Abstract
We present a case of Horner's syndrome occurring as a complication of thyroidectomy. A 42-year-old female patient presented with eyelid drop which developed immediately after thyroidectomy for goitre. Ophthalmic examination revealed eyelid ptosis, miosis and anhidrosis. Preoperative ultrasonography showed multiple isohyperechogenic solid nodules in each lobe, consistent with multinodular goitre. Therefore, the patient underwent subtotal thyroidectomy. The ophthalmic findings did not improve at the end of 6 months follow-up. Similar cases have been reported related to neck tumours or their surgery, mediastinum-located goitre and retropharyngeal abscess surgeries, but not after benign nodular goitre surgery. Several possible mechanisms have been proposed to explain this phenomenon; anatomical variations making the patient susceptible to damage to the sympathetic chain seem to be most likely in our patient.
Background
Horner's syndrome (HS) is the result of a disruption at various levels of the sympathetic innervations of the eye and adnexa.1 The syndrome is characterised by a triad of symptoms, specifically ipsilateral lid ptosis, miosis and anhidrosis. According to the localisation of the sympathetic system dysfunction, it can be classified as central, preganglionic or postganglionic.1 During a long course of preganglionic fibres, from the ciliospinal centre to the superior cervical ganglion, many factors can cause HS. Some of these are apical pleural lesions, pancoast tumour, carotid and aortic aneurysm and dissection, neck lesions and surgery to correct these problems.2–5 In the literature, HS is associated with thyroid gland malignancies, mediastinal goitre or their surgeries.6–15 In addition, temporary cases have been reported due to benign lesions.16–18 We aimed to report a permanent HS case arising after a subtotal thyroidectomy for benign multinodular goitre and evaluate its possible causes.
Case presentation
A 42-year-old female patient was admitted with eyelid drop immediately after goitre surgery. She had undergone a subtotal thyroidectomy 2 days before in a general surgery clinic with a diagnosis of multinodular goitre. In addition to a complete ophthalmic examination, preoperative and operative findings were obtained from medical records. Pulmonary diseases, general surgery and neurology consultations were carried out for differential diagnosis.
Ophthalmic examination revealed right miosis, ptosis and anhidrosis, being in accordance with Horner's syndrome (figure 1). Hertel exophthalmometer readings were 14 and 16 mm in the right and left, respectively. Globe movements, visual acuity, anterior and posterior segment examinations were normal. Preoperative ultrasonography showed isohyperechogenic multiple solid nodules in each lobe, the biggest of which was in the right lobe and had a 4.5 cm diameter; this was consistent with multinodular goitre (figure 2). Haematoma, seroma and infection were ruled out as the possible causes after a careful general surgery exploration. No other pathology which could lead to HS was found in other clinical examinations. Thus, HS was attributed to damage to the cervical sympathetic chain. Histopathological studies reported benign multinodular goitre and revealed no malignancy (figure 3).
Figure 1.

Clinical appearance of patients.
Figure 2.
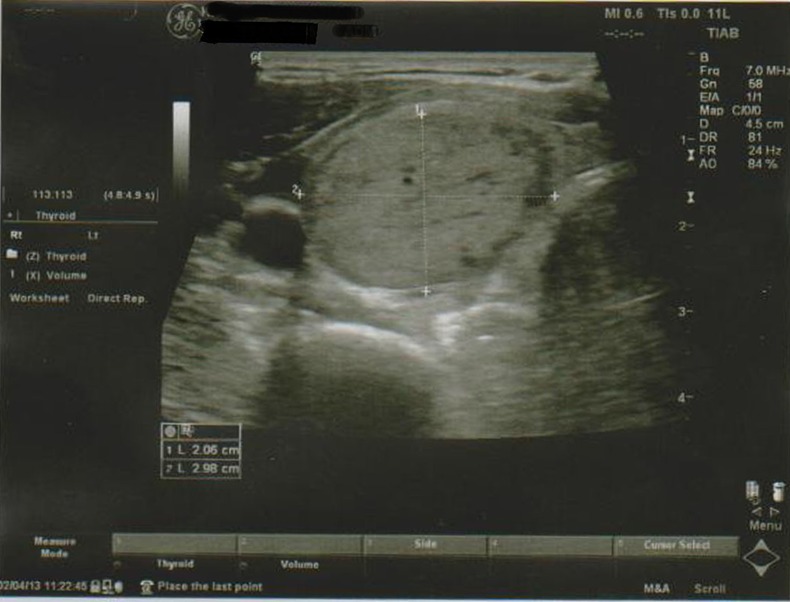
Preoperative ultrasonography.
