Abstract
Objective:
The aim of this study was to evaluate and compare the efficacy of subgingivally delivered Minocycline microspheres and 25% Metronidazole gel when used as an adjunct to scaling and root planing (SRP) in the treatment of chronic periodontitis.
Materials and Methods:
A randomized, controlled, single center study was conducted involving 60 sites in 20 patients suffering from moderate to advanced chronic periodontitis. Each patient contributed three sites which were randomized to three treatment groups: SRP + insertion of Minocycline microspheres at day 1 (Group A), SRP + insertion of Metronidazole gel at day 1 and at day 7 (Group B), and SRP alone (Group C). Gingival index (GI), plaque index (PI), probing pocket depth (PPD), and clinical attachment level (CAL) were recorded at day 1, 1 month, and 3 months post therapy.
Results:
All treatments showed significant reductions in PPD and CAL at 1 and 3 months when compared to baseline values (P < 0.001). At 3 months, sites treated with minocycline showed an additional reduction in PPD of 0.85 ± 0.03 mm, significantly greater than SRP alone. Differences in mean PPD reduction between Group B and Group C and between Group A and Group B were not significant. At 3 months, difference in CAL gain between Group A and C was 0.50 ± 0.45, which was statistically significant and between Group B and C was 0.35 ± 0.11, which was not found to be statistically significant (P = 0.20). Differences in relative CAL between Group A and Group B were also not found to be statistically significant (P = 0.53).
Conclusion:
The results concluded that treatment with Minocycline microspheres and Metronidazole gel improve PPD and CAL in patients with periodontitis compared to SRP alone.
Keywords: Local drug delivery, metronidazole gel, minocycline microspheres
Introduction
The traditional treatment modality of scaling and root planing remains the ‘gold standard’ for the non-surgical management of chronic periodontitis.[1] Mechanical therapy may, however, fail to reduce or eliminate the anaerobic infection at the base of the pocket, within the gingival tissue or in furcations. Some of the periodontal pathogens travel into lacunar defects in the cementum, which further extend into radicular dentin. These can act as bacterial reservoirs from which re-colonization of mechanically treated root surfaces can occur. The bacterial reservoirs not eliminated by conventional periodontal therapy can be further suppressed with the use of chemotherapeutic agents.[2]
Localized antimicrobial therapy, in particular, has evoked growing interest because of the site-specific nature of periodontal infections, the higher concentration of anti-microbial agent subgingivally and reduced side-effects of systemic antibiotic use.[3] Various locally delivered chemotherapeutic agents available are: Tetracycline fibers, metronidazole gel, minocycline ointment and minocycline microspheres, chlorhexidine chip, doxycycline hyclate, etc.[4]
In vitro studies have shown minocycline hydrochloride to be one of the most active anti-biotic against most microorganisms associated with periodontal disease. Moreover out of all the tetracyclines, minocycline has the most marked substantivity and greater lipid solubility.[5] Recently, minocycline has been incorporated into a controlled release bioresorbable polymer, which serves as the encapsulating medium (Arestin™ Ora Pharma, Inc).
Among the various locally delivered chemotherapeutic agents metronidazole, a member of nitroimidazole class of antibiotics has bactericidal action against anaerobes, such as Prevotela intermedia, Porphyromonas gingivalis, Tannerella forsythia, Fusobacterium species and spirochetes like Treponema denticola, Treponema vincentii, which are generally believed to be the main pathogens associated with periodontitis.[6] A metronidazole-containing gel (25%) (Elyzol®, Alpharma ApS, Denmark) is available for use as local drug-delivery agent.
Many clinical studies have been conducted to assess the efficacy of local drug delivery systems as adjuncts to SRP or as the sole treatment for untreated periodontal lesions.[7,8,9] Few studies have assessed the comparative efficacy of a number of currently marketed systems.[10]
The aim of the present study was to evaluate and compare the efficacy of two local delivery products, one containing minocycline microspheres, Arestin (Ora Pharma Inc., USA) and other containing metronidazole gel, Elyzol (Alpharma ApS, Denmark) used as an adjunct to SRP in the treatment of chronic periodontitis.
