The prevalence of individuals at high risk or with clinical eating disorders (EDs) on college campuses is high. Often, students are tasked with evaluating the urgency of their needs and knowing when to seek services, which leads to delays in seeking care. Without intervention, symptoms may worsen, resulting in adverse consequences and impaired functioning. As such, early identification and reduced symptom progression for individuals across the risk/clinical continuum of ED psychopathology is urgently needed. However, effective intervention for EDs on the college campus remains a significant challenge. Counseling centers are often understaffed and overburdened, with directors reporting an average student to counselor ratio of 1,900:11. Indeed, less than 20% of students who are screened positive for EDs report receiving treatment.2
The gap in care delivery necessitates research on ways to improve the quality and efficiency of treatment delivery for symptomatic individuals and decrease the number of individuals requiring care. We propose a population-based model, for heuristic purposes, for the identification, prevention, and treatment of EDs, to reduce the incidence and prevalence of EDs on the college campus. A population-based approach allows us to move beyond treating individuals to more broadly intervene with a population, thereby increasing real-world clinical utility of ED interventions and improving the college counseling system of care for EDs.
A Model for Population-based Prevention and Treatment
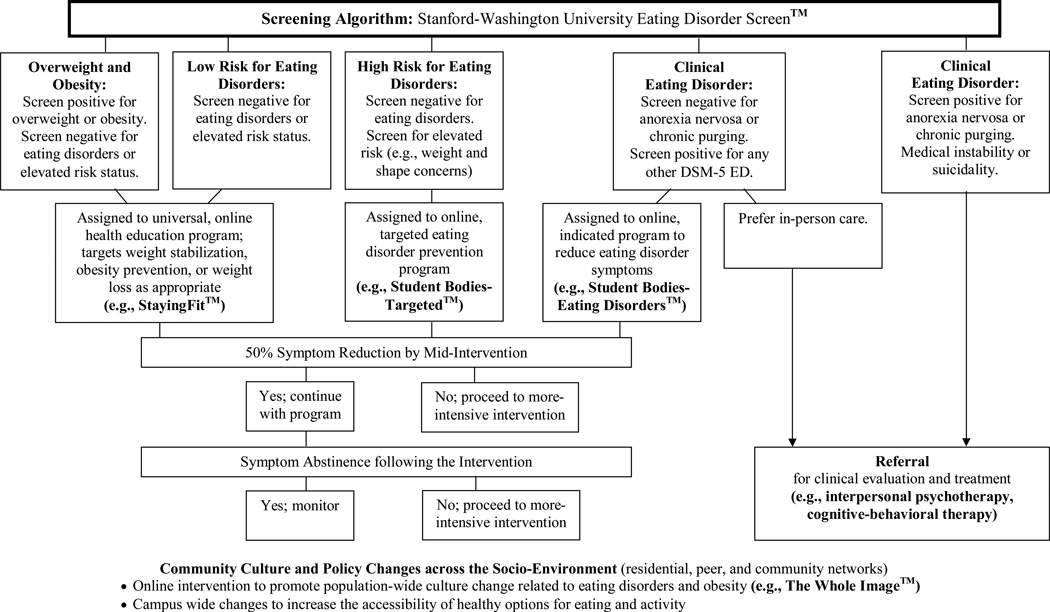
The model is based on foundational research to develop an online screening algorithm and integrate interventions (both preventive and clinical) for ED identification and intervention (excluding anorexia nervosa), and aims to create a synergy between individual-level changes in ED attitudes/behaviors and population-level changes in community and environmental norms around body image and healthy lifestyles. The proposed model involves partnering with college counseling centers and stakeholders to implement: (a) online screening and early identification with in-person follow-up evaluation as needed; (b) tailored, evidence-based interventions, delivered online or in person based on students’ symptoms and via a stepped care approach to conserve resources and reduce cost; (c) ongoing symptom monitoring to maintain intervention gains and triage non-responders or individuals with changes in symptoms to appropriate care; and (d) community culture and policy interventions across the socio-environment to establish community and environmental norms that promote healthful behaviors. (see Figure 1).3
Figure 1.
A Suite of Tailored, Evidence-Based Interventions
Community Culture and Policy Changes across the Socio-Environment (residential, peer, and community networks)
• Online intervention to promote population-wide culture change related to eating disorders and obesity (e.g., The Whole Image™)
• Campus wide changes to increase the accessibility of healthy options for eating and activity
Hypothetically, in a sample of 1,000 female college students, we would anticipate 68–77% would screen as low risk, 20–25% would screen positive for high risk, 2–5% for subclinical, and 1–2% for clinical EDs.3 Programs would then be delivered across the continuum of ED pathology to reduce symptom progression.3 Programs targeted for high risk and subclinical students would reduce ED symptoms, improve weight/shape concerns and drive for thinness, and increase adoption of healthier lifestyles. In this model, individuals identified as low risk or overweight/obese could be offered Staying Fit™ and high risk individuals (but not clinical cases) could be offered Student Bodies–Targeted™ or equally potent, low-cost interventions. Programs for subclinical and clinical students would utilize online or therapist-delivered guided self-help approaches (e.g., Student Bodies–Eating Disorders) before offering evidence-based, in-person interventions (e.g., interpersonal psychotherapy, cognitive-behavioral therapy) to reduce ED symptoms (see Table 1 for an overview of possible interventions and Bauer & Moessner (2013, this volume) for a review of online interventions for eating disorders treatment and prevention4).
