Abstract
Tobacco smoking causes cardiovascular, respiratory and malignant disease, and stopping smoking is among the key medical interventions to lower the worldwide burden of these disorders. However, the addictive properties of cigarette smoking, including nicotine inhalation, render most quit attempts unsuccessful. Recommended therapies, including combinations of counselling and medication, produce long-term continuous abstinence rates of no more than 30%. Thus, more effective treatment options are needed.
An intriguing novel therapeutic concept is vaccination against nicotine. The basic principle of this approach is that, after entering the systemic circulation, a substantial proportion of nicotine can be bound by antibodies. Once bound to antibodies, nicotine is no longer able to cross the blood-brain barrier. As a consequence, the rewarding effects of nicotine are diminished, and relapse to smoking is less likely to occur. Animal studies indicate that antibodies profoundly change the pharmacokinetics of the drug and can interfere with nicotine self-administration and impact on the severity of withdrawal symptoms. To date, five phase I/II clinical trials using vaccines against nicotine have been published. Results have been disappointing in that an increase in quit rates was only observed in small groups of smokers displaying particularly high antibody titres.
The failure of encouraging preclinical data to completely translate to clinical studies may be partially explained by shortcomings of animal models of addiction and an incomplete understanding of the complex physiological and behavioural processes contributing to tobacco addiction. This review summarizes the current status of research and suggests some directions for the future development of vaccines against nicotine. Ideally, these vaccines could one day become part of a multifaceted approach to treating tobacco addiction that includes counselling and pharmacotherapy.
1. Introduction
There are currently 1 billion tobacco smokers in the world,[1] at least half of whom will eventually die from a smoking-related disease.[2] By causing cardiovascular, respiratory and malignant disease, smoking accounts for 10% of global mortality.[3] Due to its pharmacokinetic properties, nicotine that is inhaled from cigarette smoke readily evokes addiction in many smokers (see Benowitz[4] for details). Accordingly, tobacco dependence has been called a chronic disease necessitating specific treatment.[5] The treatment of tobacco use usually involves some form of counselling[6] or pharmacotherapy;[7] ideally, both approaches should be combined.[8] Currently available pharmacotherapy increases quit rates by reducing craving or providing relief from withdrawal symptoms.
Recent research regarding drugs to support quit attempts has focussed on combination therapies,[9] pharmacogenetics[10] and modifications to existing dosing regimens.[11,12] However, long-term continuous abstinence rates achieved by approved treatment options, combined with intensive counselling, rarely exceed 30%,[8] and patient adherence to treatment is modest.[13] As smokers display diverse smoking patterns[14] and different needs when trying to quit, increased diversity of treatment options would be desirable.[15] An intriguing novel concept is nicotine vaccination. The basic principle of this approach is that, after entering the systemic circulation, a substantial proportion of nicotine can be bound by antibodies. Once bound to antibodies, nicotine is no longer able to cross the blood-brain barrier. As a consequence, the rewarding effects of nicotine are diminished, and relapse to smoking is less likely to occur.[16] Preclinical experiments have yielded promising results, and, to date, five reports of phase I–II trials using nicotine vaccines in humans have been published.[17–21]
Starting from a summary of neural mechanisms involved in nicotine addiction, this review illustrates some practical aspects relevant to the design of a nicotine vaccine. An overview of principle findings from animal studies is followed by a more detailed description of clinical trial results. The article concludes with a critical appraisal of this novel therapeutic approach and some suggestions for future research.
2. Mechanisms of Nicotine Addiction
2.1 Nicotine Pharmacokinetics
Nicotine is part of the particulate phase of tobacco smoke and constitutes the most prevalent alkaloid in tobacco. It is a small molecule (162 daltons). As indicated by its chemical name, (S)-3-(1-Methylpyrrolidin-2-yl)pyridine, this natural insecticide contains a pyridine and a pyrrolidine ring, both of which are carrying a tertiary amine. The two rings possess different acid dissociation constants, producing a net acid dissociation constant (pKa) of 8.0–8.5 (for overview, please see Hukkanen et al.[22]). The acidity of cigarette smoke (pH = 5.5–6.0) prevents large doses of nicotine from being absorbed by the oral mucosa. However, in the more alkaline environment of the pulmonary alveoli (pH 7.4), one in three nicotine molecules is non-ionized and thus capable of crossing biological membranes. The average nicotine content of a cigarette is 10–14 mg,[23] only 10% of which enters the systemic circulation,[24] resulting in peak plasma concentrations of 300–500 nM.[25] Nicotine intake from one cigarette is approximately 0.015 mg per kg,[24] and this dose has been used in most preclinical studies using nicotine infusions in animals.
The amount of nicotine binding to plasma proteins is negligible (5%[26]); its half-life is 2 hours,[27] and the greater part of nicotine is metabolized to cotinine. This conversion is almost exclusively catalyzed by one specific cytochrome P450 (CYP) isoenzyme (CYP2A6).[28] The rate of nicotine metabolism is determined by genetic[29] and hormonal[30] factors as well as concomitant medication and appears to have a direct impact on the severity of withdrawal symptoms and, ultimately, the success of a quit attempt.[31,32]
2.2 Nicotine Effects on the Brain
While most pathophysiological mechanisms underlying smoking-related disease are activated by smoke constituents other than nicotine, it has been known for several decades that nicotine effects on the brain following smoke inhalation are central to the addictive properties of smoking.[33] In the broadest sense, nicotine impacts on locomotion, cognition, affect, pain sensitivity[34] and arousal.[35] Most importantly, however, nicotine increases the brain’s responsiveness to rewarding stimuli,[36] ultimately leading to addiction. Nicotine delivery kinetics to the brain appear to be crucial in facilitating this effect in that a rapid increase in nicotine levels is much more likely to promote self-administration (a laboratory paradigm for addiction) than slow kinetics.[37,38] In humans, high levels of nicotine reach the brain within 10–20 seconds after taking a puff from a cigarette.[39] In fact, most smokers report that the subjective effects of cigarette smoking are maximal in the first few minutes after smoke inhalation.[40] This has led to the assumption that nicotine effects on the brain are primarily determined by the speed at which the compound enters the brain.[41]
Various in vivo and in vitro studies performed in the mid-1980s have identified the mesocorticolimbic dopamine system as the primary site of action regarding nicotine’s reinforcing and rewarding effects.[42] This complex neuronal network involves dopaminergic neurons located in the ventral tegmental area (VTA) projecting to diverse brain regions, including the nucleus accumbens (synonyms: NAcc, ventral striatum[43]). Nicotine activates nicotinic acetylcholine receptors (nAChR)[44,45] on VTA neurons, ultimately leading to dopamine release in the NAcc.[46] Increased dopamine levels in this region generally promote the development of drug dependence.[47,48] Notwithstanding the need for a better understanding of the complex interactions of neuronal pathways leading to addiction, reward from smoking is likely to occur as a consequence of dopamine release in the NAcc following a rapid increase in brain nicotine concentration.
In addition to triggering dopamine release, nicotine induces desensitization of nAChRs and an increase in receptor density.[49] Receptor up-regulation implies the possibility of developing a hypercholinergic state when nicotine supply is interrupted. In fact, regular smokers display an almost complete receptor saturation,[50] which may serve to prevent the occurrence of withdrawal symptoms.
2.3 Nicotine Withdrawal and Relapse to Smoking
Considering the pathophysiological basis of nicotine addiction outlined in section 2.2, the rewarding effects of peaking nicotine levels in the brain would appear to be the main drivers of nicotine addiction. However, animal research suggests that the reinforcing potential of nicotine is only moderate compared with other drugs of abuse.[51] As a consequence, pending nicotine withdrawal has been suggested to underlie continued smoking behaviour. Withdrawal can be defined as a syndrome of behavioural, affective, cognitive and physiological symptoms,[52] including depressed mood, anxiety, irritability and craving.[53] Animal research shows that spontaneous nicotine withdrawal results in a significant decrease in brain reward function.[51] Conversely, dependent smokers may use nicotine inhalations as a self-medication to relieve negative affect and other withdrawal symptoms.[54] However, there is no uniform clinical picture of withdrawal:[55] in one study,[56] three patient clusters with distinct characteristics of the syndrome were identified, highlighting the difficulties associated with developing treatments to relieve withdrawal.
Symptoms of nicotine withdrawal may act as triggers causing a smoking lapse during a quit attempt. However, other trigger factors have also been reported. Since smoking is a conditioned behaviour,[57] cues associated with smoking can urge patients to abandon their plans of quitting.[4] Likewise, consumption of coffee and alcohol,[58] specific social situations, negative feelings and times of being alone are all associated with an increased risk of experiencing a smoking lapse.[59] Particularly early lapses (occurring within the first 2 weeks of a quit attempt) are associated with low long-term success rates.[60] Progression from lapse to full-blown relapse only occurs if smoking is perceived as rewarding. Thus, further developments in pharmacotherapy for smoking cessation should focus on reducing the rewarding effects of smoking.
