Abstract
Patellofemoral pain is a frequent and often challenging clinical problem. It affects females more than males and includes many different pathologic entities that result in pain in the anterior aspect of the knee. Diagnosis of the specific cause of pain can be difficult and requires assessment of lower extremity strength, alignment, and range of motion, as well as specific patella alignment, tracking, and mobility. The treatment for patellofemoral pain is usually conservative with anti-inflammatory medications, activity modification, and a specific physical therapy program focusing on strengthening and flexibility. Infrequently, surgical treatment may be indicated after a non-operative program fails. The outcomes of surgical management may include debridement, lateral release, and realignment of the extensor mechanism to unload the patellofemoral articulation are favorable.
Keywords: Anterior knee pain, Patellofemoral pain, Chondromalacia patella
Introduction
The diagnosis and treatment of patellofemoral pain is a challenging but common clinical problem. Several terms, including “anterior knee pain” and “patellofemoral pain syndrome,” are used to describe the group of related pathologic entities resulting in pain in the anterior aspect of the knee. It is a term commonly used for knee pain that cannot be attributed to a specific anatomic pathology. Often the radiologic studies are fairly inconclusive. Recently, improved magnetic resonance imaging (MRI) of cartilage has significantly increased the ability to detect early changes in articular cartilage that may explain pain in some patients.
The prevalence of anterior knee pain is higher in females and ranges between 13 % and 27 % [1, 2]. Foss [1] evaluated adolescent females during pre-participation basketball screening and found that anterior knee pain was present in 26.6 % of athletes, with patellofemoral dysfunction the most common diagnosis with an overall prevalence of 7.3 % [1]. While Hughston focused attention on extensor mechanism malalignment as the predominant source of anterior knee pain [3], other common causes of anterior knee pain include quadriceps and patellar tendonitis, Osgood-Schlatter disease, multipartite patella, synovial and fat pad impingement, plica syndrome, patellar instability, loose bodies, and articular cartilage defects or degeneration known as chondromalacia patella [1, 4, 5]. A full clinical evaluation including history and physical examination supplemented by imaging studies is essential to define the specific pathology in each patient.
Clinical evaluation
History
The patient’s description of pain is a critical component in identification of the etiology. Important details to elucidate are association with injury or activity at onset, location, quality, aggravating activities such as stairs, prolonged sitting, wearing high heels, or playing sports, and alleviating factors. Sometimes the patient will be able to point to a specific location of the pain, but often times the pain cannot be isolated as easily. A pain diagram can be useful to localize the symptoms and focus the physical examination [6]. Prior history of any specific trauma is essential, even if remote. A history of instability is particularly important. One should inquire as to when and with what motions of the knee the pain occurs; a positive “theater sign” or pain beginning after prolonged knee flexion and pain with stairs may indicate patellofemoral pathology. Full evaluation of the problem includes assessment of duration of pain, associated symptoms such as swelling and erythema, and disability caused by the pain. A complete medical and prior surgical history is essential in addition to a complete musculoskeletal history.
Physical examination
The examination begins with observation. Lower extremity alignment is assessed with the patient standing to determine coronal alignment. In this position a rough measurement of the Q-angle can also be made. The Q-angle, or quadriceps angle, is the angle formed between the patellar tendon and the resultant line of force of the quadriceps muscle [7]. The described Q-angle is difficult to measure clinically, so a surrogate is used from the anterior superior iliac spine to the center of the patella and from the center of the patella to the tibial tubercle. A normal Q-angle is approximately 15°. The patient’s gait should be assessed with respect to patella tracking, position (such as excessive patella lateralization), and femoral rotation that can identify increased femoral anteversion. In addition, gait patterns with and without orthotics are useful to determine whether they improve patellar tracking. Skin abnormalities, muscle atrophy, or other signs of asymmetry should be noted as well.
Examination of the entire lower extremity is essential. Pes planus is an important clinical finding in patients with anterior knee pain as it can lead to a functional increase in knee valgus alignment. Kosashvili [8] reported on the association of pes planus and anterior knee pain in military recruits. The prevalence of anterior knee pain was significantly different in those with and without pes planus; 4 % in control and mild pes planus groups and 7 % in moderate and severe pes planus groups. If the pes planus is flexible, it can be corrected with arch supports that may improve the functional knee alignment and alleviate symptoms.
