Abstract
Over the past decade, there has been an increased interest in understanding the operative indications and techniques in treating scapular fractures and tracking their outcomes. Multiple studies have documented poor functional outcomes following nonoperative management of displaced scapular fractures. There is a groundswell of recognition that severe deformity from scapular malunion is associated with functional consequences for patients. This has led to a growing recognition that scapular fractures should be held to the same standards as other bodily fractures with regard to fracture fixation principles, including anatomic articular reduction, proper alignment, and stable internal fixation. Through research, there has been an improved understanding of scapular fracture patterns and the relevant surgical approaches and exposures used for fracture fixation. As with many bones, however, there still remains the absence of a compelling study that defines thresholds for surgical indication based on degrees of deformity and amounts of displacement.
Keywords: Trauma, Upper extremity trauma, Scapula fracture, Dynamic scapular function, Shoulder girdle injury, Scapular malunion, Current review, ORIF scapula, Proximal forequarter
Introduction
Although formerly felt to be rare, scapula fractures have been shown to occur with a rate of 0.7 % of all fractures. Thus, scapula fractures occur at rates approaching those of distal tibia and humerus fractures [1]. It is estimated that scapula fractures account for 3 %–5 % of all fractures about the shoulder girdle, with the most frequent fractures encountered occurring in the clavicle or proximal humerus [2, 3].
With the exception of displaced articular glenoid fractures, perhaps the rarity of scapula open reduction internal fixation (ORIF) has fostered the traditional treatment of scapular fractures with benign neglect, with the hope of minimal functional compromise. Part of the rationale for this treatment modality has stemmed from the understanding that the shoulder joint range of motion far exceeds that which is needed for the activities of daily living. However, by definition, some sort of functional compensation must occur after malunion, with possible loss of motion, strength, endurance, or reaction time of the shoulder girdle. This deficit is currently poorly understood and not yet clearly defined. Recently, however, there has been new evidence to show that the scapula acts as part of a dynamic stabilizer of the humerus and shoulder complex [4–8]. Thus, old assumptions regarding static stabilization surrounding the shoulder girdle range of motion and function may be somewhat clinically irrelevant in the real world of day-to-day dynamic shoulder activities.
It is therefore without surprise that over the past 2 decades, several studies have documented poor results following nonoperative management of both intra- and extraarticular displaced scapular fractures [9–14, 15•, 16–21]. With the development of modern techniques in both surgical approach and internal fixation, surgeons began fixing selected scapula fractures utilizing Arbeitsgemeinschaft für Osteosynthesefragen (AO) principles of restoration of articular surface, alignment, and stable internal fixation leading to a renewed interest in the operative management of both displaced intraarticular and extraarticular scapular fractures. The surgical treatment of these fractures continues to evolve as our knowledge of shoulder anatomy, indications, surgical approaches, and implants has improved.
Pathoanatomic aspects of anatomy and function
It has long been known that the shoulder girdle has several static constraints, including the glenoid labrum, the rotator cuff muscles (which apply a constant axial compressive force of the humerus against the glenoid), relative negative intraarticular joint pressure, and the joint capsule, all of which are designed to keep the shoulder joint from dislocating. However, recently, evidence has shown that the scapula acts as part of a dynamic stabilizer with respect to the humeral head and shoulder complex [4–8]. To highlight the dynamic stabilization at stake, 18 muscles originate from, insert into, or cross the scapula and glenohumeral joint.
The scapula’s glenoid has been compared with a seal balancing a ball on its nose [22], constantly adjusting to closely follow the rapid translational motion of the humeral head to prevent dislocation (just as the seal prevents a ball from falling off its nose). Keeping the humeral head correctly and precisely centered over the glenoid optimizes dynamic stability by allowing for optimal function of the rotator cuff muscles through their respective physiologic Blick’s muscle curve (the rotator cuff muscles act as both dynamic and static stabilizers to the shoulder girdle complex). Furthermore, at the extremes of humerus–glenoid translations, additional dynamic protective mechanisms guard against frank dislocation. In situations such as those in which a large impulse is applied to the humeral head, creating a relatively large scapula–humeral-head translational mismatch/subluxation (an example is a seal’s neck not being able to keep up with a falling ball), a protective reflex arc of the rotator cuff muscles prevents dislocation. For example, if such a translational mismatch were to cause anterior subluxation of the humeral head against the glenoid, the subscapularis muscle would be relatively stretched, when compared with the other rotator cuff muscles. This prestretched subscapularis muscle would have a better response time and be more effective when fired in negating the relative anterior subluxation of the humeral head (since it would already be prestretched). Myers et al. [6] demonstrated an association between this precise rotator cuff reflex arc and persistent shoulder instability. Morris et al. [8] demonstrated electromyographical altered muscle activity and imbalance affecting shoulder girdle coordination in patients with multidirectional instability. Warner et al. [5] demonstrated a difference in scapulothoracic motion in the normal shoulder versus shoulders with glenohumeral instability and impingement syndrome. Matsumura et al. [23] showed, in a recent cadaveric study, that clavicle shortening leads to significant alteration of the physiologic scapulothoracic joint kinematics. Cole et al. [15•] identified a group of patients who had developed highly symptomatic malunion following an extraarticular fracture of the scapula. These patients underwent revision surgery, which ultimately improved their Disabilities of the Arm, Shoulder, and Hand (DASH) scores to normal levels [24]. It is likely that alterations in the osseous anatomy (malunions) affect these dynamic stabilizers in a way that promotes fatigue and symptoms of dysfunction.
