Abstract
Acromioclavicular (AC) joint separations are common injuries of the shoulder girdle, especially in the young and active population. Typically the mechanism of this injury is a direct force against the lateral aspect of the adducted shoulder, the magnitude of which affects injury severity. While low-grade injuries are frequently managed successfully using non-surgical measures, high-grade injuries frequently warrant surgical intervention to minimize pain and maximize shoulder function. Factors such as duration of injury and activity level should also be taken into account in an effort to individualize each patient’s treatment. A number of surgical techniques have been introduced to manage symptomatic, high-grade injuries. The purpose of this article is to review the important anatomy, biomechanical background, and clinical management of this entity.
Keywords: Acromioclavicular joint, AC joint, AC dislocation, AC separation, Shoulder separation, Rockwood classification, AC joint reconstruction, Coracoclavicular ligaments, AC joint reconstruction complications, AC joint reconstruction outcomes
Introduction
Acromioclavicular (AC) joint injuries account for nearly half of all shoulder injuries among athletes involved in contact sports [1–3]. While most injuries can be managed non-operatively, high-grade separations may result in persistent pain or functional decline and require surgical intervention [4–9]. Many surgical techniques have been described to stabilize the AC joint, however, the utility of many of these techniques are limited secondary to reported failure and complication rates [8, 10–13]. More recently, open or arthroscopically-assisted anatomic reconstruction of the coracoclavicular (CC) ligaments have been introduced and early follow-up appears encouraging [14–16]. This review provides an update on the anatomy and biomechanics of the AC joint, clinical, and surgical management of AC joint injuries, and a description of outcomes and complications following the highlighted techniques.
Anatomical and biomechanical considerations
The AC joint is a diarthrodial joint spanning from the medial articular facet of the acromion to the distal clavicle and links the shoulder girdle to the axial skeleton. It subsequently coordinates normal movement of the glenohumeral, scapulothoracic, and sternoclavicular joints. Both ends of the articular surface are covered with hyaline cartilage with an interposed fibrocartilaginous disk of widely varying sizes [17].
Stabilization of the AC joint is achieved by the joint capsule and the CC ligaments. A healthy AC joint has been shown to accommodate 4–6 mm of translation in the anterior, posterior, and superior planes under a 70 N load [18]. Furthermore, the AC joint undergoes rotary motion of 5° to 8° during scapulothoracic motion and 40° to 45° during shoulder abduction and elevation [19, 20, 21•]. It is therefore apparent that reconstructive techniques must not only be robust, but also facilitate normal kinematics. Since both the AC and CC ligament complexes are capable of load sharing, it is important to preserve or repair these structures during resection and stabilization procedures to prevent recurrent instability [22].
The superior AC ligament is the strongest, most robust ligament of the AC capsular complex and contributes to nearly 90 % of its capsuloligamentous strength [23]. Furthermore, this strength and resulting AC joint stability is reinforced by merging fibers of the deltotrapezial fascia which coalesce and intermingle with the fibers of the superior AC ligament [17]. Along with the superior AC ligament, the lesser posterior AC ligament appears to primarily restrict posterior translation while the inferior AC ligament primarily restricts anterior motion [24].
Because the AC ligaments typically fail before the CC ligaments, it is concluded that the AC ligaments are responsible for resisting quantifiably small displacement moments while the CC ligaments resist larger displacements. Therefore, complete transection of the AC ligaments renders the CC ligaments responsible for anteroposterior and vertical stability [18, 23].
The CC ligaments are primarily responsible for vertical stability of the intact AC joint. These include the conoid (anteromedial) and trapezoid (posterolateral) ligaments which span from the inferior surface of the flattened distal clavicle to the base of the coracoid process. The conoid ligament is the primary structure preventing superior displacement and rotation of the distal clavicle and runs anteriorly from the centrally-situated conoid tubercle of the clavicle to the base of the coracoid process. By contrast, the trapezoid ligament is thought to primarily restrict anteroposterior translational forces across the clavicle and runs posteriorly from the posterior margin of the clavicle to the base of the coracoid process [17, 23, 25]. Rios et al. [26] determined that each ligament reliably inserts on the clavicle at a proportion of total clavicular length (17 % trapezoid, 31 % conoid) from the distal end. They concluded that this was a more accurate guide for anatomic CC ligament reconstruction when compared with reported mean distance measurements, regardless of gender.
Epidemiology
Although their incidence varies across populations, AC joint injuries account for about 12 % of all shoulder injuries in clinical practice [27] and nearly 50 % in athletes participating in contact sports [1–3]. Furthermore, this number likely underestimates the true prevalence since many individuals with minor (type I or II) injuries may not seek medical attention [28]. AC joint injuries are much more common in men, likely due to risk-taking behaviors and participation in contact sports. The third decade of life seems to produce the greatest number of AC joint injuries. The sports most likely to cause AC joint dislocations are football, soccer, hockey, rugby, and skiing, among others [9, 28, 29].