Assessment of hip range of motion, symmetry, and strength is informative. Excessive internal rotation and lack of external rotation may indicate an increased femoral anteversion, which changes gait and also increases the forces on the patella during activity. Staheli [9] established rotational profiles in adolescents and adults and noted that normal internal rotation was between 40° and 50° and normal external rotation was 45°. Lee [10] showed in a cadaveric study that a 20° inward rotational deformity of the femur resulted in a slight increase in lateral patellofemoral contact pressure but a marked increase in patellofemoral contact pressure was seen with both 30° and 60° rotational deformity. Eckhoff [11] also reported that adult anterior knee pain was associated with increased femoral anteversion. In addition to rotational deformities of the femur, it is important to assess rotational deformities of the tibia. Turner [12] evaluated rotational profiles in patients with and without anterior knee pain and noted that those with patellofemoral pain and instability had increased external tibial torsion to 24.5° compared with 19° in normals. The combination of excessive femoral anteversion, genu valgus, and external tibial torsion results in an increased Q-angle and is known as the torsional malalignment or ‘miserable malalignment syndrome’ and can be a cause of anterior knee pain. Referred knee pain from abnormalities in the back or hip should be excluded by specific maneuvers as indicated.
Complete examination of the knee begins with range of motion. Quadriceps and extensor mechanism tightness are determined with the patient prone. Full range of motion should allow the heel to be brought near the buttocks, but comparison should be made with the contralateral asymptomatic extremity with a focus on symmetry. With the patient in a supine and relaxed position, the range of motion should again be assessed with special attention to patella tracking during flexion and extension. When the patella tracks lateral during terminal knee extension this is referred to as a “J sign” and is indicative of patellar malalignment. The Q-angle can be measured in full extension, slight flexion, and at 90° of flexion.
Tenderness to palpation of specific anatomic structures can be performed. Palpation of the medial and lateral joint lines, quadriceps insertion, patellar tendon insertion on the patella, and the tibial tubercle, pes anserinus, iliotibial band and insertion, and fat pat are essential. Absence or presence of tenderness in these locations can rule out or rule in diagnoses such as tendinopathy, fat pad impingement, plica syndrome, and Osgood-Schlatter disease. In addition, medial and lateral patellar facet tenderness and medial and lateral trochlea tenderness should be evaluated. Free nerve endings are found in the patellar tendon, retinacular tissues, pes anserinus, synovial tissues, and the fat pad [13], Dye [14] performed knee arthroscopy without anesthesia and found that the most highly sensitive structures were the fat pad and synovial tissues whereas the articular surfaces, menisci, and ligaments were much less sensitive. In patients with anterior knee pain, the fat pad and medial retinaculum have a higher concentration of pain receptors than in controls [15]. Articular cartilage is not innervated, but subchondral bone is richly innervated and can be painful when palpated.
Patella motions should be evaluated with respect to medial and lateral translation, tilt or axial plane rotation, spin or coronal plane rotation, and sagittal plane flexion [16]. Patellar translation is assessed with the patient supine and relaxed. The best way to define translation is by dividing the patellar width into 4 quadrants and assessing mobility with regard to how many quadrants of motion are present. Medial mobility may be decreased (less than 1 quadrant) with tight lateral retinacular structures whereas hypermobility may be diagnosed with greater than 3 quadrants of mobility in either direction. The medial and lateral translation test should be repeated with the knee flexed to 30° to confirm that the patella does engage in the trochlear groove and stabilize. In extension an effusion can be assessed as can a painful patellar grind test to determine patellofemoral crepitus and arthritis. Patellar axial rotation is evaluated passively by tilting the patella laterally and assessing whether or not the patella can be passively mobilized to neutral. An assessment of patellar instability should be performed. An unstable patella can co-exist with patellofemoral pain but the 2 diagnoses are generally distinct. Evaluations of patellar instability include an apprehension test as well as the moving apprehension test [17].
The remainder of a typical knee examination should be performed including a standard assessment of the anterior cruciate and posterior cruciate ligaments, medial, and lateral collateral ligaments, meniscus, posterolateral corner, and lower extremity strength. Functional tests to perform include the single-limb hop test, toe and heel walking, single-limb squat, and deep knee bend. Of particular interest is the single-limb squat test, which evaluates the hip abductor and short external rotator muscle strength. When these muscles are not strong, the knee tends to collapse into a valgus alignment, there is often poor motion control, and the patient will experience pain.
Imaging
Radiographic evaluation begins with standard plain knee radiographs. A weight-bearing anteroposterior (AP) view, a lateral view with the knee in 30° flexion, and at least 1 axial view should be obtained. A Rosenberg view is a weight-bearing posteroanterior (PA) projection with the knee in 45° flexion and is useful for evaluation of joint space narrowing [18]. The Merchant view is taken with the knee in 45° flexion with the X-ray beam angled caudad 30° [19••]. Because the patella is normally engaged within the trochlea between 15° and 20° flexion, this axial view can show only significant malalignment.