Figure 3.
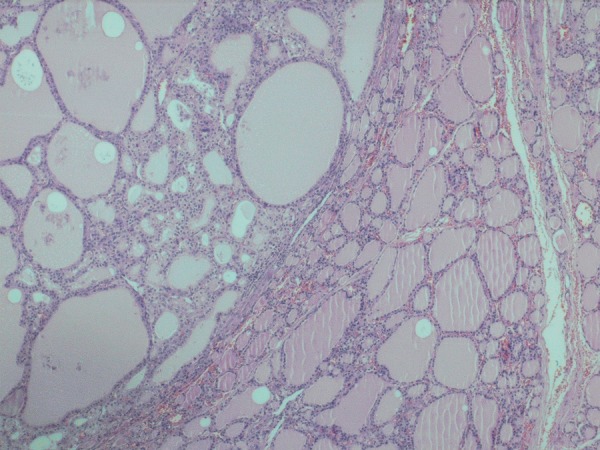
The follicle structures in various sizes and shapes, and colloid filled lumens (H&E ×100).
Outcome and follow-up
There was no improvement in the findings of HS at the end of 6-month follow-up.
Discussion
Horner's syndrome was first described by Horner in 1869 and is a combination of ptosis, miosis with or without facial anhidrosis.1 These findings are due to interruption of the sympathetic innervations to Mueller's muscle of the eyelids and to the dilator muscle of the iris, and to the sweat glands of the face.
HS occurring preoperatively as a result of thyroid pathologies reported in the literature has mainly involved with malignant tumours.9–12 14 Through the direct invasion of the cervical sympathetic nerves or a pressure effect, malignant tumours of the thyroid and parathyroid glands can cause HS. The prognoses of HS after surgery, might be depending on the mechanism of occurrence, were variable in these reports. There were partially or totally recovered or persisted cases. Contrary to these reports, a recent review by Leuchter et al14 has corrected the formerly held view that the majority results from an underlying malignant process of the thyroid rather than benign pathology. Series of Harding et al13 and Lowry et al16 supported the view of Leuchter. They observed improvement in HS in the early postoperative period.
Neck surgeries for the treatment of benign or malignant thyroid lesions may also result in HS.2 3 5–8 A few patients who underwent surgery for benign goitre were observed to develop a transient HS.19 20 The present case had a subtotal thyroidectomy due to benign multinodular goitre. However, HS did not improve at the end of 6-month follow-up.
HS after thyroid and parathyroid surgeries is a very rare complication, and it has been reported in about 0.2% of malignancies.6 13 21 Cases of HS related to benign lesions and their surgeries have been reported sporadically, and their frequency has not been noted.
The following possible mechanisms have been proposed to explain this phenomenon: sympathetic chain injury during retraction of the carotid sheath; anatomical variations making the patient susceptible to damage to the sympathetic chain; application of pressure on the sympathetic chain by postoperative haematoma or seroma; and ischaemic damage of the sympathetic chain. Of these, permanent damage to the cervical sympathetic chain due to anatomical variations seems to be the most likely in the present case.
The sympathetic chain in the neck region may be affected by a number of factors, including various pathologies and surgeries, and does not necessarily imply malignancy. Regardless of the pathology, maximum attention should be paid to the neighbouring tissues such as the recurrent laryngeal nerve and the sympathetic chain during surgical excision. Inattentive surgical dissection is likely to permanently damage the sympathetic nerve fibres showing different anatomical courses.
Learning points.
Although it is rare, Horner's syndrome may appear in relation to neck pathologies.
An effect to the sympathetic chain in the neck region due to pathologies or surgeries is not an indicative of malignancy.
