Abstract
Thyroid-associated orbitopathy (TAO) is a self-limiting auto-immune condition usually associated with Grave's disease. It is characterised by ocular pain, eyelid swelling, chemosis, proptosis and keratopathy. As the mechanism for ophthamoplegia and optic neuropathy is the orbital swelling leading to mechanical restriction of ocular muscles and compression of optic nerve, one expects proptosis rather than ptosis in TAO. We describe a case of a young adult woman who presented with acute onset restriction of movement along with partial ptosis and severe diminution of vision in left eye. The MRI of orbit revealed significant swelling of recti along with signal alteration consistent with TAO. The radio-isotope thyroid scan revealed thyroiditis, and thyroid peroxidase (TPO) antibody was significantly high; hence, the diagnosis of Hashimoto thyroiditis was considered. A course of intravenous methylprednisolone followed by oral steroid was administered, which produced marked improvement in vision and extraocular movement.
Background
Thyroid-associated orbitopathy (TAO) is an autoimmune condition characterised by a constellation of symptoms and signs in eyes. The diagnosis of TAO is established based on clinical findings, presence of thyroid stimulating hormone-receptor (TSH-R) antibody and imaging characteristics.1 In few cases TAO complicates Hashimoto's thyroiditis (5%) rather than Grave's ophthalmopathy (GO).2 The former group of patients is positive for thyroid peroxidase (TPO) antibody. The neurological deficit in TAO is similar to orbital apex syndrome as there is palsy of II, III, IV and VI cranial nerves.3 The accompanying ocular swelling, chemosis and proptosis are quite prominent which allow an easy recognition of this condition. In absence of the characteristic eye findings TAO would not be suspected primarily. In such cases the findings on imaging are important in determining the aetiology of orbital apex syndrome. We report a case of a young adult woman who presented to us with symptoms and signs which were localised to orbital apex. The diagnosis of TAO was suspected based on changes in orbital muscles on MRI. This case report is intended to highlight this rare presentation of TAO in the absence of classical eye findings where its diagnosis rests on the findings on MRI.
Case presentation
A 38-year-old woman presented with acute onset pain of moderate to severe intensity around left eye since 18 days. Two days after onset of headache she noticed double vision on gaze towards left and after 2 days there was drooping of left eyelid. Since 12 days the patient had diminution of vision progressed over 3 days to an extent the patient was barely able to perceive the faces with left eye.
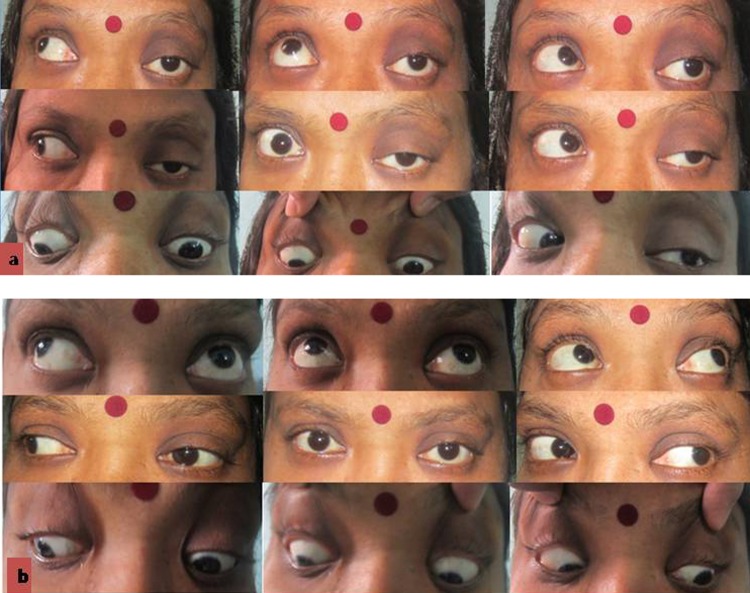
On examination the patient was conscious, oriented, and her vitals and general examination were normal. The pupils were normal and equal in size but the direct and consensual reflex were impaired on left side. The visual acuity was 6/6 on right side and 6/60 on left even after pin-hole correction. There was partial ptosis with restriction of movement of left eyeball in all directions (figure 1A). Rest of nervous system and systemic examination was normal.
Figure 1.
(Aand B) Photographs of patients showing ptosis with marked restriction of extraocular movement in left which improved after on steroids.
