Abstract
Background and Objectives:
There has been a rapid expansion of the directly observed treatment short-term (DOTS) under the revised national tuberculosis control program throughout India in the last decade. Few reports exist detailing individual DOTS centers’ experiences with regard to extrapulmonary tuberculosis (EPTB) in a medical college hospital setting.
Materials and Methods:
This is a retrospective, record-based study of patients with the diagnosis of EPTB, in all age groups. Data on all consecutive EPTB cases diagnosed at the K. S. Hegde Medical College and Hospital, Deralakatte, Mangalore from 1 January 2005 to 31 December 2011 at the DOTS centre attached to this hospital were collected, analyzed by Mantel-Haenszel Chi square for linear trend and described in proportion or percentages.
Results:
Among 1267 cases registered for treatment of all forms of tuberculosis, 528 (41.67%) had EPTB. Around half of the cases of EPTB (269, 51%) were among adult age groups and the majority of cases (342, 64.77%) received Category-I treatment. Pleural TB was the commonest type of EPTB (n = 148, 28.03%), followed by lymph node TB (n = 131, 24.81%). Involvement of lymph nodes was the commonest manifestation among the less than 14 years’ age group (27, 58.7%), while involvement of pleura was more common among > 65 years’ age group (23, 45.1%). The difference in the occurrence of EPTB by site between males and females is statistically significant with a P value of <0.005. There is a significant increase in the number of cases of tuberculosis affecting bones and joints, and other forms of tuberculosis over the years.
Conclusion:
The burden of EPTB is more among the productive age group. Increase in the trend of bone and joint tuberculosis, and other rare forms of EPTB is a point of concern highlighting the importance of strengthening the services towards this group.
Keywords: Directly observed treatment short-course, Extrapulmonary tuberculosis, India, Revised national tuberculosis control program
INTRODUCTION
The burden of tuberculosis (TB) in India is the highest, accounting for one-fifth (21%) of the global incidence.[1] TB mortality in the country as well as the prevalence of TB has reduced from 1990 to 2010 as per the World Health Organization (WHO) global TB report.[2]
From the point of view of public health, the highest priority in TB control programs is the identification and treatment of sputum-positive infectious patients. Pulmonary TB is the most important clinical manifestation of this infection, as it is both the most common presentation and practically the only form of the disease that is infectious. TB affecting other sites-known as extra-pulmonary TB is rarely smear-positive; it is generally accepted that the contagious potential of this form is negligible and it has, therefore, never been a priority in the campaigns undertaken by national TB control programs.[3] Also, the literature on the various forms of EPTB is scant and this lack of evidence is of particular concern in the case of treatment guidelines. The percentage of patients with EPTB in tertiary care centers in India was between 30% and 53%, while the percentage estimated by the national control program in India for HIV-negative adults is between 15% and 20%.[4] Extrapulmonary tuberculosis becomes more important as chances of developing EPTB in immunocompromised patients are higher than in their immunocompetent counterparts.[5,6] Recent studies have suggested that the sites of EPTB may vary according to geographic location, population groups and a wide variety of host factors.[7–10]
A call has been made for India to do more to combat the extrapulmonary form of tuberculosis. The Indian branch of Advocacy to Control TB Internationally (ACTION) says the country’s TB control program is failing to take sufficient action to diagnose cases of the condition. Diagnosis of EPTB is not covered by RNTCP; and for treatment these cases are forwarded to the DOTS regimen. Tertiary care centers appear to be an excellent place for medical education and operational research in this regard. This is much needed, as HIV-TB co-infection, multi-drug-resistant TB and EPTB continue to be major public health threats even in the era of DOTS. With this background we conducted the present study at the K. S. Hegde Medical Academy, Deralakatte, Mangalore, Karnataka, India. The primary objective of this study was to describe the basic demographic, clinical characteristics, program-specified treatment protocols and the trend of extrapulmonary tuberculosis patients registered for TB treatment in this tertiary center attached to a medical college hospital.
MATERIALS AND METHODS
The study was done at the K. S. Hegde Medical College Hospital, Deralakatte, Mangalore, Karnataka, India. A retrospective analysis of data of patients with EPTB registered for treatment under DOTS for the period of 1 January 2005 to 31 December 2011 was carried out. The DOTS program was started and implemented across Dakshina Kannada district, Karnataka over a period of time (January 2003-December 2004) covering the entire population of 18, 97, 730 (2001 census). The DOTS program was started in the center attached to the medical college hospital in the month of July 2004.
