Abstract
Background:
Studies have shown that nurses are under considerable job stress, which can lead to health disorders and failure in duties. Stressors of nursing have been studied in some of quantitative studies; however, a few investigators have studied the nurses’ life experiences in this regard. The current qualitative research aimed to understand the nurses’ experiences and perceptions of job-related stress.
Materials and Methods:
This qualitative study was conducted in 2010-2011 by using the content analysis technique. Data were collected through individual deep interviews with 19 nurses working in hospitals affiliated to Kashan University of Medical Sciences. The content of data was analyzed by the Krippendorff method.
Results:
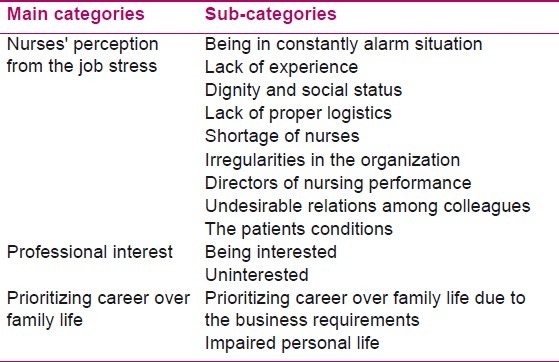
Three categories were emerged including ‘nurses’ perception from the job stress, “professional interest”, and “prioritizing career over family life”. The first category included the following subcategories of “being in constantly alarm situation,” “lack of experience”, “dignity and social status”, “lack of proper logistics”, “shortage of nurses”, “Irregularities in the organization,” “directors of nursing performance,” “undesirable relations among colleagues,” and “the patients conditions all have effects on the nurses’ level of professional stress.
Conclusion:
The study participants defined job stress as a condition in which a nurse is under pressure so that the quality of care and the nurses’ personal and family life is interrupted. Being under continuous pressure, low social dignity, and the manner of nurse managers were among the important sources of job stress. Providing appropriate logistics, improving the coordination within hospital subsystems, and improving the managers and nurses relationships may decrease the stressors in nursing profession.
Keywords: Life experiences, nurse, occupations, perception, psychological stress
INTRODUCTION
Occupational stress will result in decreasing the efficiency and increasing the occupational hazards inside and outside the work environment.[1] According to some estimates, job stress has been the main factor in 70% of absenteeism cases and nearly wasting of 10% of the country’s gross domestic product.[2] The British Health Education Authority has introduced the nursing jobs, police, social work, and teaching as the four careers with high stress. The National Occupational Safety Association of America has placed the nursing job in terms of stress at the head of the medical professions.[3] Cole and Nelson reported that 93% of the nurses were frequently under the influence of stress factors of their workplace.[4] A number of quantitative studies have paid attention to study the job stress in nurses. In one of these studies, the following factors have been introduced as the most important ones for job stress in nursing: equipment and medicine shortages, lack of standard equipments, inappropriate physical environment of hospital, disease transmission, lack of timely medical attendance, and poor communication with co-workers.[1] Ghasemi and Attar has also investigated the occupational stressors in nurses and reported that death and suffering of patients, workload, and nurse-physician conflicts were profoundly contributed to the nurses’ stress.[2] Adib-Hajbagheri, although not paid attention directly to the nurses’ stress, has reported that factors such as organizational culture, lack of support, lack of time, and insufficient clinical experience put pressure on nurses and prevent them to make appropriate clinical decisions and providing evidence-based care.[5,6] Dehghan-Nayeri et al. has also reported that factors such as shortage of nurses, lots of miscellaneous workloads, mismanagement, discrimination, poor relations, and profit-seeking enterprise put the nurses under pressure and reduce their productivity and efficiency.[7] Stora has also stated that occurrence of emergency situations, conflict with the authorities, work rotation, and frequent change of tasks are among the stressful factors for nurses.[8] However, Stora’s report was not based on an original research. There were different questionnaires designed for studying stress and occupational stress.[9–11] However, Polit and Beck have criticized the data gathered through such instruments because of the low response rate and the artificial and superficial nature of such data.[12] On the other hand, few researchers have paid attention to the life experiences of the nurses (in the field of occupational stress) and to the best of our knowledge, no qualitative study is published on occupational stress of Iranian nurses. Our investigations indicated that most studies in this field were quantitative and conducted in Western countries. On the other hand, there are fundamental differences between the health system and medical care services in our country with the developed countries. Hence, conducting a qualitative study in this regard can help to clarify the stress factors in nursing. Considering the effects of stress on physical and mental health of nurses, lack of related studies and attention to personal perceptions, and experiences of nurses in this area, we decided to perform a qualitative study and to evaluate the experiences and perceptions of nurses in the field of occupational stress.
