Abstract
The anterior cruciate ligament (ACL) is a stabilizing structure to both anterior translation of the tibia with respect to the femur as well as rotation of the knee joint. Children and adolescents are susceptible to these injuries, and there are some who believe the incidence of ACL injuries in this population is increasing due to year round single sport participation. Pediatric ACL injuries are typically seen in several forms: tibial avulsion fractures, partial ACL tears, and full thickness ligament tears. There were and still are some who feel that ACL injuries should be treated non-operatively in the pediatric and adolescent population; however, recent literature refutes this notion. Several factors must be considered during pediatric and adolescent ACL reconstruction, each of which will be examined in this manuscript, including: status of the physis, reconstruction technique, and graft source.
Keywords: Pediatric, Anterior cruciate ligament, ACL, Graft, Growth disturbance, Malalignment
Introduction
Anterior cruciate ligament injuries can be a devastating injury, with significant time lost from sport as well as potential degeneration of the knee in the future [1]. This is due not only to the meniscal and chondral damage at the time of injury but also potential changes in the kinematics of the knee due to treatment decisions [2]. ACL injuries are thought be increasing in several patient population, including pediatric and adolescents as well as in female athletes. Increasing numbers of athletes, year round sports participation, and more focus on a single sport are all theories as to why this may be occurring [3–6]. ACL injuries are one of the most researched orthopedic injuries and yet there are still many controversies surrounding the appropriate treatment of these injuries.
There are several factors that can make treating a pediatric or adolescent ACL injury more challenging. Making an accurate diagnosis can be difficult as there is a spectrum of injuries including tibial avulsions, partial ACL tears, and complete tears, and there can be multiple barriers to performing an accurate examination in this patient population. Also, there is some controversy over the appropriate treatment of these injuries in the pediatric and adolescent patient, mostly out of concern for the physis and potential growth disturbances [4, 7–9]. If surgery is chosen, there is debate over the appropriate technique as well as graft choice. Finally, the pediatric and adolescent population may have difficulty adhering to a detailed rehabilitation protocol. The purpose of this manuscript is to outline the evaluation and current evidence based management of ACL injuries in the pediatric and adolescent patient and address many of these controversies using the most recent biomechanical and clinical research.
Mechanism of injury/symptoms
The mechanism of injury can be either contact or noncontact. Most commonly, ACL tears are non-contact injuries caused by a pivoting mechanism with the knee partially flexed and the foot planted [10]. A hyperextension of the knee with a valgus or rotational force has also been described. One study demonstrated that tibial eminence fractures were more likely to occur rather than ACL tears when loading rates were slower [5, 6]. This study also noted some plastic deformation with permanent elongation of ACL fibers prior to the fracture occurring, which may cause the clinical laxity that can accompany these injuries despite anatomic fracture reduction [11–13].
Patients will typically report an audible “pop” in the knee, followed by relatively quick (12–16 hours) development of a hemarthrosis, and inability to return to sport. Weight bearing may be challenging initially, but typically is regained shortly after the injury. However, in children and adolescents, this period of inability to bear weight may be longer than in adults.
Examination
In children with a traumatic hemarthrosis of the knee, often radiographs are performed first out of fear of displacing a non-displaced tibial eminence fracture. Once this has been ruled out, a more standard knee examination can be performed. While the Lachman maneuver has classically been the test of choice for examination of ACL, the pivot shift may actually be a better determination of whether the knee is stable and the ACL is functioning [14]. Unfortunately, pivot shift examination is difficult to perform in the office setting in an acutely injured knee due to guarding of the subluxation that is caused with the maneuver. Some physicians recommend using the pivot shift as a method of determining whether a partial ACL injury is unstable enough to require a reconstruction. KT-1000 or other instrumented Lachman examination tools can also be used; however, debate remains as to whether a side to side difference of 3 mm or 5 mm is indicative of an ACL tear.
Patellar dislocations can mimic ACL tears, and thus patellar stability must be assessed. Also, a complete ligamentous examination should be performed. Some authors recommend aspiration of a hemarthrosis that may be preventing an accurate diagnosis, however, we have found this difficult to perform in an awake, alert child or adolescent in the office setting.
Imaging
AP and lateral radiographs should be obtained with weight bearing if possible. Special attention should be used to assure a perfect lateral radiograph, as this is often the best way of evaluating for and classifying tibial eminence fractures (Fig. 1).
Fig. 1.
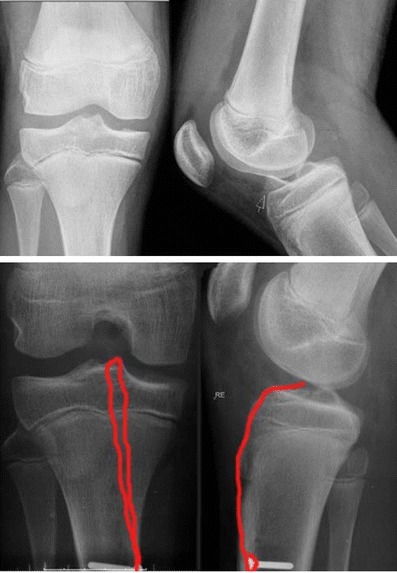
AP and lateral radiographs of the right knee of a skeletally immature athlete. The AP may be difficult to assess the displacement of the tibial eminence fracture, whereas on the lateral radiograph the fracture is easily identified. (Adapted from [15], with permission.)
Examination in the acute setting may be difficult, and thus MRI may have a more important role in a child or adolescent with a traumatic hemarthrosis. While MRI can be a useful adjunct in making an accurate diagnosis with a complete ACL tear, reports have shown poor sensitivity of MRI in detecting partial ACL tears [16, 17] (Fig. 2). MRI can also be useful in diagnosis of tibial eminence fractures, especially non-displaced, type I fractures.
Fig. 2.

Subsequent sagittal images a-c and an axial image demonstrate what appears to be an intact or partially torn ACL. At arthroscopy this patient was noted to have had a complete ACL tear. (Adapted from [18], with permission.)