Taking these factors into account, it is not a stretch to understand the pathophysiology behind why certain groups of patients would have shoulder girdle symptoms such as residual pain, weakness, and functional complaints following nonsurgical treatment of scapular fractures that lead to malunion [9–14, 15•, 16–21]. Furthermore, because of the close relationship of the scapula with respect to the clavicle via the AC joint and CC ligaments, it is not surprising that a fracture malunion of the scapula, the clavicle, or a combination would result in similar shoulder complaints being reported by patients. Ristevski et al. [25] recently reported on scapular malalignment in patients with symptomatic midshaft clavicle malunions and demonstrated scapular winging in this patient population. Ledger et al. [26] evaluated the anatomic and functional effects of shortened clavicle malunions in 10 patients and found reduced peak upper extremity abduction velocity, shoulder scores and visual analog global assessments for the affected shoulder, and reduced muscular strength for adduction, extension, and internal rotation—further evidence of dynamic shoulder dysfunction status postmalunion.. Other studies have evaluated the pathologic effects of scapular protraction on shoulder function. The scapula provides the base on which the upper extremity rests in both dynamic and static positions. A clavicle or scapular malunion both clearly alters the resting position of the scapula and causes malalignment. This places muscles attaching to the scapula in a position that alters their mechanical advantage and explains the consistencies of similar complaints between patients with clavicle and/or scapular malunions.
Clinical evaluation
The physical examination should reflect an understanding of the commonly associated injuries, particularly those that are life threatening, when a patient is examined for a scapula fracture. Associated injuries are common particularly to the spine, cranium, and thorax [27–29]. Given the high energy associated with scapula fractures, one should be aware of recent literature correlating open blunt trauma clavicle fractures with a 52 % rate of head injury and 7 % rate of associated great vessel injury [30]. Gottschalk et al. [31] demonstrated rates of head, thoracic, and great vessel injuries in patients with shoulder girdle injury to be 31.5 %, 36.8 %, and 3.9 %, respectively. Baldwin et al. conducted a retrospective review of the National Trauma Database to examine concomitant diagnoses in over 9,400 scapula fractures. Among their findings was that rib fractures were present in 52.9 %, spine fractures in 29.1 %, lung injury in 47.1 %, head injury in 39.1 %, and clavicle fractures in 25.2 % of patients diagnosed with a scapula fracture [29].
When possible, the shoulder and upper extremity should be examined with the patient sitting or standing, to give good access to the posterior forequarter, which is difficult when the patient is supine in bed. Medial and caudal displacement of the shoulder may be obvious, producing marked asymmetry, particularly if the patient is upright. Shoulder girdle injuries are frequently associated with neurovascular lesions and demand an appropriate assessment of the brachial plexus and distal perfusion, because 13 % of patients with scapula fractures sustain a brachial plexus injury [32]. The suprascapular and axillary nerves are at particular risk, yet it is usually impossible to assess their motor function, because of fracture displacement and pain; however, axillary nerve sensation should be documented. Abrasion over the scapula spine and acromion are common; therefore, skin integrity should be assessed for appropriate timing of surgery. Our preference is to wait on surgery until the skin has re-epithelialized. If the patient presents after 2 weeks postinjury, an electromyographic assessment of the suprascapular and axillary nerve and brachial plexus is possible. Fractures entering the spinoglenoid notch place the suprascapular nerve at very high risk for injury, and an EMG/NCS should be mandatory before or after surgery to document its conductive integrity.
Imaging
A standard chest radiograph should be obtained to evaluate for pneumothorax, and a trauma lateral cervical spine radiograph or sagittal cervical CT should be obtained to assess the patient for associated spinal fractures (Fig. 1). Additionally, the radiographic workup should include an upright AP, scapula (Grashey view), axillary, and scapula Y views. With the Grashey view, one should measure the glenopolar angle, which is created at the intersection of a line drawn form the inferior glenoid fossa to the superior apex of the glenoid fossa and a line drawn from the superior apex of the glenoid fossa to the inferior angle of the scapula. Medial displacement of the proximal fragment, relative to the distal fragment at the lateral border, should also be assessed, a measurement sometimes referred to as lateral border offset. In the scapula Y view, angulation is measured by drawing a line parallel to the proximal fragment and a line parallel to the distal fragment. These radiographic parameters are the basis for determining indications for surgery: glenopolar angle, lateral border offset (aka medialization), and angulation. The axillary view is used to assess fractures of the acromion and coracoid, to assess glenohumeral subluxation or dislocation and intraarticular stepoff (which can also be seen on the Grashey view).
Fig. 1.
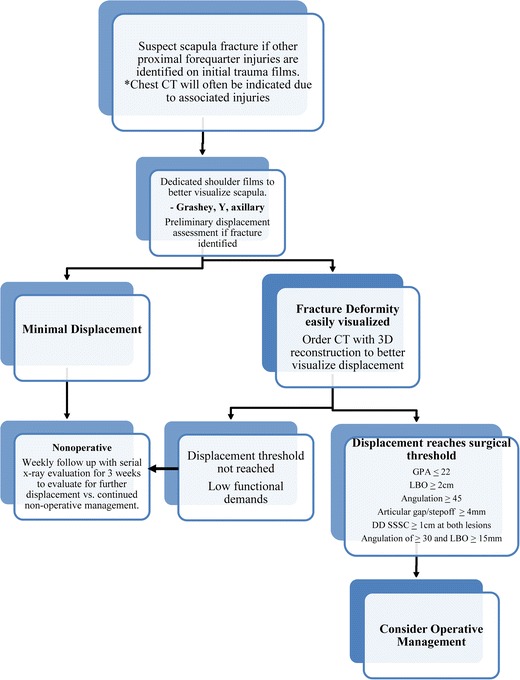
Management of scapula fractures. GPA = glenopolar angle; LBO = lateral border offset
Because patients with a scapula fracture often present as multitrauma patients, a chest CT is often already performed on such patients upon their arrival to the ER. This CT could be used, and 3-D reconstruction views of the scapula can be obtained. Cole et al. [33•] demonstrated that CT scans were more reliable than plain radiographs in the assessment of inter- and intraobserver reliability with regard to scapular angulation, translation, and glenopolar angle measurements (Fig. 2). This was confirmed in an additional study by Bartonicek et al. [34]. If marked displacement has occurred, such that there is a possibility of meeting surgical indications, a 3-D CT scan should be obtained, which allows for the most accurate measurements of deformity [35•]. Furthermore, progressive deformity of the scapular fracture during the early postinjury phase is a concern [36], and serial upright radiographs should be obtained on a weekly basis for up to 3 weeks if nonoperative management is to be undertaken. This to ensure no further displacement and accurate nonoperative management.