3. Vaccine Development: Rationale and Practical Aspects
3.1 Working Mechanism of a Nicotine Vaccine
Based on the assumptions that a rapid increase in brain nicotine levels induces feelings of reward and that quit attempts frequently fail due to early lapses, preventing nicotine from entering the brain constitutes an intriguing concept. The idea of using antibodies to bind a drug and thus disabling it from crossing the blood-brain barrier was first tested in an animal model of heroin addiction[61,62] and subsequently extended to other species and other drugs of abuse, including morphine, methamphetamine, phencyclidine,[63] cocaine[64] and nicotine.[65] To date, only nicotine and cocaine have been used as vaccination targets in human studies.[63] The term ‘vaccination’ (synonym: active immunization) refers to the administration of an immunogenic substrate that causes T and B cell activation, leading to the formation of specific antibodies within the studied individual. By virtue of imprinting this response to the immunological memory, this approach yields longer-lasting protection. However, therapeutic antibody levels are only established several weeks after the first vaccine injection. Passive immunization is defined as the administration of preformed monoclonal or polyclonal high-affinity antibodies. This strategy offers immediate protection. However, in addition to being more expensive owing to high manufacturing costs, its effects are more short lived due to rapid degradation of antibodies.[66] Moreover, the amount of injectable antibodies is limited.[67] Studies in animals have used both approaches, while clinical trials have focused on active immunization procedures.
3.2 Characteristics of an Immune Response
The minimum molecular weight for a molecule to elicit a specific immune response is 10 kDa.[67] Due to its small molecular weight, nicotine itself is not immunogenic; in order to trigger an immune response, nicotine or a structurally similar hapten needs to be linked to a carrier protein,[68,69] thus producing a conjugate vaccine. The success of an immunological strategy relies on several characteristics, including but not limited to (i) immunogenicity of the vaccine; (ii) affinity of antibodies; and (iii) specificity of antibodies.
3.2.1 Immunogenicity
Immunogenicity is assessed by the antibody titre elicited by a vaccine. Titres (as measured by ELISA) of >1 : 10.000 indicate satisfactory immunogenicity.[70] Unfortunately, published reports of vaccination studies have used different measures of immunogenicity (ELISA titres,[17] geometric mean titres,[18] absolute antibody concentrations,[71] molar antibody concentrations,[19] ratio of specific and total IgG concentrations[72]), thus complicating the comparison of results between studies. In general, immunogenicity is influenced by the choice of the carrier protein and adjuvants added to the vaccine.
3.2.2 Affinity
The primary measure of antibody affinity to the target drug is the equilibrium dissociation constant Kd, i.e. the ratio of unbound to bound molecules at given concentrations.[63] High Kd values indicate low affinity as large amounts of unbound molecules are needed to induce formation of complexes between nicotine and its antibodies. High affinity is desired in order to ascertain fast clearance of unbound nicotine from the plasma; however, extremely high affinity may be disadvantageous as saturation of all antibodies can be achieved after one single nicotine dose, thus compromising efficacy for subsequent nicotine doses.[73] Total binding capacity of the serum is influenced by both immunogenicity and affinity.[63,74] Thus, lower affinity can be compensated for by increasing antibody dose.[73]
3.2.3 Specificity
This term refers to the extent to which the elicited antibodies bind to nicotine with high specificity in preference to other molecules, indicating low cross-reactivity between the antibody and nicotine metabolites such as cotinine, nicotine-N-oxide and nornicotine.[74] High specificity is particularly important if these metabolites occur in higher concentrations than the drug itself, as is the case for cotinine. Cross-reactivity can be reduced by exposing nicotine’s pyrrolidine ring to the immune system as this ring is first metabolized and thus not contained in most nicotine derivatives.[74] At the same time, cross reactivity might be desired if drug metabolites are themselves pharmacologically active, as is the case for cotinine[75–77] and nornicotine.[78] This has practical implications for the design of conjugate vaccines. For example, one recent study showed that using longer rather than shorter linkers and attaching them to the 6- rather than the 5-position of the pyridine ring (i.e. further away from the prime site of nicotine metabolism[79]) increases antibody selectivity for nicotine.[74]
4. Preclinical Studies
4.1 Objectives of Animal Studies
Antibodies binding a drug will primarily change its pharmacokinetic profile[63] which, in the case of nicotine, should abolish the functionally critical brain concentration peak, making nicotine intake less rewarding.[66] Accordingly, the primary objectives of preclinical studies were to study the effects of nicotine antibodies on (i) pharmacokinetics (serum and brain nicotine concentrations following acute and chronic administration of the drug; nicotine half-life in serum); (ii) brain function and behaviour (dopamine release in the NAcc, nicotine self-administration); and (iii) signs of withdrawal.
4.2 Methodology
A comprehensive description of the experimental procedures used to model addiction in animals is beyond the scope of this review (see LeSage et al.[66] for details). Both passive and active immunization approaches have been used to study the effects of nicotine antibodies in animals, and the vast majority of research was done on rats. Passive immunization was usually performed by intravenous[80] or (rarely) intraperitoneal[81] application of antibodies. Most studies used the nicotine-specific monoclonal antibody Nic311 with a Kd value of 60 nM.[73] Vaccination involved the singular or repeated intraperitoneal administration of an immunogen;[70,71,82] however, subcutaneous and intranasal vaccine delivery has also been reported.[83] The majority of vaccination studies were done with one of the following:
6-(carboxymethylureido)-(6)-nicotine (CMUNic) linked to keyhole limpet hemocyanin (KLH)[84]
3-aminomethyl-nicotine (3′-AmNic) linked to Pseudomonas aeruginosa exoprotein A (rEPA)[65]
the nicotine derivate IP18 linked to KLH[85]
nicotine coupled to virus-like particles formed by the coat protein of the bacteriophage Qb.[19]
In order to produce a satisfactory immune response, these vaccines need to be combined with an adjuvant. The synthesis of a further immunogenic compound has been reported in the literature. This peptide-based vaccine containing a residue of an agonist of human complement factor C5a does not require the simultaneous administration of an adjuvant. To date, only one experimental study using this vaccine has been published.[86]
4.3 Principal Findings
This section describes principal findings from animal studies of passive immunization and vaccination against nicotine (table I). Following a brief discussion of antibody properties reported in the literature, the three primary objectives mentioned in section 4.1 will be addressed.
Table I.
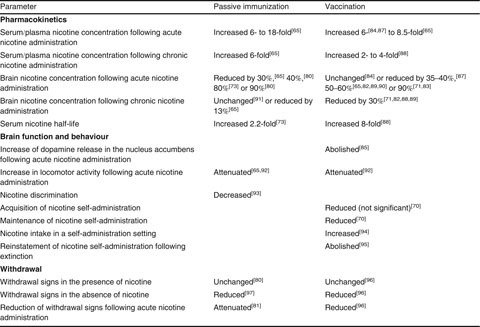
Effects of passive immunization and vaccination against nicotine on pharmacokinetics, brain function and behaviour and withdrawal in animal studies
4.3.1 Antibody Characteristics Following Vaccination
Following repeated vaccination with CMUNic-KLH[84,88] or 3′-AmNic-rEPA,[65,82] antibody titres as determined by ELISA were greater than 1 : 10 000, and antibody concentration ranged from 100 μg/mL[84] to 300 μg/mL.[71] Four injections of 3′-Am-Nic-rEPA elicited titres between 1 : 200 000 and 1 : 250 000,[70] comparable to those produced by two injections of IP18-KLH.[96] In one experiment, antibody concentrations following simultaneous bivalent vaccination with 3′-AmNic-rEPA and 6-CMUNic-KLH were greater than those elicited by monovalent vaccination.[98] Notably, antibody formation did not appear to be impeded by the presence of nicotine during the vaccination procedure.[82]
The dissociation constant Kd of antibodies was within the range of 10–30 nM,[98] and nicotine binding capacity was approximately 2 × 10-6 M (equivalent to 210 ± 110 ng/mL). Nicotine-specific IgG represented approximately 1–2% of total IgG.[65,84,88]
Antibodies yielded high specificity for nicotine,[65,85,87] with only minor cross-reactivity to major metabolites of the drug.[19,74,83]
4.3.2 Pharmacokinetics
Binding of nicotine to antibodies is expected to result in greater retention of the drug in the serum. Accordingly, serum nicotine concentrations following acute administration were increased at least 6-fold in both passively immunized and vaccinated rats as compared with controls.[65] The increase was slightly smaller in vaccinated rats receiving five nicotine injections over a period of 80 minutes, simulating repeated exposure as present in smokers.[88] Despite increased total nicotine levels, the fraction of unbound (and thus active) drug was reduced by up to 92%[89] as evidenced by attenuated cardiovascular effects in passively immunized animals[65] and the absence of seizures in vaccinated rats that would normally be observed following high-dose nicotine infusion.[99] Since nicotine binding partially protects the drug from being metabolized, plasma half-life of nicotine was increased 2.2- to 8-fold by passive immunization[73] and vaccination,[88] respectively.
