Abstract
Background:
The conjunctiva is a thin and flexible mucus membrane that provides a protective barrier to the eye. Very few histopathologic studies have been conducted on conjunctival biopsies in eastern India.
Materials and Methods:
120 conjunctival biopsies from 117 patients (76 males, 41 females) received during 8 years (January 2003–December 2010) were included in this study.
Results:
Histologic diagnoses were: degenerative lesions in 38 cases (31.66%), benign epithelial lesions in 23 cases (19.16%), premalignant and malignant epithelial lesions in 27 cases (22.5%), melanocytic lesions in 10 cases (8.33%), lymphoid in 7 cases (5.83%), and miscellaneous in 15 cases (12.5%).
Conclusion:
Squamous papilloma was the commonest benign tumor, whereas the commonest malignant tumor was squamous cell carcinoma. Melanocytic lesions were less prevalent compared to other/western studies.
Keywords: Conjunctiva, different lesions, histopathology
INTRODUCTION
The conjunctiva is a thin and flexible mucus membrane that extends from the internal surface of the eyelid (palpebral conjunctiva) to the fornix and the anterior surface of the ocular globe (bulbar conjunctiva) up to the sclerocorneal limbus (limbal conjunctiva). Its functions include contributing to the precorneal lacrimal film by means of producing the mucus layer and providing a protective barrier for infections and foreign bodies.[1]
Conjunctival tumors comprise a large variety of conditions from benign lesions such as squamous papilloma, or nevus, to malignant lesions such as melanoma or squamous cell carcinoma (SCC) which may cause visual loss. So, early diagnosis by conjunctival biopsies and treatment are essential to prevent ocular and systemic spread and to preserve visual function.
MATERIALS AND METHODS
The study was conducted in our tertiary care hospital which has a Regional Institute of Ophthalmology (RIO) and is situated in eastern India. All conjunctival biopsies received in the Department of Pathology during an 8-year period (from January 2003 to December 2010) were included in this histopathologic study. A total of 117 patients comprising 76 males and 41 females having conjunctival lesions were studied and histologic diagnoses were given. Three patients had bilateral conjunctival lesions (two males and one female). All the relevant information about the patients was collected from out-patient department tickets and case sheets. Most of the patients (80/117) were adults (>18 years), while pediatric and adolescent (<18 years) patients were 17 and elderly patients (>60 years) were 20 in number. All the tissues were fixed properly and macroscopic features were noted. After processing, paraffin sections were cut at 4–5 mm thickness and stained with Hematoxylin and Eosin stain routinely. Special stains like Periodic Acid Schiff (PAS), Masson–Fontana, and reticulin stain were used whenever necessary. Immunohistochemistry (IHC) was helpful in some of the cases to confirm histologic diagnosis.
Histologically, all the conjunctival lesions were divided into six subgroups, viz. degenerative lesion, benign epithelial lesion, premalignant and malignant epithelial, melanocytic, lymphoid, and miscellaneous lesion.
RESULTS
In this study, we received an unequal representation of male and female patients (76 vs. 41) with a male:female ratio of 1.85:1. A total of 120 conjunctival biopsies from 117 patients were analyzed with three bilateral cases. Table 1 shows the anatomic location and histologic subgroup of conjunctival lesions. Bulbar conjunctiva (limbal and extralimbal) was the commonest location for conjunctival lesions (101 cases), followed by palpebral conjunctiva (12 cases) and fornix (5 cases). Lesions were more common in extralimbal than limbal conjunctiva (72 cases vs. 29 cases). Diffuse involvement of conjunctiva was uncommon and we received only two such cases. Although degenerative, epithelial, and melanocytic lesions were commonly found in bulbar conjunctiva [Figures 1 and 2], these lesions were rare in palpebral conjunctiva. Common lesions found in palpebral conjunctiva were granulation tissue, vascular neoplasm, and rhinosporidiosis. One each case of lymphoma and SCC diffusely involved the bulbar fornix and palpebral conjunctiva. In the fornix, no degenerative or melanocytic lesion was observed in the present study.
