Abstract
Acute colonic pseudo-obstruction syndrome, also known as Ogilvie’s syndrome, is a rare condition associated with significant morbidity and mortality. We report a case that developed very rapidly after emergency caesarean section. A 20-year-old woman underwent an emergency caesarean section for failure to progress in the first stage of labour and a healthy male infant was delivered without incident. However, soon afterwards the patient developed significant abdominal distension and pain. Ogilvie's syndrome was diagnosed following an abdominal x-ray which revealed a gross large bowel obstruction without mechanical cause. To prevent caecal rupture, the patient underwent successful emergency colonic decompression.
Background
Ogilvie's syndrome is a rare surgical condition that is characterised by acute obstruction and massive dilatation of the colon in the absence of mechanical causes. Its prevalence is estimated to be 0.4%.1 Ogilvie's syndrome occurs in critically ill or post-operative patients, and in obstetrics, is mostly associated with the post-operative caesarean section patient. Ogilvie's syndrome may carry a mortality rate as high as 45%2 and if the signs and symptoms are not rapidly recognised, bowel perforation, fecal peritonitis and death may result. It typically presents 2–12 days post-operatively.3 However, in contrast to the rate of progression generally reported in the literature, here we describe a case of Ogilvie's syndrome that rapidly evolved within 6 h of caesarean section but was successfully managed by colonic decompression.
Case presentation
A healthy 20-year-old primigravida presented to hospital at term with spontaneous rupture of her membranes. After 16 h in labour, she underwent an emergency caesarean section for failure to progress in the first stage of labour. The operation was uneventful, and a male infant weighing 3500 g was delivered in good condition.
At 6 h post-operatively, the patient became pyrexic and tachycardic. On examination, a significantly distended abdomen was noted, with high pitched, tinkling bowel sounds. However, her abdomen was soft and non-tender, without any signs of peritonism. An abdominal x-ray revealed grossly dilated large bowel loops, with a maximal caecal diameter of 12.8 cm (figure 1). Ogilvie's syndrome was diagnosed, and this prompted surgical referral. On surgical review, the patient had begun to develop some tenderness in the right iliac fossa and her pyrexia persisted. Therefore, she underwent urgent decompression colonoscopy under sedation, 12 h after her caesarean section. Aside from the distended bowel, no other abnormalities were found at surgery.
Figure 1.
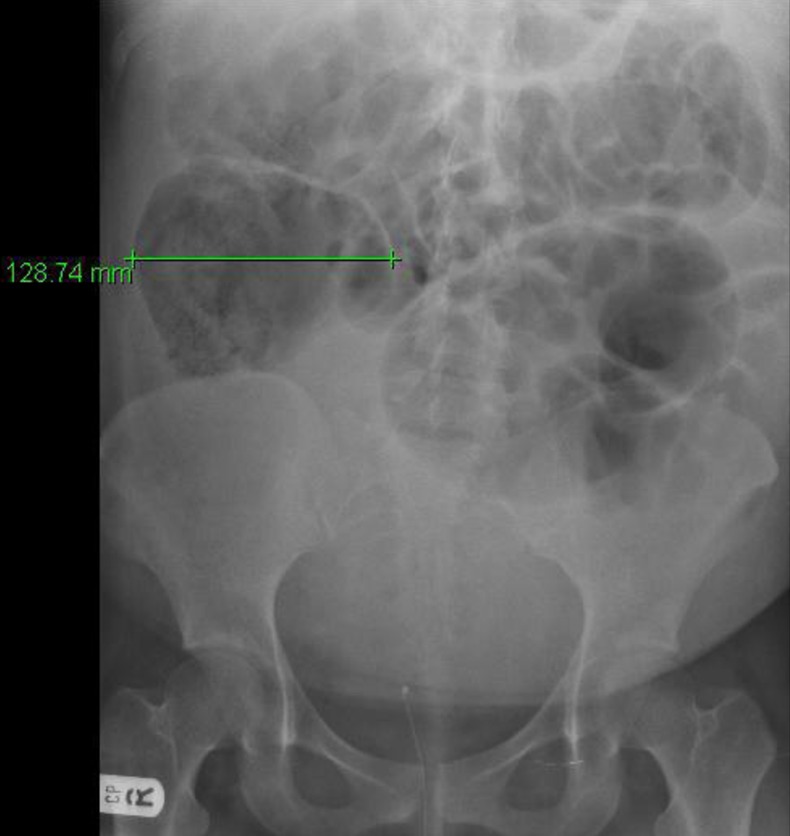
Plain abdominal x-ray showing acute colonic pseudo-obstruction.