As outlined in previous sections, the primary aim of binding nicotine in the serum is to prevent the drug from entering the brain. In most preclinical experiments, brain nicotine concentration was measured shortly (i.e. 3 minutes) after a nicotine bolus injection. Results varied significantly between studies: following acute administration, passive immunization decreased brain levels of nicotine by 30%[65] to 90%[80] compared with controls; similarly, variable reductions were observed in vaccinated rats[65,71,82,83,87,89,90] receiving a single nicotine bolus. In vaccinated rats, reductions in brain nicotine concentration were greatest shortly after acute administration of nicotine.[89] Interestingly, regardless of the mode of immunization, reductions in brain nicotine levels were considerably smaller following the chronic administration of nicotine.[65,71,82,88,89,91]
Effects of immunization on nicotine pharmacokinetics were dose dependent in that higher antibody concentrations elicited more profound nicotine retention in serum and a larger decrease in brain nicotine concentration.[65,73,80]
4.3.3 Brain Function and Behaviour
An acute increase of dopamine output in the NAcc following nicotine administration is believed to mediate the addictive properties of smoking. In vaccinated rats, this increase was abolished.[85] Likewise, the increase in locomotor activity following acute nicotine exposure was attenuated in both vaccinated[92] and passively immunized[65] animals, and the combination of both approaches further increased this effect.[100,101] Moreover, in the presence of antibodies, rats were less able to discriminate nicotine from saline injections.[93] The effect of vaccination on the development and maintenance of nicotine addiction was studied in experiments using rats that were trained to self-administer nicotine[102] at clinically relevant doses (0.01–0.06 mg/kg per dose, eliciting a [nicotine]plasma of 10–60 ng/mL[103]). While the acquisition of nicotine self-administration was not significantly impeded by the vaccine, maintenance of this learned behaviour was attenuated. One study found no evidence of compensatory overdosing aimed at surmounting the effects of vaccination,[70] while the results of another more recent study reported increased nicotine intake following vaccination. This might have been due to lower antibody concentrations and higher doses of nicotine infusions in the latter study, resulting in saturation of antibody binding sites and, consequently, insufficient sequestering of the drug.[94]
Even more importantly, vaccination abolished the reinstatement of nicotine self-administration following extinction of the conditioned response and re-exposure to nicotine, simulating a smoking lapse.[95] This effect was dependent on high antibody levels and was more pronounced with smaller priming doses of nicotine, resembling intake from one-tenth of a cigarette.[95]
4.3.4 Withdrawal
Due to a lack of effect on brain nAChRs, immunization against nicotine is unlikely to modulate withdrawal symptoms. On the contrary, it may be hypothesized that immunization during smoking might induce withdrawal as newly formed antibodies abolish brain nicotine peaks, which are essential for feelings of reward to occur. Assessment of nicotine withdrawal symptoms in an animal model of addiction is difficult. However, the available data suggest that neither passive immunization[80] nor vaccination[96] precipitate withdrawal in the presence of nicotine. Moreover, withdrawal following the termination of nicotine administration was reduced in immunized rats as compared with controls,[96] although there was evidence of persisting nicotine dependence.[97] Finally, one study investigated the effects of passive immunization on the reduction of withdrawal signs following re-exposure to nicotine.[81] In the presence of antibodies against nicotine, withdrawal relief achieved by nicotine administration was attenuated. Similar findings were reported following vaccination.[96]
4.4 Summary of Findings from Animal Studies
Vaccination of rats produced antibodies with high affinity and specificity for nicotine. One encouraging finding regarding the possibility of vaccinating active smokers was that immunogenicity of the vaccine was not impaired by the presence of nicotine. Animal studies have confirmed the hypothesis that nicotine pharmacokinetics are markedly changed in the presence of antibodies against nicotine. Effects on serum and brain concentrations of the drug were dependent on antibody concentration, greatest shortly after the application of a single nicotine dose and more pronounced when smaller priming doses were used. While vaccination may prevent acute nicotine delivery to the brain, chronic accumulation of the drug in the brain was only moderately affected by the presence of antibodies, i.e. nicotine entry into the brain was delayed rather than fully prevented. Accordingly, acute nicotine effects in dopamine release in the NAcc and related behaviours were attenuated in vaccinated animals. However, vaccination did not interfere with the development of nicotine addiction in a self-administration paradigm, and, even with favourable antibody titres, maintenance of nicotine self-administration was not affected by vaccination in some animals.[70] The attenuation of withdrawal severity observed in vaccinated animals might be explained by prolonged nicotine half-life in the presence of antibodies. The finding of reduced alleviation of withdrawal symptoms by a priming dose of nicotine in vaccinated rats suggests that nicotine vaccination might be most effective in preventing relapse in smokers trying to quit.[66,67,104]
5. Clinical Studies
At least four vaccines against nicotine are currently under clinical development,[74] but peer-reviewed reports have only been published for two of them:
NicVAX[18,20,21] contains 3′-AmNic linked to rEPA. This vaccine was developed by Nabi Pharmaceuticals and is currently being further evaluated for clinical use by GlaxoSmithKline.
NIC002 (synonym: NicotineQb[17,19]) contains a nicotine derivative coupled to a virus-like particle formed by the coat protein of the bacteriophage Qb in Escherichia coli. This vaccine was developed by Cytos Biotechnology; further clinical evaluation is being carried out by Novartis.
All published clinical trials used alum as an adjuvant to boost immune responses. Additional vaccines currently being tested are TA-NIC (containing recombinant cholera toxin B; developed by Celtic Pharma/Xenova[105]) and Niccine (developed by Pharmaceutica AB[74]), and at least two further companies are currently evaluating nicotine vaccines at the preclinical stage with no published reports available at the time of data collection for this review. A summary of preliminary results published on company websites can be found elsewhere.[106]
Results of the five published reports of phase I/II studies are summarized in table II. In the following section, principal results regarding safety, immunogenicity and efficacy are reviewed.
Table II.
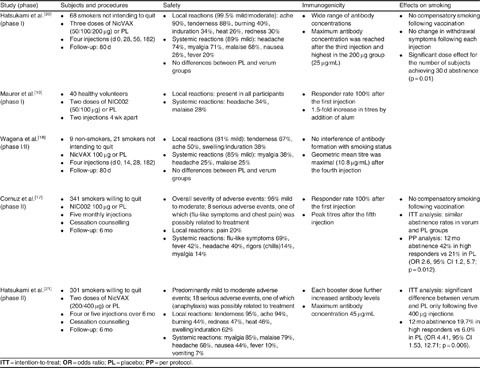
Results of phase I/II clinical trials of vaccines against nicotine
5.1 Study Design
Three studies (two using NicVAX[18,20] and one using NIC002[19]) were primarily designed to assess safety and immunogenicity and therefore included smaller groups of non-smokers or smokers not intending to quit; cessation counselling was not offered in these studies. Two more recent trials also assessing efficacy included smokers willing to quit.[17,21] In these studies, subjects were required to set a quit date following their second vaccination, and cessation counselling was provided. The comparability of results is impaired by the fact that counselling was only provided in two out of five trials. Studies differed regarding vaccine doses used and vaccination schemes (for details see table II).
5.2 Safety
Mild to moderate local reactions at injection sites (ache and tenderness) were common in all studies. Systemic reactions, which were also mild in most cases, included myalgia, malaise and headaches. The prevalence of these symptoms was similar in participants receiving a vaccine and those receiving adjuvant without the active vaccine, indicating that adverse events were not related to the vaccine itself.[20,21] Serious adverse events potentially related to treatment were rarely observed: one subject with a history of allergy to penicillin was reported to have suffered from an anaphylactic reaction 70 minutes after receiving the first 400 μg dose of NicVAX.[21]
5.3 Immunogenicity
The immune response to nicotine vaccination was highly variable in all five trials. As a common feature, higher vaccine doses elicited stronger responses, and antibody titres tended to peak following the final injection although this was not observed in all studies.[20] Comparison of immunogenicity across trials is complicated as some studies reported geometric mean titres, while others assessed ELISA titres. The maximum antibody concentration in the most recent proof-of-concept study was 45 μg/mL.[21] By including both smokers and non-smokers, one study demonstrated that immunogenicity was not impeded by the presence of nicotine.[18] Antibody affinity to nicotine was only assessed in one trial using NIC002; the Kd value was 33 nM. Data on antibody specificity following vaccination in humans have not been published.
5.4 Efficacy
Three trials reported data on smoking status.[17,20,21] Following vaccination, there was no evidence of compensatory smoking in order to overcome the effects of antibodies blocking nicotine entry into the brain. At the same time, vaccination did not appear to induce withdrawal symptoms in smokers.
The first study formally assessing continuous abstinence rates was published in 2008.[17] According to the intent-to-treat analysis, there was no significant difference between 3-month continuous abstinence rates until month 6 between the intervention and control groups (30.1% vs 26.1%). However, a per-protocol analysis excluding all subjects with concomitant use of nicotine replacement therapy revealed significantly higher abstinence rates in the upper third of responders (i.e. subjects with particularly high antibody titres) as compared with the placebo group (56.6% vs 31.3%; odds ratio [OR] 2.9, 95% CI 1.4, 5.9; p = 0.004). This difference was maintained until 12 months (41.5% vs 21.3%; OR 2.6, 95% CI 1.2, 5.7; p = 0.012).
Based on these results, a subsequent trial was intended to further establish a relationship between antibody titres and smoking outcome.[21] Continuous abstinence rates at 12 months were significantly higher in the top 30% responders than in subjects receiving placebo (19.7% vs 6.0%; OR 4.41, 95% CI 1.53, 12.71; p = 0.006). In addition, continuous abstinence was enhanced in subjects receiving the most intensive vaccination regimen. Finally, among smokers who failed to quit, smoking reduction occurred more frequently in subjects with high antibody titres (‘responders’) compared with placebo.
Recently NABI Biopharmaceuticals announced the results of the first phase III, double-blinded, placebo-controlled trial including 1000 subjects who received a total of six vaccinations with NicVAX 400 μg or placebo. A preliminary assessment of the trial data showed that continuous abstinence for 16 weeks, from week 37 to 52, was similar in both treatment arms and approximately 11%.[107] However, a peer-reviewed report of these results has not been published yet.