MATERIAL AND METHODS
This qualitative study was conducted in Kashan, Iran, by using the content analysis[13–15] after getting the approval from the Ethics Committee of Kashan University of Medical Sciences. The study population consisted of the nurses of the hospitals affiliated to this university. The sampling was continued until the data saturation, i.e., when the researcher could not achieve a new code.[16] Data were collected through in-depth individual interviews with 19 nurses. Participants had at least two years of experience and no self-reported history of mental illness. By visiting the hospital wards and explaining the research objectives, the nurses met the inclusion criteria, were identified and invited to participate in the research. Exclusion criteria included being discontent, having less than two years of experience, a history of mental illness, lack of employment at the time of research, and applications for study leaving. The main method of data collection was the open semi-structured interviews. Interview guide included a few open-ended questions to allow the participants express their detailed experiences and perceptions. For preparing the interview guide, at first a list of questions about the factors causing stress in the nursing profession were prepared. Some encouraging questions were also made for participants to express their experiences in this field. Then, the interview guide was moderated by the guidance of supervisors and the Research Council. At the beginning of each interview, the participants were asked to describe one of their normal working days. Then, they were asked to express and explain their experiences and perceptions (of all types and levels of job stress in nursing profession). Moreover, they wanted to explain real examples of the stressors in their work. For this reason, the following questions were made: As a nurse, how did you face with stress in your job? Which factors was causing you stress in your job? If possible, please describe the examples of stress for yourself. What made in these experiences that you feel the tension? Although the researcher had the key questions, the questions (largely) were based on the interaction between the interviewer and the interviewee during the interview. The interviews were performed in one or more occasions with respect to environmental factors, patience, and the willingness of the participants. Duration of each session varied from 35 minutes to an hour. Interviews were performed in a private room (at work). The interviews were recorded on a MP3 recorder. At the same day, they were transcribed word by word and were used as the primary research data. The analysis of the data was performed by content analysis according to Krippendorff method.[13–15] In this method, after designing the field work and seeking sources of information, there are some fundamental processes including unitizing, sampling and reduction, inference, and interpretation of data as well as attaining conclusion. Unitizing began after repeated reading of transcribed data until the researcher acquired a general sense of the data. Then, the “unit of analysis” (the words, sentences, and paragraphs which had special meanings and the answers to the questions of the researcher) was identified. This stage was also involved to establish the coding frame. For this purpose, the researcher has marked the risk factors and the outcome issues related to job stress, after reading the data for several times. Therefore, a basic framework occurred for coding and sampling of the data. In continuing the process of analysis, this framework was modified. In sampling stage, the researcher had extracted the representative units of data and placed them within the sampleing framework. Thus, by recognizing the frequency of the data, regarding the meanings of the words and sentences which were the same, they were placed under one structure or meaning. By the progress of the analysis and adjusting the sampling, the data reduction occurred and categories of data were developed. In later stages of inference and conclusion, the researcher interpreted the results and writing data to text. At the baseline, the researcher wrote her comments, experiences, and impressions about the professional stress and its related factors. Then, she frequently refered to this narratives for preventing her mental impact on participants and the findings.
During the study, some methods were used to ensure the data trustworthiness. The nurses were ensured for keeping confidential the names and permission was obtained from the hospital authorities. The participants reviewed and verified data and the extracted codes. For reviewing the process of analysis, the texts of the interviews, codes, and derived categories were also evaluated and confirmed by supervisors and another person experienced in qualitative research. The results were also shared with some nurses who did not participate in the study and they confirmed the fitness of the results. During the study, the confidentiality and freedom of the participants (to participate in research or leave it) was observed. They also gave written consents for recording the interviews.
RESULTS
A total of 19 nurses participated in the present study [Table 1]. Three main categories of “nurses’ perception from occupational stress,” “professional interest,” and “prioritizing career over family life” were emerged from the data [Table 2].
Table 1.