Investigations
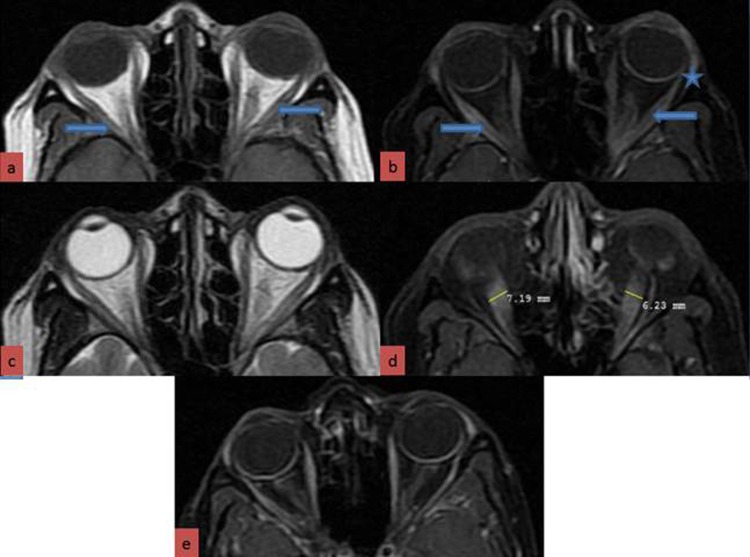
The blood glucose, renal function test, serum electrolytes and haemogram were within normal limits. MRI showed mild swelling of belly of the inferior, medial and lateral recti muscles(>4 mm) with sparing of their tendon insertions. Linear hyperintensitity was observed on T1-weighted sequences which disappeared in the fat-suppressed sequences. Also hyperintensity in these muscles was noted on the T2-weighted images. T1-fat-suppressed sequences with gadolinium showed mild enhancement of these muscles. A mild swelling and enhancement of the left optic nerve too was noticed. A minimal forward displacement of the left eyeball in comparison with its right counterpart was present. The region of apex of left orbit appeared crowded but no excess fat deposition was evident. These changes in the orbital muscles and optic nerve were consistent with thyroid associated orbitopathy (figure 2). The free T3 and FT4 were within normal limit; however, thyroid stimulating hormone (TSH) was markedly low (0.010 µIU/ml). TSH-R antibody was negative but TPO antibody was significantly elevated 185.5 U/ml.Tc-99m-pertechenate thyroid scan showed diffusely reduction in tracer uptake in both lobes. The presence of TPO antibody and a picture of thyroiditis on radio-isotope scan confirmed the diagnosis of Hashimoto's thyroiditis in our case.
Figure 2.
Swollen inferior, medial and lateral recti (A-D) T1-weighted non-enhanced orbital image showing a central linear streak in the lateral recti bilaterally (A) (arrow) which is hypointense on STIR (short tau inversion recovery) sequences (B). The muscle bellies are swollen with sparing of their tendinous insertion (asterisk). Also peripheral enhancement of the recti is seen (B). The T2-weighted images show diffuse hyperintensity (C). T-1 (STIR) gadolinium-enhanced orbital image of an another patient for comparison of abnormal recti in thyroid-associated orbitopathy compared to normal recti (E).
Treatment
Parenteral methyl-prednisolone 1 g/day was given for 5 days which was followed by oral prednisolone 1 mg/kg for month, tapered later on.
Outcome and follow-up
The visual acuity in left eye improved from 6/60 to 6/12. The movement of left eyeball also improved markedly in all gaze, though, some partial ptosis and mild gaze restriction was present (figure 1B).
Discussion
Orbital apex syndrome is a clinical entity characterised by combination of palsy of cranial nerves II, III, IV, VI and sensory loss in V1 distribution of trigeminal nerve. It results from lesions localised to the apex of the orbit. The aetiologies are quite varied and include infections, neoplasm, TAO, granulomatous, iatrogenic mucocele and vascular lesions.4–8 In our case no mass lesions or localised collections were noticed on imaging. MRI showed inflammation and swelling of ocular muscles and optic nerve. The important differentials for diagnosis were TAO and Tolosa-Hunt syndrome (THS). The spindle-shaped swelling of recti with sparing of the tendons is characteristic of TAO.9 Moreover, intramuscular fat deposition visualised as linear hyperintensity on T1-weighted sequences, disappearing on fat-suppressed sequences, is seen in TAO. In THS the T1 characteristics are quite different from that seen in TAO, the affected muscle are iso-intense rather than hyperintense.10 Also in THS the muscle tendons are also involved along with muscles. In our patient, even though thickness of recti just met the criteria laid for diagnosis of TAO, the pattern of signal alteration was quite consistent with TAO, different from that seen in THS. The diagnosis of TAO was further corroborated with the clinical picture of Hashimoto's thyroiditis as indicated by the presence of thyroid peroxidase antibodies and radio-isotope scan consistent with ongoing thyroiditis.11 The impairment of extraocular movement and visual acuity in the absence of externally apparent eye signs could be explained by the early stage of muscle inflammation, lack of orbital fat deposition and the major burden of disease being restricted to the orbital apex. The clinical activity score (CAS) in our case was 4 which predicted a good response to use of anti-inflammatory agents.12 As the parenteral glucocorticoids have been found to be having a higher efficacy, and sensing the emergency as the vision was compromised, intravenous methylprednisolone was given 1 g/day for 5 days followed by oral steroids. The response rate to glucocorticoids is in the range of 63–73%.13 In our case recti hyperintensity on T2-weighted sequences was indicative of intramuscular oedema and lymphocytic infiltration, which is predictive of a favourable response to steroids and immunosuppressants. This explains the significant recovery observed in our case.14
Learning points.