The major cause of an AC joint separation is a direct blow to the lateral acromion with the arm in an adducted position. The inherent strength of the sternoclavicular joint renders the AC joint, CC ligaments, and/or clavicle the most likely points of injury.
Classification
Numerous classifications systems have been described for AC joint separation injuries. In 1963, Tossy, Mead, and Sigmond [30] first described 3 classes of injuries to which Rockwood [31] included 3 subdivisions. The resulting Rockwood classification, developed in 1984, is the most widely utilized and will be described here (Fig. 1).
Fig. 1.
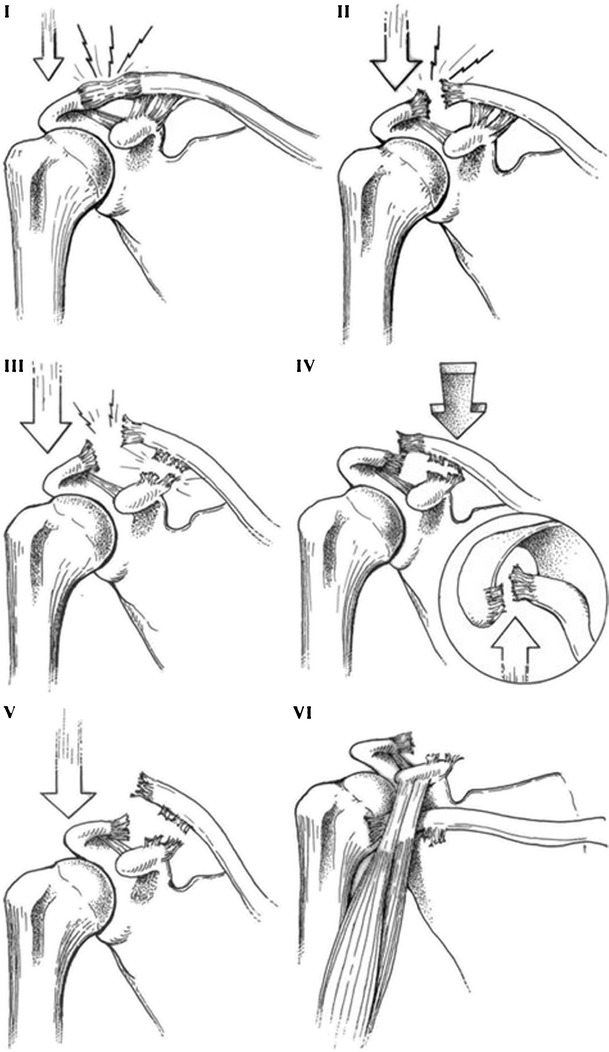
Rockwood [31] classification of AC joint injuries (Reprinted from [62], with permission)
The Rockwood classification orients the clinician to the direction and degree of displacement as determined AP, axillary, and Zanca radiographs. Type I injuries involve a sprain or partial tear of the joint capsule in which no clinical or radiographic evidence of instability exists. Type II injuries result in complete tears of the AC ligaments without disruption of the CC ligaments. Because the CC ligaments are intact, minimal radiographic depression of the acromion is apparent. Stress views can sometimes demonstrate this type although they do not typically affect the treatment. In Type III injuries, both the AC and CC ligament complexes are torn. This often results in displacement of the clavicle with increases in the CC distance that may be up to 100 % greater than the normal contralateral side. Type IV injuries are characterized by complete posterior displacement of the distal clavicle, frequently with a hole in the trapezial fascia. Type V injuries also result in complete disruption of the AC and CC ligaments with a CC distance between 100 % and 300 % greater than the uninjured side. Sometimes, these injuries result in the distal clavicle buttonholing through the deltotrapezial fascia rendering them irreducible. Type VI injuries are the result of inferior displacement of the distal clavicle into a subcoracoid position. Fortunately, these are exceedingly rare. Of note, type III–VI injuries result in the trapezius and deltoid becoming detached from the distal clavicle [31]. It is important to realize that with greater injury severity there is a greater risk for intra-articular glenohumeral injuries that may require concomitant management.
Clinical presentation
Physical examination findings are widely variable and are often dependent on injury severity and the presence of concomitant pathologies. These injuries are generally not subtle and are thus easily diagnosed by inspection and palpation. It is always important to evaluate neurovascular structures as the brachial plexus and subclavian arteries traverse inferior to the medial third of the clavicle and could be injured in rare cases. Concomitant injuries such as intra-articular, shoulder girdle, and pulmonary injuries (including tension pneumothorax) have been reported in the literature and should be promptly ruled out [32–34].
The patient typically presents using their contralateral hand to support the elbow from beneath the injured shoulder. Shortness of breath should alert the orthopedist to a potential pulmonary contusion or pneumothorax. Abrasions, swelling, and ecchymoses may be present on a prominent distal clavicle secondary to inferior displacement of the shoulder girdle.