Diagnosis
Diagnosis of ACL tears can be based almost completely on the history and physical examination. Over 70 % of patients with a traumatic hemarthrosis of the knee have an ACL tear [19].The addition of advanced imaging typically raises the sensitivity and specificity of diagnosing a complete ACL rupture over 90 % [20, 21].
Diagnosis of partial ACL tears is difficult. Partial ACL injuries occur on a spectrum making study of the natural history of these injuries impossible. The literature has wide ranging results of knee outcomes scores and progression to complete rupture [22–25]. While the pivot shift may be provide information as to whether a partial ACL injury should be reconstructed, the diagnosis of a partial ACL tear cannot be made based on physical examination alone. One study found that even with 75 % of the ligament torn, patients had normal Lachman and pivot shift testing [26].
Tibial eminence fractures are thought to occur most frequently between ages 8 and 14 [27] with an incidence of 3 per 100,000 children per year [28]. These injuries are classified by a system based on displacement described by Meyers and McKeever [29]. There have been modifications to this system [30], yet treatment is typically dictated by the degree of displacement and differentiating between a type I, II, and III, which are all parts of the original classification scheme. Most incomplete eminence avulsions involved disruption of the anteromedial bundle [31].
Management
Nonoperative
Most ACL injuries in the skeletally immature were previously treated without surgery. Instead, bracing, activity modification, and physical therapy were used with satisfactory short term results [32–34]. However, more recent reports of increased risk of subsequent surgery for meniscal and chondral pathology has shifted this paradigm [34–36]. Still more studies have shown that nonoperative treatment of ACL injuries can lead to chronic instability and poor outcomes, with fewer athletes able to return to their sport at the same or higher level than in those undergoing reconstruction [35, 37]. Therefore, most pediatric orthopedic physicians would strongly recommend surgical reconstruction once the diagnosis of a torn ACL is made with confirmation of a pivot shift during the examination under anesthesia. This holds true even for the pre-pubescent athlete, as results of operative management has yielded excellent outcomes without angular deformity or growth arrest [35, 38].
Partial ACL injuries should be treated based on the degree of instability in the knee. If the knee is grossly unstable with a positive pivot shift on examination, then reconstruction should be offered to the patient. In a patient where no pivot shift can be elucidated, a trial of non-operative care consisting of a physical therapy program as well as proprioception/neuromuscular re-education program can be prescribed [10, 39]. Bracing has been described as well, yet neither of these treatment modalities has any significant research demonstrating reduction of complete rupture or symptomatic instability in the setting of partial ACL tears [10, 40].
Type I, non-displaced, tibial eminence fractures are typically treated with cast immobilization, yet there is some disagreement amongst authors regarding the degree of flexion. During arthroscopy, one can see the ACL taking up tension as the knee is brought into full extension. Cadaveric work has found the greatest ACL tension at 0° or at 45° of flexion [41]; therefore, many authors recommend immobilization with casts at 10°–20° of flexion [42–44]. However, when each ACL bundle is examined independently, the AM bundle seems to tighten at about 60° of flexion, and the PL bundle tightens with extension [45]. In type II injuries with small displacements, aspiration of the hemarthosis may aid in reduction. If adequate reduction is not achieved closed, surgery is then indicated.
Operative
Once the decision to proceed with operative intervention is made, several other decisions must be made. First, surgical timing must be discussed. Most surgeons would agree that ACL reconstruction should only be performed once full motion has been regained, unless in the setting of a tibial eminence fracture or a bucket-handle meniscus tear [46, 47] (Cipolla M KSSTA 1995, Shelbourne KD AJSM 1991). Recently a report of increased risk of meniscal damage with delay in treatment of greater than 12 weeks may indicate that these injuries ought to be treated more urgently, however [48••]. Secondly, the reconstruction technique must be determined. For some authors, technique may be predicated on physeal closure status. Finally, the choice of graft must be discussed with the patient, and may partly be based on reconstruction technique chosen.
Partial ACL tear
Partial ACL tears in patients with symptomatic instability that have failed conservative management can be taken to the operating room for an examination under anesthesia. The patient should be consented for and the surgeon should be prepared to perform an ACL reconstruction and should have already discussed graft choice with the patient prior to anesthesia being administered. A pivot shift should be performed with the patient relaxed to determine the status of the ACL, which can be either functional or non-functional. The remainder of the ligament examination of the knee should be performed, including varus and valgus stress testing at 0° and 30° of flexion, as well as dial testing at 0° and 90°. If there is a 2+ pivot shift, meaning a true shift is felt rather than a glide, the surgeon should proceed with reconstruction of the ACL [49]. Intraoperatively, if only 1 bundle of the ACL is disrupted, some authors are reporting excellent results with reconstruction only of this injured bundle [10, 50]. However, some authors claim that this technique leaves too much tissue within the notch, which can limit motion [51]. Others believe that the remaining bundle that is not injured can have stretched similar to the plastic deformation that can occur with a tibial eminence fracture, and thus the remaining bundle, while present, is not functioning normally [25].
Physis status
The amount of growth remaining can be judged by a number of different methods. The Tanner staging system [52] has been used as a method for assessing growth remaining, and is one of the more common systems used in prior pediatric ACL reconstruction literature. The Risser sign has been used to correlate with the risk of progression of adolescent idiopathic scoliosis but also can be used as a measure of growth remaining [53, 54]. In females, the onset of menses can help predict growth completion. Parent height can also be a predictor of amount of growth remaining. Hand radiographs can be obtained to assign the patient a “bone age,” which can help predict the number of years of growth remaining [55]. The distal femur has been shown to grow 10 mm per year, and the proximal tibia 6 mm per year, thus allowing the physician to calculate a potential growth disturbance.
However, in ACL reconstruction, the entire physis is not obliterated as in growth modulation and thus these calculations may have no bearing. The concern that many have is that disruption of the physis in a localized area may lead to angulation or deformity rather than pure shortening of the extremity. A study evaluating Tanner stage 1 or 2 patients undergoing a transphyseal reconstruction using hamstrings graft found no growth disturbance at a minimum of 2 years from surgery [56••].