5.5 Summary of Findings from Phase I/II Trials
Taken together, published results of phase I/II studies indicate that nicotine vaccination is well tolerated and capable of inducing an immune response against nicotine even with concomitant smoking. However, in contrast to expectations from animal studies, vaccination failed to increase continuous abstinence rates over placebo.
6. Strengths and Limitations; Suggestions for Future Research
The basic idea of preventing nicotine from entering the brain, thereby blocking its rewarding effects in the mesolimbic system is attractive as antibodies are unlikely to elicit adverse effects within the brain[67] that have been described for other smoking-cessation medications.[108,109] In fact, no major adverse events following vaccination were reported in phase I/II clinical trials. A further advantage of this novel approach is that treatment adherence is likely to be favourable[110] as vaccination requires only a limited number of injections and no daily dosing. Clinical trials have partially confirmed preclinical observations (e.g. lack of compensatory smoking), but they failed to establish a clear effect of vaccination on smoking behaviour.
Knowledge of the reasons for this failure of the vaccination concept to successfully translate to the clinical setting is crucial for the future development of nicotine vaccines. One obvious limitation of phase I/II trials was that they were not designed to assess efficacy endpoints. Moreover, the proportion of subjects receiving all scheduled vaccinations was as low as 60% in one trial.[21] Choosing a target quit date shortly after the first booster injection might also have impaired efficacy, as peak antibody titres were only observed following several vaccinations. In addition, as nicotine-binding capacity is not only determined by antibody concentration, a more thorough investigation of antibody affinity and specificity in these trials would have been desirable. However, some issues going beyond these practical aspects need to be addressed in order to understand the obvious discrepancy between preclinical and clinical findings.
6.1 Tobacco Addiction
Recent research into the pathophysiology of drug dependence indicates that viewing nicotine peaks and subsequent dopamine release in the NAcc as an indispensable element of tobacco addiction may be too simplistic. Thus, dopaminergic VTA neurons have been found to increase their activity not only in response to nicotine but also in the presence of aversive stimuli,[111] and animal studies suggest that hedonic responses can be elicited in the absence of dopamine.[112] The finding of increased smoking-cessation rates following damage to the insula[113] further substantiates the notion that the mesolimbic reward circuit is but one brain structure relevant to nicotine addiction. Finally, the whole concept of nicotine concentration peaks underlying the rewarding effects of smoking has been questioned by a positron emission tomography (PET) study suggesting a gradual increase in brain nicotine levels during smoking with no evidence of concentration peaks following each puff.[114]
Until recently,[115] the non-nicotinic components of tobacco addiction[116] have received relatively little scientific attention. It is now recognized that tobacco addiction results from an interplay of pharmacological, psychological, genetic and environmental factors.[4] The contribution of nicotine to this complex interaction may be smaller than previously thought[117] as rewards elicited by smoking can also be induced by smoking denicotinized cigarettes.[118] In fact, substances in smoke other than nicotine have been found to enhance the reinforcing properties of nicotine.[119] Among these, acetaldehyde[120] and agents blocking monoamine oxidase activity[121] may play a major role. Results of animal experiments indicate that nicotine and other agents might support early conditioning of the reward response triggered by smoking-related cues. At a later stage, these conditioned stimuli might be sufficient to generate feelings of reward.[122]
6.2 Limitations of Animal Models
At first glance, preclinical studies provide convincing evidence that a nicotine vaccine is likely to reduce nicotine self-administration[70] and possibly even attenuate withdrawal symptoms,[96] thus facilitating smoking cessation and preventing relapse. However, although great efforts were made to adjust nicotine concentrations in animals to those observed in smokers,[123] the extent to which these findings can be applied to tobacco addiction in humans remains unclear.
First, much of this evidence relates to serum and brain nicotine concentrations measured shortly after the intravenous application of nicotine (table I). Most animal models did not use nicotine inhalation as the primary route of drug administration. In addition, these experiments have not assessed temporal patterns of nicotine distribution to different organs including the brain[114] and the lungs.[71,89,114] The clinical significance of reducing nicotine distribution to the brain by 40–60% at one fixed time-point is unclear[82] as it is the persistence of nicotine in the brain that appears to modulate structure and function of nAChRs.[4]
Second, the immune response elicited by vaccination against nicotine may differ from species to species. Accordingly, antibody levels reported in rats ranged from 100 μg/mL[84] to 300 μg/mL,[71] while much lower concentrations (up to 45 μg/mL[21]) were observed in clinical trials. Yet, this difference might be attributable to the heterogeneous methodology in determining antibody levels.
Third, as the rewarding properties of nicotine are limited,[51] preclinical research paradigms focusing on reinforcement[102] may not be sufficient to model the complex pharmacological and behavioural aspects of smoking and cessation. In fact, animal studies have rarely used the cues and psychosocial processes associated with relapse.[124] Even when cues were used,[95] the validity of experimental extinction of these conditioned stimuli to mirror quit attempts in humans is highly debatable.
6.3 Clinical Trial Design
As an introduction of nicotine vaccines to international markets will depend on the results of future trials, these studies need to be carefully designed. Despite the conclusion drawn from preclinical studies that a nicotine vaccine might be primarily useful in preventing relapse, published clinical trials were designed as smoking-cessation studies including target quit dates. They mainly assessed continuous abstinence rather than withdrawal severity, the incidence of lapses and their progression to full relapse.[125] Variables that are known to impact on continuous abstinence, including the speed of nicotine metabolism,[126–130] have not been investigated in vaccination studies. In addition, antibody characteristics, including affinity and specificity, clearly have a huge impact on functionality[74] and thus require thorough evaluation in clinical trials. Careful selection of primary study endpoints and secondary measurements is therefore warranted for these trials, and study populations must be aligned to these endpoints.
Smokers who have already quit may represent an ideal target group for a relapse prevention study. However, the formation of sufficient amounts of antibodies takes at least 6 weeks, while most relapse occurs within the first 2 weeks of a quit attempt.[131] As a consequence, subjects would have to be enrolled well before quitting, which may be difficult as 50% of quit attempts occur spontaneously.[132] Accordingly, offering nicotine vaccination to smokers willing to reduce their cigarette consumption with the ultimate goal of quitting could be a viable option. Once these smokers feel prepared to quit, adequate antibody levels might be readily available.
Finally, monotherapy with a nicotine vaccine does not appear to be a promising tool to overcome the complex physiological and psychosocial alterations observed in smokers. Thus, a nicotine vaccine with sufficient efficacy could one day become part of a multifaceted intervention[104] that includes behavioural as well as pharmacological approaches. Regarding the latter, varenicline might be used in combination with the vaccine as it produces high abstinence rates at the end of treatment,[133] after which relapse needs to be prevented. A 1-year study combining varenicline with placebo-controlled NicVAX focussing on relapse prevention in almost 600 smokers is underway and may help to unravel a possible synergism between these drugs. The utility of nicotine replacement therapy, bupropion and novel agents such as cytisine[134,135] in this setting also needs to be established. Finally, smokers who decide to quit spontaneously and seek immediate help might be offered passive immunization followed by pharmacotherapy to reduce craving and withdrawal symptoms while vaccination is started concomitantly in order to establish adequate antibody titres to prevent relapse at a later stage.
7. Conclusions
Vaccination against nicotine is an intriguing novel therapeutic approach to treating nicotine addiction.[136] By preventing nicotine from entering into the brain, antibodies might abolish the rewarding properties of smoking. Animal studies indicate that antibodies profoundly change the pharmacokinetics of the drug and can interfere with nicotine self-administration. However, in recent phase I/II trials and one unpublished phase III trial, these findings were not fully replicated. In addition to assessing alternative routes of vaccine administration[137,138] and addressing ethical issues generally associated with vaccinations against drugs of abuse,[139,140] future studies will need to more clearly define the ideal indications and target populations for nicotine vaccines. Treatment of dependent smokers cannot be reduced to a course of vaccine injections but needs to acknowledge the complex pharmacological and behavioural aspects of smoking.
Acknowledgements
The authors declare that they did not receive any funding for the preparation of this review.
T. Raupach has received grants to conduct investigator-initiated studies from Pfizer and Johnson & Johnson. He has been reimbursed for attendance and lecturing at several Pfizer symposia on smoking cessation from 2006 through 2011. He has also received travel expenses and honoraria from GlaxoSmithKline and Novartis. None of these activities were related to this manuscript. C.P.v. Schayck received funding for research proposals from GlaxoSmithKline and Pfizer, as well as reimbursement for lecturing from Pfizer. PHJ Hoogsteder has no conflicts of interest to declare.