Thyroid-associated orbitopathy (TAO) is diagnosed by the characteristic eye signs resulting from orbital inflammation and swelling.
The patient of TAO may present with ophthalmoplegia and vision impairment in the absence of other classical signs.
The marked swelling of the ocular muscles with sparing of the tendons, the pattern of signal intensity alterations also play a crucial role in clinching the diagnosis.
The distinction between TAO and Tolosa-Hunt syndrome can be well made based on the signal characteristics particularly on T1-weighted sequences.
This case highlights the importance of prompt diagnosis and benefit of institution of parenteral steroids in patients of TAO presenting with vision loss and restricted extraocular movement.
Footnotes
Contributors: RV formulated the hypothesis and rest of the authors helped in preparing the manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Krassas GE, Wiersinga WM. Thyroid eye disease: current concepts and the EUGOGO perspective. Thyroid Int 2005;2013:3–4 [Google Scholar]
- 2.Ludgate ME. Animal models of thyroid associated ophthalmopathy. Thyroid 2002;2013:205–8 [DOI] [PubMed] [Google Scholar]
- 3.Yeh S, Foroozan R. Orbital apex syndrome. Curr Opin Ophthalmol 2004;2013:490–8 [DOI] [PubMed] [Google Scholar]
- 4.Saxena R, Phuljhele S, Aalok L, et al. A rare case of orbital apex syndrome with herpes zoster ophthalmicus in a human immunodeficiency virus-positive patient. Indian J Ophthalmol 2010;2013:527–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kurimoto T, Tonari M, Ishizaki N, et al. Orbital apex syndrome associated with herpes zoster ophthalmicus. Clin Ophthalmol 2011;2013:1603–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sethi A, Sareen D, Mrig S, et al. Acute suppurative otitis media: an unusual cause of orbital apex syndrome. Orbit 2008;2013:462–5 [DOI] [PubMed] [Google Scholar]
- 7.Li Y, Wu W, Xiao Z, et al. Study on the treatment of traumatic orbital apex syndrome by nasal endoscopic surgery. Eur Arch Otorhino-laryngol 2011;2013:341–9 [DOI] [PubMed] [Google Scholar]
- 8.Venkitaraman R, Madhavan J, Ramachandran K, et al. Primary adenoid cystic carcinoma presenting as an orbital apex tumor. Neuroophthalmology 2008;2013:27–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kahaly GJ. Imaging in thyroid-associated orbitopathy. Eur J Endocrinol 2001;2013:107–18 [DOI] [PubMed] [Google Scholar]
- 10.Prabhakar BS, Bahn RS, Smith TJ. Current perspective on the pathogenesis of Grave's disease and ophthalmopathy. Endocrine Rev 2003;2013:802–35 [DOI] [PubMed] [Google Scholar]
- 11.Pearce EN, Farwell AP, Braverman LE. Thyroiditis. N Engl J Med 2003;2013:2646–55 [DOI] [PubMed] [Google Scholar]
- 12.Maheshwari R, Weis E. Thyroid associated orbitopathy. Indian J Ophthalmol 2012;2013:87–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mallika PS, Tan AK, Aziz S, et al. Thyroid associated ophthalmopathy—a review. Malays Fam Physician 2009;2013:8–14 [PMC free article] [PubMed] [Google Scholar]
- 14.Goncalves ACP, Gebrim EM, Monteiro ML. Imaging studies for diagnosing Graves’ orbitopathy and dysthyroid optic neuropathy. Clinics 2012;2013:1327–34 [DOI] [PMC free article] [PubMed] [Google Scholar]