibial component. Other anatomic knee designs reduce constraint with a relatively flat tibial surface geometry, as in the Waugh and Smith knee design, including his “rotational freedom,” or the relatively flat tibial trays of the Townley knee.
The small inventory needed of functional knee designs ultimately lead to their overwhelming success and market dominance. The large library of anatomic implant sizes needed, has, historically, brought on their failure to achieve widespread production.
However, newer technologies may reverse this trend. The customized, anatomic, iTotal (Conformis Inc. Burlington MA), relies on imaging technologies such as computer tomography (CT) and magnetic resonance imaging (MRI). Through a proprietary software system, an individualized implant with several polyethylene inserts is created. This eliminates the massive inventory traditionally needed for anatomically designed knees. Alternatively, as implant companies add additional sizes to functional knees systems, inventory will likely increase to meet the desire of more size options.
Besides inventory concerns, the iTotal includes disposable pre-navigated jigs and its direct delivery model may eventually be a more cost-effective solution in total knee replacement compared with standard functional designs. Individualized anatomic total knee replacement is not a new idea, but the desire to offer an anatomic individual cost-effective solution. What is new, however, are the methods in which engineers can balance contact area without increasing constraint. The implant is patient specific, but its design features are borrowed from the past. There is no meniscal indentation of the femoral component. The transition of the trochlear flange to the femoral condyles is smooth. The trochlear flange is a prosthetic trochlea with a fixed surface geometry to treat and address trochlear dysplasia. The trochlea is placed parallel to the transepicondylar axis, but its fit is individualized to optimize bone coverage on both femoral and tibial side. The trochlear J-curve is restored to reconstruct femoropatellar kinetics. This feature is generally neglected in functional designs where the anterior cut is referenced off the anterior cortex of the distal femur. Both femoral condyles are individually restored, not based on one single radius as marketed today in some functional designs, but to restore the multicenter individual radii of each patient. Also, the joint line is restored.
Functional designs address the opening of the flexion gap when both cruciates are cut by increasing the distal femoral resection.
There is 1 major additional difference of the individualized anatomic design: the wide range of various distal offsets ranging from 6 degree of varus to 13 degrees of valgus [19•] is individually regenerated. The difference between distal femoral medial and lateral offset is added to the 6 mm of the medial insert to the lateral tibial insert to restore a neutral mechanical axis (Fig. 2A, B, C). The tibial tray is anatomic and the medial and lateral polyethylene insert geometry is based on the reconstruction of the center of medial and lateral tibial plateaus for correct rotation [20•], avoiding the traditional position of the medial 1/3 of the tibial tubercle which is highly variable. But the slightly undersized tibial tray allows the surgeon no more than 5 degrees of internal or external rotation to optimize the tray between the ML axis and the axis of the medial 1/3 of the tibial tubercle [21•]. This is an important feature since correctly rotated femoral and tibial components have been shown to decrease pain and stiffness after total knee replacement [22, 23].
Fig. 2.
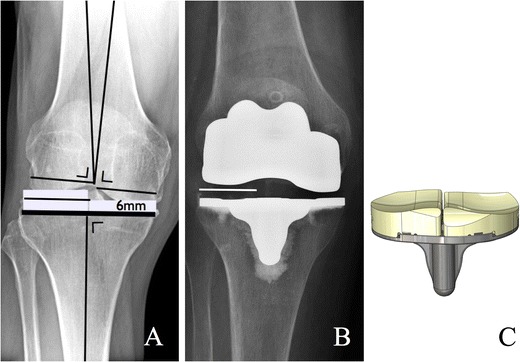
The absolute value of the distal femoral offset between distal femoral medial and lateral condyle is inversely added to 6 mm on the lateral insert to restore the neutral mechanical alignment
The individualized implant is engineered with a unique design. All cuts are pre-navigated and perpendicular to the mechanical axes. The absolute value of the distal femoral offset is inversely added to the lateral tibial insert to align the knee along the mechanical axis to avoid potential higher long-term failure rates from malalignment [24]. The tibial cut is perpendicular to the mechanical axis to avoid varus positioning, which has been associated with tibial condylar collapse [25]. The femoral component has 6 chamfer cuts, which are individually designed to minimize bone resection. The femoral component relies on chamfer cuts, which makes the preparation of the distal femur as easy as other functional knee systems. The additional sixth chamfer cut allows the femoral implant to be 2 mm thinner compared with off-the shelf implants, which reduces bone resection without mechanical fatigue properties [26]. Since the J-curve is individually restored, the coronal radius of each condyle can be optimized. The ratio between the femoral and tibial radii is similar to off-the-shelf implants in both sagittal and coronal plane providing a similar constraint compared with functional designs. While Fred Ewald used a 3D model (Fig. 1) to find the optimal ratio between distal femoral and proximal tibial geometries, this can be calculated, and the design optimized in CAD programs. As a result of this the contact area of the iTotal is twice as large compared with a RP TKR and 4 times as large as a fixed bearing TKR.