The participants’ characteristics
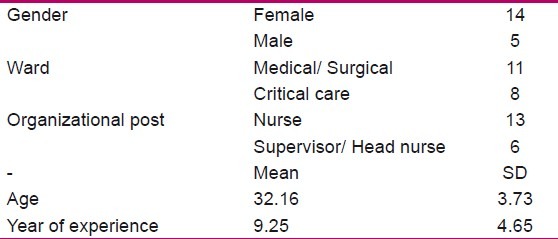
Table 2.
The list of categories and subcategories
Nurses perceptions from the job stress
Based on the experiences of the participants, the occupational stress was defined as a condition caused by working cases or environment in which nursing occurs, and put pressure on nurses. This condition negatively impacts the nursing care and also disrupts the family and personal life of the nurse. This condition (finally) will create or exacerbate the job dissatisfaction in nurses and make them exhausted. The participants’ experiences of stressors in the nursing profession were placed in the following 9 sub-categories:
Being in constantly alarm situation
Participations remembered the followings as the work-related stressors: “hard work,” “bitter events of employment,” and “fear of damage to the patient due to the nurse’s mistake.” But what affected them more than anything were “The critical and unpredictable situations” and “the vital necessity of action in the least possible time.” One nurse said: “The most influencing stress on me is about the patient. For example, the condition of a cardiac patient can be stable during a shift, but suddenly something will happen and affect me mentally very much …”(P5). A supervisor also pointed out that the nurses should always be on alarm status and it is stressful. As she said: “This state of being on constant alarm can confuse the nurse… Sometimes, when you are at home, suddenly at night, awakening from sleep by a small sound or noise, and think that someone is calling you …”(P11). He believed that such a situation kept the nurse in constant stress mode and a constant mental engagement which will wear her. Some participants noted that the stress intensity is associated with age, work experience, hours worked per week, the place of work, and the personality of the nurse. They believed that whatever the workload be greater, the alarm situation will be more annoying. Two participants said: “The amount of stress is also depends on the person, how to deal with the cases and what matters for you …”(P11). “If we just work on our assigned shift, and we do not have mandatory overtime, the stress will be less …”(P2).
Lack of experience
A number of participants, who had less work experience, mentioned the “lack of preparedness for dealing with events,” as an important stressful factor. A nurse with 5 years of experience said: “Once, at the beginning when I had come to the CCU, one night, I was alone in the station, suddenly I saw the heart beat of one of the patients dropped…, I ran toward him… and I understood that the chest leads were isolated. In that night, I was very afraid and had lots of stress, I thought that I was faced with an asystole case and the patient was dead”(P2). She believed that the reason for this was her little inexperience. Experienced nurses also pointed to tensions arising from the lack of preparedness. These tensions were created in the two situations of “sudden change in the workplace” and “concerning about the lack of readiness of the partner.” Two nurses told their ideas about these cases: “When you suddenly transferred to a new section, this issue can create stress, because your partners that you work together are changed and the patients’ situations are also different”(P14). “When they put a newcomer partner who is not familiar with the job in the shift, her stress is also entered to other personnel …”(P7).
Dignity and social status
The participants have stated that the position and social status (not very desirable for nursing profession) are stress factors. This issue has been imposed a chronic stress on them and caused occupational fatigue and loss of ability to do their social roles. One participant said: “Nursing has no social prestige at all”(P2). Another participant has noted about the transfer of stress from social adverse position to the family and its effects on professional practice. She said: “My husband’s father, so far for five or six times, told me that we did not want our bride to be a nurse…”(P4). Other participant mentioned that inadequate amount of nurse’s salary is arising from its inappropriate social status. He noted that when people are aware of the salaries of the nurses, view them humiliating. She said: “If someone at a party asks about our salaries, we add two or three hundred tomans extra to it. We were embarrassed to tell the truth”(P11).
Lack of proper logistics
All the participants remembered the lack of logistics and professional support as stress factors. Some of them have noted that the lack of procurement causes “The hospital environment to be painful” for a nurse. One nurse said: “The patient is suffering due to breathing or the heart. He/she needs to be supported. Now you should be looking where to find the ventilator… There should be a standby ventilator In the CCU”(P5). Some participants have noted that lack of logistics is not limited to the healthcare facilities, but also the care-givers do not have access to appropriate facilities in the hospital. Another nurse pointed out about the inappropriateness of the hospital nursery. She emphasized that instead of thinking about patients, she was concerned with her child in daycare center. She said: “When the children are brought to the hospital nursery, constantly, I thought about my children that nothing was happened to them. Because the kindergarten manager was an old woman who was unable to take care of herself …”(P10).
