Abstract
A key opportunity to reduce HIV transmission lies with healthcare providers counseling HIV-infected patients about safer sex. We audio-recorded and transcribed clinical encounters between 45 healthcare providers and 417 of their HIV-infected patients at four outpatient sites in the United States. We used logistic regressions to evaluate associations between patient and provider characteristics, and the occurrence of discussion (any talk about sex) and counseling (advice about safer sex). Of the 417 encounters, discussion of sex occurred in 187 (45% of encounters, 95% CI: 40–50%). Counseling occurred for 49% (95% CI: 35–63%) of patients reporting unsafe sex. Discussion of sex was more likely with younger or less-educated patients and with less cultural difference between patient and provider, while counseling was associated with greater provider mindfulness and lower provider empathy. These findings suggest targets to improve communication regarding sexual risk reduction in HIV care.
Introduction
In the United States, approximately 1.2 million people are living with HIV, and an estimated 56,000 new infections occur annually.1 The most recent available data suggest sexual transmission accounts for 84% of newly diagnosed HIV infections,2 and unsafe sexual activity is reported by some 11–30% of those with HIV infection.3–5 Fortunately, behavioral interventions are effective in reducing patients' unprotected sexual activities6,7 and in reducing their acquisition of STIs.8 Such promotion of safer sexual behavior by persons who are HIV-positive has the potential to decrease the incidence of HIV and sexually transmitted infections (STIs), and is the basis of efforts targeting “prevention with positives”.9
Guidelines from key institutions (Center for Disease Control, Health Resources and Services Administration, National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America) recommend that healthcare providers routinely discuss high-risk behaviors with their HIV-infected patients, and provide counseling to promote safer sex practices.10 Sexual risk reduction counseling by healthcare providers is feasible to incorporate into clinical settings.11 Although many factors may contribute to the risk of HIV transmission,12–14 some evidence suggests that counseling can play a role in decreasing high-risk behavior by HIV-infected patients.15–18 Although patients reporting unsafe sex are a priority to receive counseling, patients reporting safe behavior may benefit from healthcare providers' reinforcement. Even patients who practice safe sex at one time point are at risk for engaging in unsafe behaviors if followed over time.19
Despite the effectiveness of counseling by healthcare providers to reduce patients' high-risk sexual behaviors, discussion of safer sex does not occur consistently in HIV care. Only 71% of HIV-infected patients report discussing safer sex at least once with their healthcare provider.20 In recalling their most recent visit, 25% of patients discussed safer sex in general and only 6% discussed specific sexual acts.21 Most studies of sexual risk counseling in HIV care have relied on self-report by patient or provider, an approach that may be subject to recall bias. However, one study by Laws et al. (2010) audio-recorded 116 HIV clinic visits in Boston, MA, and found only 17 included any discussion of sex or STIs (i.e., about 10% of visits).22
Using direct observation of clinical encounters in four cities across the United States, we assessed how often healthcare providers discuss high-risk sexual behavior with their HIV-infected patients, how often counseling is given regarding risk reduction, and characteristics associated with the occurrence of such discussion and counseling.
Methods
Study design
We used a mixed methods design to analyze cross-sectional data from the Enhancing Communication and HIV Outcomes (ECHO) Study, which was originally designed to assess racial/ethnic disparities in patient–provider communication.23–28 Data were collected between December 2004 and January 2006, for patients and providers at four large, urban, academic outpatient clinic sites in Baltimore, Maryland; New York, New York; Detroit, Michigan; and Portland, Oregon, USA. Institutional Review Board approval was obtained at each site.
Eligible patients were 19 years or older, English-speaking, living with HIV, and had had at least one prior visit with their provider. Of the 599 patients approached for enrollment, 437 (73%) agreed to participate. Primary reasons for refusal were time constraints, not feeling well, or lack of interest.
Eligible providers were physicians, physicians' assistants, and nurse practitioners delivering care to patients at the study sites. Of the 55 eligible providers, 45 (82%) agreed to participate. Reasons for refusal were discomfort with audio-recording, and time constraints. Of the 435 total encounters, 18 were excluded due to lack of usable audio-recording; thus we had a total of 417 encounters available for study. Each patient–provider pair had one recorded encounter. The observed health care visits were routine HIV care visits with the patient's usual care provider. Visits for acute/urgent care were not included in the study.
Data collection
Data collection methods for the ECHO study have previously been described.23–27 After giving informed consent, participating providers completed questionnaires. Research assistants approached consecutive patients of participating providers in the clinic waiting rooms. Participants were informed that this study was examining patient–provider communication in general, not any particular topic of discussion. Thus, they were not prompted in any way to focus on sexual behavior. After obtaining informed consent from eligible patients, research assistants placed digital audio-recording devices in the exam rooms to record the encounter. After the clinic visit, patients were interviewed by research assistants.
Patient interview and provider questionnaire variables
Patient interviews assessed demographics, whether patients were receiving antiretroviral therapy, the length of the patient–provider relationship, and patients' perceptions of cultural dissimilarity with their providers.26,28 The cultural dissimilarity scale asked each member of the patient–provider pair to rate how similar they were on race, ethnicity, culture, skin color, values, beliefs, styles of speech and reasoning, and was reported from 1 (very similar) to 6 (very dissimilar).
Providers received two questionnaires, one at baseline and one post-visit. The providers' baseline questionnaires assessed demographics, clinician type, and measures of mindfulness29 and empathy.30 Mindfulness measured the providers' self-reported ability to be present in the moment, attentive and undistracted, and was reported as a summary score from 1 (low) to 6 (high). Empathy measured providers' self-reported sensitivity to the feelings and perspectives of others, and was reported as a summary score from 1 (low) to 5 (high).
The providers' post-visit questionnaires assessed cultural dissimilarity between the provider and the patient, and provider's rating of how busy the clinic schedule was on the visit day.