Each radiographic view has specific indices that can be measured in order to provide a diagnosis. Rough alignment can be assessed on the AP view, but for true alignment full-length weight-bearing AP films must be obtained. Concominant disease such as arthritis, tumors, oteochondritis dissecans, and loose bodies can be apparent on the initial radiographs. Additional information on the presence of arthrosis may be obtained, including patellofemoral joint space narrowing, osteophyte formation, and subchondral cyst formation.
Patella alta or baja can be evaluated by a variety of methods of the lateral x-ray. The more common methods are the Insall-Salvati ratio and the Blackburne-Peel index. The Insall-Salvati ratio [20] compares the length of the patellar tendon with the patellar height. A normal ratio is 0.8–1.2 with patella alta occurring when the ratio of the length of the tendon to the patellar height is greater than 1.2 (Fig. 1a). A modified Insall-Salvati ratio can also be calculated to determine patellar height by using the length of the patellar articular surface instead of the entire patella (Fig. 1b). The Blackburne-Peel index [21••] is calculated on the lateral view with normal values between 0.5 and 1.1. This ratio is the length of the articular surface of the patella divided by the length of the patellar tendon from the lower pole of the patella to a line extending parallel to the tibial plateau (Fig. 1c). Several studies have evaluated the ease of use of the multiple methods of assessing patellar height. Berg [22] found that the Blackburne-Peel index was the most consistent at reproducing patellar height.
Fig. 1.
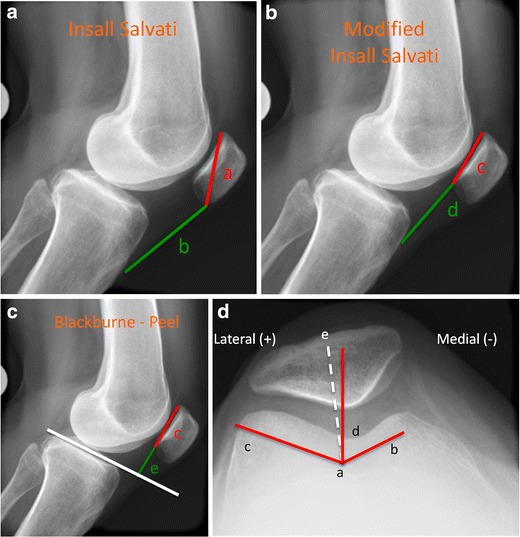
Patellofemoral radiographic measurement techniques. a Insall Salvati ratio is calculated by dividing patella length by the patellar tendon length (a/b). A normal ratio is between 0.8 and 1.2. b Modified Insall Salvati ratio is calculated by dividing the patellar articular surface length by the length of the patellar tendon (c/d). Mean normal is 1.25. c Blackburne-Peel ratio is calculated by dividing the patellar articular surface length by the length from the distal pole of the articular surface to a line extending from the tibial plateau (c/e). Normal is between 0.5 and 1.1. d The sulcus angle (b- > a- > c) helps assess femoral dysplasia. Normal is around 140°; dysplasia is indicated when the angle is larger. The congruence angle is measured between the bisector of the sulcus angle and the lowest point on the articular edge of the patella (e- > a- > d). The mean congruence angle is –6°. Medial is (–) and lateral is (+); lateral subluxation has a + angle
Patellar subluxation and trochlear dysplasia is evaluated on the axial view by measuring the congruence angle and the sulcus angle (Fig. 1d) [19••]. A different axial view, the Laurin view, taken with the knee flexed to 20°, allows better determination of lateral patellar tilt through measurement of the lateral facet angle (α angle) [23].
If the initial evaluation does not yield a diagnosis or the symptoms do not improve with conservative management, MRI may be indicated. MRI is a valuable tool because it provides 3-dimensional views, does not use ionizing radiation, and evaluates the bone as well as the soft tissues. Pihlajamaki [24] found that MRI was an accurate diagnostic tool for severe cases of chondromalacia patella although the sensitivity for low grade lesions was lower. However, this study used 1.0 Tesla magnets rather than the more detailed MRIs available currently. A more recent systematic review by Harris [25••] found that MRI is a highly sensitive, specific, and accurate modality for detection of patellofemoral chondral defects. Standardized cartilage-sensitive pulse sequences are useful as are proton density sequences that optimize visualization of the articular cartilage on the patella and trochlea [26, 27, 28••]. Fat-suppressed and T2 sequences are particularly useful on the axial view to evaluate bone edema.