Fig. 2.
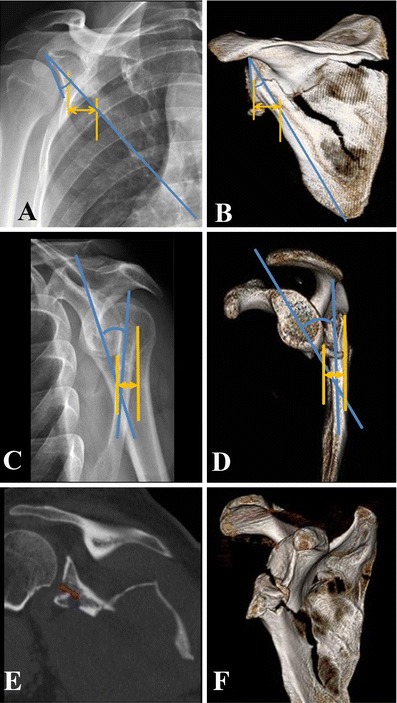
X-ray and 3-D reconstructed CT images illustrating displacement measurements described by Anavian et al. [33•]. a, b Measurements of lateral border offset (yellow arrow) and glenopolar angle (blue angle), which are measured on the Grashey x-ray view and 3-D oriented in the true AP plane. c, d Measurements of translation (yellow arrow) and angulation (blue angle), which are measured on the scapula Y x-ray and 3-D CT views. e, f Intraarticular step-off and gap. These measurements can be performed on axial, sagittal, coronal, or 3-D CT reformats, depending on orientation of fracture line
Treatment
Nonoperative management
Dimitroulias et al. [37•] recently published a nonrandomized control trial demonstrating satisfactory outcomes with nonoperative treatment of scapular body fractures in terms of final DASH scores in a series of 32 patients. Given current published operative indications, we find it hard to reach meaningful conclusions when the vast majority of the patients in this study would be treated nonoperatively by nearly anyone’s standard. Another recent study by Jones et al. [38] compared final outcomes between operative and nonoperative cohorts and found similar outcomes, despite the operative cohort having had significantly worse initial displacements. Considering the lack of randomization and the fact that the more severe surgically treated group had equal outcomes, as compared with lesser injuries treated nonoperatively, absolute conclusions are difficult to arrive at. However, a positive bias toward the surgically treated group can possibly be inferred.
Because of the lack of randomized controlled trials, there is still conflicting evidence in the literature regarding absolute surgical indications. There is a growing belief that nonoperative management of extraarticular scapula fractures is best reserved for those displaced less than 15–20 mm and angulated less than 30°–45° secondary to uniformly good outcomes with nonoperative treatment [2, 20, 37•, 39–42]. With such clinical presentations, the treatment should include patient reassurance, a sling, and physical therapy.
Surgical management
Intraarticular surgical indications
Indications for ORIF of intraarticular glenoid fractures have been addressed through the classification systems proposed by the modified Ideberg [32] and Goss. A displacement threshold for ORIF has been proposed of more than 4 mm of articular step-off or more than 20 % of the glenoid involved. Variations, however, exist regarding step-of indication ranging from 2 to 10 mm [3, 32, 43, 44•, 45–52]. Certainly, any instability involving a glenoid fracture of the glenohumeral joint warrants surgical intervention. Surgery is indicated for any glenoid fracture resulting in subluxation and/or glenohumeral instability. Anterior rim fractures involving greater than 25 % of the articular surface are relatively indicated for operative fixation [3, 53]. Posterior rim fractures larger than 33 % of the articular glenoid surface have also been considered unstable and warrant operative intervention [54].
It is therefore up to the surgeon to integrate multiple injury factors, including articular step-off and/or gap and percentage of joint involvement, as well as patient factors including age, activity level, hand dominance, job requirements, and health level, to determine an optimal treatment plan. Recently, our group [44•] reported on the largest operative series of intraarticular glenoid fractures (33 patients), with detailed documentation of functional outcome, strength, and motion. Criteria for surgical intervention included articular fracture gap or step-off greater than or equal to 4 mm. Twenty-one patients underwent a posterior approach, 7 underwent an anterior deltopectoral approach, and 5 underwent a combined approach. At a mean 25-month follow-up, 91 % of patients showed anatomic restoration of the articular surface after surgery, with no losses of reduction or failed fixation. At the time of follow-up, 87 % of the patients were pain free, with 90 % of patients returning to their preinjury level of work and/or activity. Other recent publications have demonstrated excellent outcomes in smaller series after arthroscopic-assisted reduction and percutaneous cannulated screw fixation of isolated glenoid rim lesions or noncomminuted transverse glenoid fractures [55–58].
