Abstract
Background:
According to transtheoretical model (TTM), Stage matched interventions are more effective in quitting. The objective of current study was to investigate the effect of individual counseling, line follow-up, and free nicotine replacement therapy (NRT) on smoking cessation in smokers who are in preparation stage of smoking.
Materials and Methods:
In a randomized clinical trial design, through sending the short message system, potential participants in preparation stage of smoking were recruited and divided into control (n = 60)and treatment (n = 50) groups. The treatment group received an in-person counseling, line follow-up, and free NRT. TTM variables trend; pros and cons of smoking, behavioral and experiential processes, temptation, were assessed at baseline, 3 and 6 months follow-up along with point prevalence and continuous abstinence.
Results:
Continuous abstinence at 6-month follow-up were 3.3% (n = 2) in control group and 46% (n = 23) in the treatment group (x2 = 34.041, P < 0.001). Time Χ group analyses indicated that except cons of smoking (P > 0.05), all TTM constructs had significantly changed; temptation (F = 36.864, P < 0.001), pros (F = 12.172, P < 0.001), experiential processes (F = 3.377, P < 0.001), and behavioral processes (F = 11.131, P < 0.001).
Conclusion:
Interventions based on TTM variables increased the quite rate in prepared and motivated people. Our findings suggest that interventions through individual counseling along with free NRT and line follow-up in people who prepare for quitting are beneficial for our country.
Keywords: Counseling, experiential and behavioral processes, line follow-up, nicotine replacement therapy, pros and cons, quite rate, self-efficacy, smoking cessation intervention
INTRODUCTION
According to the WHO reports; 14.2% from 15 to 64-years-old Iran's population are smokers.[1] The Iranian Health Ministry statistics show that cigarette consumption in Iran is growing. In 2003, 12% of teen 13-15-years-old were smokers, that figure has reached 27% in 2007.[2,3] Meanwhile, about 70% of smokers want to quit smoking, and few of them are about 5% who receive no help to be succeeded in quitting.[4,5] Results of a survey conducted in our country showed that only 2.4% have managed to quit smoking.[6]
Transtheorethical Model (TTM) is one of the models in the early 1980s, which was introduced by Prochaska and decremented for smoking quit.[7] TTM is one of the stage-based theories and proposes that behavior change is not a continuous process but can occur through a series of qualitatively different stages. These models, consequently, suggest that interventions will be most effective when they are tailored to individual's current stage of change. According to these models, three broad categories of individuals distinguished:[1] People who have not yet decided to change their behavior,[2] people who have decided to change, and (three people who are already engaged in overt change.[8] The TTM proposes that “tailored” interventions, which are taken in to account of current stage and the individual has reached in the change process, will be more effective than “one size fits all” interventions.[8] Results of several studies have shown the stage-based interventions by using different strategies to increase the smoking cessation rate.[9,10,11,12]
On the basis of TTM, five different stages of smoking behaviors are: (a) Precontemplation (individuals who are smokers and not intending to quit smoking in the next 6 months), (b) Contemplation (individuals who are smokers but they try to quitin the next 6 months), (c) Preparation (individuals who are smokers but they have plan to quit smoking in the next 30 days), (d) Action (individuals who actually quit smoking and been abstinent for less than 6 months), and (e) Maintenance (individuals have quit smoking and they get abstinent for more than 6 months after initial quitting).[5] The first three stages are motivational, whilst the latter two stages are actionable in nature. Progression through the stages is seen as sequential, though relapse to an earlier stage can occur.[8,13] The time of occurrence changes depends on decisional balance and self-efficacy, which are considered as two intermediate indicators.[14] They also explain behavior change strategies through 10 processes of change that are divided into two categories: Experiential process (consciousness raising, dramatic relief, environmental re-evaluation, social liberation, and self-re-evaluation) and behavioral (Self-liberation, stimulus control, helping relation, counter conditioning, and reinforcement management.[15]
Decisional balance is defined as the potential benefits (Pros) and costs (Cons) of behavior change.[16] In moving toward any decision, individuals weigh the costs and benefits of the action being contemplated. In change of behavior, these considerations are known as decisional balance, a process of cognitively appraising or evaluating the “good” aspects or pros, the “less good” aspects or cons of a behavior, the reasons to change and not to change that behavior. Lasting behavior change is associated with the pros for the behavior change increasing and the cons for change decreasing until the point of crossing over is reached.[17]
The concept of self-efficacy is a component of Bandura's social learning theory defined as one's perceived confidence in the ability to perform a specific behavior.[18] In smoking behavior; self-efficacy represents the subjects’ level of confidence that they can resist smoking across a number of tempting situations.[19] Self-confidence to resist against smoking temptations has tended to decrease among precontemplators and get much higher as the smoker acts and maintain abstinence.[20]
The first step in quitting is having preparation and motivation for quitting.[21] Besides motivation and readiness, successful smoking cessation is impressed by nicotine dependence. Avoiding the withdrawal symptoms to nicotine abstinence is a strong stimulator to continue smoking.[22] In one hand, nicotine replacement therapy (NRT) is an effective way to overcome the physiological withdrawal symptoms because it ameliorates affects and can double smoking cessation rate.[23,24] On the other hand, studies have shown that telephone follow-up in both reactive and proactive forms are effective in stopping smoking.[25,26]
There is no functional comprehensive policy to control smoking in Iran and in this area only one research center in Tehran is active. Because the smokers who are in the preparation stage committing to and planning for imminent change, we focused our interventions in this group. Hence, the aim of the current study was to examination of individualized counseling, line follow-up, and nicotine replacement on smoking cessation based on TTM constructs.