These patient, provider, and relationship variables were chosen for inclusion in the analysis because we hypothesized that they might be associated with patient–provider discussion about sexual behavior or counseling about sexual risk reduction.
Dialogue classification
The audio-recorded clinical encounters were transcribed by a professional transcription service, and then checked for accuracy by trained research assistants. We searched the 417 transcripts for key words and text strings relating to sexual activity and STIs (e.g., “sex”, “condom”, “herpes”) comparable to previously used search strategies.22 All transcripts selected by electronic search were read by one coder to verify that dialogue was relevant to sexual risk behavior. A random sample of 20% of the remaining transcripts was read by a second coder to verify that relevant dialogue had not been missed by the electronic search.
The outcome of “discussion” was defined as any exchange of dialogue between the patient and provider on a topic related to sexual activity. The topic could be initiated by either the patient or the provider. We sought to capture whether sex was brought up at all in the encounter. We further classified these dialogues according to content from a patient-focused standpoint into one of four mutually-exclusive categories: patient denies sexual activity, patient reports safe sex, patient reports unsafe sex, or patient gives unclear indication regarding whether sex was safe. Safe sex was defined as any practice to reduce risk of HIV or STI transmission, including consistent condom use, low-risk partners (reducing number of partners, monogamy, or abstinence), and disclosure of HIV status to current or prospective partners. Indications of unsafe sex included patient reports of STI diagnosis or treatment, unprotected sexual exposure, high-risk partners (new or multiple), or nondisclosure of HIV status.
The safety of sex was classified as unclear if the discussion involved routine STI screening, ambiguous STI symptoms (for example, a lesion or discharge for which the provider considered an STI but ultimately stated that a nonsexual explanation was more probable or herpes or warts that were not specified as genital), or references to sexual behaviors with unclear safety details (for example, the patient mentioned a sexual partner but did not specify whether they were monogamous, or patient requests for erectile dysfunction medications).
We further classified encounters according to whether sexual risk reduction counseling occurred. In counseling encounters, the provider specifically addressed the patient's sexual risk behavior by either reinforcing safe sex practices or encouraging a change in behavior toward safer practices. In missed counseling opportunity encounters, the provider did not specifically address the patient's sexual risk behavior.
A random sample of 20% of the classified encounters was rechecked by a second coder. Disagreements in classification (found in five encounters) were resolved through consensus. No disagreements occurred regarding whether counseling was coded. The disagreements were mostly around the distinction between the patient's denial of sexual activity and the patient reporting safe sex by choosing abstinence. Our consensus, after discovering that reviewers were classifying this scenario differently, was to classify as “denial” any brief exchange in which the patient denied sexual activity with no further information and to classify as “safe sex” any exchange in which the patient indicated choosing not to have sex in order to decrease risk.
Analysis of characteristics associated with dialogue
We coded encounters to create two dichotomous outcome variables: discussion related to sexual risk behavior (or not), and counseling regarding sexual behavior (or not). After content coding was complete, we transformed the data into counts that could then be analyzed quantitatively. We analyzed independent variables from the patient interviews, provider questionnaires, and clinical data, for association with these outcomes from the content coding. We created variables for gender concordance and age concordance (patient and provider of same age within 10 years). There were insufficient numbers of race concordant patient-provider pairs for meaningful comparison; therefore, no variable for race concordance was used in the analysis.
For descriptive statistics of the sample, we performed t-tests for continuous variables, and chi-squared tests for categorical variables, to investigate associations between the patient, provider, and relationship variables, and encounters with or without discussion of sex. The unit of analysis for evaluation was the encounter, which included a patient–provider dyad.
We performed bivariate logistic regressions using discussion and counseling as two dichotomous outcomes, and the patient, provider, and relationship factors as covariates. We used generalized estimating equations (GEE) with robust variance to account for clustering of patients within providers, and adjusted for practice site as an indicator variable. In multivariable logistic regressions, we created fully adjusted models containing all patient, provider, and relationship variables. All statistical analyses were performed using STATA 11 (College Station, TX: StataCorp).
Cultural dissimilarity by patient rating and provider rating were moderately correlated. The adjusted models were run using provider rating, and then repeated using patient rating to confirm that similar results were obtained. The adjusted models were checked using Hosmer-Lemershow goodness-of-fit tests and using multiple imputation methods to account for missing covariate data. Only 9% of observations contained any missing data, and imputation did not significantly change the results of the logistic regressions.
Results
Participant characteristics
The distribution of patient, provider, and relationship characteristics in the entire sample, and by whether discussion of sex occurred in the encounter, are shown in Table 1. Patients were predominantly male and non-white, while providers were predominantly female and white. About 60% of the patient–provider pairs had age concordance and about half had gender concordance.
Table 1.
Patient, Provider, and Relationship Characteristics Presented for Entire Sample, and by Whether Sexual Topic Was, or Was Not, Discussed During Clinic Visit
| Entire sample (N=417) | Sexual topic discussed (N=187) | Sexual topic not discussed (N=230) | p Valuea<0.05* | |
|---|---|---|---|---|
| Patient characteristics | ||||
| Age in years, mean (SD) | 45.3 (9.5) | 43.5 (0.7) | 46.8 (0.6) | 0.0003* |
| Sex, % female | 34 | 34 | 34 | 0.967 |
| Race, % white | 23 | 24 | 21 | 0.661 |
| % with high school degree | 72 | 68 | 75 | 0.091 |
| % on anti-retroviral therapy | 78 | 77 | 79 | 0.516 |
| Viral load, %<75 copies/ml | 48 | 47 | 49 | 0.705 |
| Provider characteristics | ||||
| Age in years, mean (SD) | 44.5 (8.2) | 44.9 (0.6) | 44.2 (0.5) | 0.335 |
| Sex, % female | 57 | 60 | 55 | 0.334 |
| Race, % white | 71 | 73 | 69 | 0.261 |
| Training, % physician | 73 | 72 | 74 | 0.580 |
| Empathy, mean (SD) | 4.1 (0.5) | 4.1 (0.03) | 4.1 (0.03) | 0.650 |
| Mindfulness, mean (SD) | 4.3 (0.8) | 4.3 (0.05) | 4.3 (0.05) | 0.951 |
| % with busier schedule than usual | 35 | 33 | 37 | 0.477 |
| Relationship characteristics | ||||
| % Known provider>5 years | 33 | 28 | 38 | 0.033* |
| % Age concordant | 61 | 64 | 59 | 0.240 |
| % Gender concordant | 52 | 51 | 53 | 0.661 |
| Cultural dissimilarity: Patient rating, mean (SD) | 3.3 (1.2) | 3.1 (0.09) | 3.4 (0.07) | 0.034* |
| Provider rating, mean (SD) | 3.8 (1.1) | 3.7 (0.08) | 3.9 (0.07) | 0.021* |
Descriptive statistics and p values calculated using t-tests for continuous variables, and chi-squared tests for categorical variables.