Extraarticular body and neck fracture surgical indications
Indications for extraarticular surgical intervention are even more controversial secondary to the lack of randomized controlled trials comparing operative versus nonoperative treatments. Relative indications for internal fixation of extraarticular scapular fractures are as follows: angular deformity ≥45ºon a scapular Y shoulder radiograph, lateral boarder offset (LBO) ≥15 mm plus angular deformity ≥35°, LBO ≥20 mm, Glenopolar angle ≤22º as measured on a true Grashey AP view of the shoulder, displaced double lesions of the superior shoulder suspensory complex where both the clavicle and scapula fractures are displaced ≥10 mm, or coexistence of a complete AC dislocation and scapula fracture with displacement ≥10 mm. These relative indications must be placed in the context of the patient’s functional demands. Using the above-stated criteria, the chief author [59] has been able to demonstrate low rates of subsequent complications with surgical intervention and good functional outcomes and satisfactory scores among patients.
Multiple lesions to the superior shoulder suspensory complex
In 1993, Goss [60] coined the phrase superior shoulder suspensory complex (SSSC) of the shoulder as the osseoligamentous connection of the acromion, coracoid, and glenoid processes of the scapula as they relate to their respective capsule–ligamentous connections. Goss theorized that a double disruption in any two of the four structures would cause a “floating” glenohumeral joint. This would represent a discontinuity between the axial and appendicular skeleton and would require surgical intervention. Subsequently, his theory has been challenged by some authors [61–63]. We agree with Edwards et al. [61] and Ramos et al. [63] that surgery is not indicated when each component of the double displacement is stable and minimally displaced (less than 10 mm), but we agree with Goss that the instability of the displaced floating shoulder presents a lower threshold for open reduction internal fixation. The senior author has encountered over a dozen cases of even greater than two lesions to the SSSC, all associated with high displacement and ipsilateral injuries, and we believe that all of these should be treated aggressively with ORIF, to allow immediate mobilization.
Process fracture surgical indications
With regard to isolated fractures of the acromion or coracoid process, these are uncommon. These fractures usually occur as a result of a direct blow to the superior shoulder region for acromion fractures or a violent traction injury through the biceps and coracobrachialis. We use several criteria to aid in determining the need for surgery. If either an acromion or a coracoid fracture is displaced more than 10 mm or there is an ipsilateral scapula fracture or multiple disruption of the SSSC, then ORIF is warranted [42, 43, 64–68]. When the acromion is displaced more than 5 mm, a supraspinatus outlet view should be obtained and evaluated for acromial depression, which may contribute to an impingement syndrome, much like a type III “hooked” acromion, which may warrant a lower threshold for ORIF. Outcomes following ORIF of acromion or coracoid process fractures have been generally good, with high rates of union [65, 66, 68, 69]. Anavian et al. [68] reported the results of surgical management of 14 coracoid and 13 acromion fractures treated operatively. A combination of screws, tension bands, sutures, or plate fixation was used. All of these process fractures healed with mean DASH scores that were of the same as uninjured population normative baseline DASH scores. The only complications in this series were soft tissue irritation requiring hardware removal in 2 patients and removal of ectopic bone in 1 patient.
In contrast, in the setting of patients with a reverse total shoulder arthroplasty (rTSA), the reported functional results of surgically fixed isolated scapular /acromion fractures have been less favorable [70, 71]. The occurrence of acromion fracture s/p rTSA has been reported with an incidence approaching 5 %. The mechanism appears to be either a stress riser from the superior screw of the glenoid component and/or, more frequently, a result of altered physiology status post-rTSA. The location of this fracture is related to the maximal moment arm exerted by the deltoid at its attachment along the acromial base and is likely related to superphysiologic stresses seen by the acromion secondary to altered function of the deltoid [72]. As a consequence, acromial fractures in the setting of rTSA substantially alter the biomechanics of this deltoid-dependent implant [72]. This condition in the setting of rTSA may be an emerging problem of which we do not yet know the full clinical significance. It seems reasonable to approach the fractured acromion in this setting with ORIF to restore stability in a way that renders a tension band principle to the acromial spine [70].
Surgical treatment
The decision regarding a surgical approach should be determined after careful review of the radiology studies. Recently, scapula fractures have been mapped from analysis of 3-D CT to clearly illustrate the true nature of fracture patterns [35•]. This map provides a basis for approaching the usual variants only, and each patient’s CT scan must be reviewed in detail to determine the best approach. In addition, 3-D CT has been shown to afford superior interobserver and intraobserver reliability over plain films [33•].
Fractures involving the neck and body of the scapula make up approximately 80 %–90 % of surgical injury patterns. These fracture patterns are addressed through variations of the posterior approach. A Judet incision should be used if the surgeon needs access to multiple scapula borders seen with extensive fracture patterns or in cases of chronic malunions.
The patient is positioned in the lateral decubitus position. BoneFoam (Plymouth, MN) arm positioners are helpful for this setup. A Judet posterior incision along these landmarks, 1 cm caudal to the acromion spine and 1 cm lateral to the vertebral border, is used. The surgeon’s decision making at this juncture depends on the desire for limited or complete exposure to the posterior scapula.
Limited exposure is developed via intermuscular windows [73], with an advantage of reduced trauma to the surrounding soft tissue and help in protecting the suprascapular and axillary nerves. This technique can be used to access fractures requiring reduction and fixation at the lateral border, acromial spine, and vertebral borders of the scapula. Since almost all fractures of the scapula that require surgery have displacement of the lateral border, the most important window is between the infraspinatus and teres minor. This window gives access to the lateral border, scapula, neck, and posterior glenoid. Great attention must be given to developing this interval carefully so as not to injure the neurovascular structures located in the quadrangular space, which is caudal and lateral to the desired interval. If needed, an additional window could be developed between the trapezius and the deltoid to access the spine of the scapula. A third window can be developed along the vertebral medial border of the scapula. The intermuscular plane for this window is between the infraspinatus and the rhomboids.