MATERIALS AND METHODS
Design
Participants were people in preparation stage of smoking behavior. The inclusion criteria were having readiness to quit; age range were between 12 and 80-years-old; not being pregnant; and not suffering from MI or CVA (Myocardial Infarction or cerebra Vascular Accident) in the last 3 weeks. There is no limitation for exclusion criteria.
The research design was a randomized clinical trial with a control group. Considering 95% confident coefficient andtest power 80%, the sample size was calculated on 46 people in both treatment andcontrol groups using this formula:
P was the mean success quit rate in both treatment and control group and calculated by:
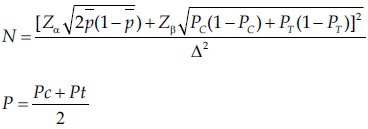
Pc was the mean success quit rate in control group and Pt was the mean success quit rate considered 0.33 according to Erol and Erdogan`s study.[27] Due to the potentially dropping rate, we added 10% for both of them, and we included 52 people in both groups. For matching purpose, we added eight people in the control group. Then, the participants randomly allocated into treatment or control groups. However, in the follow-up process, two people of the treatment group were dropped from study.
Setting
The study population was all smokers in Gorgan in Golestan province, northern of Iran.
Study population characteristics
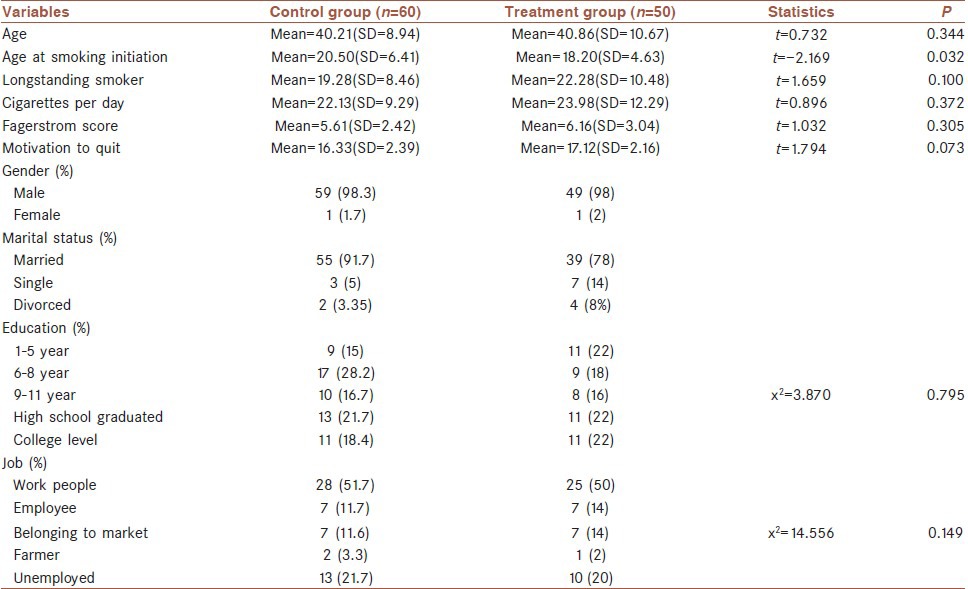
Demographic profile of the participants (both control and treatment group) were shown in Table 1. Of the 110 people, 60 were in control group and 50 in the treatment group. The participants’ ages ranged between 24 and 65 years, with a mean age of 40.50 (SD = 9.72) years. Majority of them (87.3%) were married, 98.2% were male, who smoked an average of 22.97 (SD = 10.74) cigarettes per day with median length of smoking was 20.64 (SD = 9.51) years. They had 4.89 (SD = 15.61), 24h quit attempts in last year. One-fifth had college level and 21.8% had high school graduated, and remainders educated 1-11 years. Slightly over half (51.3%) of the sample were workpeople, 12.4% belonged to the market, 11.8% were employee, 2.7% farmer, and rest of them (21.8%) were unemployed people. The mean score for nicotine dependence by means of fagerstrom test for nicotine dependence (FTND) was 5.86 (SD = 2.75) and their e mean score for motivation was 16.69 (SD = 2.31).
Table 1.
Demographic characteristics of participants
Measures
In order to identify smoking behavior, stage of smoking behavior was assessed using 5-item, Dichotomous Scale (yes/no), related to current smoking behavior and intention to quit smoking, used by Diclemente et al.[28] The decisional balance was assessed by six-item short form questionnaire designed Velicer et al.[29] Participants ratings were made on a 5-point Likert Scale, rating from “not important” to” extremely important”. The reliability assessed by internal consistency with Cronbach's alpha was acceptable (α = 0.87).