Source of information and definitions
The sources of information were the TB register and patient record sheets. In all the cases of EPTB, sputum examinations and chest radiographs were used to investigate the involvement of lung parenchyma. The diagnosis of EPTB was based on the following criteria: (i) Suggestive clinical features, (ii) Positive microbiological or histopathological evidence of Mycobacterium tuberculosis from an extrapulmonary site, (iii) Radiological changes consistent with extrapulmonary TB followed by the decision of the treating MO to treat with a full course of anti-TB therapy,[11] and (iv) A satisfactory response to antituberculosis therapy.[12] A patient diagnosed with both pulmonary and extrapulmonary TB was classified as pulmonary TB and was excluded from the study. Extrapulmonary TB is defined as TB of any organ other than the lungs, such as the pleura (TB pleurisy), peripheral lymph nodes, intestines, genitourinary tract, skin, joints and bones, meninges of the brain, etc. Investigations included fine needle aspiration cytology (FNAC) for lymph node, FNAC and histopathology for skin, genitourinary and breast tuberculosis, X-ray for bone tuberculosis, synovial biopsy for joint tuberculosis, cerebro-spinal fluid CSF cytology and biochemistry for tuberculous meningitis, contrast-enhanced computed tomography (CT) or magnetic resonance imaging (MRI) of brain, MRI of spine, chest skiagram and pleural fluid study for tuberculous pleural effusion.
Method of data collection
The institutional ethical committee clearance was taken before the study. At the first step, all the records pertaining to extrapulmonary TB cases registered from January 2005 to December 2011 were separated and analysed. All the 528 subjects were included in the study. The data was entered into a structured proforma. Study variables included: demographic (age and sex), clinical (disease classification, type of TB, site of extrapulmonary TB (EPTB)) and treatment-related (categorization and treatment regimens).
Data analysis
The collected data was entered and analyzed by using SPSS Version 12. Chi-square test was used to know if differences observed in different groups were statistically significant. To calculate the test for linear trend, Mantel-Haenszel Chi-square for linear trend was used. Data was described in proportion or percentages. P value of < 0.05 was considered significant.
RESULTS
Among 1267 cases registered for treatment of all forms of tuberculosis, 528 (41.67%) had EPTB. Males (272, 51.52%) contributed to a slightly greater number of cases than females (256, 48.48%). On classification of cases according to the treatment regimen given, 342 (64.77%), 26 (4.92%) and 157 (29.73%) cases received Category-I (2H3R3Z3E3 + 4H3R3), Category-II (2H3R3Z3E3S3 + 1H3R3Z3E3 + 5H3R3E3) and Category-III (2H3R3E3 + 4H3R3) treatment respectively. Three (0.57%) cases received non-DOTS regimen, and all of them had liver disease with elevated liver enzymes. The cases were divided into four age groups as 0–14 years, 15–44 years, 45-64 years and more than 65 years. The numbers (percentage) in the above age groups were 46 (8.71%), 269 (50.95%), 162 (30.68%) and 51 (9.66%) respectively [Table 1]. Symptoms in the study subjects included fever (n = 396), swelling at the affected site (n = 216), pain in the affected site (n = 255), headache (n = 28), neurological weakness (n = 22), altered bowel habits (n = 19) and genitourinary symptoms (n = 23). The diagnostic modalities included FNAC from the lesion (n = 166), biopsy from the lesion site (n = 94), cytological and biochemical examination of body fluids [CSF (n = 23), ascitic fluid (n = 28), pleural fluid (n = 148)] and MRI of spine (n = 28) [Figures 1 and 2].
Table 1.
Demographic and clinical characteristics of EPTB patients (N = 528)
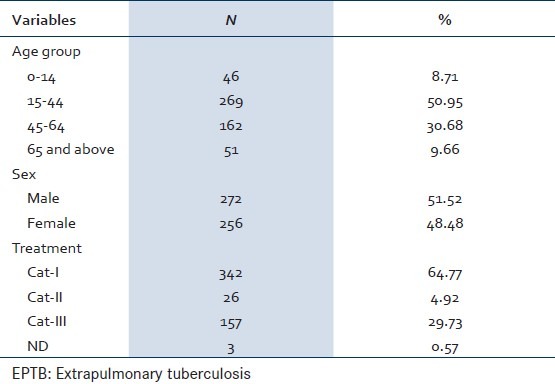
Figure 1.