Shortage of Nurses
The participants frequently mentioned about shortage of nurses as one of the main causes of occupational stress. Their experiences showed that this deficiency can cause stressful consequences, such as “forced overtime,” “physical and mental exhaustion,” “loss of family entertainment and interaction,” and “increase the likelihood of error.” One participant said: “The hospital nurses are low. We have to work overtime”(P15). A supervisor, in reference to the effect of the staff shortage on their fatigue and the increase in the likelihood of error, said: “Our nurses are tired …they have forced for overtime and this issue increases the probability of error…”(P16). Another participant, in order to show the negative effects of excessive shifts (due to the shortage of nurses) on family relations, said: “When I go home in the morning after the night shift, I only want to sleep. The family expects to go somewhere with them, but I am not able to go there, or if go, I only take a nap there…”(P11).
Irregularities in the organization
Some of the participants have mentioned about the irregularities and inconsistencies between different parts of the hospital as a cause of stress. One participant referred to this issue and its impact in the increased stress of the nurses: “For example, when you send an emergency test, we know that up to 3 hours, we will not receive the answer. If I call the lab, we do not get it anyhow. These things will cause the inconsistency and increasing the occupational stresses”(P1). Participants believed that a part of the disorder was associated with the performance of the physicians. Two nurses mentioned about the lack of coordination, delay, unavailability of doctors, disputes between doctors and nurses, which all of them are stressful. They said: “When a patient is very ill, it takes half an hour for coming the intern or the resident…to give you an order. It caused stress will be doubled, especially in the evening and night shifts”(P2). “The first year resident makes a statement, the second year resident comes and hold it, the senior resident puts another order, the attend comes and makes a DC. The nurse does not know to execute which of the commands…and it is really confusing”(P4). One of the instances of irregularities in the system was “the lack of a clear job description” and “nurses deviated from their main tasks.” Based on the experiences of the participants, these factors create a conflict with the role of the nurses, put them under pressure, and they were exhausted. One nurse said: “While we need to be at the patient bedside and give him the needed health care training, instead we should do the secretary jobs, labor work and work as of the Guardians”(P1). In this situation, the consequences of failure are transferred to the nurses and they will be called into account. So, in many cases, the nurses’ minds should deal with these disorders and are involved with their consequences. This issue increases the mental stress. One participant said: “Your mind is engaged. You are doing your best. But the system will put all the problems on your neck… such cases makes the nurse to be tired”(P11).
Directors of nursing performance
Participants referred the behavior of nursing directors as a source of tension. Terms such as the following were used by the participants in abundance (in relation to nursing managers): “ingratitude and poor magnitude,” “incorrect attitude,” “condemning all the situations,” and “unfair punishment.” One participant about the stressful behavior of the authorities said: “Once, I went to pray the Morning Prayer. The supervisor came and saw that I was not there and reported me that I was sleeping. When I protested…they told me that it is not possible to do anything”(P3). Another nurse, referring the nursing officials’ ingratitude said: “A patient recently came from the emergency room to the CCU. Upon his arrival, the arrest and CPR were happened…I did my best and the patient returned to normal condition. (On this situation), I was forgotten to write his name above his bed. The supervisor reported me…”(P5). Some participants mentioned that many of the behaviors of the directors are not just “supporting” but are “spirit destructive” for nurses. Some participants also noted that the managers maintain their authority by using the following cases: “making gap,” “insincerity,” “permanently complained,” and “creating stress in their subordinates.” One nurse said: “the directors maintain their authorities by making a series of tensions. For that reason, there is no intimacy in the high-ranking officials”(P2).
Undesirable relations among colleagues
Undesirable relations between the staff were among the stressors which the participants have mentioned. One participant said: “If we have contact with our co-workers, the work will be harder for us to perform. For example, before I came to this section, a fellow had gone and was told that this person is not suitable for our area…but I did not notice and ignored it…”(P4). Lack of cooperation and intimacy between the staff will lead to increased occupational stress. A nurse pointed to this issue that lack of intimacy between the female partners is more common: “Working in the female sections which constantly make problems for each other, is very difficult”(P10). The stress related to the partner is not always relevant to intimacy. But, it is sometimes due to the inadequate scientific and technical knowledge of the partners and sometimes is related to the stress and anxiety which is transferred to another colleague. One nurse said: “When a colleague is stressed. Inevitably, it will be transferred to you. Or when a novice is placed in your shift (that she does not know her duties)…you should work instead of her too”(P6).