Alternatively, an extensile approach to the scapula involves elevation of the entire infraspinatus muscle from medial to lateral, with exposure of the infraspinatus fossa up to the glenoid neck. The extensile exposure grants the surgeon adequate control of the fracture at multiple points to effect the reduction and mobilize the fracture in cases of severe fracture comminution or in cases in which callus formation has occurred in scapular fractures that are often more than 3 weeks old.
More recently, a minimally invasive approach to the scapula vertebral and lateral borders has been described [74]. This approach is well suited for simple neck and body variants that are addressed within 1 week of injury. This exposure promotes less dissection and quicker rehabilitation.
Complex articular fractures dictate an anterior or posterior glenohumeral approach depending on CT findings of the fracture patter and location of comminution.
Rehabilitation
With the goal of accomplishing stabilization achieved, immediate full passive and active assisted range of motion should be emphasized, a formula that has been associated with a 100 % union rate, with no evidence of hardware failure. Light strengthening and resistance with 3–5 lb of weight is begun 4 weeks postoperatively, followed by strength and endurance training beginning after 8 weeks. After 12 weeks, all restrictions are lifted, and the patient may return to normal activities.
The role of the therapist may be one component of a successful postoperative recovery. Pulleys and Therabands and a keen understanding of exercises to strengthen the rotator cuff and parascapular musculature are paramount. Most often, physical therapists are unfamiliar with treating patients with scapular fractures and are afraid to inflict harm. This tendency is associated with a failure to progress and must be defeated by clear communication to the patient and therapist.
Conclusion
Indications for surgical management of scapular fractures continue to be better defined as we improve our understanding of the pathophysiology of scapula malunion. Furthermore, increased surgical experience and surgeon awareness, improved operative approaches, and a higher number of patients who survive high-energy trauma with highly displaced scapular fractures led to good patient outcomes after surgical fixation in properly selected patients.
Surgical indications for scapular fractures are based on angular deformity and displacement. However, these indications need to be placed in the context of other ipsilateral injuries, as well as patient activity level, hand dominance, and any co-morbidities. The surgical risks of open reduction internal fixation of scapula fractures have been historically low across many operative series, and it is this relatively low-risk option that should align with the principles of treatment for other fractures. This approach provides the benefit of more immediate pain relief and quicker rehabilitation of the shoulder girdle, with the hopeful prevention of the lasting sequelae of dysfunction more recently discovered in malunions.
Acknowledgement
The authors would like to acknowledge Aaron R. Jacobson DC for helping with the manuscript draft and edits.
Disclosure
P. A. Cole: receives consulting fees/honoraria from AONA and AO International, is a consultant to J&J (Synthes-Depuy), and has stock/stock options with BoneFoams Inc, LLC; G. Freeman: none; J. Dubin: none.
Contributor Information
Peter A. Cole, Phone: +1-651-2543669, FAX: +1-651-2541519, Email: Peter.A.Cole@healthpartners.com
Gil Freeman, Phone: +1-651-2543247, FAX: +1-651-2541519, Email: gilfreeman24@gmail.com.
Jonathan R. Dubin, Phone: +1-651-2543247, FAX: +1-651-2541519, Email: Johndubin1@yahoo.com
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Court-Brown CM, Aitken SA, Forward DR, et al. The epidemiology of fractures. In: Bucholz RW, et al., editors. Fractures in adults. Wilkins: Lippincott Williams; 2009. [Google Scholar]
- 2.ROWE CR. Fractures of the scapula. Surg Clin North Am. 1963;43:1565–71. doi: 10.1016/s0039-6109(16)37145-6. [DOI] [PubMed] [Google Scholar]
- 3.Butters KP. The scapula. In: Rockwood CA Jr, Matsen FA II, editors. The shoulder. Philadelphia: WB Saunders; 1990. [Google Scholar]
- 4.McClure PW, Michener LA, Karduna AR. Shoulder function and 3-dimensional scapular kinematics in people with and without shoulder impingement syndrome. Phys Ther. 2006;86:1075–90. [PubMed] [Google Scholar]
- 5.Warner JJ, Micheli LJ, Arslanian LE, et al. Scapulothoracic motion in normal shoulders and shoulders with glenohumeral instability and impingement syndrome. A study using moire topographic analysis. Clin Orthop Relat Res. 1992;285:191–9. [PubMed] [Google Scholar]
- 6.Myers JB, Riemann BL, Ju YY, et al. Shoulder muscle reflex latencies under various levels of muscle contraction. Clin Orthop Relat Res. 2003;407:92–01. doi: 10.1097/00003086-200302000-00017. [DOI] [PubMed] [Google Scholar]
- 7.Latimer HA, Tibone JE, Pink MM, et al. Shoulder reaction time and muscle-firing patterns in response to an anterior translation force. J Shoulder Elbow Surg. 1998;7:610–5. doi: 10.1016/S1058-2746(98)90009-X. [DOI] [PubMed] [Google Scholar]
