Abstract
Mucus plugging plays a vital role in the pathophysiology of fatal and near fatal asthma as demonstrated in various postmortem studies. There is a paucity of published literature on how to manage mucus plugging in adult patients with refractory asthma exacerbation not responding to conventional therapies as compared with its paediatric cohort. We describe a dramatic improvement with the use of rhDNase, following bronchoalveolar lavage in an intubated adult female patient, with status asthmaticus refractory to conventional treatment.
Background
Acute near-fatal asthma represents the most severe form of asthma exacerbation associated with the presence of hypercapnia requiring mechanical ventilation. Postmortem series show pathological presence of inflammatory cells, mucus plugging, shedding of airway epithelium, airway oedema and smooth muscle hypertrophy.1 Airway obstruction in severe asthma that does not respond to conventional therapy, may be caused by mucus plugging. Evidence for the management of mucus plugging in adult patients with severe near fatal asthma is sparse. We describe a patient with fatal asthma who responded dramatically to DNase, following bronchoscopy and lavage after failing other therapies.
Case presentation
A fit 67-year-old woman presented with with cough, chest tightness, breathlessness and wheeze for over 2 weeks preceded by coryzal symptoms. She had underlying apparent controlled asthma for 20 years. She had been compliant on step 3 maintenance therapy2 with combination of long-acting β agonist/steroids and salbutamol inhalers. She had no prior admissions and her last exacerbation was more than a year ago. She had a 25 pack-year smoking history.
On arrival at the emergency department, she had the features of life-threatening asthma. Her oxygen saturation was 88% on air and her heart rate was 110 bpm. She was wheezy with signs of accessory muscle use. Initial investigations showed normal inflammatory markers, normal eosinophil count of 0.2 × 109/L and arterial blood gas (ABG) showed pH 7.36, pCO2 5.6, pO2 6.73, base excess 23.4, FiO2 0.21. Chest X-ray showed hyperinflation without consolidation or pneumothorax.
Despite treatment with oxygen, nebulised salbutamol and ipratropium, steroids, magnesium sulfate and aminophylline, she deteriorated with pH 7.32, pCO2 7.21, pO2 11.02, HCO3 24.3 and FiO2 0.8. She was escalated to intensive care, intubated and ventilated with biphasic positive airway pressure of Pinsp 27and positive end-expiratory pressure 7, and achieved a tidal volume of 400 mL. Intravenous salbutamol and propofol infusions were started. Despite that, she continued to deteriorate over 24 h with an ABG pH of 6.90 and PCO2 20. She was subsequently paralysed, and hence was ventilated via synchronised intermittent mandatory ventilation requiring a peak inspiratory pressure of up to 45 cm H2O.
Investigations
CT thorax showed no obstruction, pneumothorax, emphysema, bronchiectasis or parenchymal disease. On coronal sections, sudden tapering of bronchi indicated possible mucus plugging (figure 1). Total IgE was not raised, and serum aspergillus and fungi precipitins were negative.
Figure 1.
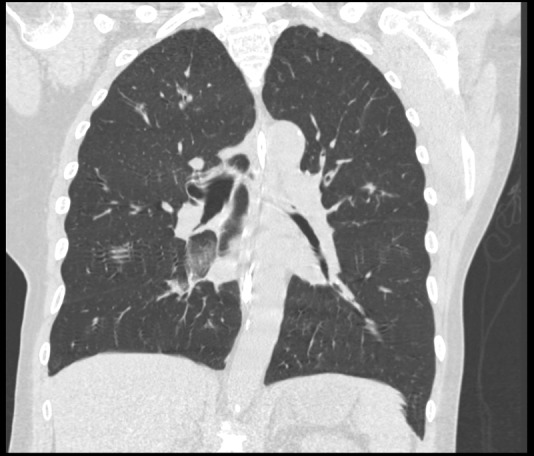
Coronal section of the lung showing sudden truncation of the bronchi.
Treatment
Bronchoscopy and toileting was subsequently performed showing copious mucus plugging in the airways. Bronchoalveolar lavage later revealed only scanty candida. Nebulised rhDNase (Dornase α) 2.5 mg was then given via endotracheal tube thrice daily, followed by aggressive physiotherapy. Peak airway pressure came down to 20–25 cmH2O within 6 h after starting of nebulised rhDNase and was sustained. She was steadily weaned and was extubated 72 h later.
Outcome and follow-up
Twelve days following admission, she was discharged on symbicort 200/64 puffs twice daily, and 1 puff when necessary up to a daily total of 12 puffs per day as per the SMART regime. Spirometry prior to discharge showed some evidence of small airways obstruction with FVC of 3.62 L (138%), FEV1 2.32 L (106%), FEV1/FVC 63, FEF25–75 33% and PEFR 365 L/min. Her symptom control on follow-up was good. A repeat spirometry 2 months later showed FVC 3.33 L (116%), FEV1 2.39 L (106%), EV1/FVC 72, FEF25–75 68%, indicating improvement with no evidence of fixed airway obstruction.
