Abstract
Objective
To estimate the demand for women's health care by 2020 using today's national utilization standards.
Methods
This descriptive study incorporated the most current national data resources to design a simulation model to create a health and economic profile for a representative sample of women from each state. Demand was determined utilizing equations about projected use of obstetrics-gynecology (ob-gyn) services. Applying patient profile and health care demand equations, we estimated the demand for providers in 2010 in each state for comparison with supply based on the 2010 American Medical Association Masterfile. U.S. Census Bureau population projections were used to project women's health care demands in 2020.
Results
The national demand for women's health care is forecast to grow by 6% by 2020. Most (81%) ob-gyn related services will be for women of reproductive age (18–44 years old). Growth in demand is forecast to be highest in states with the greatest population growth (Texas, Florida), where supply is currently less than adequate (western United States), and among Hispanic women. This increase in demand by 2020 will translate into a need for physicians or nonphysician clinicians, which is clinically equivalent to 2,090 full-time ob-gyns.
Conclusion
Using today's national norms of ob-gyn related services, a modest growth in women's health care demands is estimated by 2020 that will require a larger provider workforce.
Introduction
Adequate supply and distribution of providers are essential for there to be optimal healthcare for all women. The demand for women's health care is anticipated to only increase with institution of the Patient Protection and Affordable Care Act in 2014. Due to the length of time and expense required to train new physicians, it is prudent to anticipate well in advance any imbalances between the supply and demand for women's health care providers. Physician-to-population ratios are sometimes used to determine how many physicians should be in a region or state. Such ratios are too simple, however, and do not consider nonphysician clinicians and the many factors affecting current and future demands for women's healthcare.1
Demand determinants involve characteristics of the female population to be served. Economic, cultural, and health risk factors are examples of endpoints to measure the use and delivery of health care services. One means for quantifying healthcare demand unique to women is by examining the use of obstetrics and gynecology services. To that end, the objective of the present study was to estimate the demand for ob-gyn services in each state between 2010 and 2020. These forecasted demands will be influential when formulating strategies to better ensure accessible healthcare to all women.
Materials and Methods
This observational study was conducted after obtaining approval from the University of New Mexico Human Research Review Committee (HRCC 11-328). The investigation used a simulation approach to forecast demand for women's healthcare services at the state level. Principles of this new form of simulation modeling demand for health services have been reported by these authors.2,3
As a foundation for predicting demand, we used services provided by obstetrician-gynecologists (ob-gyns). We estimated demand for ob-gyn services under a “national norms” or baseline scenario that assumed each woman used health care services that were similar to her peers across the nation after controlling for demographic, insurance status, socioeconomic characteristics, and health risk factors. Our model simulated use of services according to the practice setting (physician office, outpatient clinic, emergency room, and hospital) and the full-time-equivalent (FTE) of ob-gyns to provide a level of care consistent with what was provided nationally in 2010.4
Demand calculations
We sought the most current population and health service data from well-accepted national databases. National data resources were used for determining demand for services and supply of providers. Each data resource was well described and easily accessible.4–12 The population database incorporated in the model contained health, demographic, and socioeconomic characteristics for women in a representative sample of the population in each state. This profile was created using statistical software (SAS) and a statistical matching process that combined socioeconomic and health profile data. Socioeconomic data from approximately 1.5 million women in the U.S. Census Bureau's 2010 American Community Survey (ACS) were combined with health profile data from the approximately 615,000 women in the 2009 and 2010 files of the Behavioral Risk Factor Surveillance System (BRFSS).5,6
To create a representative population sample, every woman in the ACS survey was randomly matched with a woman in the BRFSS from the same state according to age groups, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, other), insured/uninsured status, and household income. The patient population database also contained information about each person's home location (metropolitan, non-metropolitan), annual household income, medical insurance type (private, public, self-pay), any chronic medical condition (asthma, cardiovascular disease, diabetes, hypertension), history of cancer or stroke, body mass index (normal, overweight, obese, unknown), and smoking status (smoker, non-smoker).13 Using U.S. Census Bureau population projections for each state, we produced state-level estimates of demand in 2020.7,8
Health-seeking behaviors of women were generated from a regression analysis using data about 69,145 women from the 2005–2008 files of the Medical Expenditure Panel Survey (MEPS).9 Poisson regression quantified the relationships between patient characteristics and physician office visits or outpatient visits. We identified emergency room visits and hospitalizations using International Classification of Diseases, 10th edition (ICD-9) diagnosis codes for circumstances related to reproduction (codes v20–v29); diseases of the genitourinary system (codes 580–629); and complications of pregnancy, childbirth, and the puerperium (codes 630–679).14 Using logistic regression, we quantified the relation between patient characteristics and whether that person had an emergency room visit or a hospitalization for ob-gyn related services. The 2008 Nationwide Inpatient Sample (NIS) was used to estimate relationships between length of hospital stay and patient characteristics such as age group, race/ethnicity, insurance type, and home location.10
National practice patterns provided a starting point to model demand for services. Healthcare use prediction equations applied to the national population permitted estimates of total U.S. demand for ob-gyn services in physician offices, outpatient and emergency visits, and hospital stays. To convert demand for services into demand for FTE providers, we calculated the mean proportion of an ob-gyn's time spent in providing patient care at each practice setting, according to the 2012 American Congress of Obstetrician and Gynecologists (ACOG) Professional Liability Survey.4
Current supply of providers calculations
Estimates of the supply of physicians providing women's health care services came from an analysis of the 2010 American Medical Association (AMA) Masterfile.15 This data source included all physicians who described their primary practice as being ob-gyn—without being board certified or board eligible. We estimated the number of physicians in active ob-gyn practice in each state using responses about their primary specialty. To address concerns that the AMA Masterfile overestimates the number of active physicians, we limited our supply analysis to those under age 75. In addition, for physicians age 50 and older, we applied an algorithm that estimated a retirement probability based on responses from 1,204 ob-gyns who completed the Association of American Medical Colleges 2006 Physician Survey.12 The algorithm, based on our logistic regression, estimated the probability that a physician in the AMA Masterfile and over age 50 was not active, and therefore, should be removed from the supply estimates.12 Application of this algorithm removed 1,440 (3.7%) physicians aged 50–74 years from the national estimate. This estimate of the national supply in 2010 was used to determine a national normal (i.e., where supply was assumed to meet the demand at the national level). State-level estimates of supply in 2010 were compared between current and projected future demand.