Table 1.
Screening algorithm and evidence-based interventions for the identification, prevention, and treatment of eating disorders.
| Component | Features | Main Findings |
|---|---|---|
| Stanford-Washington University ED Screen™ (Algorithm) |
|
Sensitivity and specificity are very high for cases of DSM-IV and DSM-5 EDs (most >0.90). (Trockel M, Weisman H, Kass AE, Iacovino J, Sinton MM, Wilfley DE, et al. Screening and stepped care prevention of eating disorders in emerging adult women, using DSM-IV vs. DSM-5 diagnostic criteria. Under review) |
| Staying Fit™ (Prevention) |
|
Results in increased fruit and vegetable consumption, weight stabilization in normal weight students, and weight loss in overweight students. (Taylor CB, Taylor K, Jones M, Shorter A, Yee M, Genkin B, et al. Obesity Prevention in Defined (High School) Populations. Int J Obesity Suppl, 2012;2: S30–2.) |
| Student Bodies - Targeted™ (Prevention) |
|
Reduces ED risk and prevents ED onset in students most at risk. (Beintner I, Jacobi C, Taylor CB. Effects of an Internet-based prevention programme for eating disorders in the USA and Germany--a meta-analytic review. Eur Eat Disord Rev. 2012;20:1–8.; Taylor CB, Bryson S, Luce KH, Cunning D, Doyle AC, Abascal LB, et al.. Prevention of eating disorders in at-risk college-age women. Arch Gen Psychiatry. 2006;63:881–8) |
| Student Bodies - Eating Disorders™ (Treatment) |
|
Reduces ED symptoms and symptom progression. Program testing underway for clinical EDs. (Jacobi C, Volker U, Trockel MT, Taylor CB. Effects of an Internet-based intervention for subthreshold eating disorders: a randomized controlled trial. Behav Res Ther, 2012; 50:93–9) |
| Interpersonal Psychotherapy (Treatment) |
|
Reduces binge eating and is efficacious for patients with high weight/shape concerns, low self-esteem, negative affect, and frequent binge episodes. (Wilson GT, Wilfley DE, Agras WS, Bryson SW. Psychological treatments of binge eating disorder. Arch Gen Psychiatry. 2010; 67:94–101; Agras WS, Walsh T, Fairburn CG, Wilson GT, Kraemer HC. A multicenter comparison of cognitive-behavioral therapy and interpersonal psychotherapy for bulimia nervosa. Arch Gen Psychiatry. 2000; 57:459–66) |
| Cognitive-Behavioral Therapy (Treatment) |
|
Reduces binge eating and compensatory behaviors. (Mitchell JE, Agras S, Crow S, Halmi K, Fairburn CG, Bryson S, et al. Stepped care and cognitive-behavioural therapy for bulimia nervosa: randomised trial. Br J Psychiatry. 2011;198:391–7) |
| The Whole Image™ (Community Culture Change Intervention) |
|
Reduces weight/shape concerns, negative verbal communication about body image, and thinness ideal beliefs. (Jones M, Kass A, Trockel M, Mazina V, Jacobi C, Wilfley DE, et al. A Universal Screening and Intervention Platform for Eating Disorders on College Campuses: The Healthy Body Image Program. Under review) |
ED=Eating disorder; BMI=Body mass index; BN=Bulimia nervosa; BED=Binge eating disorder
Community culture and policy interventions can establish an environment with cultural norms that promote healthful body image, decreased acceptance of risk behaviors (e.g., binge eating, purging), reduced stigma of EDs and obesity, and enhanced well being (e.g., The Whole Image™; see Table 1). Environmental changes to the quality and availability of food and activity choices on campus can help to make the healthy lifestyle choice the default choice.
Next Steps for Research
This model has potential to achieve the goal of reducing incidence and prevalence of EDs, but we have identified several areas where further evaluation and research is needed.