MRI has largely overtaken computed tomography (CT) for diagnosis of patellofemoral pain. The exception is for assessment of bony malalignment including femoral rotation, tibial rotation, and trochlear dysplasia. The tibial tuberosity -- trochlear groove (TT-TG) distance [29] was formerly described as a CT measurement [30] but recent studies have validated the use of this measurement technique on MRI [31]. A TT-TG measurement is useful to evaluate patellar instability and is abnormal in 56 % to 93 % of patients with patellar instability [32]. A higher than normal TT TG is associated with a lateralized tibial tubercle and indicative of patellar instability that may respond to distal realignment procedures.
Nonoperative treatment
Conservative management is the mainstay of treatment for patellofemoral pain. Even patients with significant malalignment or other pathology often respond to conservative treatment. Rest, activity modification, and ice are essential components of the initial treatment. Anti-inflammatory medication is often helpful at the beginning for a few weeks to decrease inflammation, pain, and improve the patient’s ability to comply with physical therapy. Other simple interventions, such as off the shelf orthotics for pes planus, can be extremely helpful in the appropriate patients. McConnell [33] advocated a patellar taping technique to control subluxation and patellar tilt in an effort to reduce anterior knee pain. This technique is learned such that patients can apply the tape themselves. This and a variety of other taping techniques can be beneficial. Lan [34] reported a prospective cohort study on the effectiveness of taping for patellofemoral pain syndrome. Mean pain scores were significantly decreased after taping. Lan [34] concluded that taping was an effective treatment for patellofemoral pain but it was less effective in patients with a higher body mass index, larger degree of lateral tilt, and smaller Q-angle. If the response is positive from patellar taping, it may also be positive with a lateral buttress knee brace. Sleeve braces have been shown to help with patella tracking while wrap-style braces reduce peak patellofemoral pressure by changing the location of contact and pressure [35]. However, a recent randomized trial evaluating the use of bracing for patellofemoral pain associated with arthritis found no clinical benefit for bracing [36].
Physical therapy and strengthening are essential components of the non-operative management. Crossley [37•] performed a randomized trial evaluating physical therapy for the treatment of patellofemoral pain and noted that a short course of physical therapy was an effective treatment for patellofemoral pain. Specific exercises aimed at the knee such as quadriceps strengthening, quadriceps, and hamstring flexibility, lateral retinacular manual stretching in the case of patellar tilt, or tight lateral retinacula are all appropriate.
Recently, more information has emerged regarding optimizing the function of the entire lower extremity in the management of patellofemoral pain. Witvrouw [38] prospectively evaluated adolescent athletes and noted that 7 % to 10 % developed anterior knee pain. Factors that predisposed to patellofemoral pain were a shortened quadriceps muscle, an altered vastus medialis obliquus reflex response time, a decreased explosive strength, and a hypermobile patella. Van Tiggelen [39] also reported that delayed onset of electromyographic activity of the vastus medialis obliquus to vastus lateralis is a contributing factor for the development of patellofemoral pain.
Hip stability and hip strengthening are important parts of the physical therapy program. The hip extensors contribute 25 % of energy absorption during landing [40] and if the hip musculature is not strong enough to absorb the appropriate load, that load is transmitted to other joints of the lower extremity, particularly the knee. Fukuda [41] evaluated patients with patellofemoral pain who underwent a rehabilitation program focusing on knee strengthening exercises with or without hip strengthening exercises and noted that both groups had improvements in pain and function but those that received hip strengthening had significantly improved outcomes for pain relief while descending stairs. Earl [42••] found that an 8-week rehabilitation program with emphasis on strengthening and neuromuscular control of the hip and core musculature reduces the knee abduction moment, improves core and hip strength, and results in improvements in pain and functional ability.
Localized medication therapy to the knee is also an option. Corticosteroid injections are reserved for patients who have significant inflammation that has not responded well to oral anti-inflammatories, ice, and rest. Radiologic evidence of chondromalacia patella in patients who have not responded well to oral medications or a thorough physical therapy program may be an indication for hyaluronic acid injections. Although few studies exist on the efficacy of hyaluronic acid injections in the treatment of patellofemoral pain or arthritis, some data suggests that it can be useful in improving pain scores [43]. Topical non-steroidal anti-inflammatory medications such as gels or patches have been effective in some patients and offers potential relief to patients who cannot tolerate oral NSAIDS.
Nonoperative management should be pursued for at least 3 months until both clinician and patient feel that pain and function have reached a plateau. Although surgery is rarely utilized for treatment of patellofemoral pain, it should be considered in a compliant patient who has not responded well to rehabilitation.