Discussion
Acute severe asthma is characterised by severe airways obstruction secondary to bronchospasm, airway inflammation and mucus plugging. Most acute severe exacerbations respond well to conventional therapy including mechanical ventilation. A small proportion who fail to respond continue to have significant airways obstruction due to mucus plugging; giving rise to worsening dynamic hyperinflation and increased work of ventilation leading invariably to death.1 3 Postmortem series have demonstrated time and again extensive airway narrowing, extensive plugging of the airways with mucus and inflammatory infiltrates, hyperinflation and atelectasis.1 3
Although a smoker, she only had asthma, as suggested by CT thorax and spirometry. Initial management of near fatal asthma is aimed at correcting hypoxaemia and treating bronchospasm, while concurrently identifying life-threatening signs and presence of acidaemia.2 4 With this in mind, obtaining an ABG on air, as in this patient's initial assessment, highlights the potential pitfall of management. This article hopes to serve as a reminder that maintaining the ABCDs in an acutely unwell patient is crucial. Not only that, early intensive care unit involvement is paramount; as further deterioration, despite maximal therapy, would warrant invasive ventilation.2 4 5 This patient failed to respond to conventional treatment including intravenous salbutamol, propofol and mechanical ventilation. CT thorax showed truncated bronchi, and bronchoscopy confirmed the presence of mucus plugging. With bronchial toileting and nebulised rhDNase, the patient made a sustained recovery with successful weaning off mechanical ventilation. We believe that the combined use of rhDNase, bronchial toileting and aggressive physiotherapy, on top of mechanical ventilation strategies and intravenous bronchodilators, helped turn the corner.
The evidence for the use of rhDNase in management of asthma exacerbation is sparse. Elevated mucus DNA levels have been found in patients with acute asthma; albeit lower than that of cystic fibrosis.6 The use of DNase had been described in case series with good outcome.7 8 Observational data from paediatric cohort of 46 ventilated children showed good efficacy and safety of DNase use.9 However, there was no difference in outcome when compared with conventional therapy for treating moderate to severe exacerbations in a paediatric cohort.10
This patient, to our knowledge, is the second adult patient in the literature7 with status asthmaticus who responded dramatically to DNase after failing conventional therapies. We conclude that DNase is potentially an effective adjunct together with bronchioalveolar lavage in ventilated adults with refractory status asthmaticus. Further research in the form of randomised controlled studies would be useful but obviously difficult in this cohort.
Learning points.
Severe acute asthma not responding to conventional treatment may be caused by underlying mucus plugging.
Imperative early escalation to intensive care.
DNase with bronchoalveolar lavage may be a useful adjunct in management.
Footnotes
Contributors: AC and DJM were clinicians who treated the patient. AC and DJM made literature search and decisions of treatment, and sought advice from DM. AC was responsible for the write up of the case. Both DJM and DM reviewed and contributed ideas.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Kuyper LM, Pare PD, Hogg JC, et al. Characterization of airway plugging in fatal asthma. Am J Med 2003;2013:6–11 [DOI] [PubMed] [Google Scholar]
- 2. 2012 BTS/SIGN Asthma Guidelines. [Google Scholar]
- 3.Rodrigo GJ, Rodrigo C, Hall JB. Acute asthma in adults—a review. Chest 2004;2013:1081–102 [DOI] [PubMed] [Google Scholar]
- 4.Stanley D, Tunnicliffe W. Management of life-threatening asthma in adults. Oxford JMed BJA: CEACCP 2008;2013:95–9 [Google Scholar]
- 5.Restrepo RD, Peters J. Near-fatal asthma: recognition and management. Curr Opin in Pulm Med 2008;2013:13–23 [DOI] [PubMed] [Google Scholar]
- 6.Fahy JV, Steiger DJ, Liu J, et al. Markers of mucus secretion and DNA levels in induced sputum from asthmatic and from healthy subjects. Am Rev Respir Dis 1993;2013:1132–7 [DOI] [PubMed] [Google Scholar]
- 7.Hull J, Castle N, Knight R, et al. Nebulised DNAse in life threatening asthma. Resuscitation 2007;2013:175–7 [DOI] [PubMed] [Google Scholar]
- 8.Durward A, Forte V, Shemie SD. Resolution of mucus plugging and atelectasis after intratracheal rhDNase therapy in a mechanically ventilated child with refractory status asthmaticus. Crit Care Med 2000;2013:560–2 [DOI] [PubMed] [Google Scholar]
- 9.Nyman A, Puppala K, Colthurst S, et al. Safety and efficacy of intratracheal DNase with physiotherapy in severe status asthmaticus. Crit Care 2011;2013(Suppl 1):P185 [Google Scholar]
- 10.Boogaard R, Smit F, Schornagel R, et al. Recombinant human deoxyribonuclease for the treatment of acute asthma in children. Thorax 2008;2013:141–6 [DOI] [PubMed] [Google Scholar]