Anatomical variations may make the patient susceptible to damage to the sympathetic chain. Hence, thorough knowledge of anatomy, careful surgical dissection and avoidance of excessive traction with speculum should be carried out to prevent such damage.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Kanski JJ. Clinical ophthalmology. A systemic approach. 6th edn. International Edition Elsevier, 2007:804–7 [Google Scholar]
- 2.González-Aguado R, Morales-Angulo C, Obeso-Agüera S, et al. Horner's syndrome after neck surgery. Acta Otorrinolaringol Esp 2012;2013:299–302 [DOI] [PubMed] [Google Scholar]
- 3.Allen AY, Meyer DR. Neck procedures resulting in Horner syndrome. Ophthal Plast Reconstr Surg 2009;2013:16–18 [DOI] [PubMed] [Google Scholar]
- 4.Gozke E, Taştekin Toz H, Koytak P Kahraman, et al. Postcoital internal carotid artery dissection presenting as isolated painful horner syndrome: a case report. Case Rep Neurol Med 2013;Article ID 403647, 3 http://dx.doi.org/10.1155/2013/403647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bozza F, Vigili MG, Ruscito P, et al. Surgical management of parapharyngeal space tumours: results of 10-year follow-up. Acta Otorhinolaryngol Ital 2009;2013:10–15 [PMC free article] [PubMed] [Google Scholar]
- 6.Lee YS, Nam KH, Chung WY, et al. Postoperative complications of thyroid cancer in a single center experience. J Korean Med Sci 2010;2013:541–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tsakiridis K, Visouli AN, Zarogoulidis P, et al. Resection of a giant bilateral retrovascular intrathoracic goiter causing severe upper airway obstruction, 2 years after subtotal thyroidectomy: a case report and review of the literature. J Thorac Dis 2012;2013:41–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vilallonga R, Fort JM, Mazarro A, et al. Postthyroidectomy Horner's syndrome. Case Rep Med 2012;2013:316984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yip D, Drachtman R, Amorosa L, et al. Papillary thyroid cancer presenting as Horner syndrome. Pediatr Blood Cancer 2010;2013:739–41 [DOI] [PubMed] [Google Scholar]
- 10.Broome JT, Gauger PG, Miller BS, et al. Anaplastic thyroid cancer manifesting as new-onset Horner syndrome. Endocr Pract 2009;2013:563–6 [DOI] [PubMed] [Google Scholar]
- 11.Billie JD, Wetzel WJ, Suen JY. Thyroid lymphoma with adjacent nerve paralysis. Arch Otolaryngol 1982;2013:517–19 [DOI] [PubMed] [Google Scholar]
- 12.Freeman JL, Van den Brekel MW, Brown D. Carcinoma of the thyroid presenting as Horner's syndrome. J Otolaryngol 1997;2013:387–8 [PubMed] [Google Scholar]
- 13.Harding JL, Sywak MS, Sidhu S, et al. Horner's syndrome in association with thyroid and parathyroid disease. ANZ J Surg 2004;2013:442–5 [DOI] [PubMed] [Google Scholar]
- 14.Leuchter I, Becker M, Mickel R, et al. Horner's syndrome and thyroid neoplasms. ORL J Otorhinolaryngol Relat Spec 2002;2013:49–52 [DOI] [PubMed] [Google Scholar]
- 15.Van Santen HM, Aronson DC, Vulsma T, et al. Frequent adverse events after treatment for childhood-onset differentiated thyroid carcinoma: a single institute experience. Eur J Cancer 2004;2013:1743–51 [DOI] [PubMed] [Google Scholar]
- 16.Lowry SR, Shinton RA, Jamieson G, et al. Benign multinodular goitre and reversible Horner's syndrome. BMJ 1988;2013:529–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pishdad GR, Pishdad P, Pishdad R. Horner's syndrome as a complication of percutaneous ethanol treatment of thyroid nodule. Thyroid 2011;2013:327–8 [DOI] [PubMed] [Google Scholar]
- 18.Moreno P Ferriz, Infante JM Bravo, Valderrábano Garralda E, et al. [Horner syndrome secondary to thyroid hydatid cyst]. Med Clin (Barc) 1982;2013:284–6 [PubMed] [Google Scholar]
- 19.Cozzaglio L, Coladonato M, Doci R, et al. Horner's Syndrome as a complication of thyroidectomy: report of a case. Surg Today 2008;2013:1114–16 [DOI] [PubMed] [Google Scholar]
- 20.Solomon P, Irish J, Gullane P. Horner's syndrome following a thyroidectomy. J Otolaryngol 1993;2013:454–6 [PubMed] [Google Scholar]
- 21.Patel S, Ilsen PF. Acquired Horner's syndrome: clinical review. Optometry 2003;2013:245–56 [PubMed] [Google Scholar]