- 8.Morris AD, Kemp GJ, Frostick SP. Shoulder electromyography in multidirectional instability. J Shoulder Elbow Surg. 2004;13:24–9. doi: 10.1016/j.jse.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 9.Ada JR, Miller ME. Scapular fractures. Analysis of 113 cases. Clin Orthop Relat Res. 1991;269:174–80. [PubMed] [Google Scholar]
- 10.Nordqvist A, Petersson C. Fracture of the body, neck, or spine of the scapula. A long-term follow-up study. Clin Orthop Relat Res. 1992;283:139–44. [PubMed] [Google Scholar]
- 11.Wilkes RA, Halawa M. Scapular and clavicular osteotomy for malunion: case report. J Trauma. 1993;34:309. doi: 10.1097/00005373-199302000-00027. [DOI] [PubMed] [Google Scholar]
- 12.Martin SD, Weiland AJ. Missed scapular fracture after trauma. A case report and a 23-year follow-up report. Clin Orthop Relat Res. 1994;299:259–62. [PubMed] [Google Scholar]
- 13.Romero J, Schai P, Imhoff AB. Scapular neck fracture—the influence of permanent malalignment of the glenoid neck on clinical outcome. Arch Orthop Trauma Surg. 2001;121:313–6. doi: 10.1007/s004020000224. [DOI] [PubMed] [Google Scholar]
- 14.van Noort A, te Slaa RL, Marti RK, et al. The floating shoulder. A multicentre study. J Bone Joint Surg Br. 2001;83:795–8. doi: 10.1302/0301-620X.83B6.10806. [DOI] [PubMed] [Google Scholar]
- 15.• Cole PA, Talbot M, Schroder LK, et al. Extra-articular malunions of the scapula: a comparison of functional outcome before and after reconstruction. J Orthop Trauma. 2011;25:649–56. This is the first report on a series of patients who underwent corrective osteotomy for symptomatic malunion of a scapula fracture. Four of 5 patients returned to their original occupations and activities. Mean Disabilities of the Arm, Shoulder and Hand scores improved from 39 (range, 27–58) preoperatively to 10 (range, 0–35) postoperatively. There were no complications. [DOI] [PubMed]
- 16.Haraguchi N, Toga H, Sekiguchi Y, et al. Corrective osteotomy for malunited fracture of the glenoid cavity: a case report. Clin Orthop Relat Res. 2002;404:269–74. doi: 10.1097/00003086-200211000-00041. [DOI] [PubMed] [Google Scholar]
- 17.Bozkurt M, Can F, Kirdemir V, et al. Conservative treatment of scapular neck fracture: the effect of stability and glenopolar angle on clinical outcome. Injury. 2005;36:1176–81. doi: 10.1016/j.injury.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 18.Pace AM, Stuart R, Brownlow H. Outcome of glenoid neck fractures. J Shoulder Elbow Surg. 2005;14:585–90. doi: 10.1016/j.jse.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 19.McGahan JP, Rab GT, Dublin A. Fractures of the scapula. J Trauma. 1980;20:880–3. doi: 10.1097/00005373-198010000-00011. [DOI] [PubMed] [Google Scholar]
- 20.Armstrong CP, Van der Spuy J. The fractured scapula: importance and management based on a series of 62 patients. Injury. 1984;15:324–9. doi: 10.1016/0020-1383(84)90056-1. [DOI] [PubMed] [Google Scholar]
- 21.Gagey O, Curey JP, Mazas F. Recent fractures of the scapula. Apropos of 43 cases] Rev Chir Orthop Reparatrice Appar Mot. 1984;70:443–7. [PubMed] [Google Scholar]
- 22.Hackney RG. Advances in the understanding of throwing injuries of the shoulder. Br J Sports Med. 1996;30:282–8. doi: 10.1136/bjsm.30.4.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Matsumura N, Ikegami H, Nakamichi N, et al. Effect of shortening deformity of the clavicle on scapular kinematics: a cadaveric study. Am J Sports Med. 2010;38:1000–6. doi: 10.1177/0363546509355143. [DOI] [PubMed] [Google Scholar]
- 24.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. the upper extremity collaborative group (UECG) Am J Ind Med. 1996;29:602–8. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 25.Ristevski B, Hall JA, Pearce D, et al. The radiographic quantification of scapular malalignment after malunion of displaced clavicular shaft fractures. J Shoulder Elbow Surg. 2012. [DOI] [PubMed]
- 26.Ledger M, Leeks N, Ackland T, et al. Short malunions of the clavicle: an anatomic and functional study. J Shoulder Elbow Surg. 2005;14:349–54. doi: 10.1016/j.jse.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 27.Stephens NG, Morgan AS, Corvo P, et al. Significance of scapular fracture in the blunt-trauma patient. Ann Emerg Med. 1995;26:439–42. doi: 10.1016/S0196-0644(95)70111-7. [DOI] [PubMed] [Google Scholar]
- 28.Veysi VT, Mittal R, Agarwal S, et al. Multiple trauma and scapula fractures: so what? J Trauma. 2003;55:1145–7. doi: 10.1097/01.TA.0000044499.76736.9D. [DOI] [PubMed] [Google Scholar]
- 29.Baldwin KD, Ohman-Strickland P, Mehta S, et al. Scapula fractures: a marker for concomitant injury? a retrospective review of data in the national trauma database. J Trauma. 2008;65:430–5. doi: 10.1097/TA.0b013e31817fd928. [DOI] [PubMed] [Google Scholar]
- 30.Gottschalk HP, Dumont G, Khanani S, et al. Open clavicle fractures: patterns of trauma and associated injuries. J Orthop Trauma. 2012;26:107–9. doi: 10.1097/BOT.0b013e31821c0b7f. [DOI] [PubMed] [Google Scholar]
- 31.Gottschalk HP, Browne RH, Starr AJ. Shoulder girdle: patterns of trauma and associated injuries. J Orthop Trauma. 2011;25:266–71. doi: 10.1097/BOT.0b013e3181e47975. [DOI] [PubMed] [Google Scholar]