Materials and Methods
The subjects for this randomized controlled, split mouth study were selected from the out-patient department of Periodontics, D.A.V. (C) Dental College and Hospital, Yamuna Nagar (Haryana), India. Approval of the study was obtained from the institutional review board of Health Sciences University, Rohtak, Haryana, India to which D.A.V (C) Dental College and Hospital, Yamuna Nagar is affiliated.
In this clinical trial 20 patients (9 females, 11 males) were enrolled in the study. A total of 60 sites among the enrolled subjects were selected for the study. Each patient had at least three teeth with probing pocket depth of 5-8 mm that bled on probing at the initial visit. The selected patients should not have received local and/or systemic antibiotic therapy within the last 6 months prior to the baseline examination of the study. Before starting the trial all the patients underwent full mouth supra and subgingival SRP using an ultrasonic scaler and curettes. They were given careful instructions for self-performed oral hygiene measures. The study was explained to patients and all patients signed informed consent at enrolment. The selected qualifying sites were randomly divided into any of the three parallel treatment arms according to split mouth design. (1) Group A (20 sites): Treated with SRP followed by placement of minocycline microspheres. (2) Group B (20 sites): Treated with SRP followed by placement of metronidazole gel at baseline and again at 7 days. (3) Group C (Control group) (20 sites): Treated with SRP alone.
Subgingival administration of minocycline microspheres was accomplished by inserting the unit-dose cartridge to the base of the periodontal pocket and then pressing the thumb and index finger by the handle mechanism to expel the powder to the base of the pocket [Figure 1]. The metronidazole gel was supplied with a flexible, blunt needle [Figure 2]. This facilitates the application of the gel without traumatizing or damaging the periodontal tissues. After isolating and drying the sites, metronidazole gel was injected into the periodontal pocket and no periodontal dressing was used.
Figure 1.

Insertion of minocycline microspheres
Figure 2.

Insertion of metronidazole gel
Four clinical variables including plaque index,[11] gingival index,[11] probing pocket depth,[12] and clinical attachment level[13] were evaluated at the baseline prior to insertion of test agents and at 1 and 3 months interval.
Results
Computer software (SPSS 10.0 for windows) was used for data analysis. Mean values and standard deviations were calculated for plaque index, gingival index, probing pocket depth and clinical attachment level for all the three groups and at different time intervals. Paired ‘t-test’ was used for comparisons with in the groups and student “t-test” was used for intergroup comparisons. Results were regarded as statistically significant when P < 0.05.
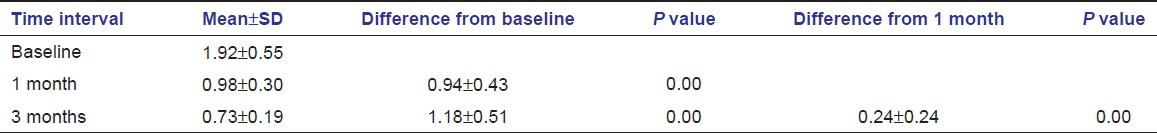
Plaque index and gingival index
The mean plaque index for all three treatment groups at baseline was2.46 ± 0.54 whereas the mean value at 1 and 3 months were 1.06 ± 0.29 and 0.71 ± 0.25 respectively. There was significant reduction in plaque index scores at both 1 month and 3 months interval [Table 1]. The mean gingival index at baseline was 1.92 ± 0.55, whereas the mean value at 1 and 3 months was 0.98 ± 0.30 and 0.73 ± 0.19, respectively. There was significant reduction in plaque index scores at both 1 month and 3 months interval [Table 2].
Table 1.
Comparison of mean values of plaque index scores at Baseline, 1 month and 3 months
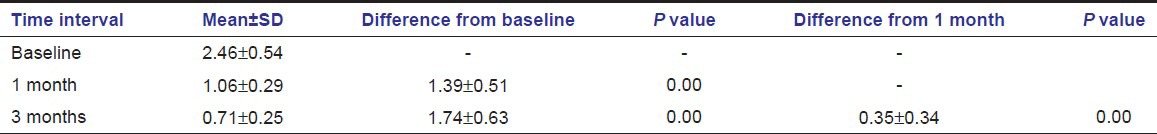
Table 2.