Technique
There are multiple techniques described, ranging from extra-articular reconstructions to all-physeal reconstructions to transphyseal reconstructions with various hybrid techniques described. Milewski et al. [57] proposed a treatment algorithm based on bone age. This algorithm recommends the Micheli-Kocher technique [58] for patients with a skeletal age of 6, the modified Anderson technique for skeletal age of 8, the Ganley-Lawrence All-Epiphyseal technique [59] (Fig. 3) for skeletal age of 10, a hybrid technique for skeletal age of 12, and a transphyseal technique for those of skeletal age 14 or older. (Fig. 4)
Fig. 3.
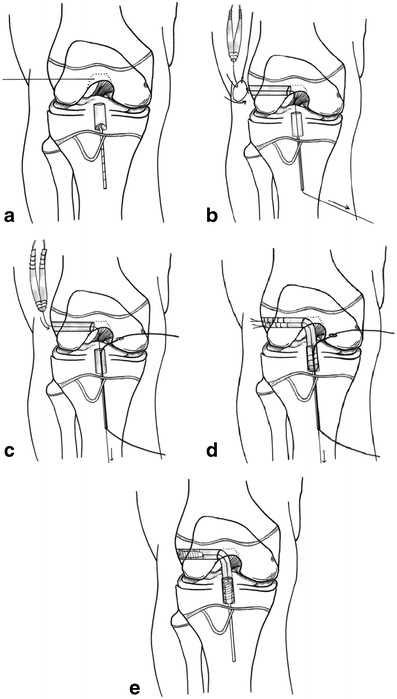
a–e The all-epiphyseal ACL reconstruction technique is shown. a A guidewire is placed in the distal femoral epiphysis parallel to the physis to the center of the femoral attachment point of the ACL. A Retrograde drill (Arthrex, Naples FL) is used in the tibia to create a tunnel in the tibial epiphysis. Proper placement can be confirmed with an intraoperative CT scan. b The femoral tunnel is drilled. A passing suture is placed up the cannulated guide pin of the Retrodrill and retrieved out the femoral tunnel. c The passing suture is used to bring a Nitinol wire and the lead sutures of the graft through the knee. The femoral end of the Nitinol wire then is retrieved out the medial portal. d The lead sutures on the graft are used to pull the graft through the femoral tunnel and into the tibial tunnel. e The Nitinol wire then is used to aid in placement of the tibial Retroscrew. The knee is brought into extension and the graft tensioned and secured in the femur with an interference screw. (Adapted from [59], with permission.)
Fig. 4.

a AP and b lateral radiographs of a skeletally immature patient treated with the transphyseal technique for ACL reconstruction
A study by Shea et al. [60••] found that even with anatomic ACL transphyseal reconstruction ,the maximum percentage of disruption of the epiphysis was 8.8 %, which occurred when using a 9 mm tunnel, yet the mean for 9 mm tunnels was 5.4 %. On the tibial side, the maximum volumetric disruption was 6.6 % using a 9 mm tunnel, with a mean of 3.8 %. The femoral tunnel was more oblique, thus accounting for the difference, as the authors simulated independent tunnel drilling which allows the tibial tunnel to be almost completely round. The obliquity and the larger amount of physis disrupted was the rational for the development of the Lawrence-Ganley all-epiphyseal technique. Less anatomic and more vertical femoral tunnel placement also decreases the percentage of the physis disrupted. However, this may lead to restoration of less desirable knee kinematics. As the purpose of ACL reconstruction in the skeletally immature patient is to provide the patient a rotationally and translationally stable knee, anatomic ACL reconstruction may be more desirable than non-anatomic vertical tunnel positioning. That said, several studies have demonstrated that even the non-anatomic reconstruction to the over the top position with an extra-articular IT band augmentation can restore near normal knee kinematics [61, 62] although 1 study found that this may overconstrain the knee [62].
Transphyseal ACL reconstruction has been found to be safe by a number of authors [63–67]. In a multi-center study, Gebhard et al. found no difference between hamstring grafts, bone-patellar tendon-bone, quadriceps tendon, and fascia lata grafts in terms of outcomes, failure, or growth disturbance [64]. These authors also found that 66 of 68 patients returned to the same level of pre-operative sport participation.
Graft source
Graft choice is somewhat dependent on reconstruction technique chosen. In the case of all-physeal or transphyseal reconstructions greater options may be present. However, there are many authors that are concerned about putting a bone plug across a growing physis with the thinking that a soft-tissue graft may have less chance of creating a bony bar and subsequent growth arrest. Soft tissue grafts have been shown to have minimal effect on growth [37, 68–70]. Several authors however have published results of using patellar tendon grafts with either periosteum [71] or bone [72], although the bone plugs were placed proximal to the physes with suture button fixation on the cortex. Neither of these studies reported any significant growth disturbances although the latter study excluded children Tanner stage 1 or 2.
Recent literature has demonstrated that allograft use in this age group leads to an unacceptable failure rate [73]. Therefore, autograft should be used if at all possible. Occasionally, hamstring tendons may be very small in this population and may need to be augmented with allograft.
Tibial eminence fracture
Many operative treatment options have been described for these fractures, including open [36, 74] or arthroscopic [42, 43] reduction and casting and open [36, 75, 76] or arthroscopic [77, 78] reduction and fixation. Fixation can be performed with sutures [77–81], (Fig. 5) metal screws [82–85], bioabsorbable nails [86], Kirschner wires [36, 41, 43, 76], or suture anchors [87, 88]. Several reports have found that screws can actually weaken the small fragment or cause comminution [78] and thus recommend suture fixation, which has demonstrated similar or improved strength profiles [89–91]. Typically some sort of visualization is required to reduce the fracture fragment as there is a high likelihood of entrapment of the intermeniscal ligament or the anterior horn of the medial or lateral meniscus [12, 84]. Most studies however, have not been able to determine a superior fixation method for these injuries and thus the surgeon must use his or her judgment based on fragment size.