The self-efficacy Scale to avoid smoking temptation was assessed by Velicer et al.[30] short form questionnaires containing nine items and assessed participants’ perceptions of their ability to refrain from smoking in various situations. Participant's ratings were made on a 5-point Likert Scale, rating from “not all tempted” to “extremely tempted”. The self-efficacy has shown acceptable psychometric properties with Chronbach's alpha = 0.62.
The Persian versions of the stages of change, self-efficacy and decisional balance scales were assessed for validity and reliability by using Banville's method and described in elsewhere.[31] Nicotine dependency was assessed by FTND.[32] The FTND reliability was acceptable by using Chronbach's alpha = 0.71.
Motivation to cessation was evaluated by using motivational test.[33] This test was applied in Persian, by Heydari.[34] The test included one question related to the current quitting importance and another one to the individual decision about giving-up. These two questions were made on a 4-point Likert Scale, rating from “not important” to “extremely important”. The third question associated with the reasons for cessation, six reasons. The last question is to ask about cessation fore sighting, rating by 6-point Likert Scale, from “extremely successful” to “very little successful”. The range of total score was four to 20. The subjects were divided into three motivation subgroups including low,[4,5,6,7,8,9] moderate,[10,11,12,13,14,15] and high.[16,17,18,19,20]
Procedure
In order to reach on potential respondents we sent the message through the short message system (SMS) of cell phone for 40,000 cell phone numbers in three periods of time, separately. These phone numbers were selected from 350,000 numbers by a private firm which activates numerous SMS. Meanwhile, 100,000 of the advertising materials in A4 size were distributed in all part of the city. The contents of the two methods were free in cost calls to smoking-cessation program that it was recruiting for quitting intervention. The respondents were asked to respond to the questions in their own privacy and were guaranteed of their responses.
To get the quitting rate, we used the self-reported “point prevalence abstinence” in 3-and 6 months follow-ups from baseline; not one puff of smoke during the past 7 days for preparation stage. The continuous abstinence for the maintenance stage was defined as not one puff of smoke during the past 6 months.[35]
The procedures were approved by the Isfahan University of Medical Sciences Institutional Review Board and registered in Iranian Register of Clinical Trials (IRCT201011025074N1). Meanwhile, the procedure followed the ethical principles outlined in the 1975 Helsinki Declaration. Prior to the study, all the participants provided written, informed consent.
Interventions
Five sessions of personal counselling, that will take about 45 min. Using free nicotine chewing gum for 2 months along with phone line follow-up, including 2 times in the 1st week with the nicotine chewing gum use. Then, continued once in a week for 3 months, and finally quarterly until the end of the 6th month.
Two milligrams of nicotine chewing gum were used based on subject's nicotine dependency for 2 months, five consulting sessions along with one booklet. The using dose of chewing nicotine gum was the basis on the subject's nicotine dependency according to Fagerstrom test that divided into three groups: Low dependency group (score 0-3), middle dependency (score 4-6), high dependency.[8,9,10] Low, middle, and high depended people of the treatment group received the maximum daily gums by 6, 9, and 12 gums, respectively. For all three groups’ nicotine chewing gum doses were tapered 2 gums biweekly. Counseling sessions were included preparation for cessation and the exact quit date, nicotine withdrawal symptoms and how to deal with them, tempting situations and their control, stress and its management, weight control and nutrition after quitting. All of these were placed in a booklet and submitted for them. A participant in the control group did not receive any drug or intervention except for recommendations for cessation.
Analysis
Data were analyzed using SPSS version 15.0. Descriptive statistics were used to demographic variables and quite rate. Normal distribution was confirmed by the Kolmogorov–Smirnov test for continuous variables. In analyses with TTM variables as the outcome, repeated measure analysis was conducted for deviations over the time (baseline, 3 and 6 months follow-up) and two factors (time × group) repeated measures analysis of variance was performed to examine the effects of group (treatment, control) and time (baseline, 3 and 6 months follow-up) on each dependent variable. ANCOVA and Chi-square were tested for group differences. Due to Mouchly`s test, sphericity assumption was not satisfied, except in cons of smoking, we used Greenhouse-Geisser for adjusting degree of freedom. ANCOVA and Chi-square were tested for group differences. Independent samples t-test were calculated for TTM variables difference between quitters and smokers. The Paired-Samples t-test was computed the differences between values of the TTM variables for each group, whether the average differs from baseline. P value of less than 0.05 was considered statistically significant.