- 32.Mayo KA, Benirschke SK, Mast JW. Displaced fractures of the glenoid fossa. Results of open reduction and internal fixation. Clin Orthop Relat Res. 1998;347:122–30. doi: 10.1097/00003086-199802000-00015. [DOI] [PubMed] [Google Scholar]
- 33.Anavian J, Conflitti JM, Khanna G, et al. A reliable radiographic measurement technique for extra-articular scapular fractures. Clin Orthop Relat Res. 2011;469:3371–8. doi: 10.1007/s11999-011-1820-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bartonicek J, Fric V. Scapular body fractures: results of operative treatment. Int Orthop. 2011;35:747–53. doi: 10.1007/s00264-010-1072-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.• Armitage BM, Wijdicks CA, Tarkin IS, et al. Mapping of scapular fractures with three-dimensional computed tomography. J Bone Joint Surg Am. 2009;91:2222–8. Ninety operatively treated scapula fractures were mapped to identify common fracture patterns. Sixty-eight percent involved the inferior aspect of the glenoid neck, and 71 % involved the superior vertebral border. Seventeen percent of the patterns included articular extension, and 22 % of the fractures entered the spinoglenoid notch. Of fractures involving the inferior aspect of the glenoid neck at the lateral scapular border, 84 % traversed medially to exit just inferior to the medial extent of the scapular spine, and 59 % of these inferior neck fractures also had propagation to the inferior third of the vertebral border. Among the fractures involving the spinoglenoid notch, 60 % of the fractures of the spinoglenoid notch exited just inferior to the glenoid, 65 % extended to the superior-medial vertebral border, and 45 % extended to the inferior-medial vertebral border. [DOI] [PubMed]
- 36.Anavian J, Khanna G, Plocher EK, et al. Progressive displacement of scapula fractures. J Trauma. 2010;69:156–61. doi: 10.1097/TA.0b013e3181b40393. [DOI] [PubMed] [Google Scholar]
- 37.• Dimitroulias A, Molinero KG, Krenk DE, et al. Outcomes of nonoperatively treated displaced scapular body fractures. Clin Orthop Relat Res. 2011;469:1459–65. Thirty-two scapula fractures with moderate amounts of displacement were managed nonoperatively. All fractures healed uneventfully. The mean change from preinjury recall DASH score to final follow-up was 10.2, which is a change with minimal clinical importance. There was a correlation between the change in this score with the ISS and presence of rib fractures. (P.A.C.) While the displacement inclusion criteria for this study is less than contemporary published operative indications, this study shows that the scapula is capable of tolerating minimal to moderate displacement with little adverse sequelae. [DOI] [PMC free article] [PubMed]
- 38.Jones CB, Sietsema DL. Analysis of Operative versus Nonoperative Treatment of Displaced Scapular Fractures. Clin Orthop Relat Res. 2011. [DOI] [PMC free article] [PubMed]
- 39.Imatani RJ. Fractures of the scapula: a review of 53 fractures. J Trauma. 1975;15:473–8. doi: 10.1097/00005373-197506000-00002. [DOI] [PubMed] [Google Scholar]
- 40.Lindholm A, Leven H. Prognosis in fractures of the body and neck of the scapula. A follow-up study. Acta Chir Scand. 1974;140:33–6. [PubMed] [Google Scholar]
- 41.McGinnis M, Denton JR. Fractures of the scapula: a retrospective study of 40 fractured scapulae. J Trauma. 1989;29:1488–93. doi: 10.1097/00005373-198911000-00006. [DOI] [PubMed] [Google Scholar]
- 42.Wilber MC, Evans EB. Fractures of the scapula. An analysis of forty cases and a review of the literature. J Bone Joint Surg Am. 1977;59:358–62. [PubMed] [Google Scholar]
- 43.Hardegger FH, Simpson LA, Weber BG. The operative treatment of scapular fractures. J Bone Joint Surg Br. 1984;66:725–31. doi: 10.1302/0301-620X.66B5.6501369. [DOI] [PubMed] [Google Scholar]
- 44.• Anavian J, Gauger EM, Schroder LK, et al. Surgical and functional outcomes after operative management of complex and displaced intra-articular glenoid fractures. J Bone Joint Surg Am. 2012;94:645–53. Thirty-three patients with displaced intraarticular fractures of the glenoid were treated surgically between 2002 and 2009.At a mean follow-up of 27 months (range, 12–73 months), all patients had radiographic union of the fracture. The mean DASH score was 10.8 (range, 0–42). All mean SF-36 subscores were comparable to those of the normal population. Twenty-six patients (87 %) were pain free at the time of follow-up, and 4 had mild pain with prolonged activity. Twenty-seven (90 %) of 30 patients returned to their preinjury level of work and/or activities. [DOI] [PubMed]
- 45.Ideberg R. Fractures of the scapula involving the glenoid fossa. In: Bateman JE, Welsh RP, editors. Surgery of the shoulder. Philadelphia, PA: B.C. Decker; 1984. [Google Scholar]
- 46.Goss TP. Fractures of the glenoid cavity. J Bone Joint Surg Am. 1992;74:299–305. [PubMed] [Google Scholar]
- 47.Goss T. Glenoid fractures: open reduction internal fixation. In: Wiss DA, editor. Master techniques in orthopaedic surgery: fractures. Philadelphia: Lippincot-Raven; 1998. [Google Scholar]
- 48.Kavanagh BF, Bradway JK, Cofield RH. Open reduction and internal fixation of displaced intra-articular fractures of the glenoid fossa. J Bone Joint Surg Am. 1993;75:479–84. doi: 10.2106/00004623-199304000-00001. [DOI] [PubMed] [Google Scholar]