Table 1.
Distribution of conjunctival lesions according to histologic subgroup and anatomic locations (N = 120)
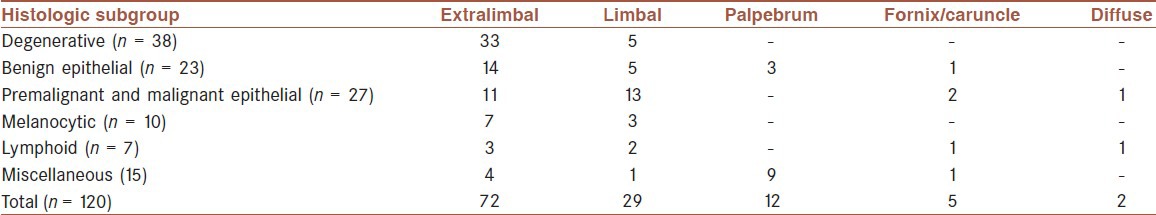
Figure 1.
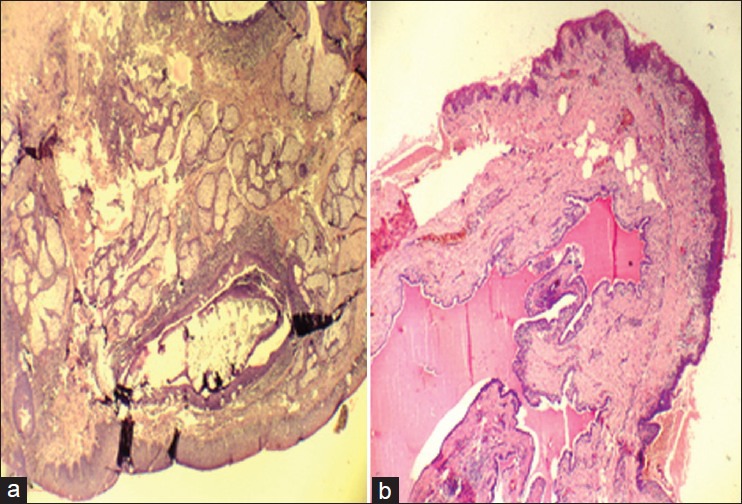
(a) Photomicrograph showing dermoid cyst (benign cystic teratoma) in conjunctiva. There are squamous epithelium and adnexal glands including sebaceous glands in the subepithelial layer (Hematoxylin and Eosin, ×100) (b) Photomicrograph showing epithelial inclusion cyst. A cystic lesion in conjunctiva is lined by epithelial cells (Hematoxylin and Eosin, ×100)
Figure 2.
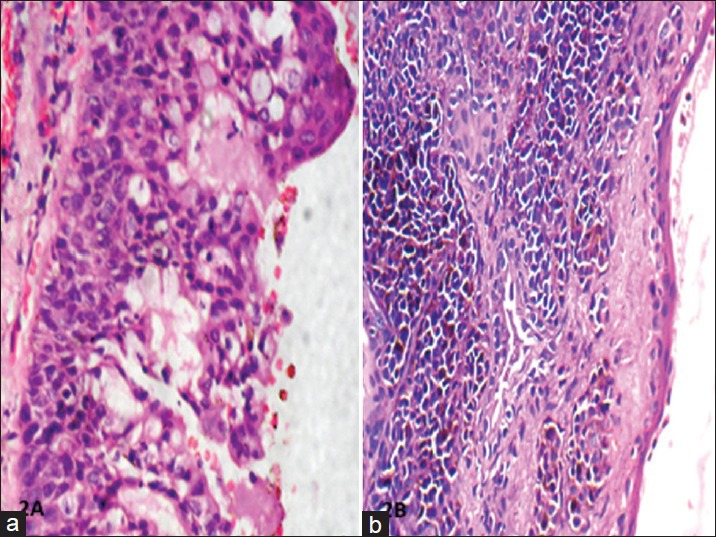
(a) Photomicrograph showing conjunctival intraepithelial neoplasia (CIN). The dysplastic cells involve the full thickness of the squamous layer, but the underlying stroma is uninvolved (Hematoxylin and Eosin, ×100) (b) Photomicrograph showing subepithelial nevus in conjunctiva. There are groups of melanin producing nevus cells underneath the non-keratinized squamous epithelial layer (Hematoxylin and Eosin, ×100)
Distribution of cases according to specific histologic diagnosis and percentage of each category are listed in Table 2. Commonest lesion was degenerative (31.66%), followed by premalignant and malignant epithelial neoplasm (22.5%), miscellaneous group (12.5%), benign epithelial (19.6%), melanocytic lesion (8.33%), and lymphoid (5.83%). Pterygium was a more common degenerative disease than pingueculum. Among the malignant lesions, SCC was the commonest (9 cases), followed by non-Hodgkin's lymphoma (NHL; 2 cases) [Figure 3].