Tenting of the skin should alert the clinician to impending soft tissue compromise, most often due to an acute clavicular fracture. Palpation will reveal tenderness over the AC joint while range of motion is typically limited due to discomfort [32–35]. Provocative tests for AC joint pathology (cross arm adduction and loading of the AC joint) can be helpful to localize shoulder pain to the AC joint. These tests are especially useful in patients with type I and II (minor) injuries in which visible or palpable deformity may not be present [28, 29].
Finally, it is important to rule out concomitant glenohumeral injuries that may simultaneously occur with AC separation [34, 36]. A study by Tischer et al. [34] demonstrated that ancillary shoulder girdle injuries may be fairly common. In this study, 14 of 77 patients with Types III–VI injuries had concurrent intra-articular injuries with 11 having superior labral anterior posterior (SLAP) lesions. Selective injections with lidocaine may be useful in discriminating chronic AC joint pain from other pathologies causing anterior or superior shoulder pain but are rarely needed for acute injuries.
Imaging
Suspicion of AC joint injury should prompt the clinician to obtain standard AP, axillary, scapular Y, and Zanca films. The Zanca view is a simple AP film with 10o–15o cephalad tilt which removes superimposing structures and allows complete visualization of the clavicle and its corresponding articulations. Inclusion of both clavicles on 1 radiograph is also helpful for comparison to the uninjured side. An axillary view is obtained to evaluate the humeral head, glenoid surface, and degree of a potential posterior displacement of the clavicle (as in type IV injuries). It is often advocated in the literature to obtain weighted stress views of the clavicle in order to distinguish between types II and III, however, the authors do not routinely recommend these radiographs since they rarely alter the course of treatment and produce unnecessary patient discomfort.
Treatment
Historically, most studies have reported satisfactory results after nonoperative treatment for those with type I and II injuries [5, 37–40]. This typically includes brief sling immobilization and rest (1–3 weeks) followed by early range of motion exercises. Despite these encouraging reports, Mikek et al. [41] suggested that as many as half of patients with Type I or II AC joint injuries experience some degree of impaired shoulder function or pain at ten-year follow up. Furthermore, a recent study by Song et al. [42] suggested that distal clavicle excision in patients with symptomatic Type II injuries may be beneficial in certain populations. Prospective, patient centric studies are necessary to determine if early distal clavicle excision is beneficial.
Considerable controversy exists regarding the treatment of type III AC separation injuries [4, 43, 44•, 45]. Historically, most type III AC injuries were managed nonoperatively with good results [4–9, 28, 29]. Some, however, fail nonoperative treatment and therefore require surgery. Recent evidence suggests that patients with type III injuries who undergo early CC ligament reconstruction have significantly improved outcomes when compared with those who underwent a trial of therapy followed by surgical treatment greater than 3 months from the index injury [8, 46]. For this reason, surgical repair of type III AC separations may be reasonably undertaken in individuals at greater risk for functional disability such as overhead workers and athletes [4, 8, 43].
Definitive evidence defining which patients benefit from early repair of type III AC separations is not available. However, it is generally accepted that a trial of non-surgical treatment is warranted for patients with type III lesions while surgical intervention is indicated for those who experience continued instability, pain, or functional decline. Early surgical management is typically recommended for high-functioning individuals with type III injuries. Furthermore, early surgical management is also recommended for those with types IV–VI injuries since this has been shown to prevent long-term sequelae [4, 6, 8, 38, 43].
Surgical techniques
Many surgical techniques have been described for the management of symptomatic AC joint separations. Rigid CC ligament fixation using screws, Kirschner wires, or Steinman pins have fallen out of favor in clinical practice due to their high failure and complication rates [12, 47, 48]. These suboptimal outcomes are likely due to the failure of rigid fixation to accommodate the normal motions that are known to occur within AC joint [21•]. Rigid fixation therefore results in decreased patient satisfaction, function, and strength [28].
Distal clavicle excision followed by transfer of the coracoacromial (CA) ligament to the resected end of the distal clavicle was first described by Weaver and Dunn in 1972 [10]. However, the value of this technique has been questioned since failure rates as high as 30 % have been reported [8, 10] and biomechanical data has demonstrated that other reconstruction techniques provide more stable fixation constructs [49–51].
As such, multiple biomechanical studies have been conducted in recent years to find a more ideal repair technique [49, 51–54, 55•, 56–58]. At present, movement towards anatomic reconstruction of the CC ligaments has taken place secondary to time-zero biomechanical studies which have examined these repairs. Anatomic reconstruction techniques typically include the use of tendon grafts [14, 55•, 59] or cortical fixation button devices to reconstruct the anatomy of the CC ligaments and, in some reconstructions, the AC ligaments [14–16, 57, 59]. Excellent biomechanical properties have been demonstrated with these techniques [55•, 57].