Comparison of mean values of gingival index scores at baseline, 1 month and 3 months
Probing pocket depth
In the present study, intragroup observations showed statistically significant reduction in pocket depth from baseline to 1 month and 3 months in all 3 groups [Table 3]. At the termination of the study (at 3 months), Group A showed an additional pocket depth reduction of 0.85 ± 0.03 over Group C, which was statistically significant and Group B showed an additional reduction of 0.50 ± 0.09 over Group C, which was statistically non-significant. Difference in mean pocket depth reduction between Group A and B was also non-significant (0.35 ± 0.12). Figure 3 represents mean pocket depth reduction at different time intervals.
Table 3.
Intergroup comparison of mean values of pocket depth at baseline, 1 month and 3 months
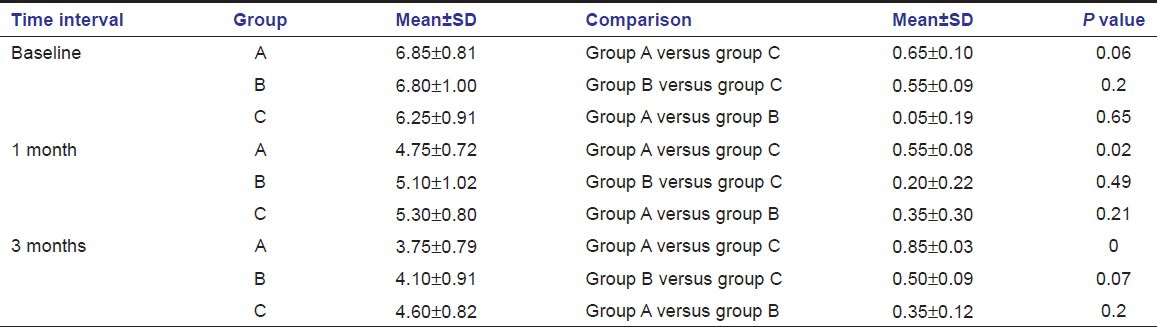
Figure 3.
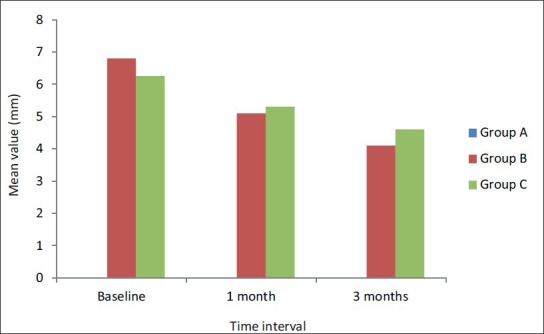
Mean pocket depth reduction at different time intervals
Clinical attachment level
Relative gain in clinical attachment levels (CAL) were observed in all sites when compared with baseline values. The improvements were statistically significant for all the three groups at 1 and 3 months when compared to baseline [Table 4]. At the termination of study, Group A showed 0.50 ± 0.45 mm more improvement in clinical attachment level than Group C, which was statistically significant. Whereas, Group B produced 0.25 ± 0.11 mm more improvement in clinical attachment level than Group C which was statistically non-significant when compared to Group C at 3 months. The difference in CAL gain between Group A and B at 3 months was 0.15 ± 0.56 which was statistically non-significant. Figure 4 shows mean clinical attachment gain at different time intervals.
Table 4.
Intergroup comparison of mean values of clinical attachment level at baseline, 1 month and 3 months
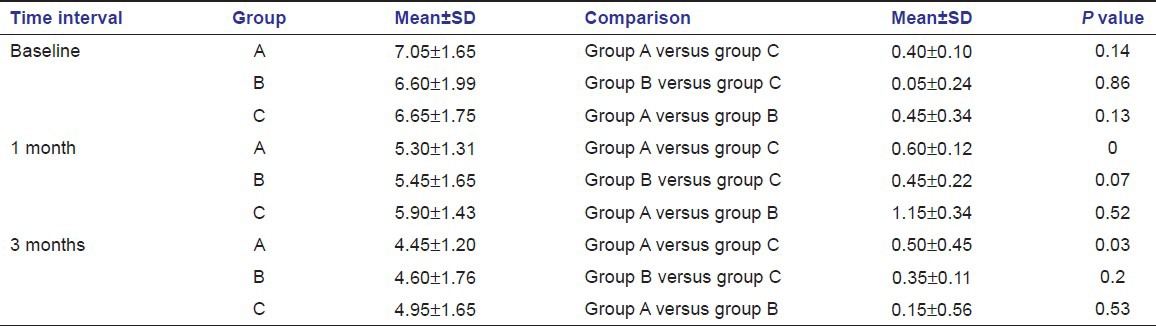
Figure 4.