The patients’ conditions
Based on the experience of the participants, the lack of congruence between the patient and nurse, the number of critically ill patients, and working with high-risk patients are some other stress factors relating to the condition of the patients. One participant said: “One night…I was alone in the ward. Suddenly, one of the male patients had been ill and had fallen in the bathroom. Now, a woman alone, think that how much stress I felt and how I got out the patient out of the bathroom”(P2). Participants also mentioned about the stressful items such as “mistrust of the patients and their relatives and arguing with them,” “tolerating abuse and insult,” and “ingratitude of some of the patients and their families.” One nurse said: “Once, we had a patient with SK (streptokinase) and a hematoma was formed in the stomach…we really worked for him…but as the patient’s friend saw the bad condition, he had grabbed a chair and threw it towards us”(P6).
Professional interest
In addition to the occupational stress factors, the participants understood that the interest in their profession can act as a stress reducer. They believed that the professional interest has a large effect on the perception of occupational stress and ways of dealing with it. Participants could be divided into two groups of interested and uninterested. However, some of them were noted that the professional interest is required for further work. One nurse said: “If there is no love in our profession, one can not continue”(P6). The participants have reported that some factors were the cause of their interest in nursing including “rising medical information,” “ability to identify and solve health problems in the family,” “improvement of patient satisfaction,” and “spiritual reward.” One of them said: “The spiritual side of the job worth very much for me, and because the public information increases and it will be possible to answer every persons’ questions, mostly with no wrong answer. So I love the nursing”(P4). Although the interest in the profession reduced the stress perceived by the participants, when there was a lack of interest, the intensity of perceived stress were added. “Labore of work” and “facing with the injustice in the system” were the other stress factors which affected some of the nurses. One of the participants said: “I am satisfied with the job of nursing… especially its spiritual aspect and the importance of our work. But there are a series of side issues (such as injustice), that they are causing discontent” (P1).
Prioritizing career over family life
According to the participants’ beliefs, the stressors of nursing profession affect all aspects of the nurses’ living. “Prioritizing career over family life due to the business requirements” and “impaired personal life” were issues that were creating stress for most of the participants. A participant regarding the priority of career on family life said: “Being in a rotating shift makes you not to be able to plan properly for your family”(P13). Another nurse said: “One of the major stresses which affects on my family is when my husband asks to do something or there is a family celebration and due to my shift work requirements, I can not do or go”(P14). Participants believed that the occupational stress has affected their body and mind. They mentioned about factors such as chronic fatigue, aggression, impatience, irritability, isolation, and depression as some concequences of job stress. One participant said: “When I get home from the work, I’m tired and bored. Even I am not able to get a simple greet with my husband”(P3). Another participant said: “When you go home after a shift full of intensive work, just you need to sleep. While you are cooking the food, you sleep and it will burn your food…”(P4). Pressures and job requirements not only were the cause of not observing their agenda and family programs, but sometimes they are denied to perform their personal interests and entertainment. Some of these participants remembered these conditions with the words of “removing yourself from your life.” One nurse said: “I like music and sports. But it does not remain any opportunities for me to get my favorite. In total I have removed and left myself aside”(P7). Another nurse regarding the lack of opportunity to address her personal interests said: “Since I have come to work, I had no time to exercise and no power and energy for exercising. I have knee and shoulder pain…”(P20).