Discussion of sex
Of the 417 encounters in which dialogue was analyzed, 187 included discussion of a sexual topic (45% of encounters, 95% CI: 40–50%). There were significant differences in three participant characteristics between those clinical encounters in which sex was discussed compared to those in which it was not: in the former, (1) patients were younger (mean age 43.5 vs. 46.8 years), (2) the patient–provider relationship was shorter (28% vs. 38% had known each other for greater than 5 years, and (3) cultural dissimilarity was lower (mean 3.7 vs. 3.9 by provider rating).
Content analysis of the dialogues showed that, in 30 of the 187 encounters, the discussion was limited to a brief denial by the patient of sexual activity. In the remaining 157 encounters, 66 patients (42%) reported engaging in sexual activity with one or more safe sex practices, 53 patients (34%) gave an indication of unsafe sexual behavior, and for 38 patients (24%) the safety of sexual behavior was unclear. Sample quotes from the dialogues in each of these categories are given in Table 2. The most commonly reported safe sex practices were consistent condom use (n=56 encounters), low-risk partners (n=20), and disclosure of HIV status to partners (n=17). The most common indications of unsafe sexual behavior were patient report of unprotected sexual exposure (n=35), followed by high-risk partners (n=21), STI symptoms or diagnosis (n=18), and nondisclosure of HIV status (n=12).
Table 2.
Examples from Dialogues of Discussion and Counseling Regarding Sexual Behavior
|
Category |
Sexual topic discussed |
|||
|---|---|---|---|---|
| Subcategory | Brief denial of sexual activity | Safety of sex unclear | Indication of unsafe sex | Indication of safe sex |
| Example |
D: Okay. And are you currently sexually active? P: No, I'm not. D: Okay. |
D: So are you seeing anybody? P: As a relationship? D: As a relationship, yeah. P: Well I have a friend. I see him off and on. D: Right, right. P: I'm sexually active, if that's the answer. D: Any questions about what you're doing or what any of that? P: No. I mean the only problem I – I keep getting this rash. |
P: I slept with someone I shouldn't have, cuz I wasn't safe, and they were positive, so. D: And when was that? P: Um I didn't tell you last time I saw you, but it was right before I saw you last time. D: All right, so we saw each other- P: Last month. D: So when you were saying you didn't use a condom, was that for both insertive and receptive? P: Yeah. |
D: You guys using safe sex? P: Always have. D: Condoms? P: Yeah, right D: Every time, right? P: Every time. D: What's her status? Is she positive? P: Uh, negative. Been together for four years. |
|
Category |
Counseling regarding sexual behavior |
|
|---|---|---|
| Subcategory | Counseling occurred | Missed opportunity for counseling |
| Example |
D: Are you sexually active? P: Yeah, I'm still with her dad every now and then. Every now and then. D: You guys use condoms? P: Sometimes. D: That's important. P: I know. I tell him that. I tell him and then – well you know how it is. [laughs] D: I know, and it's fine, it's – you want to protect yourself, too. P: Right. D: You don't want to end up with something else. P: Right. |
D: So we're gonna swab your throat, okay? P: Don't they have to swab everything? [Laughs]. D: Not if you didn't have anal sex, we don't. But if you did, we do. P: I just think the whole thing wouldn't hurt. D: OK. |
D, Provider speech; P, Patient speech.
Counseling about sexual behavior
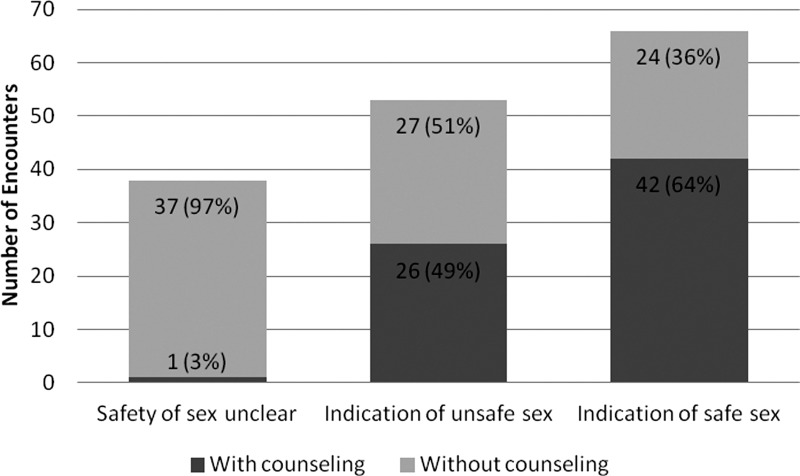
Counseling about sexual risk behavior was found in 69 out of 157 dialogues (44%). Table 2 gives sample quotes from the dialogues in which counseling occurred and in which an opportunity for counseling was missed. As shown in Fig. 1, counseling occurred in 42 of 66 encounters (64%) in which the patient reported safe sex, in 26 of 53 encounters (49%) in which the patient gave an indication of unsafe sex, and in 1 of 38 encounters (3%) in which the safety of the patient's sexual behavior was unclear.