Table 2.
Distribution of cases according to histologic diagnosis and percentage of conjunctival lesions (N = 120)
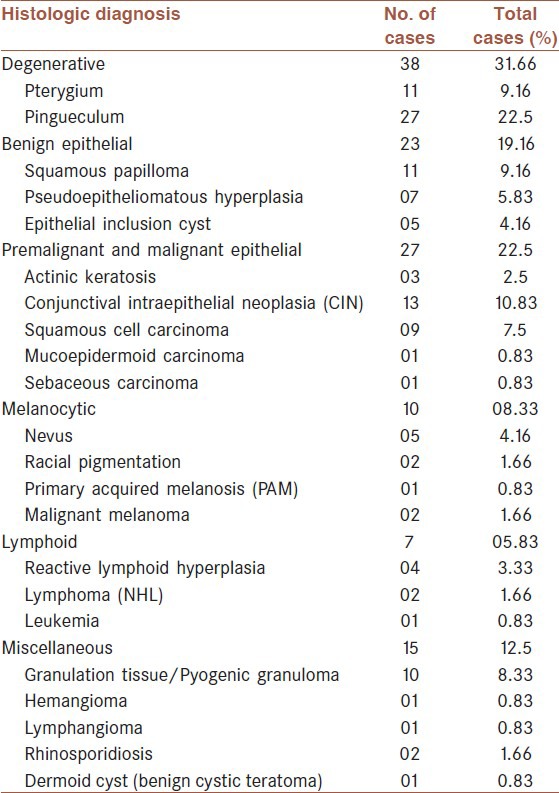
Figure 3.
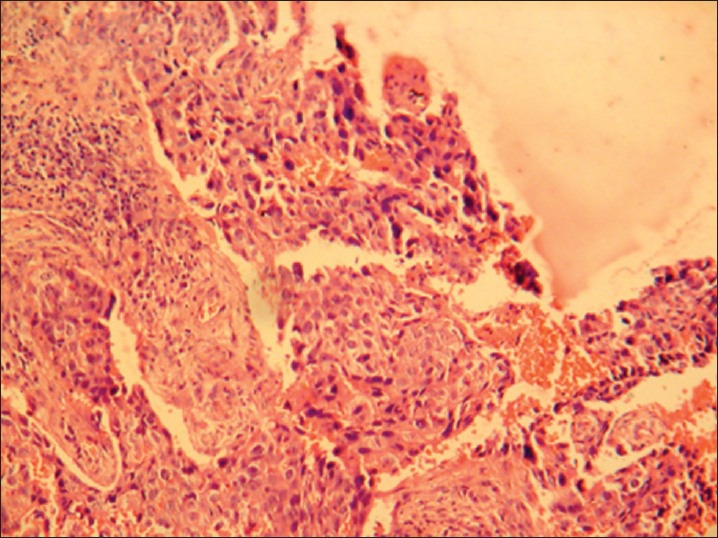
Photomicrograph showing squamous cell carcinoma; malignant squamous epithelial cells infiltrating the underlying stroma (Hematoxylin and Eosin, ×100)
DISCUSSION
Conjunctival lesions comprise a large variety of conditions which may threaten visual function and life of the patients if not diagnosed early.[2] In the epidemic review of all the eye cancers from the Singapore Cancer Registry, conjunctival cancer accounted for 12.8% of total 125 patients.[3] Yoon and Grossiuklaus published a major series on conjunctival lesions in adults, and found that the common benign lesions were pterygium (18%), dysplasia (7%), inflammation (nonspecific nongranulomatous, 7%), and epithelial inclusion cyst (6%). The common malignant lesions in their study were SCC (4%), melanoma (3%), and sebaceous cell carcinoma (<1%).[4] In our study, the common benign/nonmalignant lesions were pterygium (22.5%), pingueculum (9.16%), squamous papilloma (9.16%), and granulation tissue (8.33%). A total of 16 cases of malignancies (13.3%) were diagnosed in our study. Of these, SCC formed 7.5%, lymphoma (NHL) constituted 1.66%, and there were 2 cases of malignant melanoma (1.6%) and 1 case (0.83%) each of mucoepidermoid carcinoma, sebaceous carcinoma, and leukemic infiltration of acute myeloid leukemia (AML).