RESULTS
Abstinence rate
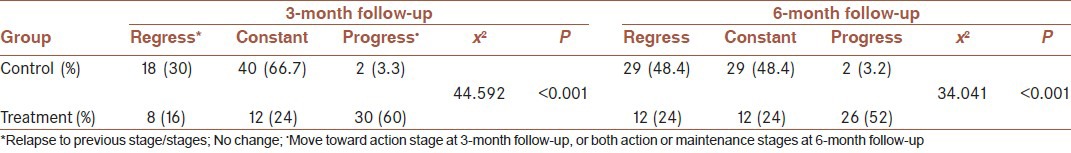
Past-week abstinence from smoking was different in control and treatment group. This amount at 3-month follow-up was 10% in control group and 64% in the treatment group (x2 = 34.114, P < 0.001). At 6-month follow-up, it was 13.3% in control and 60% in treatment (x2 = 32.021, P < 0.001). Based on self-report point prevalence abstinence the result indicated that in 3-month follow-up just 2 (3.3%) people were in action stage in control group but, this rate was 30 (60%) for people in treatment group (x2 = 44.592, P < 0.001). In 6-month follow-up the point prevalence for control group was constant 2 (3.3%) but for treatment group was 26 (52%) (x2 = 33.881, P < 0.001). The continuous abstinence based on transtheoretical model stage of change on the cut-off for the maintenance stage (183 days) was 23 (46%) (x2 = 34.041, P < 0.001)for treatment group and none for the control group. The progression and regression of the participants in two groups on the 3 and 6-month follow-up, reported in Table 2. At 6-month follow-up, the total regression rate was 29 (48.4%) in control people and 12 (24%) in treatment people.
Table 2.
Regress, constant, and progress in 3 and 6-month follow-up
Transtheorethical model constructs
According to repeated measure analysis of variance (RM-ANOVA) the results of study in line of TTM variables indicated that in treatment group at 6-months follow-up, all constructs had significant differences with baseline except cons of smoking. But in control group at 6-month follow-up, these variables were not significantly different with baseline [Table 3]. Figure 1a, shows that in treatment subjects’ temptation to smoking decreased significantly 3 and 6 months after interventions, F (1,50) = 30.215, P < 0.001, η2 = 0.44, pros of smoking decreased significantly in the treatment group over time but no significant deviation in control group, F (1,413) = 18.601, P < 0.001, η2 = 0.37, [Figure 1b]. In line with cons of smoking, both two groups were not having any differences in baseline and over the time (P > 0.05) [Figure 1c]. Further, treatment people were used significantly from behavioral process, F (1,359) = 9.239, P < 0.001, η2 = 0.21, than experiential process, F (1,687) = 5.890, P < 0.001, η2 = 0.26, [Figure 1d and e].
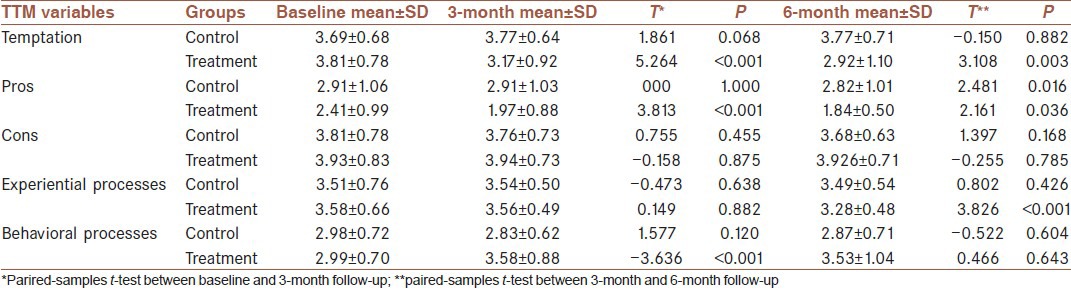
Table 3.
Deviation of transtheorethical model variables according to repeated measure analysis of variance in control and treatment group
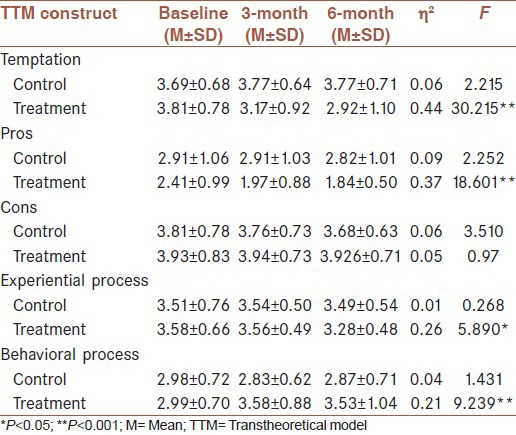
Figure 1.
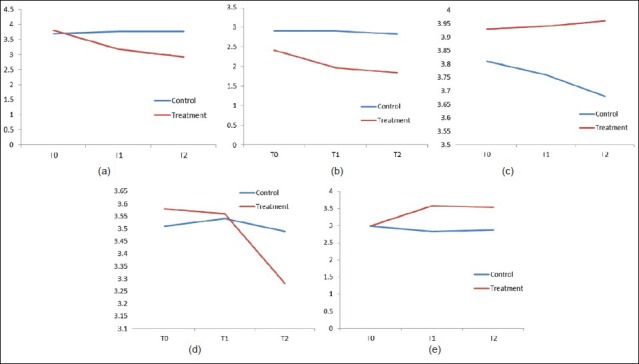
Transtheorethical model variables deviations over the time. (a) Temptation trends over the time, (b) Pros trends over the time, (c) Cons trends over the time, (d) Experiential process trends over the time, (e) Behavioral process trends over the time
Tests of repeated measure analysis of variance related to time × groups indicated that except cons of smoking (P > 0.05), all TTM constructs had significantly changes; temptation, (F (1,562) = 36.864, P < 0.001, η2 = 0.23, pros F (1,473) = 12.172, P < 0.001, η2 = 0.12, cognitive processes, F (1,797) = 3.377, P < 0.001, η2 = 0.05, and behavioral processes F (1,474) = 11.131, P < 0.001, η2 = 0.13, [Table 4]. The paired-samples t-test results showed that in control groups there was no differences within the control group except in pros of smoking in 3 month and 6month follow-up (t = 2.481, P < 0.05). Within treatment group there were no significant differences in experiential processes between baseline and 3-month follow-up, as well as in behavioral processes between 3 month and 6 month follow-up (P > 0.05). However, the cons of smoking change was not significant in both groups [Table 5].