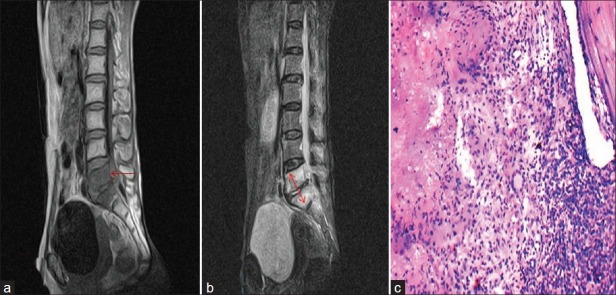
Classical paradiscal tuberculosis of the spine (a) T1W MRI sagittal view showing hypointense L5 and S1 vertebral bodies and arrow shows elevation of posterior longitudinal ligament (b) T2W MRI sagittal view showing hyperintense lesions involving L5 and S1 vertebral bodies suggestive of edema/inflammation (c) Spine TB-10 × H and E, showing caseous necrosis, epithelioid cell, giant cell and bone fragment
Figure 2.
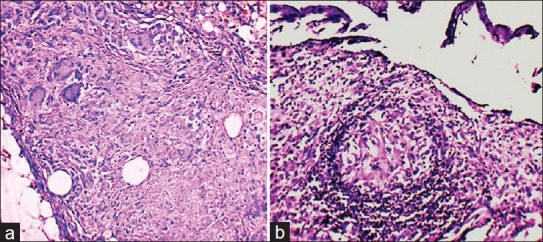
10 × H and E of the biopsy specimen showing (a) Peritoneal TB, fat, granuloma and giant cell (b) Synovial TB with caseous necrosis and the synovial membrane
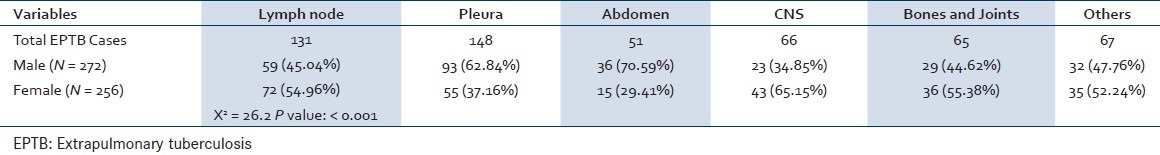
The number and percentage of cases of different types of EPTB in different age groups was calculated. Lymph node tuberculosis was the commonest type of tuberculosis accounting for 58.7% (N = 27) of cases in the age group of 0–14 years. Lymph node TB and pleural TB accounted for 28.25% (N = 76) and 26.77% (N = 72) of cases in the age group of 15–44 years. Pleural TB was the commonest type of presentation in the age group of 45–64 years as well as in the age group of > 65 years [Table 2]. Lymph node TB, central nervous system (CNS) tuberculosis and tuberculosis of bones and joints were more common in females than in males (72, 54.96% vs. 59, 45.04%; 43, 65.15% vs. 23, 34.85% and 36, 55.38% vs. 29, 44.62% respectively). Pleural TB and abdominal TB were more common in males than in females [Table 3]. In this study, 63 cases had diabetes mellitus, 46 had chronic obstructive lung disease, and 11 cases were on oral steroids.
Table 2.
Age distribution of patients with EPTB by site (2005-2011); N = 528
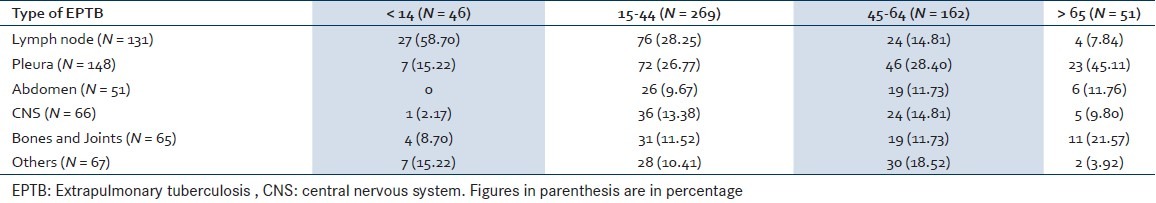
Table 3.