Fig. 5.

a The ACL attached to the proximally displaced fracture fragment. b Two sutures through the ACL that will be used for reduction of the displaced eminence fragment. c A similar view with the sutures pulled tight and the eminence piece reduced. (Adapted from [15], with permission.)
Summary
Anterior cruciate ligament injury can present as tibial eminence fractures, partial ACL injuries, and complete ACL tears. Surgical treatment has led to improved results in those with displaced eminence fractures, partial tears with a positive pivot shift under anesthesia, and complete ACL tears. Meniscal and chondral injury along with poor long term outcomes have rendered non-operative treatment obsolete in all but a few rare circumstances. Technique for ACL reconstruction is typically based on the status of the physis, yet there is an increasing body of evidence supporting transphyseal reconstruction even in the very young patient. Graft source can depend on technique used, but should be performed with autograft tissue.
Author’s preferred technique
There is no good evidence at this time that indicates significant physeal arrest or angulatory deformities result from the relatively small violations of the tibial and femoral physes that occur during transphyseal ACL reconstruction in the skeletally immature individual. Thus, the authors use a modified transphyseal technique in all skeletally immature patients regardless of physiologic maturity or skeletal age. Autologous semitendinosus and gracilis hamstring tendons are the graft of choice for all skeletally immature patients. Allograft tissue is avoided if at all possible due to the unacceptable failure rates noted in young, active patients and the potential risk of disease transmission. An oblique, near horizontal, incision over the pes anserinus is used for hamstring harvest. Both tendons are prepared separately and then doubled to create a quadrupled graft. These are then sized using cannulae that increase in size by 0.5 mm increments to determine the the smallest possible tunnel diameter that will still allow graft passage. This is done to achieve as tight a graft fit in the tunnels as possible.
The femoral and tibial footprints are retained for placement of anatomic tunnels. The tibial tunnel guide is placed in the center of the tibial footprint, and the angle of the guide is set as steep as possible to create a more vertical tunnel. This creates a more circular tunnel and keeps the tunnel origin as far distal to the physis as possible. Care is also taken to place the starting point of the tibial tunnel somewhat more medial on the tibial metaphysis than in the adult patient so as to avoid any compromise of the tibial tubercle apophysis. A low-speed, high torque drill is used to reduce the heat produced during drilling. The femoral tunnel is drilled from a low and steeply oriented anteromedial portal. The starting point is placed within the center of the preserved anatomic footprint of the ACL. As long as the tunnel aperture is within the anatomic center of the femoral footprint the drill angle of the femoral tunnel can take any course off of this and the graft remains anatomic. Therefore, we try to create as vertical a tunnel as possible while maintaining the anatomic location of the tunnel aperture. This approach minimizes obliquity of the tunnel and results in as little cross-sectional and volume damage to the physis as possible. Again, the more vertical the tunnel, the more circular it is and the less percentile volume of physis disrupted. Alternatively, a 2 incision technique or a retrograde drilling system can be used with adherence to the same principles. The authors typically use suspensory fixation on the femoral side and a ligament staple or screw and post on the tibial side. Suspensory fixation can also be used on the tibial side. Placement of screws or other hardware across the physis is always avoided. Rehabilitation is the same as in the skeletally mature patient and is a program consisting of early motion, progressive weight bearing, and muscle strengthening.
Acknowledgments
Conflict of interest
Nathan A. Mall declares that he has no conflict of interest. George A. Paletta declares that he has no conflict of interest.
Contributor Information
Nathan A. Mall, Email: nmall@regenerationortho.com
George A. Paletta, Email: gpaletta@toc-stl.com
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
- 1.Øiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009;37:1434–43. doi: 10.1177/0363546509338827. [DOI] [PubMed] [Google Scholar]
- 2.Lohmander LS, Englund PM, Dahl LL, Roos EM. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med. 2007;35:1756–69. doi: 10.1177/0363546507307396. [DOI] [PubMed] [Google Scholar]
- 3.Anderson AF. Transepiphyseal replacement of the anterior cruciate ligament in skeletally immature patients. A preliminary report. J Bone Joint Surg Am. 2003;85-A:1255–63. doi: 10.2106/00004623-200307000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Kocher MS, Saxon HS, Hovis WD, Hawkins RJ. Management and complications of anterior cruciate ligament injuries in skeletally immature patients: survey of the Herodicus Society and the ACL Study Group. J Pediatr Orthop. 2002;22:452–7. [PubMed] [Google Scholar]