The delivery model is simple. Six weeks after the order is received, the implant, including disposable pre-navigated jigs, is delivered to the OR. There is no inventory. Turnover is easier for OR personnel. All instruments, with the exception of one tray for drills and punches, are disposable. All instruments are pre-navigated restoring the mechanical alignment to neutral. The surgeon has the choice between 2 different medial PE thicknesses (6 and 8 mm) and 3 lateral (6, 7, 8 mm plus absolute value of distal femoral offset). The implant is delivered with a detailed surgical plan providing the surgeon the accurate bone resections. By measuring each cut intra-operatively the surgeon can verify his cut and potentially can make the necessary changes either by placing a thicker insert or by recutting bone.
Conclusions
Customized total knee replacement is more than an old idea of an anatomic approach to total knee replacement. Using today’s technologies, an anatomic TKR is generated based on modern imaging technologies to generate an individual fit to optimize coverage, to restore the individual J-curves of all 3 knee compartments, and to restore the distal femoral individual offset, which decreases the need for balancing of the ligaments. The original distance between origin and insertion of all ligaments are restored. The customized knee is engineered to optimize the contact area without increasing constraint, to restore the mechanical axis to neutral using pre-navigated disposable instruments, and to reduce the femoral component thickness to preserve bone stock. The delivery model with disposable, pre-navigated jigs is simple, efficient, and timely. With increasing pressure to decrease the cost of total knee replacement in our changing health care environment, individualized anatomic TKR has an opportunity to grow. TKR may prove to be more cost effective compared with functional TKR, with an increasing library of various implants that need to be delivered and available for each case.
Acknowledgments
Disclosure
EM Schwechter: none; W. Fitz: Member of scientific advisory board, consultancy, patents, stock/stock options, and receives royalties from Conformis, Inc.
Contributor Information
Evan M. Schwechter, Email: eschwec@gmail.com
Wolfgang Fitz, Email: wfitz@partners.org.
References
Papers of particular interest, published recently, have been highlighted as: • of importance
- 1.Ranawat CS, Shine JJ. Duo-condylar total knee arthroplasty. Clin Orthop Relat Res. 1973;185–95. [DOI] [PubMed]
- 2.Walker PS, Wang C-J, Masse Y. Joint laxity as a criterion for the design of condylar knee prostheses. Proc Inst Mech Eng. 1974;CP16:22. [DOI] [PubMed]
- 3.Walker PS, Ranawat C, Insall J. Fixation of the tibial components of condylar replacement knee prostheses. J Biomech. 1976;9:269–75. doi: 10.1016/0021-9290(76)90013-0. [DOI] [PubMed] [Google Scholar]
- 4.Robinson RP. The early innovators of today's resurfacing condylar knees. J Arthroplasty. 2005;20(1 Suppl 1):2–26. doi: 10.1016/j.arth.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 5.Murray DG JHS, Inventor. Knee joint prosthesis. US patent 4,016,606. April 12, 1977, 1977.
- 6.Goodfellow JW JJS, Nigel G. Inventor. Prosthetic joint device. US patent 4,085,466. April 25, 1978. 1978.
- 7.Yamamoto S. Total knee replacement with the Kodama-Yamamoto knee prosthesis. Clin Orthop Relat Res. 1979;145:60–7. [PubMed] [Google Scholar]
- 8.Townley CO. Total knee arthroplasty, a personal retrospective and prospective review. Clin Orthop. 1988;236:8. [PubMed]
- 9.Townley CO. The anatomic total knee resurfacing arthroplasty. Clin Orthop Relat Res. 1985;192:82–96. [PubMed] [Google Scholar]
- 10.Mallory TH, Smalley D, Danyi J. Townley anatomic total knee arthroplasty using total tibial component with cruciate release. Clin Orthop Relat Res. 1982;169:197–201. [PubMed] [Google Scholar]
- 11.Ewald FC Inventor. Joint Protheses. US patent 3,798,6791971.