FIG. 1.
Number of encounters in which patients gave indications of safe, unsafe, or unclear sexual behavior and received counseling from providers regarding risk reduction.
Patient, provider, and relationship factors associated with discussion
The unadjusted and adjusted odds ratios of the patient, provider, and relationship characteristics on the occurrence of discussion of sex are shown in Table 3. In adjusted logistic regressions, the odds of discussion of sex were lower for older patients (OR: 0.96, 95% CI: 0.94–0.99), and for more culturally dissimilar patient–provider pairs (OR: 0.64, 95% CI: 0.47–0.86). Length of patient–provider relationship was no longer significant in the fully adjusted model. The level of patient education was significant, showing lower odds of discussion of sex with patients who completed high school versus those who did not (OR: 0.57, 95% CI: 0.36–0.91).
Table 3.
Odds Ratios for Patient, Provider, and Relationship Variables on Discussion of Sexual Topic (n=417)
| |
Unadjusteda |
Adjustedb |
||
|---|---|---|---|---|
| Odds ratio (95% CI) | p Value<0.05* | Odds ratio (95% CI) | p Value<0.05* | |
| Patient characteristics | ||||
| Age in years | 0.96 (0.94–0.98) | 0.001* | 0.96 (0.94–0.99) | 0.002* |
| Male sex | 1.01 (0.59–1.72) | 0.978 | 1.00 (0.64–2.02) | 0.863 |
| Race (ref: white) | 1.00 | 0.718 | 1.00 | 0.230 |
| Non-Hispanic black | 0.86 (0.50–1.48) | 1.56 (0.79–3.08) | ||
| Hispanic/Latino | 0.73 (0.36–1.48) | 1.11 (0.50–2.49) | ||
| Other | 0.62 (0.36–1.58) | 0.80 (0.26–2.46) | ||
| With high school degree | 0.70 (0.48–1.00) | 0.052 | 0.57 (0.36–0.91) | 0.019* |
| On anti-retroviral therapy | 0.86 (0.58–1.26) | 0.430 | 1.06 (0.58–1.97) | 0.841 |
| Viral load<75 copies/mL | 0.93 (0.67–1.29) | 0.664 | 1.03 (0.70–1.50) | 0.898 |
| Provider characteristics | ||||
| Age in years | 1.01 (0.97–1.04) | 0.730 | 1.00 (0.97–1.04) | 0.863 |
| Male sex | 0.74 (0.43–1.28) | 0.287 | 0.62 (0.28–1.35) | 0.229 |
| Race (ref: white) | 1.00 | 0.133 | 1.00 | 0.268 |
| Black or Latino | 1.04 (0.22–4.82) | 0.39 (0.09–1.80) | ||
| Asian | 0.61 (0.37–1.01) | 0.67 (0.34–1.34) | ||
| Training (physician) | 0.82 (0.43–1.58) | 0.555 | 0.79 (0.41–1.52) | 0.473 |
| Empathy | 0.90 (0.51–1.58) | 0.702 | 0.71 (0.39–1.31) | 0.278 |
| Mindfulness | 0.98 (0.65–1.48) | 0.934 | 1.02 (0.58–1.77) | 0.956 |
| Busier schedule than usual | 0.86 (0.51–1.45) | 0.570 | 0.78 (0.46–1.33) | 0.362 |
| Relationship characteristics | ||||
| Known provider>5 years | 0.60 (0.38–0.93) | 0.023* | 0.65 (0.41–1.01) | 0.057 |
| Age concordant | 1.26 (0.84–1.89) | 0.263 | 1.22 (0.80–1.87) | 0.362 |
| Gender concordant | 0.92 (0.55–1.54) | 0.756 | 1.23 (0.68–2.22) | 0.499 |
| Cultural dissimilarityc | ||||
| Higher patient rating | 0.81 (0.69–0.97) | 0.018* | 0.75 (0.59–0.95) | 0.018* |
| Higher provider rating | 0.78 (0.64–0.96) | 0.017* | 0.64 (0.47–0.86) | 0.003* |
CI, confidence interval.
Odds ratios, confidence intervals, and p values obtained using bivariate logistic regressions for each independent variable with generalized estimating equations to account for clustering of patients within providers, adjusted for practice site. bOdds ratios, confidence intervals, and p values obtained using multivariable logistic regressions with generalized estimating equations to account for clustering of patients within providers, adjusted for practice site and all independent variables. cValues reported for multivariable model using provider rating; patient rating run separately.
Patient, provider, and relationship factors associated with counseling
The unadjusted and adjusted odds ratios of the patient, provider, and relationship characteristics on the occurrence of counseling regarding sexual behavior are shown in Table 4. In the adjusted model, the odds of counseling regarding sexual behavior were higher with providers who had higher levels of mindfulness (OR: 3.15, 95% CI: 1.04–9.54), and lower levels of empathy (OR: 0.14, 95% CI: 0.03–0.78).
Table 4.