Operative treatment
When conservative management fails to improve the patellofemoral pain, a few surgical options exist. The mainstays of surgical treatment are distal realignment or unloading procedures that offload the patellofemoral articulation by moving the tibial tubercle. Fulkerson [44] reported that 2 % of patients with patellofemoral pain require a tibial tubercle transfer. The first osteotomy described for patellofemoral pain associated with malalignment was the Elmslie-Trillat procedure [45] which involved a medial capsular reefing, lateral retinacular release, and a medial displacement of the tibial tubercle. This procedure is indicated mostly for patients with primarily lateral patellar subluxation or dislocation and without any significant patellofemoral articular damage as it moves the tibial tubercle directly medial without offloading the articular surface. There are several studies evaluating the outcomes of patients following the Elmslie-Trillat procedure with reports of recurrent instability around 9 % and improved functional outcomes [46].
Fulkerson [47••] modified the Elmslie-Trillat medialization procedure by adding a component of anteriorization to decrease the contact stresses of the patellofemoral articulation. The main indications for this procedure are persistent patellofemoral pain with associated chondromalacia patella. The most common articular cartilage abnormalities are found on the distal medial or central lateral patellar facets. This procedure allows anteriorization of the tubercle up to 15 mm, which decreases the lateral facet contact pressure. A lateral release can be added if lateral patellar tilt is present. Elevation of 12.5 mm decreases patellofemoral contact forces by 60 % to 80 % [48]. The anterior displacement offloads the distal and lateral facets while improving the extensor mechanism vector by medializing the tubercle. It is essential that the proximal medial patella articular cartilage is preserved as the load is transferred to this aspect of the patella. Outcomes following this anteromedialization of the tibial tubercle for patients with patellar malalignment and articular degeneration are generally good with 93 % good and excellent subjective outcomes and 89 % good and excellent objective outcomes [47••]. Complications of this procedure exist and include prominent hardware, tibial tubercle fracture, proximal tibia fracture, compartment syndrome, and vascular injury.
The Maquet procedure [49] is a straight anteriorization of the tibial tubercle designed to decrease the patellofemoral contact forces in patients with significant arthrosis of the patellofemoral compartments. This is of historic interest as this has no effect on the extensor mechanism alignment and also has a high rate of wound complications. Currently, the procedure of choice to offload the patellofemoral compartment is the Fulkerson osteotomy.
Lateral retinacular release alone is a controversial surgical option. An in vitro study by Ostermeier [50] showed that patellofemoral contact pressure did not change significantly with a lateral release except on the lateral facet in flexion and that it did not stabilize the patella through knee range of motion. Vaatainen [51] in a prospective study found that isolated lateral release for anterior knee pain reduced lateral patellar tilt but did not improve the functional capacity of patients at 4 years. Thus, lateral release may be indicated in patients with lateral tilt and anterior knee pain, but it should be used cautiously because it may actually worsen symptoms in the absence of lateral tilt. A lateral release has been shown to benefit less than 25 % of patients with significant patellofemoral arthrosis at long term follow up [52].
Patellofemoral arthroplasty may be considered with evidence of severe chondromalacia patella and absence of arthrosis involving the other knee compartments. Isolated patellofemoral arthrosis occurs in 9 % of symptomatic individuals over age 40 [53]. Dy [54] performed a meta-analysis of patellofemoral arthroplasty vs total knee arthroplasty in the setting of isolated patellofemoral osteoarthritis and found that the results were equivalent between second generation patellofemoral implants used today and total knee arthroplasties.
Conclusion
Patellofemoral pain is a common clinical problem that most orthopedic surgeons will face. It can be a challenging complaint because it often involves a variety of diagnoses that result in anterior knee pain. A thorough history and physical examination focusing on the alignment and strength of the lower extremity as well as specific maneuvers to assess patella mobility and tracking are essential to diagnosis. Radiographs as well as advanced imaging including MRI can evaluate the alignment as well as articular cartilage of the patellofemoral joint. Patellofemoral pain can be well treated with oral anti-inflammatory medication, activity modification, physical therapy focused on strengthening and flexibility, and, if indicated, intra-articular injections. When conservative management fails, surgical treatment in the form of distal realignment and unloading procedures are effective.