References
- 1.WHO. WHO report on the global tobacco epidemic, 2011: warning about the dangers of tobacco. Geneva: WHO, 2011 [online]. Available from URL: http://whqlibdoc.who.int/publications/2011/9789240687813_eng.pdf [Accessed 2012 Feb 14]
- 2.Doll R, Peto R, Boreham J, et al. Mortality in relation to smoking: 50 years’ observations on male British doctors. BMJ. 2004;328(7455):1519. doi: 10.1136/bmj.38142.554479.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Benowitz NL. Nicotine addiction. N Engl J Med. 2010;362(24):2295–303. doi: 10.1056/NEJMra0809890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Steinberg MB, Schmelzer AC, Richardson DL, et al. The case for treating tobacco dependence as a chronic disease. Ann Intern Med. 2008;148(7):554–6. doi: 10.7326/0003-4819-148-7-200804010-00012. [DOI] [PubMed] [Google Scholar]
- 6.Lancaster T, Stead LF. Individual behavioural counselling for smoking cessation. Cochrane Database Syst Rev 2005 Apr 18; (2): CD001292 [DOI] [PubMed]
- 7.Raupach T, van Schayck CP. Pharmacotherapy for smoking cessation: current advances and research topics. CNS Drugs. 2011;25(5):371–82. doi: 10.2165/11590620-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 8.Fiore MC, Jaén CR, Baker TB. Clinical practice guideline. Rockville (MD): US Department of Health and Human Services; Public Health Service; 2008. Treating tobacco use and dependence: 2008 update. [Google Scholar]
- 9.Ebbert JO, Hays JT, Hurt RD. Combination pharmacotherapy for stopping smoking: what advantages does it offer? Drugs. 2010;70(6):643–50. doi: 10.2165/11536100-000000000-00000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kortmann GL, Dobler CJ, Bizarro L, et al. Pharmacogenetics of smoking cessation therapy. Am J Med Genet B Neuropsychiatr Genet. 2010;153B(1):17–28. doi: 10.1002/ajmg.b.30978. [DOI] [PubMed] [Google Scholar]
- 11.Rennard S, Hughes J, Cincirpini PM, et al. A randomized placebo-controlled trial of varenicline for smoking cessation allowing flexible quit dates. Nicotine Tob Res. Epub 2011 Nov 11 [DOI] [PMC free article] [PubMed]
- 12.Lindson N, Aveyard P. An updated meta-analysis of nicotine preloading for smoking cessation: investigating mediators of the effect. Psychopharmacology (Berl) 2011;214(3):579–92. doi: 10.1007/s00213-010-2069-3. [DOI] [PubMed] [Google Scholar]
- 13.Balmford J, Borland R, Hammond D, et al. Adherence to and reasons for premature discontinuation from stopsmoking medications: data from the ITC Four-Country Survey. Nicotine Tob Res. 2011;13(2):94–102. doi: 10.1093/ntr/ntq215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shiffman S. Light and intermittent smokers: background and perspective. Nicotine Tob Res. 2009;11(2):122–5. doi: 10.1093/ntr/ntn020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Buchhalter AR, Fant RV, Henningfield JE. Novel pharmacological approaches for treating tobacco dependence and withdrawal: current status. Drugs. 2008;68(8):1067–88. doi: 10.2165/00003495-200868080-00005. [DOI] [PubMed] [Google Scholar]
- 16.Vocci FJ, Chiang CN. Vaccines against nicotine: how effective are they likely to be in preventing smoking? CNS Drugs. 2001;15(7):505–14. doi: 10.2165/00023210-200115070-00001. [DOI] [PubMed] [Google Scholar]
- 17.Cornuz J, Zwahlen S, Jungi WF, et al. A vaccine against nicotine for smoking cessation: a randomized controlled trial. PLoS One. 2008;3(6):e2547. doi: 10.1371/journal.pone.0002547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wagena EJ, de Vos A, Horwith G, et al. The immunogenicity and safety of a nicotine vaccine in smokers and nonsmokers: results of a randomized, placebo-controlled phase 1/2 trial. Nicotine Tob Res. 2008;10(1):213–8. doi: 10.1080/14622200701704921. [DOI] [PubMed] [Google Scholar]
- 19.Maurer P, Jennings GT, Willers J, et al. A therapeutic vaccine for nicotine dependence: preclinical efficacy, and phase I safety and immunogenicity. Eur J Immunol. 2005;35(7):2031–40. doi: 10.1002/eji.200526285. [DOI] [PubMed] [Google Scholar]
- 20.Hatsukami DK, Rennard S, Jorenby D, et al. Safety and immunogenicity of a nicotine conjugate vaccine in current smokers. Clin Pharmacol Ther. 2005;78(5):456–67. doi: 10.1016/j.clpt.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 21.Hatsukami DK, Jorenby DE, Gonzales D, et al. Immunogenicity and smoking-cessation outcomes for a novel nicotine immunotherapeutic. Clin Pharmacol Ther. 2011;89(3):392–9. doi: 10.1038/clpt.2010.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hukkanen J, Jacob P, 3rd, Benowitz NL. Metabolism and disposition kinetics of nicotine. Pharmacol Rev. 2005;57(1):79–115. doi: 10.1124/pr.57.1.3. [DOI] [PubMed] [Google Scholar]
- 23.Kozlowski LT, Mehta NY, Sweeney CT, et al. Filter ventilation and nicotine content of tobacco in cigarettes from Canada, the United Kingdom, and the United States. Tob Control. 1998;7(4):369–75. doi: 10.1136/tc.7.4.369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Benowitz NL, Jacob P., 3rd Daily intake of nicotine during cigarette smoking. Clin Pharmacol Ther. 1984;35(4):499–504. doi: 10.1038/clpt.1984.67. [DOI] [PubMed] [Google Scholar]
- 25.Henningfield JE, Stapleton JM, Benowitz NL, et al. Higher levels of nicotine in arterial than in venous blood after cigarette smoking. Drug Alcohol Depend. 1993;33(1):23–9. doi: 10.1016/0376-8716(93)90030-T. [DOI] [PubMed] [Google Scholar]
- 26.Benowitz NL, Jacob P, 3rd, Jones RT, et al. Interindividual variability in the metabolism and cardiovascular effects of nicotine in man. J Pharmacol Exp Ther. 1982;221(2):368–72. [PubMed] [Google Scholar]
- 27.Benowitz NL, Jacob P., 3rd Nicotine and cotinine elimination pharmacokinetics in smokers and nonsmokers. Clin Pharmacol Ther. 1993;53(3):316–23. doi: 10.1038/clpt.1993.27. [DOI] [PubMed] [Google Scholar]
- 28.Berkman CE, Park SB, Wrighton SA, et al. In vitro-in vivo correlations of human (S)-nicotine metabolism. Biochem Pharmacol. 1995;50(4):565–70. doi: 10.1016/0006-2952(95)00168-Y. [DOI] [PubMed] [Google Scholar]
- 29.Benowitz NL, Swan GE, Jacob P, 3rd, et al. CYP2A6 genotype and the metabolism and disposition kinetics of nicotine. Clin Pharmacol Ther. 2006;80(5):457–67. doi: 10.1016/j.clpt.2006.08.011. [DOI] [PubMed] [Google Scholar]
- 30.Benowitz NL, Lessov-Schlaggar CN, Swan GE, et al. Female sex and oral contraceptive use accelerate nicotine metabolism. Clin Pharmacol Ther. 2006;79(5):480–8. doi: 10.1016/j.clpt.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 31.Lerman C, Tyndale R, Patterson F, et al. Nicotine metabolite ratio predicts efficacy of transdermal nicotine for smoking cessation. Clin Pharmacol Ther. 2006;79(6):600–8. doi: 10.1016/j.clpt.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 32.Patterson F, Schnoll RA, Wileyto EP, et al. Toward personalized therapy for smoking cessation: a randomized placebo-controlled trial of bupropion. Clin Pharmacol Ther. 2008;84(3):320–5. doi: 10.1038/clpt.2008.57. [DOI] [PubMed] [Google Scholar]
- 33.Balfour DJ. Neural mechanisms underlying nicotine dependence. Addiction. 1994;89(11):1419–23. doi: 10.1111/j.1360-0443.1994.tb03738.x. [DOI] [PubMed] [Google Scholar]
- 34.Picciotto MR, Caldarone BJ, King SL, et al. Nicotinic receptors in the brain: links between molecular biology and behavior. Neuropsychopharmacology. 2000;22(5):451–65. doi: 10.1016/S0893-133X(99)00146-3. [DOI] [PubMed] [Google Scholar]
- 35.Rose JE, Behm FM, Westman EC, et al. PET studies of the influences of nicotine on neural systems in cigarette smokers. Am J Psychiatry. 2003;160(2):323–33. doi: 10.1176/appi.ajp.160.2.323. [DOI] [PubMed] [Google Scholar]
- 36.Kenny PJ, Markou A. Nicotine self-administration acutely activates brain reward systems and induces a long-lasting increase in reward sensitivity. Neuropsychopharmacology. 2006;31(6):1203–11. doi: 10.1038/sj.npp.1300905. [DOI] [PubMed] [Google Scholar]
- 37.Henningfield JE, Keenan RM. Nicotine delivery kinetics and abuse liability. J Consult Clin Psychol. 1993;61(5):743–50. doi: 10.1037/0022-006X.61.5.743. [DOI] [PubMed] [Google Scholar]