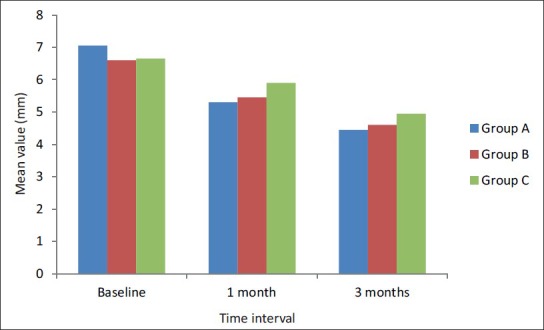
Mean clinical attachment gain at different time intervals
Adverse reaction
Adverse effects were in direct relation to the treatments (scaling, application of microspheres or gel). The most common complaint was related to the bitter taste of the metronidazole reported in majority of patients. The other minor complaints included tooth sensitivity, dental pain, headache, etc., which did not influence patient compliance.
No clinically significant changes in vital signs or hard- or soft-tissues were noted during the course of study.
Discussion
The present study was designed to evaluate the clinical efficacy of locally delivered minocycline microspheres and metronidazole gel use as an adjunct to SRP.
The use of local drugs dates back to 1979 when Goodson et al., 1st discovered local drug delivery system for tetracycline antibiotic.[14] Since then, chlorhexidine (Addy 1982),[15] doxycycline (Garret 1999),[8] minocycline (Jones 1994),[5] metronidazole (Addy 1982)[15] and ofloxacin (Higashi 1990)[16] antimicrobials in the formulation of local delivery devices, have been used for the treatment of periodontitis with variable results.
Amongst the advantages of local drug delivery, most important is that it can attain 100-fold higher concentration of an anti-microbial agent in subgingival sites compared with a systemic drug regimen. It may employ antimicrobial agents not suitable for systemic administration, e.g., broad-spectrum antiseptic solutions. It reduces potential problems with patient compliance. It reduces systemic side effects. It reduces the risk of developing drug-resistant microbial populations at non oral body sites.[17]
Tetracycline group of antibiotics are the most commonly used active agents for the treatment of periodontitis because they are active against periodontopathic micro-organisms, and they offer better resorption, protein binding, diffusion into tissue structure and anti-collagenase property. High degree substantivity is one of the most important characteristics of the drugs and agents to be used for control of microbial plaque.[18] Substantive effects of the tetracyclines within the periodontal pocket-adjacent tooth surface environment have been well documented.[19] The local drug delivery system (Arestin™) in the present study uses a technology of microencapsulating minocycline hydrochloride in a bioabsorbable polymer as the vehicle (polyglycolide-co-dl-lactide). The resulting microspheres are administered in powder form into the diseased periodontal site. Immediately upon contact with moisture, the polymer begins to hydrolyze and release minocycline. The administration results in a sustained local release of the antibiotic whereby concentrations of 340 μgm/ml have been measured in human crevicular fluid even after 14 days. These concentrations far exceed the Minimum Inhibitory Concentrations (MICs) for periodontal pathogens.[20]
Metronidazole specifically targets anaerobic microorganisms but has essentially no activity against aerobic or microaerophilic bacteria. Since anaerobic bacteria are believed to be the predominant causative factor in periodontitis, it might be advantageous to use it in the treatment of chronic periodontitis.[21]
The local drug delivery system (Elyzol) uses a semi-solid suspension of metronidazole benzoate in a mixture of glyceryl mono-oleate and triglyceride (Sesame oil). It is applied in viscous consistency to the pocket where it is liquidized by the body heat and then hardens again forming crystals in contact with water. As a precursor, the preparation contains metronidazole-benozate, which is converted into active substances by esterases in the Gingival Crevicular Fluid (GCF). The MIC50 (minimum inhibiting concentration with 50% inhibitory effect) for the suspected pathogens has been shown to be maintained throughout a 24-hour period after one single gel application.[22] Since metronidazole does not have substantivity beyond 24 h, the application of Elyzol was repeated at 7 days, to maintain effective levels for periopathogens, and to produce additional benefit of the drug for remaining microbes.[23]