Sex distribution of patients with EPTB (2005-2011); N = 528
Overall, the total number of different types of EPTB cases included lymph node (n = 131, 24.81%), pleural (n = 148, 28.03%), abdomen (n = 51, 9.66%), CNS (n = 66, 12.50%), bones and joints (n = 65, 12.31%) and others (n = 67, 12.69%). Among 51 abdominal TB cases, 28 had ascites, 12 cases had omental involvement with lymphadenopathy, 9 cases had intestinal TB and 2 cases had esophageal TB. EPTB cases treated as others included mainly genitourinary TB (23), skin (9), pericardium (8), eye (6) and breast lump (5). Over the years, the time trend showed that there is a significant increase in the trend of bones and joints’ (X2 = 4.576, P = 0.032), and other forms of tuberculosis (X2 = 4.313, P = 0.038) [Table 4, Figure 3].
Table 4.
Trend of extra-pulmonary TB cases from 2005 to 2011 (N = 528)
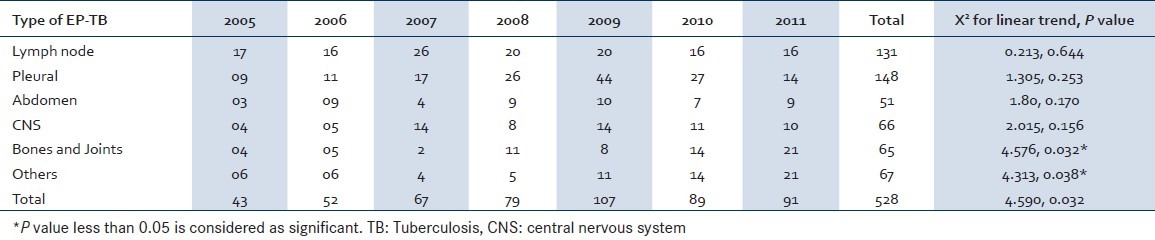
Figure 3.
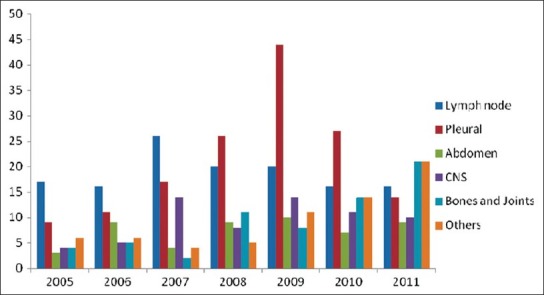
Trend of various types of EPTB cases over 2005-2011
DISCUSSION
The study was done to know the demographic and clinical characteristics of various EPTB patients in this single-center experience, wherein mainly patients from the neighboring three districts seek medical care. Firstly, males (272, 51.52%) and females (256, 48.48%) contributed to nearly an equal number of cases overall. The majority of cases (342, 64.77%) received Category-I treatment, highlighting the faith of treating doctors to use four drugs in the intensive phase even in extrapulmonary cases. This is significant considering the fact that 279 cases (52.84%) belonged to the less serious forms of EPTB, like lymph node and pleural TB. However, with the new RNTCP guidelines since 1 April 2009, there are only two treatment categories, either a new case or a retreatment case. This is a significant positive step in terms of attracting more cases to the program and will also help to reduce the number of retreatment cases in the future. The majority of cases (269, 50.95%) belonged to the age group of 15–44 years, who are young and working individuals, highlighting the socio-economic burden of extrapulmonary tuberculosis. Similar reports of higher incidence of EPTB in younger individuals are reported by other studies as well.[13,14] The number of cases in the pediatric age group (< 14 years) registered for DOTS treatment is only 46 (8.71%) in this study.
Secondly, lymph node tuberculosis was the commonest type of EPTB accounting for 58.7% of cases in the age group of 0–14 years. Lymph node and pleural TB were the common EPTB cases in the age group of 15–44 years. But, pleural TB was the commonest type of presentation in the age group of 45–64 years as well as in the age group of > 65 years. This raises the possibility that the probability of reactivation in pleura may be higher as the age increases.