Authors’ preferred surgical technique
There are many different methods to address AC instability. The technique described is the senior author’s evidence- and experience-based approach to stabilize the AC joint while simultaneously minimizing the possibility for complications. Typically, a non-irradiated tibialis anterior cadaveric allograft is used in an arthroscopically-assisted anatomic reconstruction of the CC ligaments. The patient is positioned in the modified beach chair position and, after anesthesia is induced, the operative extremity is prepped free. A standard posterior arthroscopic portal is established, the arthroscope is introduced and diagnostic arthroscopy is performed. Once concomitant intra-articular injuries are addressed, the anterior joint capsule is opened using a radiofrequency probe through the rotator interval between the middle and superior glenohumeral ligaments. The coracoid process is identified just superior to the subscapularis and initial exposure is performed. An accessory anteroinferolateral portal is established inferior to the anterolateral acromial border at the level of the coracoid. This portal is used to facilitate coracoid exposure and graft passage. The pectoralis minor and conjoined tendon attachments are preserved while skeletonizing the coracoid base. Dissection along the medial coracoid border is done cautiously to avoid inadvertent injury to the brachial plexus.
A 1.5 to 2.0 cm incision is made within Langer’s lines perpendicular to the clavicle approximately 35 mm medial to the AC joint. The AC joint capsule and any remaining deltotrapezial fascia is incised in-line with the clavicle. The anterior and posterior flaps are elevated subperiosteally as a single layer for later imbrication over the reconstructed clavicle. The distal clavicle is typically preserved as this has been shown to improve the biomechanical stability of the AC joint [55•]. When concerns about post-traumatic AC arthrosis exist, the distal clavicle is elevated from the incision and a distal clavicle excision can be performed. The anterior (lateral) and posterior (medial) deltotrapezial fascia is elevated from the clavicle over a short distance to facilitate graft passage.
Under arthroscopic visualization, a switching stick is advanced along the posterior clavicle, deep to the deltoid and medial to the border of the coracoid. A dilator is passed over the switching stick and is visualized inferior to the coracoid. The switching stick is removed and a passing suture is placed down the dilator. A grasper is used through the accessory anteroinferolateral portal and docked for subsequent graft passage. This creates a soft tissue tunnel through which the graft will pass, following the path of the conoid ligament. A second passing suture is placed from lateral and anterior on the clavicle to the lateral side of the coracoid to recreate the path of the trapezoid ligament.
We prefer to avoid tunnels in the clavicle, as described by Mazzocca et al. [55•], to avoid risk of an iatrogenic postoperative fracture which we and others have seen. An 8 mm tibialis anterior allograft is passed from posterior and medial on the clavicle around the medial aspect of the coracoid and out the accessory anterolateral portal using the previously placed passing suture. The graft is then shuttled superiorly along the lateral coracoid, deep to the deltoid, and anterior to the clavicle to recreate the trapezoid ligament. The allograft is secured to itself and tied over the top of the clavicle. The clavicle is anatomically reduced and the graft is tensioned and secured with figure-of-eight sutures. It is important to anatomically reduce the clavicle.
The free ends of the allograft may be used to reconstruct the AC capsule, however, we prefer to simply imbricate the native AC tissues since fixation to the acromion can often be challenging and, again, we have concerns about drilling tunnels into the acromion. The reconstruction can also be supplemented with specially-designed cortical fixation buttons and suture tape (Arthrex, Naples, FL). We prefer to add this through a single 3 mm drill hole in the coracoid and a single 3 mm drill hole in the clavicle.
Following the reconstruction, fluoroscopy is typically used to ensure the joint is fully reduced and the arthroscopic portals and superior incision are closed routinely.
Rehabilitation
A shoulder immobilizer is worn for 4 to 6 weeks postoperatively to minimize strain on the CC ligament reconstruction. Full passive motion in the supine position is encouraged immediately postoperatively. Active motion and strengthening in the upright position begins after the 4th postoperative week and advanced per the patient’s tolerance. Return to full sport typically occurs 4 to 6 months postoperatively.
Outcomes and complications of the modern anatomic reconstruction techniques
Several clinical trials have been published in recent years reporting early clinical results after modern anatomic reconstruction of the AC joint. Good to excellent clinical outcomes have been reported, yet complications do occur [14, 15, 59–61].
In 2010, Salzmann et al. [15] reported outcomes of the anatomic 2-bundle cortical fixation button reconstruction of acute AC joint separations. They showed satisfactory clinical results in 23 patients at a minimum of 24 months follow-up. However, an 11.5 % (3/26) revision rate included 1 coracoid fracture, 1 button slippage, and 1 wound infection. Caudal migration of the button (4 patients) or break out (1 patient) was noted in 22 %, however, these radiographic findings did not negatively influence clinical outcomes. Scheibel et al. [16] also reported on 37 patients treated for acute AC separation using a double cortical fixation button reconstruction technique. They found good to excellent early clinical outcomes (mean follow-up 26.5 months) without coracoid fracture or early loss of reduction within the first 6 weeks. The authors of this paper, however, prefer to use biological augmentation as we have found an unacceptably high failure rate with cortical fixation button devices even in acute (less than 2 weeks from injury) cases (unpublished data).