- 38.Samaha AN, Yau WY, Yang P, et al. Rapid delivery of nicotine promotes behavioral sensitization and alters its neurobiological impact. Biol Psychiatry. 2005;57(4):351–60. doi: 10.1016/j.biopsych.2004.11.040. [DOI] [PubMed] [Google Scholar]
- 39.Benowitz NL, Porchet H, Sheiner L, et al. Nicotine absorption and cardiovascular effects with smokeless tobacco use: comparison with cigarettes and nicotine gum. Clin Pharmacol Ther. 1988;44(1):23–8. doi: 10.1038/clpt.1988.107. [DOI] [PubMed] [Google Scholar]
- 40.Henningfield JE, Miyasato K, Jasinski DR. Abuse liability and pharmacodynamic characteristics of intravenous and inhaled nicotine. J Pharmacol Exp Ther. 1985;234(1):1–12. [PubMed] [Google Scholar]
- 41.Benowitz NL. Pharmacology of nicotine: addiction and therapeutics. Annu Rev Pharmacol Toxicol. 1996;36:597–613. doi: 10.1146/annurev.pa.36.040196.003121. [DOI] [PubMed] [Google Scholar]
- 42.Corrigall WA, Franklin KB, Coen KM, et al. The mesolimbic dopaminergic system is implicated in the reinforcing effects of nicotine. Psychopharmacology (Berl) 1992;107(2–3):285–9. doi: 10.1007/BF02245149. [DOI] [PubMed] [Google Scholar]
- 43.Pierce RC, Kumaresan V. The mesolimbic dopamine system: the final common pathway for the reinforcing effect of drugs of abuse? Neurosci Biobehav Rev. 2006;30(2):215–38. doi: 10.1016/j.neubiorev.2005.04.016. [DOI] [PubMed] [Google Scholar]
- 44.Dome P, Lazary J, Kalapos MP, et al. Smoking, nicotine and neuropsychiatric disorders. Neurosci Biobehav Rev. 2010;34(3):295–342. doi: 10.1016/j.neubiorev.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 45.Leonard S, Bertrand D. Neuronal nicotinic receptors: from structure to function. Nicotine Tob Res. 2001;3(3):203–23. doi: 10.1080/14622200110050213. [DOI] [PubMed] [Google Scholar]
- 46.Suaud-Chagny MF, Chergui K, Chouvet G, et al. Relationship between dopamine release in the rat nucleus accumbens and the discharge activity of dopaminergic neurons during local in vivo application of amino acids in the ventral tegmental area. Neuroscience. 1992;49(1):63–72. doi: 10.1016/0306-4522(92)90076-E. [DOI] [PubMed] [Google Scholar]
- 47.Nestler EJ. Is there a common molecular pathway for addiction? Nat Neurosci. 2005;8(11):1445–9. doi: 10.1038/nn1578. [DOI] [PubMed] [Google Scholar]
- 48.Di Chiara G, Imperato A. Drugs abused by humans preferentially increase synaptic dopamine concentrations in the mesolimbic system of freely moving rats. Proc Natl Acad Sci U S A. 1988;85(14):5274–8. doi: 10.1073/pnas.85.14.5274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Picciotto MR, Addy NA, Mineur YS, et al. It is not “either/or”: activation and desensitization of nicotinic acetylcholine receptors both contribute to behaviors related to nicotine addiction and mood. Prog Neurobiol. 2008;84(4):329–42. doi: 10.1016/j.pneurobio.2007.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Brody AL, Mandelkern MA, London ED, et al. Cigarette smoking saturates brain alpha 4 beta 2 nicotinic acetylcholine receptors. Arch Gen Psychiatry. 2006;63(8):907–15. doi: 10.1001/archpsyc.63.8.907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Epping-Jordan MP, Watkins SS, Koob GF, et al. Dramatic decreases in brain reward function during nicotine withrawal. Nature. 1998;393(6680):76–9. doi: 10.1038/30001. [DOI] [PubMed] [Google Scholar]
- 52.Shiffman S, West R, Gilbert D. Recommendation for the assessment of tobacco craving and withdrawal in smoking cessation trials. Nicotine Tob Res. 2004;6(4):599–614. doi: 10.1080/14622200410001734067. [DOI] [PubMed] [Google Scholar]
- 53.Hughes JR, Hatsukami D. Signs and symptoms of tobacco withdrawal. Arch Gen Psychiatry. 1986;43(3):289–94. doi: 10.1001/archpsyc.1986.01800030107013. [DOI] [PubMed] [Google Scholar]
- 54.Benowitz NL. Clinical pharmacology of nicotine: implications for understanding, preventing, and treating tobacco addiction. Clin Pharmacol Ther. 2008;83(4):531–41. doi: 10.1038/clpt.2008.3. [DOI] [PubMed] [Google Scholar]
- 55.Piasecki TM. Relapse to smoking. Clin Psychol Rev. 2006;26(2):196–215. doi: 10.1016/j.cpr.2005.11.007. [DOI] [PubMed] [Google Scholar]
- 56.Piasecki TM, Fiore MC, Baker TB. Profiles in discouragement: two studies of variability in the time course of smoking withdrawal symptoms. J Abnorm Psychol. 1998;107(2):238–51. doi: 10.1037/0021-843X.107.2.238. [DOI] [PubMed] [Google Scholar]
- 57.Davis JA, Gould TJ. Associative learning, the hippocampus, and nicotine addiction. Curr Drug Abuse Rev. 2008;1(1):9–19. doi: 10.2174/1874473710801010009. [DOI] [PubMed] [Google Scholar]
- 58.Krall EA, Garvey AJ, Garcia RI. Smoking relapse after 2 years of abstinence: findings from the VA Normative Aging Study. Nicotine Tob Res. 2002;4(1):95–100. doi: 10.1080/14622200110098428. [DOI] [PubMed] [Google Scholar]
- 59.Yang T, Fisher KJ, Li F, et al. Attitudes to smoking cessation and triggers to relapse among Chinese male smokers. BMC Public Health. 2006;6:65. doi: 10.1186/1471-2458-6-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kenford SL, Fiore MC, Jorenby DE, et al. Predicting smoking cessation: who will quit with and without the nicotine patch. JAMA. 1994;271(8):589–94. doi: 10.1001/jama.1994.03510320029025. [DOI] [PubMed] [Google Scholar]
- 61.Bonese KF, Wainer BH, Fitch FW, et al. Changes in heroin self-administration by a rhesus monkey after morphine immunisation. Nature. 1974;252(5485):708–10. doi: 10.1038/252708a0. [DOI] [PubMed] [Google Scholar]
- 62.Killian A, Bonese K, Rothberg RM, et al. Effects of passive immunization against morphine on heroin selfadministration. Pharmacol Biochem Behav. 1978;9(3):347–52. doi: 10.1016/0091-3057(78)90295-2. [DOI] [PubMed] [Google Scholar]
- 63.Orson FM, Kinsey BM, Singh RA, et al. Substance abuse vaccines. Ann N Y Acad Sci. 2008;1141:257–69. doi: 10.1196/annals.1441.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Fox BS, Kantak KM, Edwards MA, et al. Efficacy of a therapeutic cocaine vaccine in rodent models. Nat Med. 1996;2(10):1129–32. doi: 10.1038/nm1096-1129. [DOI] [PubMed] [Google Scholar]
- 65.Pentel PR, Malin DH, Ennifar S, et al. A nicotine conjugate vaccine reduces nicotine distribution to brain and attenuates its behavioral and cardiovascular effects in rats. Pharmacol Biochem Behav. 2000;65(1):191–8. doi: 10.1016/S0091-3057(99)00206-3. [DOI] [PubMed] [Google Scholar]
- 66.LeSage MG, Keyler DE, Pentel PR. Current status of immunologic approaches to treating tobacco dependence: vaccines and nicotine-specific antibodies. AAPS J. 2006;8(1):E65–75. doi: 10.1208/aapsj080108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Moreno AY, Janda KD. Immunopharmacotherapy: vaccination strategies as a treatment for drug abuse and dependence. Pharmacol Biochem Behav. 2009;92(2):199–205. doi: 10.1016/j.pbb.2009.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Matsushita H, Noguchi M, Tamaki E. Conjugate of bovine serum albumin with nicotine. Biochem Biophys Res Commun. 1974;57(4):1006–10. doi: 10.1016/0006-291X(74)90796-7. [DOI] [PubMed] [Google Scholar]
- 69.Castro A, Monji N, Ali H, et al. Nicotine antibodies: comparison of ligand specificities of antibodies produced against two nicotine conjugates. Eur J Biochem. 1980;104(2):331–40. doi: 10.1111/j.1432-1033.1980.tb04433.x. [DOI] [PubMed] [Google Scholar]
- 70.Le Sage MG, Keyler DE, Hieda Y, et al. Effects of a nicotine conjugate vaccine on the acquisition and maintenance of nicotine self-administration in rats. Psychopharmacology (Berl) 2006;184(3–4):409–16. doi: 10.1007/s00213-005-0027-2. [DOI] [PubMed] [Google Scholar]
- 71.Pravetoni M, Keyler DE, Raleigh MD, et al. Vaccination against nicotine alters the distribution of nicotine delivered via cigarette smoke inhalation to rats. Biochem Pharmacol. 2011;81(9):1164–70. doi: 10.1016/j.bcp.2011.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Pentel P, Malin D. A vaccine for nicotine dependence: targeting the drug rather than the brain. Respiration. 2002;69(3):193–7. doi: 10.1159/000063617. [DOI] [PubMed] [Google Scholar]