Table 4.
Repeated measure analyses of variance (group, time, and time×group) for transtheoretical model variable

Table 5.
Paired-samples t-test within groups for transtheorethical model constructs
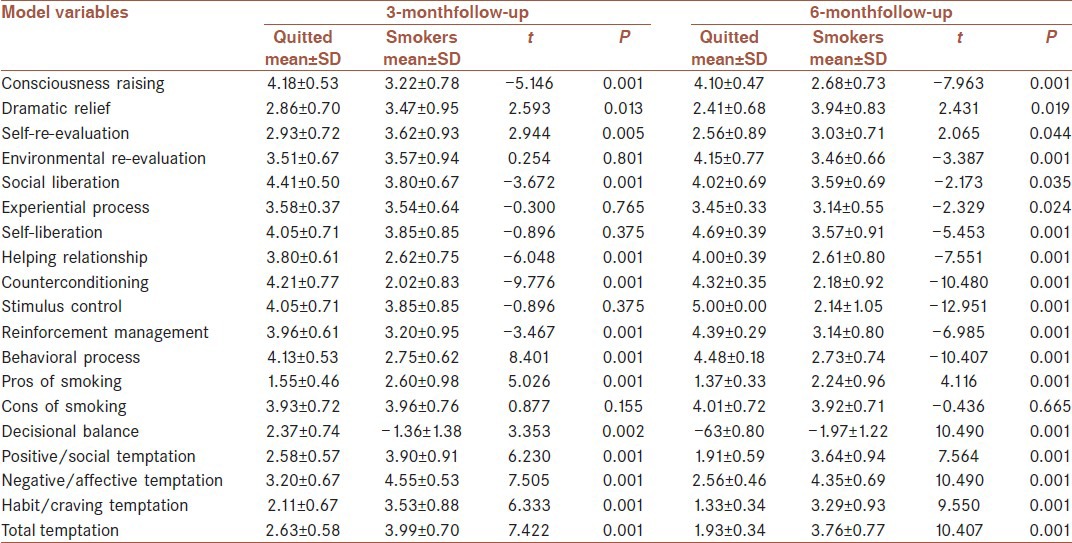
Independent samples t-test were calculated between succeed in quitting and those who were till smoking on the TTM constructs for 3 and 6 month follow-up within treatment group and showed some differences [Table 6]. In total, Quitted had higher scores on the behavioral process in both 3 and 6 months follow-up (t = −8.401, P < 0.001 and t = −10.407, P < 0.001). But, higher scores on experiential process only at 6-month follow-up (t = −2.329, P < 0.05). Further, they had perceived lower pros of smoking over the time (t = 5.026, P < 0.001 and 4.116, P < 0.001). There were no differences between smokers and nonsmokers in cons of smoking in 3-month (t = 0.877, P = 0.155) and 6-month (−0.436, P = 0.665). Temptation to smoking was lower in the quitted people than in smokers (t = 7.422, P < 0.001and t = 10.407, P < 0.001).
Table 6.
Transtheorethical model variables differences between quitted and smokers at 3 and 6 months follow-up
There were no differences between quitted people and smokers in FTND scores, quit attempt in past year, number of cigarettes daily consumed, education level, job profile, and marital status both at 3 and 6 months follow-up.
DISCUSSION
To our knowledge, this study was the first work that included all TTM variables in smoking cessation. The result indicated that the continuous abstinence rate based on the maintenance stage was 46% in the treatment group. This finding emphasis on the role of tailored intervention, individual counseling, and NRT as well as. According to TTM, stage matched intervention increase the abstinence rate in smokers, especially who were in preparation stage.[8] Because the individual in preparation stage motivated to quitting, their success in quitting could be enhanced by NRT, line follow-up, and in person counseling. Nicotine is addictive material that could be influenced any successful quitting by its withdrawal symptoms. Hence, including NRT for overcoming on psychological and physiological symptoms is very important issue. Several studies have shown that nicotine dependency role in the success or failure of smoking cessation and that using NRT, especially in people with high nicotine dependence in the first few weeks of smoking cessation has a great impact.[36,37] In the meantime, the offering of free NRT should be considered because the economic barrier to NRT is one of the barrier that can alter the quit attempts and decrease the motivation for cessation. Alberg et al.[38] reported that free transdermal nicotine patches provision increased quit rate from 38% to 56%. Meanwhile, referred to smoking cessation in a period of 18-month increased by 37%.