Reconstructions that incorporate a biologic graft with suture fixation (cortical fixation buttons and anchors) have shown better results. DeBerardino et al. [14] showed excellent early clinical results without complications after AC reconstruction using a hybrid device that incorporated a graft with suture fixation (GraftRope system, Arthrex Inc., Naples, FL), although concerns exist regarding coracoid fractures due to the size of the hole that needs to be drilled and the technical aspects of drilling such a hole in the base of the coracoid. Using a similar device, Cook et al. [61] found that 80 % of patients lost some degree of reduction and 40 % required revision surgery. In this series, 5 of 10 patients reported fair (1) or poor (4) results.
The potential problems of graft reconstruction techniques are supported by a recent study conducted by Milewski et al. [59] in which an anatomic graft reconstruction was performed using either 2 biotenodesis screws (by passing the graft around the coracoid process [n = 17]) or a hybrid device (GraftRope, Arthrex Inc., Naples, FL) (n = 10). They found 8 complications (80 %) in the hybrid device group including 2 coracoid fractures, 5 re-dislocations, and 1 intraoperative failure of the coracoid button fixation. There were 6 (35 %) complications in the coracoid loop group including 3 clavicle fractures, 1 loss of reduction, 1 infection and 1 case of adhesive capsulitis. Furthermore, unpublished results from this institution suggest a complication rate of 22 % (13/59) with a 79 % survivorship at 24 months in patients undergoing either suture button or tendon allograft AC reconstruction procedures. Many of the complications were similar to that of Milewski et al. [59] including coracoid and clavicular fractures, hardware failure, and symptomatic loss of reduction, however, most patients significantly improved with regard to pain, function, and return to sport.
It is evident that longer-term follow up is necessary to determine the true efficacy of these types of reconstructive procedures. The method described above by the authors of this article was developed to minimize many of these potential complications while still providing very strong fixation and biological enhancement.
Conclusion
AC joint injuries are common and numerous treatment options exist. Rockwood types I and II injury patterns should be initially managed non-surgically. Patients with these injury patterns, particularly that of type II, should be informed that a distal clavicle excision may be required at some future juncture if symptomatic post-traumatic arthrosis should develop. Surgical treatment is indicated in high-grade lesions (type IV through VI) and may be also beneficial in selected type III injuries such as those that occur in heavy laborers or high-level athletes. Today, there is a trend towards anatomic reconstruction of the CC ligaments (as opposed to the classic Weaver-Dunn CA ligament transfer) due to recent biomechanical studies which show improved kinematics and much higher ultimate failure loads. While some early outcomes reports appear encouraging, high complication rates have been reported in some series [14, 15, 59–61]. Anatomic reconstructive techniques, while developed to improve the biomechanics and decrease the risk of loss of reduction, have resulted in a unique set of complications that include migration of the cortical fixation buttons and coracoid and clavicle fractures. The anatomically-based reconstruction technique presented in this article was developed to improve the strength of fixation and to decrease loss of reduction while, at the same time, minimizing the risk of significant complications such as that of clavicle and/or coracoid fractures. Future biomechanical and clinical studies will lead us to the optimal method for treating this common sports-related shoulder injury.
Acknowledgments
Disclosure
F Martetschläger: none; TR Gaskill: none; RJ Warth: none; PJ Millett: consultant to and receives royalties from Arthrex Inc., has stock/stock options with Game Ready, VuMedi.
References
Papers of particular interest, published recently, have been highlighted as • Of importance
- 1.Agel J, Dompier TP, Dick R, Marshall SW. Descriptive epidemiology of collegiate men’s ice hockey injuries: National Collegiate Athletic Association Injury Surveillance System, 1988–1989 through 2003–2004. J Athl Train. 2007;42:241–8. [PMC free article] [PubMed] [Google Scholar]