In another study, the relative incidence of SCC and malignant melanoma was 50% and 31.25%, respectively.[3] But in our study, incidence of SCC was much higher than that of melanoma (7.5% vs. 0.83%) when compared to other/western studies.[5,6] This might be due to the fact that light pigmentation which is seen in the Whites may be a risk factor for malignant melanoma. Two out of nine cases of SCC had HIV infection in our study, which is presumed to be a causative factor for SCC.[4,7]
Premalignant and malignant epithelial lesions were seen commonly in older patients.[8] Actinic keratosis was located in the interpalpebral area, usually over pre-existing pterygium. Conjunctival intraepithelial neoplasia (CIN)/dysplasia was commonly found in limbus with poorly defined edges. Sometimes it was found to extend over the corneal epithelium. In 2 out of 13 CIN cases, SCC developed later on.[1,9] Three out of the five benign nevi were histologically proved to be compound nevi and two of them were subepithelial nevi. Majority of the patients were from pediatric and adolescent age group, which correlates with other studies.[5,10,11] In one of the nevi, cyst was also found. In the two cases of racial pigmentation, uniform hyperpigmentation of the conjunctival basal layer was noted. Primary acquired melanosis (PAM) appeared as flat lesions in contrast to benign nevi which were scarcely pigmented, slightly elevated lesions. In both the cases of PAM, no atypia was found.[12,13] The only case of malignant melanoma was present in fornix and was composed of both epithelioid and spindle cells (mixed type). Maly et al. proposed a histological scoring protocol in melanocytic conjunctival lesions (MCL). A scoring method of atypia was suggested according to histologic parameters: nest cohesion, melanocytic hyperplasia, nuclear features, and pagetoid spread. Lesions were scored according to the number of criteria as mild (1–2), moderate (3–4), and severe (5–8).[14]
Both the lymphoma cases in our study were of low-degree non-Hodgkin's type and classified as marginal zone B cell lymphoma according to World Health Organization (WHO) or mucosa associated lymphoid tissue (MALT) lymphoma. One of them involved the conjunctiva bilaterally.[15] Vascular neoplasm (hemangioma and lymphangioma, one case each) was diagnosed by indocyanine green angiography pre-biopsy which subsequently correlated with histologic examination.[1,16]
To conclude, a large variety of conjunctival lesions may appear in the conjunctiva. Premalignant and malignant tumors such as carcinoma, lymphoma, or melanoma are aggressive, which jeopardize the vision and may endanger the patient's life. Therefore, early diagnosis is important and their existence must be confirmed by biopsy with histologic evaluation. Surgery combined with different supporting therapies (cryotherapy, chemotherapy, or others) is required to treat these lesions and for achieving local control of the disease. The core of a good approach for treating conjunctival tumors continues to hinge on a good histopathologic study and diagnostic. So, clinicopathological correlation is crucial, requiring good communication between the clinician (ophthalmologist) and the pathologist.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Rodrigues MM, Hidayat AA. Conjunctival and corneal pathology. In: Albert DM, Jackobiec FJ, editors. Principles and Practice of Ophthalmology. Vol. 4. Philadelphia: WB Saunders; 2000. pp. 3609–33. [Google Scholar]