It is well established that in organized biofilms, the microorganisms are less susceptible to antimicrobials and there is retarded or incomplete penetration of the agent into the biofilm.[24] Thus, previous biofilm removal could favor greater effectiveness of the antibiotic against subgingival pathogens, leading to improved healing response.[25]
A split mouth design was used in the present study. It has been suggested that a split mouth design may induce a carry-over effect of subgingival antibiotic administration due to wash out of anti-microbial agent and boosting of systemic responses.[10] Although, its’ true, Imery 1986 believed that gingival crevicular fluid is relatively isolated from saliva.[26] Moreover, split mouth design has the big advantage in that it allows paired comparisons to be made.[27]
All the patients showed statistically and clinically significant improvements in gingival and plaque index at both follow-up visit, when compared to baseline levels. Both the gingival and plaque indices remained satisfactory during the entire study period, suggesting that patients complied with the oral hygiene instructions.[13]
In the group treated with minocycline microspheres (Group A), the clinical reduction in probing depth and gain in CAL was substantial and consistent with the reduction of inflammation in the adjacent gingival tissues and reduction in subgingival bacterial load due to minocycline.[12,28] The seemingly greater closure of pockets could be due to possibility of minocycline absorbing onto mineralized dental structures, where it may act as a transient reservoir of the antimicrobial agent during period of substantivity. The drug release kinetics of minocycline is of zero order i.e., it maintains a steady drug concentration for prolonged period of time.[4]
In the group treated with metronidazole gel (Group B) the clinical reduction in probing depth was substantial and consistent with the reduction of inflammation in the adjacent gingival tissues and reduction in subgingival bacterial load due to metronidazole. This reduction in inflammation and presence of healing in the connective tissue subjacent to the junctional epithelium is the primary reason for reducing the depth of periodontal probe penetration after treatment.[23] Metronidazole follows first order kinetics i.e., gel provides increased drug concentration for 24 h after which it subsequently decreases rapidly at a rate directly proportional to their pocket concentration.[27]
Clinical improvement, that is reduction in pocket probing depth and gain in clinical attachment in Group C is due to elimination of local etiologic factors, It has also been proposed that SRP may also elicit a local and systemic host response that would aid in eliminating local infection and promote healing.[29]
The greater gain in CAL in Group A than Group B could be attributed to the non-antibiotic properties of Tetracyclines namely anti-collagenase and anti-inflammatory effect.
Paquette et al.(2004)[30] and Williams et al.(2001)[20] concluded that minocycline microspheres were more effective than SRP alone in reducing probing depths in chronic Periodontitis patients. Griffiths et al.(2000)[26] concluded that metronidazole gel produced significantly better results in terms of pocket depth and CAL when used in combination with SRP. These reports demonstrated improvements related to probing depth reductions and gain in clinical attachment levels that coincided with the results of the current study.
Conclusion
All treatment groups showed significant reduction in probing pocket depth and clinical attachment level gain at 1 and 3 months when compared to baseline. Minocycline treated group showed better efficacy in terms of gain in clinical attachment level and reduction in probing pocket depth followed by metronidazole treated group and then by SRP group.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