- 12.Waugh TR, Smith RC, Orofino CF, Anzel SM. Total knee replacement: operative technical and preliminary results. Clin Orthop Relat Res. 1973;94:196–201. doi: 10.1097/00003086-197307000-00024. [DOI] [PubMed] [Google Scholar]
- 13.Mahoney OM, Kinsey T. Overhang of the femoral component in total knee arthroplasty: risk factors and clinical consequences. J Bone Joint Surg Am. 2010;92:1115–21. doi: 10.2106/JBJS.H.00434. [DOI] [PubMed] [Google Scholar]
- 14.Sell D. Legal tussle in market for medical devices. The Inquirer. April 5, 2012. 2012.
- 15.Kadoya Y, Kobayashi A, Komatsu T, Nakagawa S, Yamano Y. Effects of posterior cruciate ligament resection on the tibiofemoral joint gap. Clin Orthop Relat Res. 2001;391:210–7. doi: 10.1097/00003086-200110000-00023. [DOI] [PubMed] [Google Scholar]
- 16.Fitz W, Sodha S, Reichmann W, Minas T. Does a modified gap-balancing technique result in medial-pivot knee kinematics in cruciate-retaining total knee arthroplasty? a pilot study. Clin Orthop Relat Res. 2012;470:91–8. doi: 10.1007/s11999-011-2121-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Howell SM, Kuznik K, Hull ML, Siston RA. Results of an initial experience with custom-fit positioning total knee arthroplasty in a series of 48 patients. Orthopedics. 2008;31:857–63. doi: 10.3928/01477447-20080901-15. [DOI] [PubMed] [Google Scholar]
- 18.Fishkin Z, Miller D, Ritter C, Ziv I. Changes in human knee ligament stiffness secondary to osteoarthritis. J Orthop Res. 2002;20:204–7. doi: 10.1016/S0736-0266(01)00087-0. [DOI] [PubMed] [Google Scholar]
- 19.Hunter DJ, Niu J, Felson DT, Harvey WF, Gross KD, McCree P, et al. Knee alignment does not predict incident osteoarthritis: the Framingham osteoarthritis study. Arthritis Rheum. 2007;56:1212–8. doi: 10.1002/art.22508. [DOI] [PubMed] [Google Scholar]
- 20.Cobb JP, Dixon H, Dandachli W, Iranpour F. The anatomical tibial axis: reliable rotational orientation in knee replacement. J Bone Joint Surg Br. 2008;90(8):1032–8. doi: 10.1302/0301-620X.90B8.19905. [DOI] [PubMed] [Google Scholar]
- 21.Lawrie CM, Noble PC, Ismaily SK, Stal D, Incavo SJ. The flexion-extension axis of the knee and its relationship to the rotational orientation of the tibial plateau. J Arthroplast. 2011;26(6 Suppl)):53–8. doi: 10.1016/j.arth.2011.04.026. [DOI] [PubMed] [Google Scholar]
- 22.Bedard M, Vince KG, Redfern J, Collen SR. Internal rotation of the tibial component is frequent in stiff total knee arthroplasty. Clin Orthop Relat Res. 2011;469:2346–55. doi: 10.1007/s11999-011-1889-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nicoll D, Rowley DI. Internal rotational error of the tibial component is a major cause of pain after total knee replacement. J Bone Joint Surg Br. 2010;92:1238–44. doi: 10.1302/0301-620X.92B9.23516. [DOI] [PubMed] [Google Scholar]
- 24.Fang DM, Ritter MA, Davis KE. Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplast. 2009;24(6 Suppl):39–43. doi: 10.1016/j.arth.2009.04.034. [DOI] [PubMed] [Google Scholar]
- 25.Berend ME, Ritter MA, Meding JB, Faris PM, Keating EM, Redelman R, et al. Tibial component failure mechanisms in total knee arthroplasty. Clin Orthop Relat Res. 2004;428:26–34. doi: 10.1097/01.blo.0000148578.22729.0e. [DOI] [PubMed] [Google Scholar]
- 26.Slamin J, Ketelhon, R. Bojarski, R., Parsley, B. Optimizing Knee Femoral Component Strength and Bone Preservation with Finite Element Analysis. Proceedings of the Orthopaedic Research Society; 02/042012–02/07/2012, 2012; San Francisco, CA.