Odds Ratios for Patient, Provider, and Relationship Variables on Counseling Regarding Sexual Behavior (n=157)
| |
Unadjusteda |
Adjustedb |
||
|---|---|---|---|---|
| Odds ratio (95% CI) | p Value<0.05* | Odds ratio (95% CI) | p Value<0.05* | |
| Patient characteristics | ||||
| Age in years | 0.99 (0.95–1.03) | 0.541 | 0.97 (0.92–1.01) | 0.164 |
| Male sex | 1.28 (0.66–2.51) | 0.466 | 1.81 (0.72–4.50) | 0.206 |
| Race (ref: white) | 1.00 | 0.282 | 1.00 | 0.084 |
| Non-Hispanic black | 2.06 (0.88–4.83) | 2.11 (0.74–6.06) | ||
| Hispanic/Latino | 2.47 (0.65–9.31) | 2.69 (0.40–17.95) | ||
| Other | 2.82 (0.46–17.28) | 13.40 (1.31–137.36) | ||
| With high school degree | 1.24 (0.57–8.49) | 0.590 | 1.60 (0.56–4.62) | 0.382 |
| On anti-retroviral therapy | 0.77 (0.37–1.61) | 0.489 | 1.01 (0.35–2.94) | 0.983 |
| Viral load<75 copies/mL | 1.67 (0.91–3.06) | 0.097 | 1.50 (0.62–3.61) | 0.371 |
| Provider characteristics | ||||
| Age in years | 1.05 (1.00–3.45) | 0.061 | 1.04 (0.96–1.34) | 0.310 |
| Male sex | 1.73 (0.80–3.73) | 0.160 | 1.85 (0.59–5.82) | 0.294 |
| Race (ref: white) | 1.00 | 0.879 | 1.00 | 0.157 |
| Black or Latino | 0.65 (0.09–4.90) | 0.26 (0.03–2.63) | ||
| Asian | 1.11 (0.39–3.12) | 1.49 (0.37–5.95) | ||
| Training (physician) | 0.69 (0.26–1.79) | 0.440 | 1.96 (0.49–7.92) | 0.343 |
| Empathy | 0.42 (0.16–1.06) | 0.065 | 0.14 (0.026–0.78) | 0.025* |
| Mindfulness | 1.36 (0.76–2.45) | 0.306 | 3.15 (1.04–9.54) | 0.042* |
| Busier schedule than usual | 0.83 (0.39–1.77) | 0.629 | 0.68 (0.25–1.86) | 0.453 |
| Relationship characteristics | ||||
| Known provider>5 yrs | 1.73 (0.80–3.75) | 0.163 | 1.66 (0.56–4.90) | 0.356 |
| Age concordant | 1.57 (0.71–3.45) | 0.261 | 1.60 (0.61–4.01) | 0.357 |
| Gender concordant | 1.07 (0.57–2.01) | 0.835 | 1.22 (0.64–2.33) | 0.558 |
| Cultural dissimilarityc | ||||
| Higher patient rating | 1.16 (0.85–1.58) | 0.343 | 1.09 (0.69–1.74) | 0.707 |
| Higher provider rating | 1.21 (0.85–1.71) | 0.294 | 1.16 (0.73–1.86) | 0.525 |
CI, confidence interval.
Odds ratios, confidence intervals, and p values obtained using bivariate logistic regressions for each independent variable with generalized estimating equations to account for clustering of patients within providers, adjusted for practice site. bOdds ratios, confidence intervals, and p values obtained using multivariable logistic regressions with generalized estimating equations to account for clustering of patients within providers, adjusted for practice site and all independent variables. cValues reported for multivariable model using patient rating; provider rating run separately.
Discussion
This is the first large, multi-center study to use direct observation of audio-recorded clinical encounters between HIV-infected patients and their healthcare providers to investigate the frequency and correlates of discussion of sex and counseling regarding sexual risk reduction. We found that just fewer than half of clinical encounters included discussion relevant to sex. Of particular note, during these encounters, and even when patients described unsafe sex, providers tended to miss opportunities for risk reduction counseling. Finally, we found that some patient, provider, and relationship factors were related to the presence of discussion and counseling, and this knowledge may help guide interventions to improve care quality.
In our study, counseling to reduce risk behavior occurred in just half of encounters in which the patient reported unsafe sex. Despite evidence that sexual risk reduction counseling is effective, studies of physician attitudes show a lack of self-efficacy in talking to patients about behavior change.31,32 Physicians also cite discomfort with sexual topics, time constraints, concerns about state reporting requirements, and perceived risk of harming their relationships with patients as barriers.33 Unfortunately, this discomfort may be creating a deficit in the quality of healthcare provided.
However, we found that counseling was more likely to be given by providers with higher versus lower levels of mindfulness. Mindfulness can be beneficial in several aspects of providers' practice, including clinical accuracy, effectively handling emotions, and dealing with stress.34 In addition, mindfulness may help providers to relate better to patients, in identifying psychosocial concerns and being attuned to the patients' perspective.35 Mindfulness can be improved in healthcare providers through several methods, including self-awareness exercises, reflection, and discussion of clinical experiences.36 In our study, providers with higher mindfulness may have given more counseling because they were better able to pick up cues in the conversation that counseling was indicated, or may have been more aware of and better able to deal with their own emotional response to the situation. Interventions to enhance mindfulness may help providers to recognize opportunities for counseling during clinic visits.
We also found that counseling regarding patients' sexual behavior was more likely to be given by providers with lower versus higher levels of self-reported empathy. The inverse relationship between empathy and counseling may appear counterintuitive, since empathy is usually considered a favorable quality in forming patient–provider relationships. However, empathy could also make providers more sensitive to patients' discomfort in awkward conversations,37 and prevent providers from offering patients advice on their behavior because of reluctance to cause offense. Prior qualitative studies have shown providers' fears of harming their relationships with patients to be a barrier to counseling about sexual risk reduction.33 However, it may be possible to overcome some provider discomfort with such discussion through improved self-awareness and education in effective, non-judgmental communication techniques.
In our study, having a discussion related to sex in the first place was more likely to occur with younger versus older patients and patients with lower versus higher levels of education. Prior studies have shown higher rates of STIs among younger versus older HIV-infected patients.38–40 Lower educational status has been associated with higher rates of unsafe sexual behavior41,42 and STI incidence.43,44 Healthcare providers may be more likely to discuss sexual topics with younger and less educated patients because they perceive these groups to be at higher risk of unsafe sexual behavior, HIV transmission, and STI acquisition; however it is important to remember that older and more educated patients may be at risk as well.