- 5.Noyes FR, DeLucas JL, Torvik PJ. Biomechanics of anterior cruciate ligament failure: an analysis of strain-rate sensitivity and mechanisms of failure in primates. J Bone Joint Surg Am. 1974;56:236–53. [PubMed] [Google Scholar]
- 6.Noyes FR, Torvik PJ, Hyde WB, DeLucas JL. Biomechanics of ligament failure. II. An analysis of immobilization, exercise, and reconditioning effects in primates. J Bone Joint Surg Am. 1974;56:1406–18. [PubMed] [Google Scholar]
- 7.Koman JD, Sanders JO. Valgus deformity after reconstruction of the anterior cruciate ligament in a skeletally immature patient. A case report. J Bone Joint Surg Am. 1999;81:711–5. doi: 10.2106/00004623-199905000-00014. [DOI] [PubMed] [Google Scholar]
- 8.Mohtadi N, Grant J. Managing anterior cruciate ligament deficiency in the skeletally immature individual: a systematic review of the literature. Clin J Sport Med. 2006;16:457–64. doi: 10.1097/01.jsm.0000248844.39498.1f. [DOI] [PubMed] [Google Scholar]
- 9.Woods GW, O'Connor DP. Delayed anterior cruciate ligament reconstruction in adolescents with open physes. Am J Sports Med. 2004;32:201–10. doi: 10.1177/0363546503258868. [DOI] [PubMed] [Google Scholar]
- 10.Tjoumakaris FP, Donegan DJ, Sekiya JK. Partial tears of the anterior cruciate ligament: diagnosis and treatment. Am J Orthop. 2011;40:92–7. [PubMed] [Google Scholar]
- 11.Perugia D, Basiglini L, Vadalà A, Ferretti A. Clinical and radiological results of arthroscopically treated tibial spine fractures in childhood. Int Orthop. 2009;33:243–8. doi: 10.1007/s00264-008-0697-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kocher MS, Micheli LJ, Gerbino P, Hresko MT. Tibial eminence fractures in children: prevalence of meniscal entrapment. Am J Sports Med. 2003;31:404–7. doi: 10.1177/03635465030310031301. [DOI] [PubMed] [Google Scholar]
- 13.Tudisco C, Giovarruscio R, Febo A, Savarese E, Bisicchia S. Intercondylar eminence avulsion fracture in children: long-term follow-up of 14 cases at the end of skeletal growth. J Pediatr Orthop B. 2010;19:403–8. doi: 10.1097/BPB.0b013e32833a5f4d. [DOI] [PubMed] [Google Scholar]
- 14.Bach BR, Warren RF, Wickiewicz TL. The pivot shift phenomenon: results and description of a modified clinical test for anterior cruciate ligament insufficiency. Am J Sports Med. 1988;16:571–6. doi: 10.1177/036354658801600603. [DOI] [PubMed] [Google Scholar]
- 15.Hirschmann MT, Mayer RR, Kentsch A, Friederich NF. Physeal sparing arthroscopic fixation of displaced tibial eminence fractures: a new surgical technique. Knee Surg Sports Traumatol Arthrosc. 2009;17:741–7. doi: 10.1007/s00167-009-0733-0. [DOI] [PubMed] [Google Scholar]
- 16.Umans H, Wimpfheimer O, Haramati N, Applbaum YH, Adler M, Bosco J. Diagnosis of partial tears of the anterior cruciate ligament of the knee: value of MR imaging. Am J Roentgenol. 1995;165:893–7. doi: 10.2214/ajr.165.4.7676988. [DOI] [PubMed] [Google Scholar]
- 17.Lawrance JA, Ostlere SJ, Dodd CA. MRI diagnosis of partial tears of the anterior cruciate ligament. Injury. 1996;27:153–5. doi: 10.1016/0020-1383(95)00220-0. [DOI] [PubMed] [Google Scholar]
- 18.Van Dyck P, Vanhoenacker FM, Gielen JL, Dossche L, Gestel JV, Wouters K, et al. Three tesla magnetic resonance imaging of the anterior cruciate ligament of the knee: can we differentiate complete from partial tears. Skeletal Radiol. 2011;40:701–7. [DOI] [PubMed]
- 19.Noyes FR, Bassett RW, Grood ES, Butler DL. Arthroscopy in acute traumatic hemarthrosis of the knee. Incidence of anterior cruciate tears and other injuries. J Bone Joint Surg Am. 1980;62:687–95. [PubMed] [Google Scholar]
- 20.Guenoun D, Le Corroller T, Amous Z, Pauly V, Sbihi A, Champsaur P. The contribution of MRI to the diagnosis of traumatic tears of the anterior cruciate ligament. Diagn Interv Imaging. 2012;93:331–41. doi: 10.1016/j.diii.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 21.Moore SL. Imaging the anterior cruciate ligament. Orthop Clin N Am. 2002;33:663–74. doi: 10.1016/S0030-5898(02)00022-6. [DOI] [PubMed] [Google Scholar]
- 22.Bak K, Scavenius M, Hansen S, Nørring K, Jensen KH, Jørgensen U. Isolated partial rupture of the anterior cruciate ligament. Long-term follow-up of 56 cases. Knee Surg Sports Traumatol Arthrosc. 1997;5:66–71. doi: 10.1007/s001670050028. [DOI] [PubMed] [Google Scholar]
- 23.Barrack RL, Buckley SL, Bruckner JD, Kneisl JS, Alexander AH. Partial vs complete acute anterior cruciate ligament tears. The results of nonoperative treatment. J Bone Joint Surg Br. 1990;72:622–4. doi: 10.1302/0301-620X.72B4.2380216. [DOI] [PubMed] [Google Scholar]
- 24.Fritschy D, Panoussopoulos A, Wallensten R, Peter R. Can we predict the outcome of a partial rupture of the anterior cruciate ligament? A prospective study of 43 cases. Knee Surg Sports Traumatol Arthrosc. 1997;5:2–5. doi: 10.1007/s001670050015. [DOI] [PubMed] [Google Scholar]
- 25.Noyes FR, Mooar LA, Moorman CT, McGinniss GH. Partial tears of the anterior cruciate ligament. Progression to complete ligament deficiency. J Bone Joint Surg Br. 1989;71:825–33. doi: 10.1302/0301-620X.71B5.2584255. [DOI] [PubMed] [Google Scholar]