References
- 1.Vandekerckhove BN, Quirynen M, van Steenberghe D. The use of locally delivered minocycline in the treatment of chronic periodontitis. A review of the literature. J Clin Periodontol. 1998;25:964–8. doi: 10.1111/j.1600-051x.1998.tb02399.x. [DOI] [PubMed] [Google Scholar]
- 2.Adriaens PA, De Boever JA, Loesche WJ. Bacterial invasion in root cementum and radicular dentin of periodontally diseased teeth in humans. A reservoir of periodontopathic bacteria. J Periodontol. 1988;59:222–30. doi: 10.1902/jop.1988.59.4.222. [DOI] [PubMed] [Google Scholar]
- 3.Tonetti MS, Pini-Prato G, Cortellini P. Principles and clinical applications of periodontal controlled drug delivery with tetracycline fibers. Int J Periodontics Restorative Dent. 1994;14:421–35. [PubMed] [Google Scholar]
- 4.Greenstein G, Polson A. The role of local drug delivery in the management of periodontal diseases: A comprehensive review. J Periodontol. 1998;69:507–20. doi: 10.1902/jop.1998.69.5.507. [DOI] [PubMed] [Google Scholar]
- 5.Jones AA, Kornman KS, Newbold DA, Manwell MA. Clinical and microbiological effects of controlled-release locally delivered minocycline in periodontitis. J Periodontol. 1994;65:1058–66. doi: 10.1902/jop.1994.65.11.1058. [DOI] [PubMed] [Google Scholar]
- 6.Awartani FA, Zulqarnain BJ. Comparison of the clinical effects of subgingival application of metronidazole 25% gel and scaling in the treatment of adult periodontitis. Quintessence Int. 1998;29:41–8. [PubMed] [Google Scholar]
- 7.Cortelli JR, Querido SM, Aquino DR, Ricardo LH, Pallos D. Longitudinal clinical evaluation of adjunct minocycline in the treatment of chronic periodontitis. J Periodontol. 2006;77:161–6. doi: 10.1902/jop.2006.040409. [DOI] [PubMed] [Google Scholar]
- 8.Garrett S, Johnson L, Drisko CH, Adams DF, Bandt C, Beiswanger B, et al. Two multi-center studies evaluating locally delivered doxycycline hyclate, placebo control, oral hygiene, and scaling and root planing in the treatment of periodontitis. J Periodontol. 1999;70:490–503. doi: 10.1902/jop.1999.70.5.490. [DOI] [PubMed] [Google Scholar]
- 9.Knöfler G, Purschwitz R, Jentsch H, Birkenmeier G, Schmidt H. Gingival crevicular fluid levels of aspartate aminotransferase and alpha2-macroglobulin before and after topical application of metronidazole or scaling and root planing. Quintessence Int. 2008;39:381–9. [PubMed] [Google Scholar]
- 10.Radvar M, Pourtaghi N, Kinane DF. Comparison of 3 periodontal local antibiotic therapies in persistent periodontal pockets. J Periodontol. 1996;67:860–5. doi: 10.1902/jop.1996.67.9.860. [DOI] [PubMed] [Google Scholar]
- 11.Timmerman MF, van der Weijden GA, van Steenbergen TJ, Mantel MS, de Graaff J, van der Velden U. Evaluation of the long-term efficacy and safety of locally-applied minocycline in adult periodontitis patients. J Clin Periodontol. 1996;23:707–16. doi: 10.1111/j.1600-051x.1996.tb00599.x. [DOI] [PubMed] [Google Scholar]
- 12.Lu HK, Chei CJ. Efficacy of subgingivally applied minocycline in the treatment of chronic periodontitis. J Periodontal Res. 2005;40:20–7. doi: 10.1111/j.1600-0765.2004.00763.x. [DOI] [PubMed] [Google Scholar]
- 13.van Steenberghe D, Bercy P, Kohl J, De Boever J, Adriaens P, Vanderfaeillie A, et al. Subgingival minocycline hydrochloride ointment in moderate to severe chronic adult periodontitis: A randomized, double-blind, vehicle-controlled, multicenter study. J Periodontol. 1993;64:637–44. doi: 10.1902/jop.1993.64.7.637. [DOI] [PubMed] [Google Scholar]
- 14.Goodson JM, Haffajee A, Socransky SS. Periodontal therapy by local delivery of tetracycline. J Clin Periodontol. 1979;6:83–92. doi: 10.1111/j.1600-051x.1979.tb02186.x. [DOI] [PubMed] [Google Scholar]
- 15.Addy M, Langeroudi M. Comparison of the immediate effects on the sub-gingival microflora of acrylic strips containing 40% chlorhexidine, metronidazole or tetracycline. J Clin Periodontol. 1984;11:379–86. doi: 10.1111/j.1600-051x.1984.tb01336.x. [DOI] [PubMed] [Google Scholar]