- 2.Dick R, Romani WA, Agel J, et al. Descriptive epidemiology of collegiate men’s lacrosse injuries: National collegiate athletic association injury surveillance system, 1988–1989 through 2003–2004. J Athl Train. 2007;42:255–61. [PMC free article] [PubMed] [Google Scholar]
- 3.Kaplan LD, Flanigan DC, Norwig J, et al. Prevalence and variance of shoulder injuries in elite collegiate football players. Am J Sports Med. 2005;33:1142–6. doi: 10.1177/0363546505274718. [DOI] [PubMed] [Google Scholar]
- 4.Larsen E, Bjerg-Nielsen A, Christensen P. Conservative or surgical treatment of acromioclavicular dislocation. A prospective, controlled, randomized study. J Bone Joint Surg Am. 1986;68:552–5. [PubMed] [Google Scholar]
- 5.Lemos MJ. The evaluation and treatment of the injured acromioclavicular joint in athletes. Am J Sports Med. 1998;26:137–44. doi: 10.1177/03635465980260010801. [DOI] [PubMed] [Google Scholar]
- 6.Millett PJ, Braun S, Gobezie R, Pacheco IH. Acromioclavicular joint reconstruction with coracoacromial ligament transfer using the docking technique. BMC Musculoskelet Disord. 2009;10:6. doi: 10.1186/1471-2474-10-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Simovitch R, Sanders B, Ozbaydar M, et al. Acromioclavicular joint injuries: Diagnosis and management. J Am Acad Orthop Surg. 2009;17:207–19. doi: 10.5435/00124635-200904000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Weinstein DM, McCann PD, McIlveen SJ, et al. Surgical treatment of complete acromioclavicular dislocations. Am J Sports Med. 1995;23:324–31. doi: 10.1177/036354659502300313. [DOI] [PubMed] [Google Scholar]
- 9.Willimon SC, Gaskill TR, Millett PJ. Acromioclavicular joint injuries: Anatomy, diagnosis, and treatment. Phys Sportsmed. 2011;39:116–22. doi: 10.3810/psm.2011.02.1869. [DOI] [PubMed] [Google Scholar]
- 10.Weaver JK, Dunn HK. Treatment of acromioclavicular injuries, especially complete acromioclavicular separation. J Bone Joint Surg Am. 1972;54:1187–94. [PubMed] [Google Scholar]
- 11.Thiel E, Mutnal A, Gilot GJ. Surgical outcome following arthroscopic fixation of acromioclavicular joint disruption with the tightrope device. Orthopedics. 2011;34:e267–74. doi: 10.3928/01477447-20110526-11. [DOI] [PubMed] [Google Scholar]
- 12.Norrell H, Jr, Llewellyn RC. Migration of a threaded steinmann pin from an acromioclavicular joint into the spinal canal. A case report. J Bone Joint Surg Am. 1965;47:1024–6. [PubMed] [Google Scholar]
- 13.Gerhardt DC, VanDerWerf JD, Rylander LS, McCarty EC. Postoperative coracoid fracture after transcoracoid acromioclavicular joint reconstruction. J Shoulder Elbow Surg. 2011;20:e6–10. doi: 10.1016/j.jse.2011.01.017. [DOI] [PubMed] [Google Scholar]
- 14.DeBerardino TM, Pensak MJ, Ferreira J, Mazzocca AD. Arthroscopic stabilization of acromioclavicular joint dislocation using the AC graftrope system. J Shoulder Elbow Surg. 2010;19(2 Suppl):47–52. doi: 10.1016/j.jse.2009.12.014. [DOI] [PubMed] [Google Scholar]
- 15.Salzmann GM, Walz L, Buchmann S, et al. Arthroscopically assisted 2-bundle anatomical reduction of acute acromioclavicular joint separations. Am J Sports Med. 2010;38:1179–87. doi: 10.1177/0363546509355645. [DOI] [PubMed] [Google Scholar]
- 16.Scheibel M, Droschel S, Gerhardt C, Kraus N. Arthroscopically assisted stabilization of acute high-grade acromioclavicular joint separations. Am J Sports Med. 2011;39:1507–16. doi: 10.1177/0363546511399379. [DOI] [PubMed] [Google Scholar]
- 17.Iannotti JP, Williams GR. Disorders of the shoulder: Diagnosis and management. Philadelphia: Lippincott Williams & Wilkins; 1999. [Google Scholar]
- 18.Debski RE, Parsons IM, III, Fenwick J, Vangura A. Ligament mechanics during 3 degree-of-freedom motion at the acromioclavicular joint. Ann Biomed Eng. 2000;28:612–8. doi: 10.1114/1.1304848. [DOI] [PubMed] [Google Scholar]
- 19.Flatow EL. The biomechanics of the acromioclavicular, sternoclavicular, and scapulothoracic joints. Instr Course Lect. 1993;42:237–45. [PubMed] [Google Scholar]
- 20.Kennedy JC. Complete dislocation of the acromioclavicular joint: 14 years later. Trauma. 1968;8:311–8. [PubMed] [Google Scholar]
- 21.• Giphart JE, van der Meijden OA, Millett PJ. The effects of arm elevation on the 3-dimensional acromiohumeral distance: A biplane fluoroscopy study with normative data. J Shoulder Elbow Surg. 2012 (in press). This study quantifies the significant motion that occurs around the acromioclavicular joint which may be an explanation as to why rigid coracoclavicular fixation in acute AC joint injuries often fails. [DOI] [PubMed]