Thirdly, lymph node TB, CNS tuberculosis and tuberculosis of bones and joints were more common in females than in males. But, pleural TB and abdominal TB were more common in males than in females. The difference in the occurrence of EPTB by site between males and females is statistically significant in this study. The above two facts show the difference in the occurrence of various types of EPTB cases in different age groups and sexes and the predilection to involve one site over the other depending on the host factors as well. Such demographic and social factors contributing to the development of EPTB were identified by previous reports as well.[9,15–17]
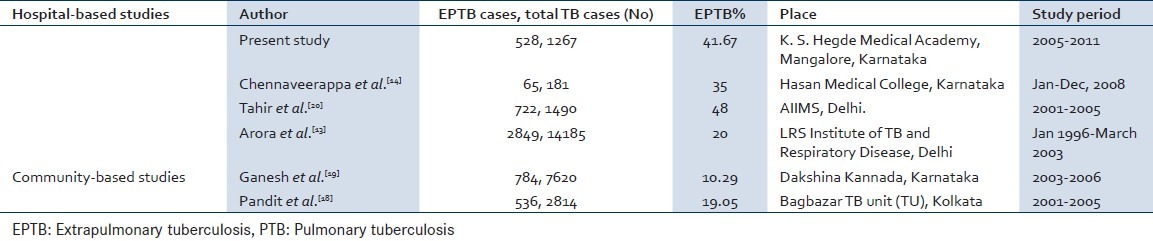
In the present study, there is a gradual, but sustained increase in the number of extrapulmonary cases diagnosed and treated under RNTCP, though the numbers are marginally less in the last two years. The time trend showed that although there is a marginal decrease in lymph node involvement, there is a significant increase in the trend of bones and joints’ and other forms of tuberculosis. A similar trend was observed in Kolkata with an increase in the new EPTB cases during 2000 to 2005.[18] In this study in a tertiary center in Dakshina Kannada district, 41.67% of tuberculosis cases registered for treatment under DOTS had EPTB. But, only 10.29% of tuberculosis cases (784/7620) belonged to the EPTB group during 2003 to 2006 in the entire Dakshina Kannada district of Karnataka.[19] Comparison of the number of PTB and EPTB cases in India by various studies has shown a higher incidence of EPTB cases in tertiary centers and medical college hospitals [Table 5]. EPTB cases need more investigations and invasive procedures for definitive diagnosis and hence are reported more in tertiary centers under the program. Well-defined program-specified protocols and ongoing medical education will increase the total number of EPTB cases detected in the community and treated under the program by gaining the confidence of treating practitioners. This will also help many patients in developing countries who cannot access private healthcare.
Table 5.
Comparison of the number of PTB and EPTB cases in India by various studies
The main limitation of the study is that the treatment outcome and the response to therapy could not be assessed, since cases enrolled for treatment in this tertiary center are transferred out to the neighboring districts of Karnataka as well as Kasaragod and Kannur of northern Kerala for the continuation of treatment. Since this is a hospital-based study, the findings cannot be generalized to the community. But it gives valuable information which can be utilized by the health administrators for the pattern and changing trend of reporting EPTB cases in a tertiary level healthcare center. Testing for HIV infection was carried out only on a fraction of our cases, since the introduction of a voluntary counseling and testing center in the hospital in 2010. Therefore, we did not have enough data for analysis of the association between HIV infection and EPTB.