- 49.Leung KS, Lam TP, Poon KM. Operative treatment of displaced intra-articular glenoid fractures. Injury. 1993;24:324–8. doi: 10.1016/0020-1383(93)90056-C. [DOI] [PubMed] [Google Scholar]
- 50.Adam FF. Surgical treatment of displaced fractures of the glenoid cavity. Int Orthop. 2002;26:150–3. doi: 10.1007/s00264-002-0342-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schandelmaier P, Blauth M, Schneider C, et al. Fractures of the glenoid treated by operation. A 5- to 23-year follow-up of 22 cases. J Bone Joint Surg Br. 2002;84:173–7. doi: 10.1302/0301-620X.84B2.12357. [DOI] [PubMed] [Google Scholar]
- 52.Guttentag IJ, Rechtine GR. Fractures of the scapula. A review of the literature. Orthop Rev. 1988;17:147–58. [PubMed] [Google Scholar]
- 53.DePalma A. Fractures and fracture-dislocations of the shoulder girdle. Surgery of the shoulder. 3. Philadelphia: Lippincott Company; 983. pp. 348–427. [Google Scholar]
- 54.Gramstad GD, Marra G. Treatment of glenoid fractures. Tech Shoulder Elbow Surg. 2002;3:102–10. doi: 10.1097/00132589-200206000-00006. [DOI] [Google Scholar]
- 55.Yang H, Wang D, He X. Arthroscopic-assisted reduction and percutaneous cannulated screw fixation for ideberg type III glenoid fractures a minimum 2-year follow-up of 18 cases. Am J Sports Med. 2011;39:1923–8. doi: 10.1177/0363546511408873. [DOI] [PubMed] [Google Scholar]
- 56.Carro LP, Nuñez MP, Llata J. Arthroscopic-assisted reduction and percutaneous external fixation of a displaced intra-articular glenoid fracture. Arthrosc: J Arthrosc Relat Surg. 1999;15:211–4. doi: 10.1053/ar.1999.v15.015021. [DOI] [PubMed] [Google Scholar]
- 57.Gigante A, Marinelli M, Verdenelli A, et al. Arthroscopy-assisted reduction and percutaneous fixation of a multiple glenoid fracture. Knee Surg Sports Traumatol Arthrosc. 2003;11:112–5. doi: 10.1007/s00167-002-0340-9. [DOI] [PubMed] [Google Scholar]
- 58.Yallapragada R, Patel K, Davuluri P, et al. Arthroscopy-assisted percutaneous fixation of glenoid fossa fracture. Int J Should Surg. 2007;1:96. doi: 10.4103/0973-6042.34515. [DOI] [Google Scholar]
- 59.Cole PA, Gauger EM, Herrera DA, et al. Radiographic follow-up of 84 operatively treated scapula neck and body fractures. Injury. 2012;43:327–33. doi: 10.1016/j.injury.2011.09.029. [DOI] [PubMed] [Google Scholar]
- 60.Goss TP. Double disruptions of the superior shoulder suspensory complex. J Orthop Trauma. 1993;7:99–106. doi: 10.1097/00005131-199304000-00001. [DOI] [PubMed] [Google Scholar]
- 61.Edwards SG, Whittle AP, Wood GW., 2nd Nonoperative treatment of ipsilateral fractures of the scapula and clavicle. J Bone Joint Surg Am. 2000;82:774–80. doi: 10.1302/0301-620X.82B5.11311. [DOI] [PubMed] [Google Scholar]
- 62.Williams GR, Jr, Naranja J, Klimkiewicz J, et al. The floating shoulder: a biomechanical basis for classification and management. J Bone Joint Surg Am. 2001;83-A:1182–7. doi: 10.2106/00004623-200108000-00007. [DOI] [PubMed] [Google Scholar]
- 63.Ramos L, Mencia R, Alonso A, et al. Conservative treatment of ipsilateral fractures of the scapula and clavicle. J Trauma. 1997;42:239–42. doi: 10.1097/00005373-199702000-00009. [DOI] [PubMed] [Google Scholar]
- 64.Goss TP. The scapula: coracoid, acromial, and avulsion fractures. Am J Orthop. 1996;25:106–15. [PubMed] [Google Scholar]
- 65.Ogawa K, Yoshida A, Takahashi M, et al. Fractures of the coracoid process. J Bone Joint Surg Br. 1997;79:17–9. doi: 10.1302/0301-620X.79B1.6912. [DOI] [PubMed] [Google Scholar]
- 66.Ogawa K, Naniwa T. Fractures of the acromion and the lateral scapular spine. J Shoulder Elbow Surg. 1997;6:544–8. doi: 10.1016/S1058-2746(97)90087-2. [DOI] [PubMed] [Google Scholar]
- 67.Eyres KS, Brooks A, Stanley D. Fractures of the coracoid process. J Bone Joint Surg Br. 1995;77:425–8. [PubMed] [Google Scholar]
- 68.Anavian J, Wijdicks CA, Schroder LK, et al. Surgery for scapula process fractures. Acta Orthop. 2009;80:344–50. doi: 10.3109/17453670903025394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ogawa K, Matsumura N, Ikegami H. Coracoid fractures: therapeutic strategy and surgical outcomes. J Trauma Acute Care Surg. 2012;72:E20–6. [PubMed] [Google Scholar]
- 70.Wahlquist TC, Hunt AF, Braman JP. Acromial base fractures after reverse total shoulder arthroplasty: report of five cases. J Shoulder Elbow Surg. 2011;20:1178–83. doi: 10.1016/j.jse.2011.01.029. [DOI] [PubMed] [Google Scholar]
- 71.Crosby LA, Hamilton A, Twiss T. Scapula fractures after reverse total shoulder arthroplasty: classification and treatment. Clin Orthop Relat Res. 2011;469:2544–9. doi: 10.1007/s11999-011-1881-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Boileau P, Watkinson DJ, Hatzidakis AM, et al. Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elbow Surg. 2005;14:147S–61. doi: 10.1016/j.jse.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 73.Obremskey WT, Lyman JR. A modified judet approach to the scapula. J Orthop Trauma. 2004;18:696–9. doi: 10.1097/00005131-200411000-00007. [DOI] [PubMed] [Google Scholar]
- 74.Gauger EM, Cole PA. Surgical technique: a minimally invasive approach to scapula neck and body fractures. Clin Orthop Relat Res. 2011;469:3390–9. doi: 10.1007/s11999-011-1970-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