- 22.Renfree KJ, Wright TW. Anatomy and biomechanics of the acromioclavicular and sternoclavicular joints. Clin Sports Med. 2003;22:219–37. doi: 10.1016/S0278-5919(02)00104-7. [DOI] [PubMed] [Google Scholar]
- 23.Fukuda K, Craig EV, An KN, et al. Biomechanical study of the ligamentous system of the acromioclavicular joint. J Bone Joint Surg Am. 1986;68:434–40. [PubMed] [Google Scholar]
- 24.Lee KW, Debski RE, Chen CH, et al. Functional evaluation of the ligaments at the acromioclavicular joint during anteroposterior and superoinferior translation. Am J Sports Med. 1997;25:858–62. doi: 10.1177/036354659702500622. [DOI] [PubMed] [Google Scholar]
- 25.Klimkiewicz JJ, Williams GR, Sher JS, et al. The acromioclavicular capsule as a restraint to posterior translation of the clavicle: A biomechanical analysis. J Shoulder Elbow Surg. 1999;8:119–24. doi: 10.1016/S1058-2746(99)90003-4. [DOI] [PubMed] [Google Scholar]
- 26.Rios CG, Arciero RA, Mazzocca AD. Anatomy of the clavicle and coracoid process for reconstruction of the coracoclavicular ligaments. Am J Sports Med. 2007;35:811–7. doi: 10.1177/0363546506297536. [DOI] [PubMed] [Google Scholar]
- 27.Emery R. Acromioclavicular and Sternoclavicular joints. In: Copeland S, editor. Shoulder Surgery. London: WB Saunders; 1997. [Google Scholar]
- 28.Fraser-Moodie JA, Shortt NL, Robinson CM. Injuries to the acromioclavicular joint. J Bone Joint Surg Br. 2008;90:697–707. doi: 10.1302/0301-620X.90B6.20704. [DOI] [PubMed] [Google Scholar]
- 29.Mazzocca AD, Arciero RA, Bicos J. Evaluation and treatment of acromioclavicular joint injuries. Am J Sports Med. 2007;35:316–29. doi: 10.1177/0363546506298022. [DOI] [PubMed] [Google Scholar]
- 30.Tossy JD, Mead NC, Sigmond HM. Acromioclavicular separations: Useful and practical classification for treatment. Clin Orthop Relat Res. 1963;28:111–9. [PubMed] [Google Scholar]
- 31.Williams GR, Nguyen VD, Rockwood CA. Classification and radiographic analysis of acromioclavicular dislocations. Appl Radiol. 1989;18:29–34. [Google Scholar]
- 32.Ebraheim NA, An HS, Jackson WT, et al. Scapulothoracic dissociation. J Bone Joint Surg Am. 1988;70:428–32. [PubMed] [Google Scholar]
- 33.Egol KA, Connor PM, Karunakar MA, et al. The floating shoulder: Clinical and functional results. J Bone Joint Surg Am. 2001;83A:1188–94. doi: 10.2106/00004623-200108000-00008. [DOI] [PubMed] [Google Scholar]
- 34.Tischer T, Salzmann GM, El-Azab H, et al. Incidence of associated injuries with acute acromioclavicular joint dislocations types III through V. Am J Sports Med. 2009;37:136–9. doi: 10.1177/0363546508322891. [DOI] [PubMed] [Google Scholar]
- 35.Wilson KM, Colwill JC. Combined acromioclavicular dislocation with coracoclavicular ligament disruption and coracoid process fracture. Am J Sports Med. 1989;17:697–8. doi: 10.1177/036354658901700521. [DOI] [PubMed] [Google Scholar]
- 36.Pauly S, Gerhardt C, Haas NP, Scheibel M. Prevalence of concomitant intra-articular lesions in patients treated operatively for high-grade acromioclavicular joint separations. Knee Surg Sports Traumatol Arthrosc. 2009;17:513–7. doi: 10.1007/s00167-008-0666-z. [DOI] [PubMed] [Google Scholar]
- 37.Bergfeld JA, Andrish JT, Clancy WG. Evaluation of the acromioclavicular joint following first- and second-degree sprains. Am J Sports Med. 1978;6:153–9. doi: 10.1177/036354657800600402. [DOI] [PubMed] [Google Scholar]
- 38.Cox JS. The fate of the acromioclavicular joint in athletic injuries. Am J Sports Med. 1981;9:50–3. doi: 10.1177/036354658100900111. [DOI] [PubMed] [Google Scholar]
- 39.Dias JJ, Steingold RF, Richardson RA, et al. The conservative treatment of acromioclavicular dislocation. Review after 5 years. J Bone Joint Surg Br. 1987;69:719–22. doi: 10.1302/0301-620X.69B5.3680330. [DOI] [PubMed] [Google Scholar]
- 40.Glick JM, Milburn LJ, Haggerty JF, Nishimoto D. Dislocated acromioclavicular joint: Follow-up study of 35 unreduced acromioclavicular dislocations. Am J Sports Med. 1977;5:264–70. doi: 10.1177/036354657700500614. [DOI] [PubMed] [Google Scholar]
- 41.Mikek M. Long-term shoulder function after type I and II acromioclavicular joint disruption. Am J Sports Med. 2008;36:2147–50. doi: 10.1177/0363546508319047. [DOI] [PubMed] [Google Scholar]
- 42.Song HS, Song SY, Yoo YS, et al. Symptomatic residual instability with grade II acromioclavicular injury. J Orthop Sci. 2012. [DOI] [PubMed]