DISCUSSION
This study aimed to investigate the nurses’ experiences and perceptions regarding the occupational stress. Experiences and perceptions of participants have been placed in three main categories: “nurses’ perceptions of occupational stress,” “professional interest,” and “prioritizing career over family life.” The first category had several subsets that in overall, they were the most important professional stressors for the nurses of this study. The nurses felt to be in a constant alarm situation. The severe and unpredictable changes in patient status were among the most stressful experiences that the participants faced with. Excessive workload and workplace bitter events had added the intensity of this stress. These findings are consistent with the reports of Aoki et al.[17] and Seyedfatemi et al.[18] Jonsson et al. have also reported that continuous job stress not only endanger the quality of the services, but also the health of the healthcare providers. It can cause the symptoms of stress syndrome.[19] Based on the participants’ experiences, the following items were some of the stress factors for the nurses: lack of experience, poor social status, lack of proper logistics, nurse shortages, irregularities in the organization, managers’ poor performance, colleagues’ poor relations, and patients’ conditions. These findings are consistent with the reports of Adib-Hajbaghery.[6,20] Stora[8] and Ratner and Sawatzky[21] have reported that the nurses faced with multiple occupational risk factors. Some studies which have been conducted in Iran mentioned about the sources of stress for nurses such as patient care, inappropriate treatment of the patient’s family, increasing workload, dissatisfaction with the wages, work on holidays, not having enough sleep and rest, lack of social acceptance, work environment, contact with contaminated objects, and lack of access to physician in emergency situations.[22–26] A number of studies in other countries as well have reached to similar findings.[27–29] The most important factors creating stress which were mentioned by the participants of the present study have been referred to the organization management. Factors such as lack of proper logistics, nurse shortages, irregularities in the organization, and poor management performance showed that if the senior management ranks perform their responsibilities (in terms of supplies needed to provide the quality care), it will largely reduce the pressure and stress imposed on nurses. The nurses should also try with the development of good relations between themselves to reduce the occupational stress.
According to the participants, the professional interest will affect the level of perceived stress and the ways of dealing with stress. Factors such as “rising the medical information,” “ability to identify and solve health problems in the family,” “satisfaction from the patient improvement,” and “spiritual reward” have contributed to the professional interest. However, “labore of work” and “facing with the injustice in the system” will result dissatisfaction. Rahimi et al. have reported that with increasing the stress, the job satisfaction of nurses’ decreases.[30] Cottrell,[31] Cavalheiro et al.,[32] and Ho et al.[33] mentioned that as well as professional interest has the impact on job satisfaction, lack of interest will cause job dissatisfaction.
One of the most important sources of occupational stress for the nurses in this research was the priority of work on their family and personal life. Aggression, impatience, irritability, and limited family connections were the symptoms which the participants had experienced. This category of the findings was relatively new which the study found. None of the previous studies paid attention directly to the stressors associated with nursing and their relationship with nurses’ family. However, in some of them they have mentioned about the existing problems in the nurses’ families. Khaghanizadeh et al. have reported about an imbalance between work and life of the military nurses.[34] Yaghoobian and Parhizgar[35] and Abdi and Shahbazi[36] have reported from the foreign researchers that divorce and family disputes are more in occupations such as nursing (which has shift works or have a high workload). A number of researchers have reported that integration of the family of nurses (with evening shift work and school-age children) has been disrupted.[37–39]
The job stressors on nursing job were already examined in some quantitative studies. But few studies have been conducted to investigate the life experiences of nurses. In one of the few studies in this area, YazdanPanah and Dianat used focused group discussions to investigate the environmental stressors of nursing. However, he primarily investigated the nurses’ views, not their life experiences.[1] Adib-Hajbagheri et al.,[5] Dehghan-Nayeri et al.[7] and Adib-Hajbaghery[6] have also studied the affecting factors on decision-making, care practices, and nurses’ productivity with qualitative methods. They have mentioned some of the stressors affecting their performance, but not directly the stressors of their career. For the first time in Iran, and as one of the few qualitative studies, the present study has focused on this issues and showed that the nurses not only are facing with multiple job stressors, but their private and family life is affected with these factors.
CONCLUSION
The present study indicated that there are many stressors in the nursing profession. The most important items among these cases can be noted as follows: the shortage of nurses, the adverse authorities, developing critical and unpredictable situations, disharmony, and poor social status. According to the research findings, the job stressors influence the private and family life of the nurses. According to these findings, the attention of the hospital authorities for the required action should seek to reduce the occupational stress. This can help to reduce the job stress to a large extent. Avoiding frequent handling without the consent of the nurses and improving the relations between the ranks of management and the nurses can be offered. Some actions also seem to be nessesary in order to improve the social status of nursing profession in the society and media. The study results suggest that a qualitative study to be done for investigating the nurses’ family problems and disorders of their personal life. It also recommended a study to identify practical solutions to reduce the nurses’ occupational stress. In the end, it should be noted that the low number of samples in this study may limit the generalization of the results. Of course, this is considered as the inherent limitations of the qualitative studies.
Footnotes
Source of Support: Kashan University of Medical Sciences
Conflict of Interest: Nil.