Acknowledgments
Disclosure
No potential conflicts of interest relevant to this article were reported.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Foss KB, Myer GD, Chen SS, et al. Expected prevalence from the differential diagnosis of anterior knee pain in adolescent female athletes during preparticipation screening. J Athl Train. 2012;47:519–524. doi: 10.4085/1062-6050-47.5.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roush JR, Curtis Bay R. Prevalence of anterior knee pain in 18–35 year-old females. Int J Sports Phys Ther. 2012;7:396–401. [PMC free article] [PubMed] [Google Scholar]
- 3.Hughston JC. Subluxation of the patella. J Bone Joint Surg Am. 1968;50:1003–1026. [PubMed] [Google Scholar]
- 4.Insall J, Falvo KA, Wise DW. Chondromalacia Patellae. A prospective study. J Bone Joint Surg Am. 1976;58:1–8. [PubMed] [Google Scholar]
- 5.Stanitski CL. Anterior knee pain syndromes in the adolescent. Instr Course Lect. 1994;43:211–220. [PubMed] [Google Scholar]
- 6.Post WR, Fulkerson J. Knee pain diagrams: correlation with physical examination findings in patients with anterior knee pain. Arthroscopy. 1994;10:618–623. doi: 10.1016/S0749-8063(05)80058-1. [DOI] [PubMed] [Google Scholar]
- 7.Brattstroem H. Shape of the intercondylar groove normally and in recurrent dislocation of patella. A clinical and X-ray-anatomical investigation. Acta Orthop Scand Suppl. 1964;68(Suppl 68):1–148. [PubMed] [Google Scholar]
- 8.Kosashvili Y, Fridman T, Backstein D, et al. The correlation between pes planus and anterior knee or intermittent low back pain. Foot Ankle Int. 2008;29:910–913. doi: 10.3113/FAI.2008.0910. [DOI] [PubMed] [Google Scholar]
- 9.Staheli LT, Corbett M, Wyss C, et al. Lower-extremity rotational problems in children. Normal values to guide management. J Bone Joint Surg Am. 1985;67:39–47. [PubMed] [Google Scholar]
- 10.Lee TQ, Anzel SH, Bennett KA, et al. The influence of fixed rotational deformities of the femur on the patellofemoral contact pressures in human cadaver knees. Clin Orthop Relat Res. 1994;302:69–74. [PubMed]
- 11.Eckhoff DG, Montgomery WK, Kilcoyne RF, et al. Femoral morphometry and anterior knee pain. Clin Orthop Relat Res. 1994;302:64–68. [PubMed]
- 12.Turner MS. The association between tibial torsion and knee joint pathology. Clin Orthop Relat Res. 1994;302:47–51. [PubMed]
- 13.Biedert RM, Stauffer E, Friederich NF. Occurrence of free nerve endings in the soft tissue of the knee joint. A histologic investigation. Am J Sports Med. 1992;20:430–433. doi: 10.1177/036354659202000411. [DOI] [PubMed] [Google Scholar]
- 14.Dye SF, Vaupel GL, Dye CC. Conscious neurosensory mapping of the internal structures of the human knee without intra-articular anesthesia. Am J Sports Med. 1998;26:773–777. doi: 10.1177/03635465980260060601. [DOI] [PubMed] [Google Scholar]
- 15.Witonski D, Wagrowska-Danielewicz M. Distribution of substance-P nerve fibers in the knee joint in patients with anterior knee pain syndrome. A preliminary report. Knee Surg Sports Traumatol Arthrosc. 1999;7:177–183. doi: 10.1007/s001670050144. [DOI] [PubMed] [Google Scholar]
- 16.Post WR, Teitge R, Amis A. Patellofemoral malalignment: looking beyond the view box. Clin Sports Med. 2002;21:521–546. doi: 10.1016/S0278-5919(02)00011-X. [DOI] [PubMed] [Google Scholar]
- 17.Ahmad CS, McCarthy M, Gomez JA, et al. The moving patellar apprehension test for lateral patellar instability. Am J Sports Med. 2009;37:791–796. doi: 10.1177/0363546508328113. [DOI] [PubMed] [Google Scholar]
- 18.Rosenberg TD, Paulos LE, Parker RD, et al. The forty-five-degree posteroanterior flexion weight-bearing radiograph of the knee. J Bone Joint Surg Am. 1988;70:1479–1483. [PubMed] [Google Scholar]
- 19.Merchant AC, Mercer RL, Jacobsen RH, et al. Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am. 1974;56:1391–1396. [PubMed] [Google Scholar]
- 20.Insall J, Salvati E. Patella position in the normal knee joint. Radiology. 1971;101:101–104. doi: 10.1148/101.1.101. [DOI] [PubMed] [Google Scholar]