- 73.Keyler DE, Roiko SA, Benlhabib E, et al. Monoclonal nicotine-specific antibodies reduce nicotine distribution to brain in rats: dose- and affinity-response relationships. Drug Metab Dispos. 2005;33(7):1056–61. doi: 10.1124/dmd.105.004234. [DOI] [PubMed] [Google Scholar]
- 74.de Villiers SH, Lindblom N, Kalayanov G, et al. Nicotine hapten structure, antibody selectivity and effect relationships: results from a nicotine vaccine screening procedure. Vaccine. 2010;28(10):2161–8. doi: 10.1016/j.vaccine.2009.12.051. [DOI] [PubMed] [Google Scholar]
- 75.Oliver JL, Pashmi G, Barnett P, et al. Development of an anti-cotinine vaccine to potentiate nicotine-based smoking cessation strategies. Vaccine. 2007;25(42):7354–62. doi: 10.1016/j.vaccine.2007.08.019. [DOI] [PubMed] [Google Scholar]
- 76.Sziraki I, Sershen H, Benuck M, et al. The effect of cotinine on nicotine- and cocaine-induced dopamine release in the nucleus accumbens. Neurochem Res. 1999;24(11):1471–8. doi: 10.1007/s11064-999-0001-1. [DOI] [PubMed] [Google Scholar]
- 77.Buccafusco JJ, Shuster LC, Terry AV., Jr Disconnection between activation and desensitization of autonomic nicotinic receptors by nicotine and cotinine. Neurosci Lett. 2007;413(1):68–71. doi: 10.1016/j.neulet.2006.11.028. [DOI] [PubMed] [Google Scholar]
- 78.Bardo MT, Green TA, Crooks PA, et al. Nornicotine is self-administered intravenously by rats. Psychopharmacology (Berl) 1999;146(3):290–6. doi: 10.1007/s002130051119. [DOI] [PubMed] [Google Scholar]
- 79.Matsukura S, Sakamoto N, Imura H, et al. Radioimmunoassay of nicotine. Biochem Biophys Res Commun. 1975;64(2):574–80. doi: 10.1016/0006-291X(75)90360-5. [DOI] [PubMed] [Google Scholar]
- 80.Roiko SA, Harris AC, LeSage MG, et al. Passive immunization with a nicotine-specific monoclonal antibody decreases brain nicotine levels but does not precipitate withdrawal in nicotine-dependent rats. Pharmacol Biochem Behav. 2009;93(2):105–11. doi: 10.1016/j.pbb.2009.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Malin DH, Lake JR, Lin A, et al. Passive immunization against nicotine prevents nicotine alleviation of nicotine abstinence syndrome. Pharmacol Biochem Behav. 2001;68(1):87–92. doi: 10.1016/S0091-3057(00)00436-6. [DOI] [PubMed] [Google Scholar]
- 82.Hieda Y, Keyler DE, Ennifar S, et al. Vaccination against nicotine during continued nicotine administration in rats: immunogenicity of the vaccine and effects on nicotine distribution to brain. Int J Immunopharmacol. 2000;22(10):809–19. doi: 10.1016/S0192-0561(00)00042-4. [DOI] [PubMed] [Google Scholar]
- 83.Cerny EH, Levy R, Mauel J, et al. Preclinical development of a vaccine ‘against smoking’. Onkologie. 2002;25(5):406–11. doi: 10.1159/000067433. [DOI] [PubMed] [Google Scholar]
- 84.Hieda Y, Keyler DE, Vandevoort JT, et al. Active immunization alters the plasma nicotine concentration in rats. J Pharmacol Exp Ther. 1997;283(3):1076–81. [PubMed] [Google Scholar]
- 85.de Villiers SH, Lindblom N, Kalayanov G, et al. Active immunization against nicotine suppresses nicotineinduced dopamine release in the rat nucleus accumbens shell. Respiration. 2002;69(3):247–53. doi: 10.1159/000063628. [DOI] [PubMed] [Google Scholar]
- 86.Sanderson SD, Cheruku SR, Padmanilayam MP, et al. Immunization to nicotine with a peptide-based vaccine composed of a conformationally biased agonist of C5a as a molecular adjuvant. Int Immunopharmacol. 2003;3(1):137–46. doi: 10.1016/S1567-5769(02)00260-6. [DOI] [PubMed] [Google Scholar]
- 87.de Villiers SH, Lindblom N, Kalayanov G, et al. Active immunization against nicotine alters the distribution of nicoine but not the metabolism to cotinine in the rat. Naunyn Schmiedebergs Arch Pharmacol. 2004;370(4):299–304. doi: 10.1007/s00210-004-0960-3. [DOI] [PubMed] [Google Scholar]
- 88.Keyler DE, Hieda Y, St Peter J, et al. Altered disposition of repeated nicotine doses in rats immunized against nicotine. Nicotine Tob Res. 1999;1(3):241–9. doi: 10.1080/14622299050011361. [DOI] [PubMed] [Google Scholar]
- 89.Satoskar SD, Keyler DE, LeSage MG, et al. Tissuedependent effects of immunization with a nicotine conjugate vaccine on the distribution of nicotine in rats. Int Immunopharmacol. 2003;3(7):957–70. doi: 10.1016/S1567-5769(03)00094-8. [DOI] [PubMed] [Google Scholar]
- 90.Hieda Y, Keyler DE, VanDe Voort JT, et al. Immunization of rats reduces nicotine distribution to brain. Psychopharmacology (Berl) 1999;143(2):150–7. doi: 10.1007/s002130050930. [DOI] [PubMed] [Google Scholar]
- 91.Pentel PR, Dufek MB, Roiko SA, et al. Differential effects of passive immunization with nicotine-specific antibodies on the acute and chronic distribution of nicotine to brain in rats. J Pharmacol Exp Ther. 2006;317(2):660–6. doi: 10.1124/jpet.105.097873. [DOI] [PubMed] [Google Scholar]
- 92.Carrera MR, Ashley JA, Hoffman TZ, et al. Investigations using immunization to attenuate the psychoactive effects of nicotine. Bioorg Med Chem. 2004;12(3):563–70. doi: 10.1016/j.bmc.2003.11.029. [DOI] [PubMed] [Google Scholar]
- 93.Malin DH, Alvarado CL, Woodhouse KS, et al. Passive immunization against nicotine attenuates nicotine discrimination. Life Sci. 2002;70(23):2793–8. doi: 10.1016/S0024-3205(02)01523-0. [DOI] [PubMed] [Google Scholar]
- 94.Moreno AY, Azar MR, Warren NA, et al. A critical evaluation of a nicotine vaccine within a self-administration behavioral model. Mol Pharm. 2010;7(2):431–41. doi: 10.1021/mp900213u. [DOI] [PubMed] [Google Scholar]
- 95.Lindblom N, de Villiers SH, Kalayanov G, et al. Active immunization against nicotine prevents reinstatement of nicotine-seeking behavior in rats. Respiration. 2002;69(3):254–60. doi: 10.1159/000063629. [DOI] [PubMed] [Google Scholar]
- 96.Lindblom N, de Villiers SH, Semenova S, et al. Active immunisation against nicotine blocks the reward facilitating effects of nicotine and partially prevents nicotine withdrawal in the rat as measured by dopamine output in the nucleus accumbens, brain reward thresholds and somatic signs. Naunyn Schmiedebergs Arch Pharmacol. 2005;372(3):182–94. doi: 10.1007/s00210-005-0019-0. [DOI] [PubMed] [Google Scholar]
- 97.Malin DH, Moon WD, Goyarzu P, et al. Passive immunization against nicotine attenuates somatic nicotine withdrawal syndrome in the rat. Nicotine Tob Res. 2010;12(4):438–44. doi: 10.1093/ntr/ntq021. [DOI] [PubMed] [Google Scholar]
- 98.Keyler DE, Roiko SA, Earley CA, et al. Enhanced immunogenicity of a bivalent nicotine vaccine. Int Immunopharmacol. 2008;8(11):1589–94. doi: 10.1016/j.intimp.2008.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Tuncok Y, Hieda Y, Keyler DE, et al. Inhibition of nicotine-induced seizures in rats by combining vaccination against nicotine with chronic nicotine infusion. Exp Clin Psychopharmacol. 2001;9(2):228–34. doi: 10.1037/1064-1297.9.2.228. [DOI] [PubMed] [Google Scholar]
- 100.Roiko SA, Harris AC, Keyler DE, et al. Combined active and passive immunization enhances the efficacy of immunotherapy against nicotine in rats. J Pharmacol Exp Ther. 2008;325(3):985–93. doi: 10.1124/jpet.107.135111. [DOI] [PubMed] [Google Scholar]
- 101.Cornish KE, Harris AC, LeSage MG, et al. Combined active and passive immunization against nicotine: minimizing monoclonal antibody requirements using a target antibody concentration strategy. Int Immunopharmacol. 2011;11(11):1809–15. doi: 10.1016/j.intimp.2011.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Corrigall WA. Nicotine self-administration in animals as a dependence model. Nicotine Tob Res. 1999;1(1):11–20. doi: 10.1080/14622299050011121. [DOI] [PubMed] [Google Scholar]
- 103.LeSage MG, Keyler DE, Collins G, et al. Effects of continuous nicotine infusion on nicotine self-administration in rats: relationship between continuously infused and selfadministered nicotine doses and serum concentrations. Psychopharmacology (Berl) 2003;170(3):278–86. doi: 10.1007/s00213-003-1539-2. [DOI] [PubMed] [Google Scholar]