REFERENCES
- 1.YazdanPanah S, Dianat M. A survey on work-related stressors in nursing and methods of their reduction: A focus group discussion. Iran South Med J. 2004;6:178–2. [Google Scholar]
- 2.Ghacemi A, Attar M. Evaluation of stressful factors in nurses of Babol, Sari and Behshahr hospitals. 2006. [Last accessed on 2011 Nov 24]. Available from: http://www.betsa.ir .
- 3.Farhadiyan M. Evaluation of occupational stress and occupational satisfaction in nurses of Intensive care units in Tehran University of Medical Sciences. Tehran: Tehran University of Medical Sciences; 1996. [Google Scholar]
- 4.Cole D, Nelson L. Stress at work: The relationship between hope and health in hospital nurse. Psychosoc Nurs. 2001;26:7–18. doi: 10.1097/00004010-200110000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Adib-Hajbagheri M, Salsali M, Ahmadi F. Clinical Decision-Making: A way to professional empowerment in nursing. Iran J Med Educ. 2003;3:3–13. [Google Scholar]
- 6.Adib-Hajbaghery M. Factors facilitating and inhibiting evidence-based nursing in Iran. J Adv Nurs. 2007;58:566–75. doi: 10.1111/j.1365-2648.2007.04253.x. [DOI] [PubMed] [Google Scholar]
- 7.Dehghan-nayeri N, Nazari A, Salsali M, Ahmadi F. To assess role of staffing in nursing productivity: A qualitative research. Hayat. 2006;12:5–15. [Google Scholar]
- 8.Stora JB. In: Stress. Dadcetan P, translator. Tehran: Islamic Ershad Publications; 1998. pp. 73–4. [Google Scholar]
- 9.Navidian A, Masoudi G, Mousavi SS. Work-related Stress and the General Health of Nursing Staffs in Zahedans’ Hospitals Emergency Wards (2004) Behbood, The Scientific Quarterly. 2005;9(26):17–26. [Google Scholar]
- 10.Salmaani Barough N, Taghavi Larijani T, Monjamed Z, Sharifi N, Bahrani N. Coping with stress. Hayat. 2005;10:21–7. [Google Scholar]
- 11.Haghighat SH. Evaluation of occupational stress in employees of Kashan Shahid Beheshti hospital. Kashan University of Medical Sciences; 2005. [Google Scholar]
- 12.Polit DF, Beck CT. Nursing_Research Principles and Methods. 7th ed. Philadelphia: Lippincott, Williams and Wilkins; 2004. [Google Scholar]
- 13.Krippendorff K. Content analysis: An introduction to its methodology. 2nd ed. Thousand Oaks: Sage Publications; 2004. [Google Scholar]
- 14.Garson D. Content analysis and qualitative research. [Last accessed on 2010 Jun 08]. Available from: http://www.faculty.chass.ncsu.edu/garson/PA765/content.htm .
- 15.Hodgins D. Father involvement in parenting young children: A content analysis of parent education programs in BC. University of Victoria: 2007. [Last accessed on 2010 Jun 08]. pp. 42–60. Available from: http://www.faculty.chass.ncsu.edu/garson/PA765/content.htm . [Google Scholar]
- 16.Adib-Hajbaghery M. Grounded theory research method. Tehran: Boshra Publications; 2006. [Google Scholar]
- 17.Aoki M, Keiwkarnka B, Chompikul J. Job stress among nurses in public hospitals in Ratchaburi province, Thailand. J Pub Health Dev. 2011;9:19–27. [Google Scholar]
- 18.Seyedfatemi N, Tafreshi M, Hagani H. Experienced stressors and coping strategies among Iranian nursing students. BMC Nurs. 2007;6:11. doi: 10.1186/1472-6955-6-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jonsson A, Segesten K, Mattsson B. Post-traumatic stress among Swedish ambulance personnel. Emerg Med J. 2003;20:79–84. doi: 10.1136/emj.20.1.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Adib Hajbaghery M, Salsali M, Ahmadi F. The factors facilitating and inhibiting effective clinical decision-making in nursing: A qualitative study. BMC Nurs. 2004;3:2. doi: 10.1186/1472-6955-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ratner PA, Sawatzky R. Health status, preventive behavior and risk factors among female nurses. Health Rep. 2009;20:53–61. [PubMed] [Google Scholar]