Evaluating Outcomes
Examination of efficacy of this model is warranted, including demonstration of reduced incidence and prevalence of EDs. We hypothesize that, of the 200–250 students at high risk in a sample of 1,000 females, 10% (i.e., 20–25 people) would likely go on to develop an ED. With preventive intervention, half of these women would likely improve (i.e., 10–12 people) and half (i.e., 10–12 people) would likely progress into the clinical category. Similarly, half of the identified 10–20 clinical cases (i.e., 5–10 people) would likely improve with clinical intervention and half (i.e., 5–10 people) would likely remain symptomatic and require further care. Combined, this would reduce the incidence and prevalence of EDs by 50% over two years. Accordingly, at a university with 40,000 students (~20,000 female), model implementation could effectively eliminate 400 cases of EDs, thereby conserving resources for the remaining ED cases.
Evaluation of model cost-effectiveness may identify ways to reduce costs. Demonstration of cost-savings could help shift the ED care paradigm in the college setting.
Enhancing Intervention Potency
Identification of sub-groups with specialized needs, including characterization of the potentially unique needs of males and non-responders, can facilitate intervention tailoring or more rapid delivery of intensive care.
Detection of sub-populations at elevated risk for relapse (such as whether successfully-treated clinical cases are at higher risk than high-risk individuals without an ED history) can be used to establish targets for tailored maintenance intervention.
Incorporation of modular designs, in which various intervention components are integrated into one platform and provided to patients based on skill/mastery, may improve tailoring.
Use of new trial designs, such as sequential multiple assignment randomized trials and adaptive designs, can allow for simultaneous evaluation of variations of an intervention.
Enhancing Technological Capacity
Inclusion of clinical management “dashboards” (i.e., online tools that allow providers to visually represent both individual and population progress) may facilitate program delivery.
Incorporation of mobile applications may increase intervention potency by providing in-the-moment coaching to reduce urges and improving efficiency of symptom monitoring.
Integration of an online social network with recursive peer incentive strategies may improve environmental and system factors that increase risk.
Translating for Dissemination and Implementation
Use of innovative methods to train providers to competency to deliver in-person and online interventions will improve fidelity. For example, the train-the-trainer method (i.e., training an internal champion who trains others in the organization) may improve sustainability.
Development of new methods for program monitoring will ensure quality of program delivery. Blends of automatic and therapist delivered guidance are needed; tools such as text analysis may help to potentiate automated response systems and improve scale up and reach.
Engagement with the community (e.g., involvement in campus activities) can improve and maintain user and stakeholder investment over time.
Expanding the Model
Evaluation across campuses will inform model fit within the college care system. Ongoing formative evaluation and flexibility for innovation and “exnovation” (i.e., discarding ineffective components that do not fit within the system) can maximize sustainability.
Expansion of the model to integrate data capture and intervention for comorbid disorders (e.g., depression, alcohol use) will lead to a comprehensive system for mental health care.
Formation of a college mental health research network will advance uptake of best practices. Leveraging organizations such as the Association of University and College Counseling Center Directors and the American College Health Association can enhance these efforts.
Summary
Population-based models aim to improve treatment delivery for symptomatic individuals and decrease the number of individuals requiring care. The proposed model has the potential to increase early intervention, reduce costs, and maximize capacity to serve the entire student body, resulting in improvements in students’ overall health and well being, self image, academic performance, and quality of life. Although there is preliminary support for this approach, a programmatic line of research to better inform model implementation including long-term effectiveness and cost-effectiveness is needed. Successful implementation has potential for rapid dissemination to reach the 20 million students enrolled in US colleges and universities.
Acknowledgments
Supported by: R01 MH095748 from the National Institute of Mental Health, R01 MH064153 from the National Institute of Mental Health; R01 MH059303 from the National Institute of Mental Health; R01 MH081125 from the National Institute of Mental Health; T32 HL007456 from the National Heart, Lung, and Blood Institute; and K24 MH070446 from the National Institute of Mental Health.
The authors thank Andrea Kass, Heather Waldron, and Alison Yee for assistance with manuscript preparation, and Andrea Kass, Megan Jones, and Mickey Trockel for assistance with model development and formative evaluation.
References
- 1.Hunt, Eisenberg Mental Health Problems and Help-Seeking Behavior Among College Students. J Adolesc Health. 2010 Jan;46(1):3–10. doi: 10.1016/j.jadohealth.2009.08.008. [DOI] [PubMed] [Google Scholar]
- 2.Eisenberg D, Nicklett EJ, Roeder K, Kirz NE. Eating disorder symptoms among college students: prevalence, persistence, correlates, and treatment-seeking. J Am Coll Health. 2011;59(8):700–707. doi: 10.1080/07448481.2010.546461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jones M, Kass A, Trockel M, Mazina V, Jacobi C, Wilfley DE, et al. A Universal Screening and Intervention Platform for Eating Disorders on College Campuses: The Healthy Body Image Program. J Am Coll Health. doi: 10.1080/07448481.2014.901330. Under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bauer S, Moessner M. Harnessing the Power of Technology for the Treatment and Prevention of Eating Disorders. Int J Eat Disord. 2013 doi: 10.1002/eat.22109. [DOI] [PubMed] [Google Scholar]