Discussion was also more likely to occur when patients and providers perceived themselves to be more culturally similar to each other, than when there was perceived cultural dissimilarity. This is a new finding, which has not previously been evaluated in analysis of sexual risk discussion. An association was seen even after adjusting for age, gender, and race. In our sample, most providers were white and most patients were non-white. Therefore, it was not possible to compare potential differences between white provider/non-white patient pairs and non-white provider/white patient pairs in ratings of cultural dissimilarity. The construct of cultural dissimilarity includes domains of race, ethnicity, and skin color, but also captures other dimensions of values, beliefs, styles of speaking and reasoning, and may be a broader measure of perceived interpersonal differences than race alone. Although one's culture of origin is fixed, competence in cross-cultural communication may be learned.45,46 Finding ways to bridge cultural gaps may help providers discuss sensitive subjects with patients.47–50
Several limitations of this study should be considered. (1) Only one encounter was recorded for each patient–provider pair. Thus we do not know whether sexual behavior was discussed in a previous clinic visit, or what the relationship was between counseling and subsequent sexual behavior. (2) Selection bias may have been present if the patients and providers in our study were not representative of their peers, though this risk was likely reduced by high rates of patient and provider participation. (3) Generalizability may be limited by the fact that only HIV clinics in urban settings were included and all participants were engaged in ongoing care.
In this, the largest direct-observation study to analyze communication about sexual behavior between HIV-infected patients and their healthcare providers, we demonstrate that providers often miss opportunities to discuss sexual behavior and to counsel their patients about sexual risk reduction. Training of HIV care providers can improve both the frequency and quality of prevention counseling.51–53 Our findings suggest that training interventions that also target providers' mindfulness or their ability to bridge cultural differences may be helpful in overcoming potential barriers to addressing high-risk sexual behavior in clinic settings. Further exploration of the roles of cultural dissimilarity, mindfulness, and empathy in patient–provider dialogue regarding sexual behavior is essential, as they offer targets for future interventions to improve risk reduction counseling, with the ultimate goal of improving sexual health for HIV-infected patients, and reducing transmission of STIs and HIV. Improving safer sex counseling, particularly for these high-risk patients, also represents an important goal in decreasing the spread of HIV.
Acknowledgments
The authors thank Dr. Sarah Poynton for assistance with manuscript preparation. This research was supported by a contract from the Health Resources Service Administration and the Agency for Healthcare Research and Quality (AHRQ 290-01-0012). In addition, Dr. Flickinger was supported by the National Institutes of Health (5 T32 HL007180-35), Dr. Berry was supported by the National Institute of Allergy and Infectious Disease (K23 AI084854), Dr. Korthuis was supported by the National Institute of Drug Abuse (K23 DA019809), Dr. Saha was supported by the Department of Veterans Affairs, Dr. Beach was supported by the Agency for Healthcare Research and Quality (K08 HS013903-05), and both Drs. Beach and Saha were supported by Robert Wood Johnson Generalist Physician Faculty Scholars Awards. None of the funders had a role in the design and conduct of this analysis, nor was it subject to their final approval.
Author Disclosure Statement
None of the authors have any relevant financial conflicts of interest.
References
- 1.Hall HI. Song R. Rhodes P, et al. Estimation of HIV incidence in the United States. JAMA. 2008;300:520–529. doi: 10.1001/jama.300.5.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. HIV prevalence estimates—US, 2006. MMWR. 2008;57:1073–1076. [Google Scholar]
- 3.Metsch LR. Pereyra M. Messinger S, et al. HIV transmission risk behaviors among HIV-infected persons who are successfully linked to care. Clin Infect Dis. 2008;47:577–584. doi: 10.1086/590153. [DOI] [PubMed] [Google Scholar]
- 4.Morin SF. Myers JJ. Shade SB, et al. Predicting HIV transmission risk among HIV-infected patients seen in clinical settings. AIDS Behav. 2007;11:S6–16. doi: 10.1007/s10461-007-9253-4. [DOI] [PubMed] [Google Scholar]
- 5.Crepaz N. Marks G. Liau A, et al. Prevalence of unprotected anal intercourse among HIV-diagnosed MSM in the United States: A meta-analysis. AIDS. 2009;23:1617–1629. doi: 10.1097/QAD.0b013e32832effae. [DOI] [PubMed] [Google Scholar]
- 6.Johnson WD. Diaz RM. Flanders WD, et al. Behavioral interventions to reduce risk for sexual transmission of HIV among men who have sex with men. Cochrane Database Syst Rev. 2008:CD001230. doi: 10.1002/14651858.CD001230.pub2. [DOI] [PubMed] [Google Scholar]
- 7.Darbes L. Crepaz N. Lyles C, et al. The efficacy of behavioral interventions in reducing HIV risk behaviors and incident sexually transmitted diseases in heterosexual African Americans. AIDS. 2008;22:1177–1194. doi: 10.1097/QAD.0b013e3282ff624e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Crepaz N. Horn AK. Rama SM, et al. The efficacy of behavioral interventions in reducing HIV risk sex behaviors and incident sexually transmitted disease in black and Hispanic sexually transmitted disease clinic patients in the United States: A meta-analytic review. Sex Transm Dis. 2007;34:319–332. doi: 10.1097/01.olq.0000240342.12960.73. [DOI] [PubMed] [Google Scholar]