CONCLUSION
The burden of EPTB is more among the productive age group. The difference in the occurrence of various types of EPTB cases in different age groups and sexes without the declining trend highlights the importance of strengthening the services for this vulnerable group. Higher reporting of EPTB cases in tertiary centers necessitates the need for ongoing medical education on a larger scale and well-defined program-specified protocols for the diagnosis and treatment of extrapulmonary tuberculosis cases.[20]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.DGHS, Central TB Division, Ministry of Health and Family Welfare. TB India, RNTCP Status Report. 2011:114–5. [Google Scholar]
- 2.World Health Organization. Report on Global Tuberculosis Control: Epidemiology, Strategy, Financing. Geneva, Switzerland: WHO; 2009. pp. 1–9. [Google Scholar]
- 3.World Health Organization. Tuberculosis programme: Framework for effective tuberculosis control. Geneva, Switzerland: WHO; 1994. p. 179. [Google Scholar]
- 4.Sharma SK, Mohan A. Extrapulmonary tuberculosis. Indian J Med Res. 2004;120:316–53. [PubMed] [Google Scholar]
- 5.Jones BE, Young SM, Antoniskis D, Davidson PT, Kramer F, Barnes PF. Relationship of the manifestations of tuberculosis to CD4 cell counts in patients with human immunodeficiency virus infection. Am Rev Respir Dis. 1993;148:1292–7. doi: 10.1164/ajrccm/148.5.1292. [DOI] [PubMed] [Google Scholar]
- 6.Narain JP, Lo YR. Epidemiology of HIV-TB in Asia. Indian J Med Res. 2004;120:277–89. [PubMed] [Google Scholar]
- 7.Yang Z, Kong Y, Wilson F, Foxman B, Fowler AH, Marrs CF, et al. Identification of risk factors for extra pulmonary tuberculosis. Clin Infect Dis. 2004;38:199–205. doi: 10.1086/380644. [DOI] [PubMed] [Google Scholar]
- 8.Noertjojo K, Tam CM, Chan SL, Chan-Yeung MM. Extra-pulmonary and pulmonary tuberculosis in Hong Kong. Int J Tuberc Lung Dis. 2002;6:879–86. [PubMed] [Google Scholar]
- 9.Musellim B, Erturan S, Sonmez Duman E, Ongen G. Comparison of extra-pulmonary and pulmonary tuberculosis cases: Factors influencing the site of reactivation. Int J Tuberc Lung Dis. 2005;9:1220–3. [PubMed] [Google Scholar]
- 10.Ilgazli A, Boyaci H, Basyigit I, Yildiz F. Extra pulmonary tuberculosis: Clinical and epidemiologic spectrum of 636 cases. Arch Med Res. 2004;35:435–41. doi: 10.1016/j.arcmed.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 11.Ministry of health and family welfare; Govt of India. Revised National Tuberculosis Control Programme. 2004:5–7. [Google Scholar]
- 12.Sharma SK, Lawaniya S, Lal H, Singh UB, Sinha PK. DOTS centre at a tertiary care teaching hospital: Lessons learned and future directions. Indian J Chest Dis Allied Sci. 2004;46:251–6. [PubMed] [Google Scholar]
- 13.Arora VK, Gupta R. Trends of extra-pulmonary tuberculosis under Revised National Tuberculosis Control Programme: A study from South Delhi. Indian J Tuberc. 2006;53:77–83. [Google Scholar]
- 14.Chennaveerappa PK, Siddharam SM, Halesha BR, Vittal BG, Jayashree N. Treatment outcome of tuberculosis patients registered at dots centre in a teaching hospital, South India. Int J Biol Med Res. 2011;2:487–9. [Google Scholar]
- 15.Cailhol J, Decludt B, Che D. Sociodemographic factors that contribute to the development of extrapulmonary tuberculosis were identified. J Clin Epidemiol. 2005;58:1066–71. doi: 10.1016/j.jclinepi.2005.02.023. [DOI] [PubMed] [Google Scholar]
- 16.Sreeramareddy CT, Panduru KV, Verma SC, Joshi HS, Bates MN. Comparison of pulmonary and extrapulmonary tuberculosis in Nepal-a hospital-based retrospective study. BMC Infect Dis. 2008;8:8. doi: 10.1186/1471-2334-8-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ullah S, Shah SH, Aziz-ur-Rehman, Kamal A, Begum N, Khan G. Extrapulmonary tuberculosis in lady reading hospital Peshawar, NWFP, Pakistan: Survey of biopsy results. J Ayub Med Coll Abbottabad. 2008;20:43–6. [PubMed] [Google Scholar]
- 18.Pandit S, Dey A, Chaudhuri AD, Saha M, Sengupta A, Kundu S, et al. Five-years experiences of the revised national tuberculosis control programme in northern part of Kolkata, India. Lung India. 2009;26:109–13. doi: 10.4103/0970-2113.56343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ganesh KS, Kumar HH, Ramakrishna R, Jayarama S, Kotian MS. Trend of tuberculosis cases under DOTS strategy in dakshina kannada district of Karnataka, India: Issues and challenges. Iran J Public Health. 2009;38:72–6. [Google Scholar]
- 20.Tahir M, Sharma SK, Rohrberg D, Gupta D, Singh UB, Sinha K. DOTS at a tertiary care center in northern India: Successes, challenges and the next steps in tuberculosis control. Indian J Med Res. 2006;123:702–6. [PubMed] [Google Scholar]