The study conducted by Nohlert and colleagues showed that the success rate of continues abstinence rate in the group that had received high-intensity counseling twice the depth of a group that had received only short-term counseling.[39] Besides, phone calls follow-ups and in-person counseling provide the social support for smoking abstinence. Some studies have shown that providing telephone counseling can cause to help quit smoking. McAlister et al.[40] study's estimated that telephone counseling services had about 8% more quit rate than self-help group and was 1 year cost-effective in smoking cessation. Another study results showed the effectiveness of quit lines as auxiliary method, if it is to be used along with health care system.[25] Heydari et al.[41] study on efficacy of telephone quit-line for smokers in Iran showed the sustained abstinence rate after 1, 3, 6 and 12 months was 59%, 41%, 31% and 18%; respectively. However, our proactive calling provided access to counseling and was helpful in quit processing.
We did found a considerable effect size related to TTM variables in treatment group at two follow-up measurements. These results confirmed the role of behavioral counseling, social support and NRT to succeed quitting rate.
The current study showed that non-smokers use more behavioral process and some cognitive process like consciousness raising, social liberation, and environmental re-evaluation in their quitting process. Smokers reported more relapse and greater temptation and little self-efficacy to smoke, especially in negative/affective situations. Furthermore, the pros of quitting were lower in quitted person but cons of smoking were not different between smokers and non-smokers. This could be explained by high perceived costs of smoking in two groups. The smokers perceived more benefits and costs from smoking simultaneously but, non-smokers perceive low benefit and higher costs of smoking. Furthermore, the temptation rate decreased and self-efficacy increased over the time. In consistent with our findings Fang et al.[42] reported that their intervention resulted in greater self-efficacy, and greater pros of quitting over time but, in contrast to our study their participants reported fewer cons of quitting at 3-month follow-up. In this area, it should be noted that the cons and barriers of smoking in both control and treatment groups were high in baseline and not changed in post baselines. In the study, the minimal intervention strategy was influenced only the intention to quit and self-efficacy only for high educated patients but, did not increased pros of quitting and pros of smoking.[43]
The results showed that people who quit are more likely to use behavioral process than smokers. According to TTM, smokers who are in the early stages apply more cognitive and experiential processes but when they started to quit and moving to later stages, they use behavioral processes.[44]
In contrast to TTM, quit participants reported more consciousness raisings and social liberation than smokers. In this area, Glanz et al.,[45] reported that social liberation has unclear relationship to the stages. In line with consciousness raising, it could be explained that people who quit may increase their awareness about smoking and its complications. However, others reported that there was not consistent relationship between the stages of change and processes that used and suggested that more basic research, especially longitudinal studies are need.[15,46,47,48]
Our research encountered with some limitations to its generalizing. First, quit rate was based on participants self-report, and not verified biochemically. Second, its inclusion criteria was only smokers who were in preparation stage. Third, it's small sample size and follow-up until 6-month. Further researches should be useful that included smokers in earlier stage like precontemplation and contemplation.
CONCLUSION
Our findings revealed that uses of individual counseling, telephone follow-ups, and free NRT in motivated and prepared people to quit, increased the continuous abstinence rate. Hence, it is recommended that to establish counseling centers in primary care systems, along with free provision of NRT, and access to quit line. Definitely, it could be possible to change the current tobacco control policy by policymakers.
Footnotes
Source of Support: Isfahan University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.WHO. Report on the Global Tobacco Epidemic, 2008. [Last accessed 7 Apr 2008]. Available from: http://www. who.int/tobacco/mpower/en/index.html .
- 2.Mohammad K, Noorbala AA, Majdzadeh SR, Karimloo M. Trends of prevalence of tobacco consumption in Iran, (1991-99) according to two national health and disease projects. Hakim J. 2000;197:290–4. [Google Scholar]
- 3.Trends in tobacco use among school students in the Eastern Mediterranean Region, 2007. Available from: http://www.emro.who.int/tfi/pdf/tobacco%20-among-school-students.pdf .
- 4.Fiore MC, Bailey WC, Cohen SJ, Dorfman SF, Goldstein MG, Gritz ER, et al. Rockville, MD, US: Department of Health and Human Services, Public Health Service; 2000. Treating tobacco use and dependence: Clinical Practice Guideline; p. 197. [Google Scholar]
- 5.National Heart, Lung and Blood Institute. Report of the task force on behavioral research in Cardiovascular, lung and blood health and disease (executive summary) 2003. [Last accessed 2003 Jul 10, at 12:30]. Available form: http://www.nhlbi.nih.gov/resource/docs/task forc.pdf .