- 43.Bannister GC, Wallace WA, Stableforth PG, Hutson MA. The management of acute acromioclavicular dislocation. A randomized prospective controlled trial. J Bone Joint Surg Br. 1989;71:848–50. doi: 10.1302/0301-620X.71B5.2684990. [DOI] [PubMed] [Google Scholar]
- 44.Spencer EE., Jr Treatment of grade III acromioclavicular joint injuries: A systematic review. Clin Orthop Relat Res. 2007;455:38–44. doi: 10.1097/BLO.0b013e318030df83. [DOI] [PubMed] [Google Scholar]
- 45.Tibone J, Sellers R, Tonino P. Strength testing after third-degree acromioclavicular dislocations. Am J Sports Med. 1992;20:328–31. doi: 10.1177/036354659202000316. [DOI] [PubMed] [Google Scholar]
- 46.Rolf O, Hann von Weyhern A, Ewers A, et al. Acromioclavicular dislocation Rockwood III-V: Results of early vs delayed surgical treatment. Arch Orthop Trauma Surg. 2008;128:1153–7. doi: 10.1007/s00402-007-0524-3. [DOI] [PubMed] [Google Scholar]
- 47.Sethi GK, Scott SM. Subclavian artery laceration due to migration of a Hagie pin. Surgery. 1976;80:644–6. [PubMed] [Google Scholar]
- 48.Sim E, Schwarz N, Hocker K, Berzlanovich A. Repair of complete acromioclavicular separations using the acromioclavicular-hook plate. Clin Orthop Relat Res. 1995;314:134–42. [PubMed] [Google Scholar]
- 49.Grutter PW, Petersen SA. Anatomical acromioclavicular ligament reconstruction: A biomechanical comparison of reconstructive techniques of the acromioclavicular joint. Am J Sports Med. 2005;33:1723–8. doi: 10.1177/0363546505275646. [DOI] [PubMed] [Google Scholar]
- 50.Lee SJ, Nicholas SJ, Akizuki KH, et al. Reconstruction of the coracoclavicular ligaments with tendon grafts: A comparative biomechanical study. Am J Sports Med. 2003;31:648–55. doi: 10.1177/03635465030310050301. [DOI] [PubMed] [Google Scholar]
- 51.Michlitsch MG, Adamson GJ, Pink M, et al. Biomechanical comparison of a modified Weaver-Dunn and a free-tissue graft reconstruction of the acromioclavicular joint complex. Am J Sports Med. 2010;38:1196–203. doi: 10.1177/0363546509361160. [DOI] [PubMed] [Google Scholar]
- 52.Jari R, Costic RS, Rodosky MW, Debski RE. Biomechanical function of surgical procedures for acromioclavicular joint dislocations. Arthroscopy. 2004;20:237–45. doi: 10.1016/j.arthro.2004.01.011. [DOI] [PubMed] [Google Scholar]
- 53.Lee SJ, Keefer EP, McHugh MP, et al. Cyclical loading of coracoclavicular ligament reconstructions: A comparative biomechanical study. Am J Sports Med. 2008;36:1990–7. doi: 10.1177/0363546508324284. [DOI] [PubMed] [Google Scholar]
- 54.Martetschlager F, Buchholz A, Sandmann G, et al. Acromioclavicular and coracoclavicular PDS augmentation for complete AC joint dislocation showed insufficient properties in a cadaver model. Knee Surg Sports Traumatol Arthrosc. 2012 [DOI] [PubMed]
- 55.Mazzocca AD, Santangelo SA, Johnson ST, et al. A biomechanical evaluation of an anatomical coracoclavicular ligament reconstruction. Am J Sports Med. 2006;34:236–46. doi: 10.1177/0363546505281795. [DOI] [PubMed] [Google Scholar]
- 56.Motamedi AR, Blevins FT, Willis MC, et al. Biomechanics of the coracoclavicular ligament complex and augmentations used in its repair and reconstruction. Am J Sports Med. 2000;28:380–4. doi: 10.1177/03635465000280031701. [DOI] [PubMed] [Google Scholar]
- 57.Walz L, Salzmann GM, Fabbro T, et al. The anatomic reconstruction of acromioclavicular joint dislocations using 2 TightRope devices: A biomechanical study. Am J Sports Med. 2008;36:2398–406. doi: 10.1177/0363546508322524. [DOI] [PubMed] [Google Scholar]
- 58.Wellmann M, Zantop T, Weimann A, et al. Biomechanical evaluation of minimally invasive repairs for complete acromioclavicular joint dislocation. Am J Sports Med. 2007;35:955–61. doi: 10.1177/0363546506298585. [DOI] [PubMed] [Google Scholar]
- 59.Milewski MD, Tompkins M, Giugale JM, et al. Complications related to anatomic reconstruction of the coracoclavicular ligaments. Am J Sports Med. 2012. [DOI] [PubMed]
- 60.Carofino BC, Mazzocca AD. The anatomic coracoclavicular ligament reconstruction: Surgical technique and indications. J Shoulder Elbow Surg. 2010;19(2 Suppl):37–46. doi: 10.1016/j.jse.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 61.Cook JB, Shaha JS, Rowles DJ, et al. Early failures with single clavicular transosseous coracoclavicular ligament reconstruction. J Shoulder Elbow Surg. 2012. [DOI] [PubMed]
- 62.Ponce BA, Millett PJ, Warner JP. Acromioclavicular joint instability – reconstruction indications and techniques. Operative Techniques Sports Med. 2004;12:36–37. [Google Scholar]