- 26.Hole RL, Lintner DM, Kamaric E, Moseley JB. Increased tibial translation after partial sectioning of the anterior cruciate ligament. The posterolateral bundle. Am J Sports Med. 1996;24:556–60. doi: 10.1177/036354659602400423. [DOI] [PubMed] [Google Scholar]
- 27.Zionts L. Fractures and dislocations about the knee. In: Green NE, Swiontkowski MR, editors. Skeletal trauma in children. Philadelphia: WB Saunders; 2009. pp. 452–5. [Google Scholar]
- 28.Skak SV, Jensen TT, Poulsen TD, Stürup J. Epidemiology of knee injuries in children. Acta Orthop Scand. 1987;58:78–81. doi: 10.3109/17453678709146348. [DOI] [PubMed] [Google Scholar]
- 29.Meyers MH, McKeever FM. Fracture of the intercondylar eminence of the tibia. J Bone Joint Surg Am. 1959;41-A:209–20. [PubMed] [Google Scholar]
- 30.Zaricznyj B. Avulsion fracture of the tibial eminence: treatment by open reduction and pinning. J Bone Joint Surg Am. 1977;59:1111–4. [PubMed] [Google Scholar]
- 31.Griffith JF, Antonio GE, Tong CWC, Ming CK. Cruciate ligament avulsion fractures. Arthroscopy. 2004;20:803–12. doi: 10.1016/j.arthro.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 32.McCarroll JR, Rettig AC, Shelbourne KD. Anterior cruciate ligament injuries in the young athlete with open physes. Am J Sports Med. 1988;16:44–7. doi: 10.1177/036354658801600107. [DOI] [PubMed] [Google Scholar]
- 33.Buckley SL, Barrack RL, Alexander AH. The natural history of conservatively treated partial anterior cruciate ligament tears. Am J Sports Med. 1989;17:221–5. doi: 10.1177/036354658901700212. [DOI] [PubMed] [Google Scholar]
- 34.Mizuta H, Kubota K, Shiraishi M, Otsuka Y, Nagamoto N, Takagi K. The conservative treatment of complete tears of the anterior cruciate ligament in skeletally immature patients. J Bone Joint Surg Br. 1995;77:890–4. [PubMed] [Google Scholar]
- 35.Vavken P, Fleming BC, Mastrangelo AN, Machan JT, Murray MM. Biomechanical outcomes after bioenhanced anterior cruciate ligament repair and anterior cruciate ligament reconstruction are equal in a porcine model. Arthroscopy. 2012;28:672–80. doi: 10.1016/j.arthro.2011.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Janarv PM, Nyström A, Werner S, Hirsch G. Anterior cruciate ligament injuries in skeletally immature patients. J Pediatr Orthop. 1996;16:673–7. doi: 10.1097/01241398-199609000-00024. [DOI] [PubMed] [Google Scholar]
- 37.Aronowitz ER, Ganley TJ, Goode JR, Gregg JR, Meyer JS. Anterior cruciate ligament reconstruction in adolescents with open physes. Am J Sports Med. 2000;28:168–75. doi: 10.1177/03635465000280020601. [DOI] [PubMed] [Google Scholar]
- 38.Kaeding CC, Flanigan D, Donaldson C. Surgical techniques and outcomes after anterior cruciate ligament reconstruction in preadolescent patients. Arthroscopy. 2010;26:1530–8. doi: 10.1016/j.arthro.2010.04.065. [DOI] [PubMed] [Google Scholar]
- 39.Mandelbaum BR, Silvers HJ, Watanabe DS, Knarr JF, Thomas SD, Griffin LY, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am J Sports Med. 2005;33:1003–10. [DOI] [PubMed]
- 40.Swirtun LR, Jansson A, Renström P. The effects of a functional knee brace during early treatment of patients with a nonoperated acute anterior cruciate ligament tear: a prospective randomized study. Clin J Sport Med. 2005;15:299–304. doi: 10.1097/01.jsm.0000180018.14394.7e. [DOI] [PubMed] [Google Scholar]
- 41.McLennan JG. Lessons learned after second-look arthroscopy in type III fractures of the tibial spine. J Pediatr Orthop. 1995;15:59–62. doi: 10.1097/01241398-199501000-00013. [DOI] [PubMed] [Google Scholar]
- 42.Meyers MH, McKeever FM. Fracture of the intercondylar eminence of the tibia. J Bone Joint Surg Am. 1970;52:1677–84. [PubMed] [Google Scholar]
- 43.Willis RB, Blokker C, Stoll TM, Paterson DC, Galpin RD. Long-term follow-up of anterior tibial eminence fractures. J Pediatr Orthop. 1993;13:361–4. doi: 10.1097/01241398-199305000-00016. [DOI] [PubMed] [Google Scholar]
- 44.Beaty JH, Kumar A. Fractures about the knee in children. J Bone Joint Surg Am. 1994;76:1870–80. doi: 10.2106/00004623-199412000-00016. [DOI] [PubMed] [Google Scholar]
- 45.Gabriel MT, Wong EK, Woo SL-Y, Yagi M, Debski RE. Distribution of in situ forces in the anterior cruciate ligament in response to rotatory loads. J Orthop Res. 2004;22:85–9. doi: 10.1016/S0736-0266(03)00133-5. [DOI] [PubMed] [Google Scholar]
- 46.Shelbourne KD, Wilckens JH, Mollabashy A, DeCarlo M. Arthrofibrosis in acute anterior cruciate ligament reconstruction. The effect of timing of reconstruction and rehabilitation. Am J Sports Med. 1991;19:332–6. doi: 10.1177/036354659101900402. [DOI] [PubMed] [Google Scholar]
- 47.Cipolla M, Scala A, Gianni E, Puddu G. Different patterns of meniscal tears in acute anterior cruciate ligament (ACL) ruptures and in chronic ACL-deficient knees. Classification, staging, and timing of treatment. Knee Surg Sports Traumatol Arthrosc. 1995;3:130–4. doi: 10.1007/BF01565470. [DOI] [PubMed] [Google Scholar]
- 48.Lawrence JTR, Argawal N, Ganley TJ. Degeneration of the knee joint in skeletally immature patients with a diagnosis of an anterior cruciate ligament tear: is there harm in delay of treatment? Am J Sports Med. 2011;39:2582–7. doi: 10.1177/0363546511420818. [DOI] [PubMed] [Google Scholar]