- 9.Fisher JD. Smith L. Secondary prevention of HIV infection: The current state of prevention for positives. Curr Opin HIV AIDS. 2009;4:279–287. doi: 10.1097/COH.0b013e32832c7ce5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention (CDC), Health Resources and Services Administration, National Institutes of Health, et al. Incorporating HIV prevention into the medical care of persons living with HIV. Recommendations of CDC, the Health Resources and Services Administration, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. MMWR Recomm Rep. 2003;52:1–24. [PubMed] [Google Scholar]
- 11.Patel SN. Golin CE. Marks G, et al. Delivery of an HIV prevention counseling program in an infectious diseases clinic: Implementation process and lessons learned. AIDS Patient Care STDS. 2009;23:433–441. doi: 10.1089/apc.2008.0189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beidas RS. Birkett M. Newcomb ME. Mustanski B. Do psychiatric disorders moderate the relationship between psychological distress and sexual risk-taking behaviors in young men who have sex with men? A longitudinal perspective. AIDS Patient Care STDS. 2012;26:366–374. doi: 10.1089/apc.2011.0418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mimiaga MJ. Reisner SL. Pantalone DW. O'Cleirigh C. Mayer KH. Safren SA. A pilot trial of integrated behavioral activation and sexual risk reduction counseling for HIV-uninfected men who have sex with men abusing crystal methamphetamine. AIDS Patient Care STDS. 2012;26:681–693. doi: 10.1089/apc.2012.0216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.VanDevanter N. Duncan A. Burrell-Piggott T, et al. The influence of substance use, social sexual environment, psychosocial factors, and partner characteristics on high-risk sexual behavior among young black and Latino men who have sex with men living with HIV: A qualitative study. AIDS Patient Care STDS. 2011;25:113–121. doi: 10.1089/apc.2010.0100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Myers JJ. Shade SB. Rose CD, et al. Interventions delivered in clinical settings are effective in reducing risk of HIV transmission among people living with HIV: Results from the Health Resources and Services Administration (HRSA)'s Special Projects of National Significance initiative. AIDS Behav. 2010;14:483–492. doi: 10.1007/s10461-010-9679-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Richardson JL. Milam J. McCutchan A, et al. Effect of brief safer-sex counseling by medical providers to HIV-1 seropositive patients: A multi-clinic assessment. AIDS. 2004;18:1179–1186. doi: 10.1097/00002030-200405210-00011. [DOI] [PubMed] [Google Scholar]
- 17.Fisher JD. Fisher WA. Cornman DH, et al. Clinician-delivered intervention during routine clinical care reduces unprotected sexual behavior among HIV-infected patients. J Acquir Immune Defic Syndr. 2006;41:44–52. doi: 10.1097/01.qai.0000192000.15777.5c. [DOI] [PubMed] [Google Scholar]
- 18.Patel P. Bush T. Mayer K, et al. Routine brief risk-reduction counseling with biannual STD testing reduces STD incidence among HIV-infected men who have sex with men in care. Sex Transm Dis. 2012;39:470–474. doi: 10.1097/OLQ.0b013e31824b3110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ferrer RA. Amico KR. Bryan A, et al. Accuracy of the stages of change algorithm: Sexual risk reported in the maintenance stage of change. Prev Sci. 2009;10:13–21. doi: 10.1007/s11121-008-0108-7. [DOI] [PubMed] [Google Scholar]
- 20.Marks G. Richardson JL. Crepaz N, et al. Are HIV care providers talking with patients about safer sex and disclosure?: A multi-clinic assessment. AIDS. 2002;16:1953–1957. doi: 10.1097/00002030-200209270-00013. [DOI] [PubMed] [Google Scholar]
- 21.Morin SF. Koester KA. Steward WT, et al. Missed opportunities: Prevention with HIV-infected patients in clinical care settings. J Acquir Immune Defic Syndr. 2004;36:960–966. doi: 10.1097/00126334-200408010-00010. [DOI] [PubMed] [Google Scholar]
- 22.Laws MB. Bradshaw YS. Safren SA, et al. Discussion of sexual risk behavior in HIV care is infrequent and appears ineffectual: A mixed methods study. AIDS Behav. 2011;15:812–822. doi: 10.1007/s10461-010-9844-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Beach MC. Saha S. Korthuis PT, et al. Differences in patient-provider communication for Hispanic compared to non-Hispanic white patients in HIV care. J Gen Intern Med. 2010;25:682–687. doi: 10.1007/s11606-010-1310-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Beach MC. Saha S. Korthuis PT, et al. Patient-provider communication differs for black compared to white HIV-infected patients. AIDS Behav. 2011;15:805–811. doi: 10.1007/s10461-009-9664-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Korthuis PT. Saha S. Chander G, et al. Substance use and the quality of patient-provider communication in HIV clinics. AIDS Behav. 2011;15:832–841. doi: 10.1007/s10461-010-9779-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Saha S. Sanders DS. Korthuis PT, et al. The role of cultural distance between patient and provider in explaining racial/ethnic disparities in HIV care. Patient Educ Couns. 2011;85:e278–284. doi: 10.1016/j.pec.2011.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kinsman H. Roter D. Berkenblit G, et al. “We'll do this together”: The role of the first person plural in fostering partnership in patient-physician relationships. J Gen Intern Med. 2010;25:186–193. doi: 10.1007/s11606-009-1178-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Street RL., Jr. O'Malley KJ. Cooper LA, et al. Understanding concordance in patient-physician relationships: Personal and ethnic dimensions of shared identity. Ann Fam Med. 2008;6:198–205. doi: 10.1370/afm.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brown KW. Ryan RM. The benefits of being present: Mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84:822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- 30.Turknett Leadership Group. Emotional Intelligence Quiz. http://www.leadershipcharacter.com/eq_quiz2.htm. [Mar 27;2013 ]. http://www.leadershipcharacter.com/eq_quiz2.htm