- 16.Higashi K, Morisaki K, Hayashi S, Kitamura M, Fujimoto N, Kimura S, et al. Local ofloxacin delivery using a controlled-release insert (PT-01) in the human periodontal pocket. J Periodontal Res. 1990;25:1–5. doi: 10.1111/j.1600-0765.1990.tb01201.x. [DOI] [PubMed] [Google Scholar]
- 17.Rams TE, Slots J. Local delivery of antimicrobial agents in the periodontal pocket. Periodontol 2000. 1996;10:139–59. doi: 10.1111/j.1600-0757.1996.tb00072.x. [DOI] [PubMed] [Google Scholar]
- 18.Goodson JM. Pharmcokinetic principles controlling the efficacy of local therapy. J Dent Res. 1989;68:1625–32. [Google Scholar]
- 19.Polson AM, Garrett S, Stoller NH, Bandt CL, Hanes PJ, Killoy WJ, et al. Multi-center comparative evaluation of subgingivally delivered sanguinarine and doxycycline in the treatment of periodontitis. II. Clinical results. J Periodontol. 1997;68:119–26. doi: 10.1902/jop.1997.68.2.119. [DOI] [PubMed] [Google Scholar]
- 20.Williams RC, Paquette DW, Offenbacher S, Adams DF, Armitage GC, Bray K, et al. Treatment of periodontitis by local administration of minocycline microspheres: A controlled trial. J Periodontol. 2001;72:1535–44. doi: 10.1902/jop.2001.72.11.1535. [DOI] [PubMed] [Google Scholar]
- 21.Ainamo J, Lie T, Ellingsen BH, Hansen BF, Johansson LA, Karring T, et al. Clinical responses to subgingival application of a metronidazole 25% gel compared to the effect of subgingival scaling in adult periodontitis. J Clin Periodontol. 1992;19:723–9. doi: 10.1111/j.1600-051x.1992.tb02535.x. [DOI] [PubMed] [Google Scholar]
- 22.Stoltze K. Concentration of metronidazole in periodontal pockets after application of a metronidazole 25% dental gel. J Clin Periodontol. 1992;19:698–701. doi: 10.1111/j.1600-051x.1992.tb02531.x. [DOI] [PubMed] [Google Scholar]
- 23.Stelzel M, Florès-de-Jacoby L. Topical metronidazole application compared with subgingival scaling. A clinical and microbiological study on recall patients. J Clin Periodontol. 1996;23:24–9. doi: 10.1111/j.1600-051x.1996.tb00500.x. [DOI] [PubMed] [Google Scholar]
- 24.Scheie AA, Petersen FC. The biofilm concept: Consequences for future prophylaxis of oral diseases? Crit Rev Oral Biol Med. 2004;15:4–12. doi: 10.1177/154411130401500102. [DOI] [PubMed] [Google Scholar]
- 25.Walker CB, Karpinia K, Baehni P. Chemotherapeutics: Antibiotics and other antimicrobials. Periodontol 2000. 2004;36:146–65. doi: 10.1111/j.1600-0757.2004.03677.x. [DOI] [PubMed] [Google Scholar]
- 26.Griffiths GS, Smart GJ, Bulman JS, Weiss G, Shrowder J, Newman HN. Comparison of clinical outcomes following treatment of chronic adult periodontitis with subgingival scaling or subgingival scaling plus metronidazole gel. J Clin Periodontol. 2000;27:910–7. doi: 10.1034/j.1600-051x.2000.027012910.x. [DOI] [PubMed] [Google Scholar]
- 27.Klinge B, Attström R, Karring T, Kisch J, Lewin B, Stoltze K. 3 regimens of topical metronidazole compared with subgingival scaling on periodontal pathology in adults. J Clin Periodontol. 1992;19:708–14. doi: 10.1111/j.1600-051x.1992.tb02533.x. [DOI] [PubMed] [Google Scholar]
- 28.Johnson LR, Stoller NH, Polson A, Harrold CQ, Ryder M, Garrett S. The effects of subgingival calculus on the clinical outcomes of locally-delivered controlled-release doxycycline compared to scaling and root planing. J Clin Periodontol. 2002;29:87–91. doi: 10.1034/j.1600-051x.2002.290201.x. [DOI] [PubMed] [Google Scholar]
- 29.Offenbacher S. Periodontal diseases: Pathogenesis. Ann Periodontol. 1996;1:821–78. doi: 10.1902/annals.1996.1.1.821. [DOI] [PubMed] [Google Scholar]
- 30.Paquette DW, Hanlon A, Lessem J, Williams RC. Clinical relevance of adjunctive minocycline microspheres in patients with chronic periodontitis: Secondary analysis of a phase 3 trial. J Periodontol. 2004;75:531–6. doi: 10.1902/jop.2004.75.4.531. [DOI] [PubMed] [Google Scholar]