- 22.Khodayar F. Congress of nursing theories. Tabriz, Iran: Tabriz University of Medical Sciences; 1994. Evaluation of stress in nurses of Intensive care units. [Google Scholar]
- 23.Molazem Z, Mohammad Hosseini S, Karimi Z, Zadeh Bagheri Gh. A study on job stress-making factors and their degrees of stressfulness from the nurses› viewpoint in the university hospitals of Kohgiluyeh and Boyerahmad. Armaghene-Danesh. 2005;10:103–95. [Google Scholar]
- 24.Labbaf Quassemi F, Marbaghi A, Kabiri FG, Hosseini F. Assessment of work Experiences of the temporary employed nurses within the program of human research project. Iran J Nurs. 2005;18:7–19. [Google Scholar]
- 25.Fathi M. Incidence rate and sources of stress among nurses working in intensive care unit of Kurdistan University of Medical Sciences. Scientific J Kurdistan Univ Med Sci. 2003;7:53–62. [Google Scholar]
- 26.Kaheni S, Farajzadeh Z, Saadatjoo AR, Nasiri Fourg A, Avan M. Job Stress, Stress Signs and Methods of Coping with Stress by Employed Nurses in Birjand University of Medical Sciences 2007. Dena, Q J Yasuj Fac Nurs Midwifery. 2008;2:37–46. [Google Scholar]
- 27.Chen WC, Hwu HG, Kung SM, Chiu HJ, Wang JD. Prevalence and determinants of workplace violence of health care workers in a psychiatric hospital in Taiwan. J Occup Health. 2008;50:288–93. doi: 10.1539/joh.l7132. [DOI] [PubMed] [Google Scholar]
- 28.Tyson PD, Pangruengphant R. Five year fallow-up Study at Stress among nurses in public and private hospitals in Thailand. Int J Nurs Stud. 2004;41:24754. doi: 10.1016/S0020-7489(03)00134-2. [DOI] [PubMed] [Google Scholar]
- 29.Arfa MA, Nazel MW. Predictors of psychological well being of nurses in Alexanderi, Egypt. Int J Nurs. 2003;9:313–20. doi: 10.1046/j.1440-172x.2003.00437.x. [DOI] [PubMed] [Google Scholar]
- 30.Rahimi A, Ahmadi F, Akhond MR. An investigation of amount and factors affecting nurses› job stress in some hospitals in Tehran. Hayat. 2004;10:13–22. [Google Scholar]
- 31.Cottrell S. Occupational stress and job satisfaction in mental health nursing: focused interventions through evidence-based assessment. J Psychiatr Ment Health Nurs. 2001;8:157–64. doi: 10.1046/j.1365-2850.2001.00373.x. [DOI] [PubMed] [Google Scholar]
- 32.Cavalheiro AM, Moura DF, Junior, Lopes AC. Stress in nurses working in intensive care units. Rev Lat Am Enfermagem. 2008;16:29–35. doi: 10.1590/s0104-11692008000100005. [DOI] [PubMed] [Google Scholar]
- 33.Ho WH, Chang CS, Shih YL, Liang RD. Effects of Job Rotation and Role Stress among Nurses on Job Satisfaction and Organizational Commitment. BMC Health Serv Res. 2009;9:8. doi: 10.1186/1472-6963-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Khghanizadeh M, Ebadi A, Siratinayyer M, Rahmani M. The study of relationship between job stress and quality of work life of nurses in military hospitals. J Military Med. 2008;10:175–84. [Google Scholar]
- 35.Yaghoobian M, Parhizgar S. A study on job stress among nurses working in hospitals in eastern Mazandaran province in 1999. Armaghene-Danesh. 2002;7:20–13. [Google Scholar]
- 36.Abdi H, Shahbazi L. Correlation between occupational stress in nurses at intensive care unit with job burnout. J Shahid Sadoughi Univ Med Sci. 2001;9:63–58. [Google Scholar]
- 37.Bullock HE, Waugh IM. Care-giving around the Clock: How Women in Nursing Manage Career and Family Demands. J Soc Issues. 2004;60:767–86. [Google Scholar]
- 38.Barnett RC, Gareis K, Brennan R. Wives› Shift Work Schedules and Husbands› and Wives› Well-Being in Dual-Earner Couples with Children: A Within-Couple Analysis. J Fam Issues. 2008;29:396–422. [Google Scholar]
- 39.Grzywacz JG, Frone MR, Brewer CS, Kovner CT. Quantifying work-family conflict among registered nurses. Res Nurs Health. 2006;29:414–26. doi: 10.1002/nur.20133. [DOI] [PubMed] [Google Scholar]