- 104.Bevins RA, Wilkinson JL, Sanderson SD. Vaccines to combat smoking. Expert Opin Biol Ther. 2008;8(4):379–83. doi: 10.1517/14712598.8.4.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Trial watch: Xenova’s TA-NIC vaccine shows promise Expert Rev Vaccines. 2004;3(4):386. doi: 10.1586/14760584.3.4.386. [DOI] [PubMed] [Google Scholar]
- 106.Cerny EH, Cerny T. Vaccines against nicotine. Hum Vaccin. 2009;5(4):200–5. doi: 10.4161/hv.5.4.7310. [DOI] [PubMed] [Google Scholar]
- 107.Nabi Biopharmaceuticals announces results of first NicVAX® phase III clinical trial: smoking cessation immunotherapy failed to meet primary endpoint. Rockville (MD): Nabi Pharmaceuticals, 2011
- 108.Gunnell D, Irvine D, Wise L, et al. Varenicline and suicidal behaviour: a cohort study based on data from the General Practice Research Database. BMJ. 2009;339:b3805. doi: 10.1136/bmj.b3805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ross S, Williams D. Bupropion: risks and benefits. Expert Opin Drug Saf. 2005;4(6):995–1003. doi: 10.1517/14740338.4.6.995. [DOI] [PubMed] [Google Scholar]
- 110.Hall W. The prospects for immunotherapy in smoking cessation. Lancet. 2002;360(9339):1089–91. doi: 10.1016/S0140-6736(02)11134-2. [DOI] [PubMed] [Google Scholar]
- 111.Brischoux F, Chakraborty S, Brierley DI, et al. Phasic excitation of dopamine neurons in ventral VTA by noxious stimuli. Proc Natl Acad Sci U S A. 2009;106(12):4894–9. doi: 10.1073/pnas.0811507106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Hnasko TS, Sotak BN, Palmiter RD. Morphine reward in dopamine-deficient mice. Nature. 2005;438(7069):854–7. doi: 10.1038/nature04172. [DOI] [PubMed] [Google Scholar]
- 113.Naqvi NH, Rudrauf D, Damasio H, et al. Damage to the insula disrupts addiction to cigarette smoking. Science. 2007;315(5811):531–4. doi: 10.1126/science.1135926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Rose JE, Mukhin AG, Lokitz SJ, et al. Kinetics of brain nicotine accumulation in dependent and nondependent smokers assessed with PET and cigarettes containing 1 1C-nicotine. Proc Natl Acad Sci U S A. 2010;107(11):5190–5. doi: 10.1073/pnas.0909184107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Fagerström K. Determinants of tobacco use and renaming the FTND to the Fagerström Test for Cigarette Dependence. Nicotine Tob Res. 2012;14(1):75–9. doi: 10.1093/ntr/ntr137. [DOI] [PubMed] [Google Scholar]
- 116.Rose JE, Behm FM, Westman EC, et al. Dissociating nicotine and nonnicotine components of cigarette smoking. Pharmacol Biochem Behav. 2000;67(1):71–81. doi: 10.1016/S0091-3057(00)00301-4. [DOI] [PubMed] [Google Scholar]
- 117.Hughes JR, Rose GL, Callas PW. Nicotine is more reinforcing in smokers with a past history of alcoholism than in smokers without this history. Alcohol Clin Exp Res. 2000;24(11):1633–8. doi: 10.1111/j.1530-0277.2000.tb01964.x. [DOI] [PubMed] [Google Scholar]
- 118.Rose JE. Nicotine and nonnicotine factors in cigarette addiction. Psychopharmacology (Berl) 2006;184(3–4):274–85. doi: 10.1007/s00213-005-0250-x. [DOI] [PubMed] [Google Scholar]
- 119.Clemens KJ, Caille S, Stinus L, et al. The addition of five minor tobacco alkaloids increases nicotine-induced hyperactivity, sensitization and intravenous self-administration in rats. Int J Neuropsychopharmacol. 2009;12(10):1355–66. doi: 10.1017/S1461145709000273. [DOI] [PubMed] [Google Scholar]
- 120.Belluzzi JD, Wang R, Leslie FM. Acetaldehyde enhances acquisition of nicotine self-administration in adolescent rats. Neuropsychopharmacology. 2005;30(4):705–12. doi: 10.1038/sj.npp.1300586. [DOI] [PubMed] [Google Scholar]
- 121.van Amsterdam J, Talhout R, Vleeming W, et al. Contribution of monoamine oxidase (MAO) inhibition to tobacco and alcohol addiction. Life Sci. 2006;79(21):1969–73. doi: 10.1016/j.lfs.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 122.Barrett SP. The effects of nicotine, denicotinized tobacco, and nicotine-containing tobacco on cigarette craving, withdrawal, and self-administration in male and female smokers. Behav Pharmacol. 2010;21(2):144–52. doi: 10.1097/FBP.0b013e328337be68. [DOI] [PubMed] [Google Scholar]
- 123.Benowitz NL, Hall SM, Herning RI, et al. Smokers of lowyield cigarettes do not consume less nicotine. N Engl J Med. 1983;309(3):139–42. doi: 10.1056/NEJM198307213090303. [DOI] [PubMed] [Google Scholar]
- 124.Caggiula AR, Donny EC, White AR, et al. Cue dependency of nicotine self-administration and smoking. Pharmacol Biochem Behav. 2001;70(4):515–30. doi: 10.1016/S0091-3057(01)00676-1. [DOI] [PubMed] [Google Scholar]
- 125.Shiffman S, Ferguson SG, Gwaltney CJ. Immediate hedonic response to smoking lapses: relationship to smoking relapse, and effects of nicotine replacement therapy. Psychopharmacology (Berl) 2006;184(3-4):608–18. doi: 10.1007/s00213-005-0175-4. [DOI] [PubMed] [Google Scholar]
- 126.Malaiyandi V, Sellers EM, Tyndale RF. Implications of CYP2A6 genetic variation for smoking behaviors and nicotine dependence. Clin Pharmacol Ther. 2005;77(3):145–58. doi: 10.1016/j.clpt.2004.10.011. [DOI] [PubMed] [Google Scholar]
- 127.Schoedel KA, Hoffmann EB, Rao Y, et al. Ethnic variation in CYP2A6 and association of genetically slow nicotine metabolism and smoking in adult Caucasians. Pharmacogenetics. 2004;14(9):615–26. doi: 10.1097/00008571-200409000-00006. [DOI] [PubMed] [Google Scholar]
- 128.Benowitz NL, Perez-Stable EJ, Herrera B, et al. Slower metabolism and reduced intake of nicotine from cigarette smoking in Chinese-Americans. J Natl Cancer Inst. 2002;94(2):108–15. doi: 10.1093/jnci/94.2.108. [DOI] [PubMed] [Google Scholar]
- 129.Tyndale RF, Sellers EM. Genetic variation in CYP2A6-mediated nicotine metabolism alters smoking behavior. Ther Drug Monit. 2002;24(1):163–71. doi: 10.1097/00007691-200202000-00026. [DOI] [PubMed] [Google Scholar]
- 130.Schnoll RA, Patterson F, Wileyto EP, et al. Nicotine metabolic rate predicts successful smoking cessation with transdermal nicotine: a validation study. Pharmacol Biochem Behav. 2009;92(1):6–11. doi: 10.1016/j.pbb.2008.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Hughes JR, Keely J, Naud S. Shape of the relapse curve and long-term abstinence among untreated smokers. Addiction. 2004;99(1):29–38. doi: 10.1111/j.1360-0443.2004.00540.x. [DOI] [PubMed] [Google Scholar]
- 132.West R, Sohal T. ‘Catastrophic’ pathways to smoking cessation: findings from national survey. Bmj. 2006;332(7539):458–60. doi: 10.1136/bmj.38723.573866.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Gonzales D, Rennard SI, Nides M, et al. Varenicline, an alpha4beta2 nicotinic acetylcholine receptor partial agonist, vs sustained-release bupropion and placebo for smoking cessation: a randomized controlled trial. JAMA. 2006;296(1):47–55. doi: 10.1001/jama.296.1.47. [DOI] [PubMed] [Google Scholar]
- 134.Zatonski W, Cedzynska M, Tutka P, et al. An uncontrolled trial of cytisine (Tabex) for smoking cessation. Tob Control. 2006;15(6):481–4. doi: 10.1136/tc.2006.016097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.West R, Zatonski W, Cedzynska M, et al. Placebocontrolled trial of cytisine for smoking cessation. N Engl J Med. 2011;365(13):1193–200. doi: 10.1056/NEJMoa1102035. [DOI] [PubMed] [Google Scholar]
- 136.Leader AE, Lerman C, Cappella JN. Nicotine vaccines: will smokers take a shot at quitting? Nicotine Tob Res. 2010;12(4):390–7. doi: 10.1093/ntr/ntq015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Lu D, Hickey AJ. Pulmonary vaccine delivery. Expert Rev Vaccines. 2007;6(2):213–26. doi: 10.1586/14760584.6.2.213. [DOI] [PubMed] [Google Scholar]
- 138.Davis SS. Nasal vaccines. Adv Drug Deliv Rev. 2001;51(1–3):21–42. doi: 10.1016/S0169-409X(01)00162-4. [DOI] [PubMed] [Google Scholar]
- 139.Hall W, Gartner C. Ethical and policy issues in using vaccines to treat and prevent cocaine and nicotine dependence. Curr Opin Psychiatry. 2011;24(3):191–6. doi: 10.1097/YCO.0b013e328345922b. [DOI] [PubMed] [Google Scholar]
- 140.Hasman A, Holm S. Nicotine conjugate vaccine: is there a right to a smoking future? J Med Ethics. 2004;30(4):344–5. doi: 10.1136/jme.2002.001602. [DOI] [PMC free article] [PubMed] [Google Scholar]