- 49.DeFranco MJ, Bach BR. A comprehensive review of partial anterior cruciate ligament tears. J Bone Joint Surg Am. 2009;91:198–208. doi: 10.2106/JBJS.H.00819. [DOI] [PubMed] [Google Scholar]
- 50.Buda R, Ferruzzi A, Vannini F, Zambelli L, Di Caprio F. Augmentation technique with semitendinosus and gracilis tendons in chronic partial lesions of the ACL: clinical and arthrometric analysis. Knee Surg Sports Traumatol Arthrosc. 2006;14:1101–7. doi: 10.1007/s00167-006-0117-7. [DOI] [PubMed] [Google Scholar]
- 51.Busch MT, Fernandez MD, Aarons C. Partial tears of the anterior cruciate ligament in children and adolescents. Clin Sports Med. 2011;30:743–50. doi: 10.1016/j.csm.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 52.Tanner JM, Whitehouse RH. Clinical longitudinal standards for height, weight, height velocity, weight velocity, and stages of puberty. Arch Dis Child. 1976;51:170–9. doi: 10.1136/adc.51.3.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Risser JC. The Iliac apophysis; an invaluable sign in the management of scoliosis. Clin Orthop. 1958;11:111–9. [PubMed] [Google Scholar]
- 54.Scoles PV, Salvagno R, Villalba K, Riew D. Relationship of iliac crest maturation to skeletal and chronologic age. J Pediatr Orthop. 1988;8:639–44. doi: 10.1097/01241398-198811000-00002. [DOI] [PubMed] [Google Scholar]
- 55.Gruelich WW, Pyle SI. Radiographic atlas of skeletal development of the hand and wrist. 2. Stanford: Stanford University Press; 1959. [Google Scholar]
- 56.Hui C, Roe J, Ferguson D, Waller A, Salmon L, Pinczewski L. Outcome of anatomic transphyseal anterior cruciate ligament reconstruction in Tanner stage 1 and 2 patients with open physes. Am J Sports Med. 2012;40:1093–8. doi: 10.1177/0363546512438508. [DOI] [PubMed] [Google Scholar]
- 57.Milewski MD, Beck NA, Lawrence JT, Ganley TJ. Anterior cruciate ligament reconstruction in the young athlete: a treatment algorithm for the skeletally immature. Clin Sports Med. 2011;30:801–10. doi: 10.1016/j.csm.2011.08.001. [DOI] [PubMed] [Google Scholar]
- 58.Kocher MS, Garg S, Micheli LJ. Physeal sparing reconstruction of the anterior cruciate ligament in skeletally immature prepubescent children and adolescents. J Bone Joint Surg Am. 2005;87:2371–9. doi: 10.2106/JBJS.D.02802. [DOI] [PubMed] [Google Scholar]
- 59.Lawrence JTR, Bowers AL, Belding J, Cody SR, Ganley TJ. All-epiphyseal anterior cruciate ligament reconstruction in skeletally immature patients. Clin Orthop Relat Res. 2010;468:1971–7. doi: 10.1007/s11999-010-1255-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Shea KG, Belzer J, Apel PJ, Nilsson K, Grimm NL, Pfeiffer RP. Volumetric injury of the physis during single-bundle anterior cruciate ligament reconstruction in children: a 3-dimensional study using magnetic resonance imaging. Arthroscopy. 2009;25:1415–22. doi: 10.1016/j.arthro.2009.06.023. [DOI] [PubMed] [Google Scholar]
- 61.Lertwanich P, Kato Y, Martins CAQ, Maeyama A, Ingham SJM, Kramer S, et al. A biomechanical comparison of 2 femoral fixation techniques for anterior cruciate ligament reconstruction in skeletally immature patients: over-the-top fixation vs transphyseal technique. Arthroscopy. 2011;27:672–80. [DOI] [PubMed]
- 62.Kennedy A, Coughlin DG, Metzger MF, Tang R, Pearle AD, Lotz JC, et al. Biomechanical evaluation of pediatric anterior cruciate ligament reconstruction techniques. Am J Sports Med. 2011;39:964–71. [DOI] [PubMed]
- 63.Courvoisier A, Grimaldi M, Plaweski S. Good surgical outcome of transphyseal ACL reconstruction in skeletally immature patients using 4-strand hamstring graft. Knee Surg Sports Traumatol Arthrosc. 2011;19:588–91. doi: 10.1007/s00167-010-1282-2. [DOI] [PubMed] [Google Scholar]
- 64.Gebhard F, Ellermann A, Hoffmann F, Jaeger J-H, Friederich NF. Multicenter-study of operative treatment of intraligamentous tears of the anterior cruciate ligament in children and adolescents: comparison of 4 different techniques. Knee Surg Sports Traumatol Arthrosc. 2006;14:797–803. doi: 10.1007/s00167-006-0055-4. [DOI] [PubMed] [Google Scholar]
- 65.Paletta GA. Comparison of trans-physeal vs over-the-top reconstruction: Is there a difference? Big Sky, MT; 2005.
- 66.Redler LH, Brafman RT, Trentacosta N, Ahmad CS. Anterior cruciate ligament reconstruction in skeletally immature patients with transphyseal tunnels. Arthroscopy. 2012. [DOI] [PubMed]
- 67.Kocher MS, Smith JT, Zoric BJ, Lee B, Micheli LJ. Transphyseal anterior cruciate ligament reconstruction in skeletally immature pubescent adolescents. J Bone Joint Surg Am. 2007;89:2632–9. doi: 10.2106/JBJS.F.01560. [DOI] [PubMed] [Google Scholar]
- 68.Guzzanti V, Falciglia F, Gigante A, Fabbriciani C. The effect of intra-articular ACL reconstruction on the growth plates of rabbits. J Bone Joint Surg Br. 1994;76:960–3. [PubMed] [Google Scholar]
- 69.Matava MJ, Siegel MG. Arthroscopic reconstruction of the ACL with semitendinosus-gracilis autograft in skeletally immature adolescent patients. Am J Knee Surg. 1997;10:60–9. [PubMed] [Google Scholar]
- 70.Stadelmaier DM, Arnoczky SP, Dodds J, Ross H. The effect of drilling and soft tissue grafting across open growth plates. A histologic study. Am J Sports Med. 1995;23:431–5. doi: 10.1177/036354659502300410. [DOI] [PubMed] [Google Scholar]