- 2.Font RL, Croxatto O, Rao N. Washington: American Registry of Pathology and Armed Forces Institute of Pathology; 2006. Tumors of the eye and ocular adnexa; pp. 1–40. [Google Scholar]
- 3.Lee SB, Au Eong KG, Saw SM, Chan TK, Lee HP. Eye cancer incidence in Singapore. Br J Ophthalmol. 2000;84:767–70. doi: 10.1136/bjo.84.7.767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yoon YD, Grossniklaus H. Tumors of the cornea and conjunctiva. Curr Opin Ophthalmol. 1997;8:55–8. doi: 10.1097/00055735-199708000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Shields CL, Shields JA. Tumors of conjunctiva and cornea. Surv Ophthalmol. 2004;49:3–24. doi: 10.1016/j.survophthal.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 6.Spraul CW, Grossniklaus HE. Tumors of the cornea and conjunctiva. Curr Opin Ophthalmol. 1996;7:28–34. doi: 10.1097/00055735-199608000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Saronil MA, Becerra E, Mendez MC, Blanco G. Conjunctival tumors. Arch Soc Esp Oftalmol. 2009;84:7–22. doi: 10.4321/s0365-66912009000100003. [DOI] [PubMed] [Google Scholar]
- 8.Tost F, Evert M. Conjunctival tumors in elderly patients. Klin Monbl Augenheilkd. 2010;227:33–42. doi: 10.1055/s-0028-1109952. [DOI] [PubMed] [Google Scholar]
- 9.Mauriello JA, Jr, Napolatino J, McLean I. Actinic keratosis and dysplasia of conjunctiva: A clinicopathological study of 45 cases. Can J Ophthalmol. 1995;30:312–6. [PubMed] [Google Scholar]
- 10.Shields CL, Shields JA. Conjunctival tumors in children. Curr Opin Ophthalmol. 2007;18:351–60. doi: 10.1097/ICU.0b013e32823ecfbb. [DOI] [PubMed] [Google Scholar]
- 11.Bella LA, Aftane Evina T, Omgbwa Eballe A. Childhood ocular tumors: Epidemological and histopathological aspects at the Yaounde gynaeco obstetric and pediatric hospital. Sante. 2010;20:139–41. doi: 10.1684/san.2010.0198. [DOI] [PubMed] [Google Scholar]
- 12.Shields CL, Demirci H, Karatza E, Shields JA. Clinical survey of 1643 melanocytic and nonmelanocytic conjunctival tumors. Ophthalmology. 2004;111:1747–54. doi: 10.1016/j.ophtha.2004.02.013. [DOI] [PubMed] [Google Scholar]
- 13.Alkatan HM, Al-Afraj KM, Maktabi A. Conjunctival nevi: Clinical and histopathologic features in a Saudi population. Ann Saudi Med. 2010;30:306–12. doi: 10.4103/0256-4947.65265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maly A, Epstein D, Meir K, Pe’er J. Histologic criteria for grading of atypia in melanocytic conjunctival lesions. Pathology. 2008;40:676–81. doi: 10.1080/00313020802436428. [DOI] [PubMed] [Google Scholar]
- 15.Mondal SK. Mucosa associated lymphoid tissue lymphoma of conjunctiva: A case report. Indian J Pathol Microbiol. 2008;51:407–8. doi: 10.4103/0377-4929.42539. [DOI] [PubMed] [Google Scholar]
- 16.Baumuller S, Kosanetzky N, Charbel IP, Holz FG, Loffler KU. Vascular lesion of the conjunctiva. Ophthalmologe. 2009;106:832–5. doi: 10.1007/s00347-009-1939-8. [DOI] [PubMed] [Google Scholar]