- 6.Mehrabi S, Delavari A, Moradi GH, Esmailnasab N, Pooladi A, Alikhani S, et al. Smoking among 15-to 64-year-old Iranian people in 2005. J Epidemiol. 2007;1-2:1–9. [Google Scholar]
- 7.Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: Toward an integrative model of change. J Consult Clin Psychol. 1983;51:390–5. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- 8.Bridle C, Riemsma RP, Pattenden J, Sowden AJ, Mather L, Watt IS, et al. Systematic review of the effectiveness of health behavior intervention based on transtheoretical model. Psychol Health. 2005;20:283–301. [Google Scholar]
- 9.Dijkstra A, De Vries H. The development of computer-generated tailored interventions. Patient EducCouns. 1999;36:193–203. doi: 10.1016/s0738-3991(98)00135-9. [DOI] [PubMed] [Google Scholar]
- 10.Dijkstra A, De Vries H, Roijackers J. Targeting smokers with low readiness to change with tailored and nontailored self-help materials. Prev Med. 1999;28:203–11. doi: 10.1006/pmed.1998.0407. [DOI] [PubMed] [Google Scholar]
- 11.Strecher VJ. Computer-tailored smoking cessation materials: A review and discussion. Patient Educ Couns. 1999;36:107–17. doi: 10.1016/s0738-3991(98)00128-1. [DOI] [PubMed] [Google Scholar]
- 12.Velicer WF, Norman GJ, Fava JL, Prochaska JO. Testing 40 predictions from the transtheoretical model. Addict Behav. 1999;24:455–69. doi: 10.1016/s0306-4603(98)00100-2. [DOI] [PubMed] [Google Scholar]
- 13.Velicer WF, Prochaska JO, Rossi JS, Snow MG. Assessing outcome in smoking cessation studies. Psychol Bull. 1992;111:23–41. doi: 10.1037/0033-2909.111.1.23. [DOI] [PubMed] [Google Scholar]
- 14.Hall KL, Rossi JS. Meta-analytic examination of the strong and weak principles across 48 health behaviors. Prev Med. 2008;46:266–74. doi: 10.1016/j.ypmed.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 15.Prochaska JO, Velicer WF, DiClemente CC, Fava J. Measuring processes of change: Applications to the cessation of smoking. J Consult Clin Psychol. 1988;56:520–8. doi: 10.1037//0022-006x.56.4.520. [DOI] [PubMed] [Google Scholar]
- 16.Prochaska JO, Veliver WF. The transtheoretical model of health behavior change. Am J Health Prom. 1997;12:38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- 17.Chacko MR, von Sternberg K, Velasquez MM, Wiemann CM, Smith PB, DiClemente R. Young women's perspective of the pros and cons to seeking screening for chlamydia and gonorrhea: An exploratory study. J Pediatr Adolesc Gynecol. 2008;21:187–93. doi: 10.1016/j.jpag.2007.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bandura A. New York: W.H. Freeman; 1997. chapter 6. Self-efficacy: The Exercise and Control; p. 18. [Google Scholar]
- 19.DiClemente CC, Prochaska JO, Gilbertini M. Self-efficacy and the stages of self-change of smoking. Cognit Ther Res. 1985;9:181–200. [Google Scholar]
- 20.Prochaska JO, DiClemente CC, Velicer WF, Ginpil S, Norcross JC. Predicting change in smoking status for self-changers. Addict Behav. 1985;10:395–406. doi: 10.1016/0306-4603(85)90036-x. [DOI] [PubMed] [Google Scholar]
- 21.Wakai K, Marugame T, Kuriyama S, Sobue T, Tamakoshi A, Satoh H, et al. Decrease in risk of lung cancer death in Japanese men after smoking cessation by age at quitting: Pooled analysis of three large-scale cohort studies. Cancer Sci. 2007;98:584–9. doi: 10.1111/j.1349-7006.2007.00423.x. 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Le Houezec J. Non-dopaminergic pathways in nicotine dependence. Psycoloquy. 2001;12:002. Nicotine Addiction (2) Available from: http://www.cogsci.ecs.soton.ac.uk/cgi/psyc/newpsy?12.002 . [Google Scholar]
- 23.Cinciripini PM, McClure JB. Smoking cessation: Recent developments in behavioral and pharmacologic interventions. Oncology (Williston Park) 1998;12:249–56. 259. [PubMed] [Google Scholar]
- 24.Silagy C, Lancaster T, Stead L, Mant D, Fowler G. Nicotine replacement therapy for smoking cessation. Cochrane Database Syst Rev. 2004;3:CD000146. doi: 10.1002/14651858.CD000146.pub2. [DOI] [PubMed] [Google Scholar]
- 25.Helgason AR, Tomson T, Lund KE, Galanti R, Ahnve S, Gilljam H. Factors related to abstinence in a telephone helpline for smoking cessation. Eur J Public Health. 2004;14:306–10. doi: 10.1093/eurpub/14.3.306. [DOI] [PubMed] [Google Scholar]
- 26.Stead LF, Perera R, Lancaster T. Telephone counselling for smoking cessation. Cochrane Database Syst Rev. 2006;3:CD002850. doi: 10.1002/14651858.CD002850.pub2. [DOI] [PubMed] [Google Scholar]
- 27.Erol S, Erdogan S. Application of a stage based motivational interviewing approach to adolescent smoking cessation: The Transtheoretical Model-based study. Patient Educ Couns. 2008;72:42–8. doi: 10.1016/j.pec.2008.01.011. [DOI] [PubMed] [Google Scholar]