- 71.Bonnard C, Fournier J, Babusiaux D, Planchenault M, Bergerault F, de Courtivron B. Physeal-sparing reconstruction of anterior cruciate ligament tears in children: results of 57 cases using patellar tendon. J Bone Joint Surg Br. 2011;93:542–7. doi: 10.1302/0301-620X.93B4.25801. [DOI] [PubMed] [Google Scholar]
- 72.Shelbourne KD, Gray T, Wiley BV. Results of transphyseal anterior cruciate ligament reconstruction using patellar tendon autograft in tanner stage 3 or 4 adolescents with clearly open growth plates. Am J Sports Med. 2004;32:1218–22. doi: 10.1177/0363546503262169. [DOI] [PubMed] [Google Scholar]
- 73.Kaeding CC, Aros B, Pedroza A, Pifel E, Amendola A, Andrish JT, et al. Allograft versus autograft anterior cruciate ligament reconstruction: predictors of failure from a MOON Prospective Longitudinal Cohort. Sports Health Multidiscip Approach. 2011;3:73–81. [DOI] [PMC free article] [PubMed]
- 74.Molander ML, Wallin G, Wikstad I. Fracture of the intercondylar eminence of the tibia: a review of 35 patients. J Bone Joint Surg Br. 1981;63-B:89–91. doi: 10.1302/0301-620X.63B1.7225187. [DOI] [PubMed] [Google Scholar]
- 75.Kendall NS, Hsu SY, Chan KM. Fracture of the tibial spine in adults and children. A review of 31 cases. J Bone Joint Surg Br. 1992;74:848–52. doi: 10.1302/0301-620X.74B6.1447245. [DOI] [PubMed] [Google Scholar]
- 76.Wiley JJ, Baxter MP. Tibial spine fractures in children. Clin Orthop Relat Res. 1990;255:54–60. [PubMed] [Google Scholar]
- 77.Lubowitz JH, Elson WS, Guttmann D. Part II: arthroscopic treatment of tibial plateau fractures: intercondylar eminence avulsion fractures. Arthroscopy. 2005;21:86–92. doi: 10.1016/j.arthro.2004.09.031. [DOI] [PubMed] [Google Scholar]
- 78.Berg EE. Comminuted tibial eminence anterior cruciate ligament avulsion fractures: failure of arthroscopic treatment. Arthroscopy. 1993;9:446–50. doi: 10.1016/S0749-8063(05)80320-2. [DOI] [PubMed] [Google Scholar]
- 79.Medler RG, Jansson KA. Arthroscopic treatment of fractures of the tibial spine. Arthroscopy. 1994;10:292–5. doi: 10.1016/S0749-8063(05)80114-8. [DOI] [PubMed] [Google Scholar]
- 80.Kim Y-M, Kim S-J, Yang J-Y, Kim K-C. Pullout reattachment of tibial avulsion fractures of the anterior cruciate ligament: a firm, effective suture-tying method using a tensioner. Knee Surg Sports Traumatol Arthrosc. 2007;15:847–50. doi: 10.1007/s00167-007-0315-y. [DOI] [PubMed] [Google Scholar]
- 81.Delcogliano A, Chiossi S, Caporaso A, Menghi A, Rinonapoli G. Tibial intercondylar eminence fractures in adults: arthroscopic treatment. Knee Surg Sports Traumatol Arthrosc. 2003;11:255–9. doi: 10.1007/s00167-003-0373-8. [DOI] [PubMed] [Google Scholar]
- 82.Ahmad CS, Stein BE, Jeshuran W, Nercessian OA, Henry JH. Anterior cruciate ligament function after tibial eminence fracture in skeletally mature patients. Am J Sports Med. 2001;29:339–45. doi: 10.1177/03635465010290031501. [DOI] [PubMed] [Google Scholar]
- 83.Binnet MS, Gürkan I, Yilmaz C, Karakas A, Cetin C. Arthroscopic fixation of intercondylar eminence fractures using a 4-portal technique. Arthroscopy. 2001;17:450–60. doi: 10.1053/jars.2001.23573. [DOI] [PubMed] [Google Scholar]
- 84.Senekovic V, Veselko M. Anterograde arthroscopic fixation of avulsion fractures of the tibial eminence with a cannulated screw: 5-year results. Arthroscopy. 2003;19:54–61. doi: 10.1053/jars.2003.50012. [DOI] [PubMed] [Google Scholar]
- 85.Doral MN, Atay OA, Leblebicioğlu G, Tetik O. Arthroscopic fixation of the fractures of the intercondylar eminence via transquadricipital tendinous portal. Knee Surg Sports Traumatol Arthrosc. 2001;9:346–9. doi: 10.1007/s001670100235. [DOI] [PubMed] [Google Scholar]
- 86.Liljeros K, Werner S, Janarv P-M. Arthroscopic fixation of anterior tibial spine fractures with bioabsorbable nails in skeletally immature patients. Am J Sports Med. 2009;37:923–8. doi: 10.1177/0363546508330133. [DOI] [PubMed] [Google Scholar]
- 87.Vega JR, Irribarra LA, Baar AK, Iñiguez M, Salgado M, Gana N. Arthroscopic fixation of displaced tibial eminence fractures: a new growth plate-sparing method. Arthroscopy. 2008;24:1239–43. doi: 10.1016/j.arthro.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 88.Louis M-L, Guillaume J-M, Launay F, Toth C, Jouvre J-L, Bollini G. Surgical management of type II tibial intercondylar eminence fractures in children. J Pediatr Orthop B. 2008;17:231–5. doi: 10.1097/BPB.0b013e32830b61f4. [DOI] [PubMed] [Google Scholar]
- 89.Mahar AT, Duncan D, Oka R, Lowry A, Gillingham B, Chambers H. Biomechanical comparison of four different fixation techniques for pediatric tibial eminence avulsion fractures. J Pediatr Orthop. 2008;28:159–62. doi: 10.1097/BPO.0b013e318164ee43. [DOI] [PubMed] [Google Scholar]
- 90.Eggers AK, Becker C, Weimann A, Herbort M, Zantop T, Raschke MJ, et al. Biomechanical evaluation of different fixation methods for tibial eminence fractures. Am J Sports Med. 2007;35:404–10. [DOI] [PubMed]
- 91.Bong MR, Romero A, Kubiak E, Iesaka K, Heywood CS, Kummer F, et al. Suture vs screw fixation of displaced tibial eminence fractures: a biomechanical comparison. Arthroscopy. 2005;21:1172–6. [DOI] [PubMed]