Outcome and follow-up
The patient received 48 h of intravenous antibiotics and quickly recovered. She was discharged on day 3 with a follow-up appointment with the general surgeons 6 weeks later.
Discussion
Ogilvie's syndrome is the uncommon condition of acute pseudo-obstruction first described in 1948 by Sir William Heneage Ogilvie. However, its exact patho-physiology remains unknown. It has been suggested that it may be caused by dampened parasympathetic innervation of the colon, leading to atony of the distal colon resulting in progressive dilation of the proximal colon.2 In obstetric cases, others speculate that this autonomic imbalance may be triggered by damage to the sacral parasympathetic nerves that supply the colon and run close to the cervix, vagina and broad ligament4 and are thus at risk of injury during caesarean section.
Almost all published reports suggest that Ogilvie's syndrome typically presents within 48 h and up to 12 days post-operatively. However, as this case highlights, its onset may be as rapid as within 6 h of surgery. Plain abdominal x-ray is the most useful diagnostic tool and importantly reveals a grossly dilated large bowel, especially the caecum.
The general consensus seems to be that treatment is dictated by caecal diameter. If the caecal diameter is under 10–12 cm, then conservative treatment with intravenous fluids and electrolyte replacement and insertion of a nasogastric tube is recommended. Recently, neostigmine, an acetylcholinesterase inhibitor, given intravenously at a dose of 2 mg over 3–5 min has been shown to be effective if the caecum is not significantly over-distended.5–7
However, a caecal diameter that exceeds 10–12 cm warrants surgical treatment by colonic decompression. Should conservative management fail or if bowel perforation or peritonitis develop, then surgery is required, usually laparotomy with bowel resection. In our case, a caecal diameter above 12 cm and the development of localised tenderness in the right iliac fossa, perhaps implying impending caecal rupture, prompted urgent treatment by colonic decompression, which was successful.
Learning points.
Ogilvie's syndrome is a surgical condition characterised by acute large bowel obstruction in the absence of a mechanical cause.
Although a rare post-operative complication, Ogilvie's syndrome should always be considered in the differential diagnosis when bowel obstruction is suspected post-operatively.
Patients may rapidly deteriorate if the signs and symptoms of the syndrome are not swiftly recognised and surgery performed to avoid the high rates of morbidity and mortality associated with this condition.
The syndrome classically presents between 2 and 12 days post-operatively, but, as demonstrated in this case, may develop as soon as 6 h after a surgical procedure or insult.
With the increasing numbers of caesarean sections, Ogilvie's syndrome will be encountered more frequently in clinical practice.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Srivastava G, Pilkington D, Nallala D, et al. Ogilvie's syndrome: a case report. Arch Gynecol Obstet 2007;2013:555–7 [DOI] [PubMed] [Google Scholar]
- 2.Vanek V, Al Salti M. Acute pseudo-obstruction of the colon (Ogilvie's syndrome). Dis Colon Rectum 1986;2013:203–10 [DOI] [PubMed] [Google Scholar]
- 3.Kakarla A, Posnett H, Jain A, et al. Acute colonic pseudo-obstruction after caesarean section. Obstet Gynaecol 2006;2013:207–13 [Google Scholar]
- 4.Kadesky K, Purdue GF, Hunt JL. Acute pseudo-obstruction in critically ill patients with burns. J Burn Care Rehabil 1995;2013:132–5 [DOI] [PubMed] [Google Scholar]
- 5.Hutchinson R, Griffiths C. Acute colonic pseudo-obstruction: a pharmacological approach. Ann R Coll Eng 1992;2013:364–7 [PMC free article] [PubMed] [Google Scholar]
- 6.Ponec RJ, Saunders MD, Kimmey MB. Neostigmine for the treatment of acute colonic pseudo obstruction. N Eng J Med 1999;2013:137–41 [DOI] [PubMed] [Google Scholar]
- 7.Trevisani GT, Hyman NH, Church JM. Neostigmine: safe and effective treatment for acute pseudo-obstruction. Dis Colon Rectum 2000;2013:599–603 [DOI] [PubMed] [Google Scholar]