- 28.DiClemente CC, Prochaska JO, Fairhurst SK, Velicer WF, Velasquez MM, Rossi JS. The process of smoking cessation: An analysis of precontemplation, contemplation, and preparation stages of change. J Consult Clin Psychol. 1991;59:295–304. doi: 10.1037//0022-006x.59.2.295. [DOI] [PubMed] [Google Scholar]
- 29.Velicer WF, DiClemente CC, Prochaska JO, Brandenburg N. Decisional balance measure for assessing and predicting smoking status. J Pers Soc Psychol. 1985;48:1279–89. doi: 10.1037//0022-3514.48.5.1279. [DOI] [PubMed] [Google Scholar]
- 30.Velicer WF, Diclemente CC, Rossi JS, Prochaska JO. Relapse situations and self-efficacy: An integrative model. Addict Behav. 1990;15:271–83. doi: 10.1016/0306-4603(90)90070-e. [DOI] [PubMed] [Google Scholar]
- 31.Charkazi A, Shahnazi H, Ghourchaei AB, Mirkarimi K. Smoking behaviors in Iranian male students: An application of transtheoretical model. J Educ Health Promot. 2012;1:62–6. doi: 10.4103/2277-9531.99954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerströmtest for nicotine dependence: A revision of the Fagerströmtolerance questionnaire. Br J Addict. 1991;86:1119–27. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 33.Fagerstrom KO, Schneider NG. Measuring nicotine dependence: A review of the Fagerstromtolerance questionnaire. J Behav Med. 1989;12:159–82. doi: 10.1007/BF00846549. [DOI] [PubMed] [Google Scholar]
- 34.Heydari GH. Good time for starting smoking cessation programs. Pajohandeh. J Shahid Beheshti Univ Med Sci. 2009;14:53–7. [Google Scholar]
- 35.Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: Toward an integrative model of change. J Consult Clin Psychol. 1983;51:390–5. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- 36.Stapleton JA, Russell MA, Feyerabend C, Wiseman SM, Gustavsson G, Sawe U, et al. Dose effects and predictors of outcome in a randomized trial of transdermal nicotine patches in general practice. Addiction. 1995;90:31–42. doi: 10.1046/j.1360-0443.1995.901316.x. [DOI] [PubMed] [Google Scholar]
- 37.American Psychiatric Association. Practice guideline for the treatment of patients with nicotine dependence. Am J Psychiatry. 1996;153(10):31–37. doi: 10.1176/ajp.153.10.1. [DOI] [PubMed] [Google Scholar]
- 38.Alberg AJ, StashefskyMargalit R, Burke A, Rasch KA, Stewart N, Kline JA, et al. The influence of offering free transdermal nicotine patches on quit rates in a local health department's smoking cessation program. Addict Behav. 2004;29:1763–78. doi: 10.1016/j.addbeh.2004.04.007. [DOI] [PubMed] [Google Scholar]
- 39.Nohlert E, Tegelberg A, Tillgren P, Johansson P, Rosenblad A, Helgason AR. Comparison of a high and a low intensity smoking cessation intervention in a dentistry setting in Sweden: A randomized trial. BMC Public Health. 2009;9:121. doi: 10.1186/1471-2458-9-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McAlister AL, Rabius V, Geiger A, Glynn TJ, Huang P, Todd R. Telephone assistance for smoking cessation: One year cost effectiveness estimations. Tob Control. 2004;13:85–6. doi: 10.1136/tc.2003.004515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Heydari GR, Jianfar G, Alvanpour A, Hesami Z, Talischi F, Masjedi MR. Efficacy of telephone quit-line for smokers in Iran: 12 months follow up results. Tanaffos. 2011;10:42–8. [PMC free article] [PubMed] [Google Scholar]
- 42.Fang CY, Ma GX, Miller SM, Tan Y, Su X, Shive S. A brief smoking cessation intervention for Chinese and Korean American smokers. Prev Med. 2006;43:321–4. doi: 10.1016/j.ypmed.2006.06.009. [DOI] [PubMed] [Google Scholar]
- 43.Wiggers LC, Oort FJ, Dijkstra A, de Haes JC, Legemate DA, Smets EM. Cognitive changes in cardiovascular patients following a tailored behavioral smoking cessation intervention. Prev Med. 2005;40:812–21. doi: 10.1016/j.ypmed.2004.09.028. [DOI] [PubMed] [Google Scholar]
- 44.Prochaska JO, DiClemente CC, Norcross JC. In search of how people change. Applications to addictive behaviors. Am Psychol. 1992;47:1102–14. doi: 10.1037//0003-066x.47.9.1102. [DOI] [PubMed] [Google Scholar]
- 45.Glanz K, Rimer BK, Viswanath K. 4th ed. San Francisco: Jossey-Bass; 2008. chapter 6. Health behavior and health education, theory research, and practice; pp. 105–7. [Google Scholar]
- 46.Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12:38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- 47.Littell JH, Girvin H. Stages of change. A critique. Behav Modif. 2002;26:223–73. doi: 10.1177/0145445502026002006. [DOI] [PubMed] [Google Scholar]
- 48.Sutton S. Back to the drawing board? A review of applications of the transtheoretical model to substance use. Addiction. 2001;96:175–86. doi: 10.1046/j.1360-0443.2001.96117513.x. [DOI] [PubMed] [Google Scholar]