- 21.Blackburne JS, Peel TE. A new method of measuring patellar height. J Bone Joint Surg Br. 1977;59:241–242. doi: 10.1302/0301-620X.59B2.873986. [DOI] [PubMed] [Google Scholar]
- 22.Berg EE, Mason SL, Lucas MJ. Patellar height ratios. A comparison of 4 measurement methods. Am J Sports Med. 1996;24:218–221. doi: 10.1177/036354659602400218. [DOI] [PubMed] [Google Scholar]
- 23.Laurin CA, Dussault R, Levesque HP. The tangential x-ray investigation of the patellofemoral joint: x-ray technique, diagnostic criteria and their interpretation. Clin Orthop Relat Res. 1979;144:16–26. [PubMed]
- 24.Pihlajamaki HK, Kuikka PI, Leppanen VV, et al. Reliability of clinical findings and magnetic resonance imaging for the diagnosis of chondromalacia patellae. J Bone Joint Surg Am. 2010;92:927–934. doi: 10.2106/JBJS.H.01527. [DOI] [PubMed] [Google Scholar]
- 25.Harris JD, Brophy RH, Jia G, et al. Sensitivity of magnetic resonance imaging for detection of patellofemoral articular cartilage defects. Arthroscopy. 2012;28:1728–1737. doi: 10.1016/j.arthro.2012.03.018. [DOI] [PubMed] [Google Scholar]
- 26.Bredella MA, Tirman PF, Peterfy CG, et al. Accuracy of T2-weighted fast spin-echo MR imaging with fat saturation in detecting cartilage defects in the knee: comparison with arthroscopy in 130 patients. Am J Roentgenol. 1999;172:1073–1080. doi: 10.2214/ajr.172.4.10587150. [DOI] [PubMed] [Google Scholar]
- 27.Disler DG, McCauley TR, Kelman CG, et al. Fat-suppressed 3-dimensional spoiled gradient-echo MR imaging of hyaline cartilage defects in the knee: comparison with standard MR imaging and arthroscopy. Am J Roentgenol. 1996;167:127–132. doi: 10.2214/ajr.167.1.8659356. [DOI] [PubMed] [Google Scholar]
- 28.Potter HG, Linklater JM, Allen AA, et al. Magnetic resonance imaging of articular cartilage in the knee. An evaluation with use of fast-spin-echo imaging. J Bone Joint Surg Am. 1998;80:1276–1284. doi: 10.2106/00004623-199809000-00005. [DOI] [PubMed] [Google Scholar]
- 29.Bland JM, Altman DG. Statistical methods for assessing agreement between 2 methods of clinical measurement. Lancet. 1986;1:307–310. doi: 10.1016/S0140-6736(86)90837-8. [DOI] [PubMed] [Google Scholar]
- 30.Goutallier D, Bernageau J, Lecudonnec B. The measurement of the tibial tuberosity. Patella groove distanced technique and results (author’s translation) Rev Chir Orthop Reparatrice Appar Mot. 1978;64:423–428. [PubMed] [Google Scholar]
- 31.Schoettle PB, Zanetti M, Seifert B, et al. The tibial tuberosity-trochlear groove distance; a comparative study between CT and MRI scanning. Knee. 2006;13:26–31. doi: 10.1016/j.knee.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 32.Dejour H, Walch G, Nove-Josserand L, et al. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2:19–26. doi: 10.1007/BF01552649. [DOI] [PubMed] [Google Scholar]
- 33.McConnell J. The management of chondromalacia patella: a longterm solution. Austral J Physiother. 1986;32:215–23. [DOI] [PubMed]
- 34.Lan TY, Lin WP, Jiang CC, et al. Immediate effect and predictors of effectiveness of taping for patellofemoral pain syndrome: a prospective cohort study. Am J Sports Med. 2010;38:1626–1630. doi: 10.1177/0363546510364840. [DOI] [PubMed] [Google Scholar]
- 35.Wilson NA, Mazahery BT, Koh JL, et al. Effect of bracing on dynamic patellofemoral contact mechanics. J Rehabil Res Dev. 2010;47:531–541. doi: 10.1682/JRRD.2009.12.0204. [DOI] [PubMed] [Google Scholar]
- 36.Hunter DJ, Harvey W, Gross KD, et al. A randomized trial of patellofemoral bracing for treatment of patellofemoral osteoarthritis. Osteoarthr Cartil. 2011;19:792–800. doi: 10.1016/j.joca.2010.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Crossley K, Bennell K, Green S, et al. Physical therapy for patellofemoral pain: a randomized, double-blinded, placebo-controlled trial. Am J Sports Med. 2002;30:857–865. doi: 10.1177/03635465020300061701. [DOI] [PubMed] [Google Scholar]