- 31.Myers JJ. Rose CD. Shade SB, et al. Sex, risk and responsibility: Provider attitudes and beliefs predict HIV transmission risk prevention counseling in clinical care settings. AIDS Behav. 2007;11:S30–38. doi: 10.1007/s10461-007-9269-9. [DOI] [PubMed] [Google Scholar]
- 32.Steward WT. Koester KA. Myers JJ, et al. Provider fatalism reduces the likelihood of HIV-prevention counseling in primary care settings. AIDS Behav. 2006;10:3–12. doi: 10.1007/s10461-005-9024-z. [DOI] [PubMed] [Google Scholar]
- 33.Grodensky CA. Golin CE. Boland MS, et al. Translating concern into action: HIV care providers' views on counseling patients about HIV prevention in the clinical setting. AIDS Behav. 2008;12:404–411. doi: 10.1007/s10461-007-9225-8. [DOI] [PubMed] [Google Scholar]
- 34.Epstein RM. Siegel DJ. Silberman J. Self-monitoring in clinical practice: A challenge for medical educators. J Contin Educ Health Prof. 2008;28:5–13. doi: 10.1002/chp.149. [DOI] [PubMed] [Google Scholar]
- 35.Scott JG. Cohen D. DiCicco-Bloom B, et al. Understanding healing relationships in primary care. Ann Fam Med. 2008;6:315–322. doi: 10.1370/afm.860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Krasner MS. Epstein RM. Beckman H, et al. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA. 2009;302:1284–1293. doi: 10.1001/jama.2009.1384. [DOI] [PubMed] [Google Scholar]
- 37.Smajdor A. Stockl A. Salter C. The limits of empathy: Problems in medical education and practice. J Med Ethics. 2011;37:380–383. doi: 10.1136/jme.2010.039628. [DOI] [PubMed] [Google Scholar]
- 38.Farley TA. Cohen DA. Wu SY, et al. The value of screening for sexually transmitted diseases in an HIV clinic. J Acquir Immune Defic Syndr. 2003;33:642–648. doi: 10.1097/00126334-200308150-00014. [DOI] [PubMed] [Google Scholar]
- 39.Rieg G. Lewis RJ. Miller LG, et al. Asymptomatic sexually transmitted infections in HIV-infected men who have sex with men: prevalence, incidence, predictors, and screening strategies. AIDS Patient Care STDS. 2008;22:947–954. doi: 10.1089/apc.2007.0240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mayer KH. O'Cleirigh C. Skeer M, et al. Which HIV-infected men who have sex with men in care are engaging in risky sex and acquiring sexually transmitted infections: Findings from a Boston community health centre. Sex Transm Infect. 2010;86:66–70. doi: 10.1136/sti.2009.036608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Paasche-Orlow MK. Clarke JG. Hebert MR, et al. Education attainment but not literacy is associated with HIV risk behavior among incarcerated women. J Womens Health. 2005;14:852–859. doi: 10.1089/jwh.2005.14.852. [DOI] [PubMed] [Google Scholar]
- 42.Operario D. Nemoto T. Iwamoto M, et al. Unprotected sexual behavior and HIV risk in the context of primary partnerships for transgender women. AIDS Behav. 2011;15:674–682. doi: 10.1007/s10461-010-9795-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Annang L. Walsemann KM. Maitra D, et al. Does education matter? Examining racial differences in the association between education and STI diagnosis among black and white young adult females in the U.S. Public Health Rep. 2010;125:110–121. doi: 10.1177/00333549101250S415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Op de Coul EL. Gotz HM. van Bergen JE, et al. Who participates in the Dutch chlamydia screening? A study on demographic and behavioral correlates of participation and positivity. Sex Transm Dis. 2012;39:97–103. doi: 10.1097/OLQ.0b013e3182383097. [DOI] [PubMed] [Google Scholar]
- 45.Crenshaw K. Shewchuk RM. Qu H, et al. What should we include in a cultural competence curriculum? An emerging formative evaluation process to foster curriculum development. Acad Med. 2011;86:333–341. doi: 10.1097/ACM.0b013e3182087314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Like RC. Educating clinicians about cultural competence and disparities in health and health care. J Contin Educ Health Prof. 2011;31:196–206. doi: 10.1002/chp.20127. [DOI] [PubMed] [Google Scholar]
- 47.Duarté-Vélez Y. Bernal G. Bonilla K. Culturally adapted cognitive-behavioral therapy: Integrating sexual, spiritual, and family identities in an evidence-based treatment of a depressed Latino adolescent. J Clin Psychol. 2010;66:895–906. doi: 10.1002/jclp.20710. [DOI] [PubMed] [Google Scholar]
- 48.Ehsanzadeh-Cheemeh P. Sadeque A. Grimes RM, et al. Sociocultural dimensions of HIV/AIDS among Middle Eastern immigrants in the US: Bridging culture with HIV/AIDS programmes. Perspect Public Health. 2009;129:228–233. doi: 10.1177/1466424008094807. [DOI] [PubMed] [Google Scholar]
- 49.Spector AY. Pinto RM. Let's talk about sex: Helping substance abuse counsellors address HIV prevention with men who have sex with men. Cult Health Sex. 2011;13:399–413. doi: 10.1080/13691058.2010.550322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Williams JK. Ramamurthi HC. Manago C, et al. Learning from successful interventions: A culturally congruent HIV risk—Reduction intervention for African American men who have sex with men and women. Am J Public Health. 2009;99:1008–1012. doi: 10.2105/AJPH.2008.140558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rose CD. Koester KA. Kang Dufour MS, et al. Messages HIV clinicians use in prevention with positives interventions. AIDS Care. 2012;24:704–711. doi: 10.1080/09540121.2011.644232. [DOI] [PubMed] [Google Scholar]
- 52.Thrun M. Cook PF. Bradley-Springer LA, et al. Improved prevention counseling by HIV care providers in a multisite, clinic-based intervention: Positive STEPs. AIDS Educ Prev. 2009;21:55–66. doi: 10.1521/aeap.2009.21.1.55. [DOI] [PubMed] [Google Scholar]
- 53.Patel SN. Marks G. Gardner L, et al. Brief training of HIV medical providers increases their frequency of delivering prevention counselling to patients at risk of transmitting HIV to others. first published on. Health Edu J. 2012 Jul 11; doi: 10.1177/0017896912446740. 0017896912446740. [DOI] [Google Scholar]