- 38.Witvrouw E, Lysens R, Bellemans J, et al. Intrinsic risk factors for the development of anterior knee pain in an athletic population. A 2-year prospective study. Am J Sports Med. 2000;28:480–489. doi: 10.1177/03635465000280040701. [DOI] [PubMed] [Google Scholar]
- 39.Van Tiggelen D, Cowan S, Coorevits P, et al. Delayed vastus medialis obliquus to vastus lateralis onset timing contributes to the development of patellofemoral pain in previously healthy men: a prospective study. Am J Sports Med. 2009;37:1099–1105. doi: 10.1177/0363546508331135. [DOI] [PubMed] [Google Scholar]
- 40.Zhang SN, Bates BT, Dufek JS. Contributions of lower extremity joints to energy dissipation during landings. Med Sci Sports Exerc. 2000;32:812–819. doi: 10.1097/00005768-200004000-00014. [DOI] [PubMed] [Google Scholar]
- 41.Fukuda TY, Rossetto FM, Magalhaes E, et al. Short-term effects of hip abductors and lateral rotators strengthening in females with patellofemoral pain syndrome: a randomized controlled clinical trial. J Orthop Sports Phys Ther. 2010;40:736–742. doi: 10.2519/jospt.2010.3246. [DOI] [PubMed] [Google Scholar]
- 42.Earl JE, Hoch AZ. A proximal strengthening program improves pain, function, and biomechanics in women with patellofemoral pain syndrome. Am J Sports Med. 2011;39:154–163. doi: 10.1177/0363546510379967. [DOI] [PubMed] [Google Scholar]
- 43.Clarke S, Lock V, Duddy J, et al. Intra-articular hylan G-F 20 (Synvisc) in the management of patellofemoral osteoarthritis of the knee (POAK) Knee. 2005;12:57–62. doi: 10.1016/j.knee.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 44.Fulkerson JP, Shea KP. Disorders of patellofemoral alignment. J Bone Joint Surg Am. 1990;72:1424–1429. [PubMed] [Google Scholar]
- 45.Cox JS. An evaluation of the Elmslie-Trillat procedure for management of patellar dislocations and subluxations: a preliminary report. Am J Sports Med. 1976;4:72–77. doi: 10.1177/036354657600400204. [DOI] [PubMed] [Google Scholar]
- 46.Barber FA, McGarry JE. Elmslie-Trillat procedure for the treatment of recurrent patellar instability. Arthroscopy. 2008;24:77–81. doi: 10.1016/j.arthro.2007.07.028. [DOI] [PubMed] [Google Scholar]
- 47.Fulkerson JP, Becker GJ, Meaney JA, et al. Anteromedial tibial tubercle transfer without bone graft. Am J Sports Med. 1990;18:490–496. doi: 10.1177/036354659001800508. [DOI] [PubMed] [Google Scholar]
- 48.Ferguson AB., Jr Elevation of the insertion of the patellar ligament for patellofemoral pain. J Bone Joint Surg Am. 1982;64:766–771. [PubMed] [Google Scholar]
- 49.Maquet P. Considerations biomecaniques sur l’arthrose du genou. Un traitment biomecanique de l’arthrose femoro-patellaire. L’avancement du tendon rotulien. Rev Rhum Mal Osteoartic. 1963;30:779–783. [PubMed]
- 50.Ostermeier S, Holst M, Hurschler C, et al. Dynamic measurement of patellofemoral kinematics and contact pressure after lateral retinacular release: an in vitro study. Knee Surg Sports Traumatol Arthrosc. 2007;15:547–554. doi: 10.1007/s00167-006-0261-0. [DOI] [PubMed] [Google Scholar]
- 51.Vaatainen U, Kiviranta I, Jaroma H, et al. Lateral release in chondromalacia patellae using clinical, radiologic, electromyographic, and muscle force testing evaluation. Arch Phys Med Rehabil. 1994;75:1127–1131. doi: 10.1016/0003-9993(94)90089-2. [DOI] [PubMed] [Google Scholar]
- 52.Shea KP, Fulkerson JP. Preoperative computed tomography scanning and arthroscopy in predicting outcome after lateral retinacular release. Arthroscopy. 1992;8:327–334. doi: 10.1016/0749-8063(92)90063-H. [DOI] [PubMed] [Google Scholar]
- 53.Davies AP, Vince AS, Shepstone L, et al. The radiologic prevalence of patellofemoral osteoarthritis. Clin Orthop Relat Res. 2002;402:206–212. doi: 10.1097/00003086-200209000-00020. [DOI] [PubMed] [Google Scholar]
- 54.Dy CJ, Franco N, Ma Y, et al. Complications after patello-femoral vs total knee replacement in the treatment of isolated patello-femoral osteoarthritis. A meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2012;20:2174–2190. doi: 10.1007/s00167-011-1677-8. [DOI] [PubMed] [Google Scholar]