Comparisons in demands between 2010 and 2020
Demand for ob-gyn related services was determined for 2010 and 2020 on a state-by-state basis. The difference between supply and demand for each state permitted a calculation of either a percent surplus or shortage of ob-gyn related services. We then estimated the growth in demand for 2020 by estimating the number of additional clinical FTEs of ob-gyns needed to meet the forecast patient demand.
Results
A supply of 37,370 physicians were engaged primarily in women's health care activities in 2010. Percentages of time dedicated to patient care were calculated to be 59% (22,140 FTEs) at physician offices, 29% (10,780 FTEs) in the operating room or labor and delivery unit, 8% (2,800 FTEs) to conduct hospital rounds, 4% (1,650 FTEs) at outpatient centers and emergency rooms, and 2% (971 FTEs) to interpret laboratory test results and correspondence.
Use of services across all settings varied in 2010 by the patient's age group, with those aged 18–34 years utilizing the most ob-gyn related services. Having third-party payment (especially Medicaid) was associated with much higher use. Factors that correlated with higher rates of visits to physicians' offices included being non-Hispanic white, living in a metropolitan area, being a non-smoker, and not having any chronic medical illness. Outpatient center visits were more likely to be used by women being overweight, having a lower income, having chronic medical conditions, and living in a metropolitan area. Black and Hispanic women were less likely to have scheduled visits at physician's offices and more inclined to seek care at unscheduled outpatient centers. Compared with other ethnic groups, Hispanic women were substantially most likely to use emergency rooms for ob-gyn-related care.
Demand for services was calculated for 2010 and shown for each state in Table 1. A supply–demand equilibrium (±5%) was met in 16 states. The greatest estimated shortage in supply of ob-gyns was notable in the following states: North Dakota (–60%), Iowa (–54%), Oklahoma (–34%), Arkansas (–32%), and Nebraska (–24%). The ob-gyn supply was more than adequate (surplus) to meet the demand in Connecticut (25%), Hawaii (25%), Maryland (23%), New Jersey (19%), and New York (18%).
Table 1.
Supply of Clinical Full Time Equivalent Obstetrician-Gynecologists in 2010 and Percent Change in Demand for Women's Health Care Services by 2020
| State | Ob-gyn supply 2010 | Patient demand* 2010 | Patient demand* 2020 | Change in demand (%) 2010–2020 |
|---|---|---|---|---|
| AK | 80 | 80 | 90 | +13 |
| AL | 520 | 560 | 540 | −4 |
| AR | 250 | 330 | 330 | 0 |
| AZ | 680 | 780 | 970 | +24 |
| CA | 4,400 | 4,670 | 5,310 | +14 |
| CO | 630 | 610 | 650 | +7 |
| CT | 590 | 440 | 450 | +2 |
| DC | 190 | 110 | 100 | −9 |
| DE | 100 | 110 | 110 | 0 |
| FL | 2,090 | 2,060 | 2,430 | +18 |
| GA | 1,260 | 1,130 | 1,230 | +9 |
| HI | 200 | 150 | 160 | +7 |
| IA | 240 | 370 | 350 | −5 |
| ID | 150 | 180 | 190 | +6 |
| IL | 1,650 | 1,630 | 1,620 | −1 |
| IN | 650 | 780 | 780 | 0 |
| KS | 270 | 330 | 320 | −3 |
| KY | 490 | 490 | 470 | −4 |
| LA | 590 | 540 | 520 | −4 |
| MA | 970 | 940 | 950 | +1 |
| MD | 930 | 720 | 780 | +8 |
| ME | 150 | 160 | 150 | −6 |
| MI | 1,200 | 1,180 | 1,140 | −3 |
| MN | 580 | 680 | 690 | −1 |
| MO | 670 | 710 | 700 | −1 |
| MS | 310 | 340 | 320 | −6 |
| MT | 100 | 110 | 100 | −9 |
| NC | 1,170 | 1,150 | 1,270 | +10 |
| ND | 50 | 80 | 70 | −13 |
| NE | 170 | 210 | 200 | +5 |
| NH | 170 | 160 | 160 | 0 |
| NJ | 1,280 | 1,040 | 1,080 | +4 |
| NM | 210 | 230 | 240 | +4 |
| NV | 290 | 300 | 380 | +27 |
| NY | 3,060 | 2,520 | 2,520 | 0 |
| OH | 1,330 | 1,390 | 1,320 | −5 |
| OK | 320 | 430 | 430 | 0 |
| OR | 490 | 460 | 490 | +7 |
| PA | 1,550 | 1,540 | 1,490 | −3 |
| RI | 160 | 140 | 140 | 0 |
| SC | 530 | 550 | 560 | +2 |
| SD | 80 | 90 | 80 | −11 |
| TN | 810 | 780 | 810 | +4 |
| TX | 2,730 | 2,860 | 3,350 | +17 |
| UT | 300 | 370 | 400 | +8 |
| VA | 1,080 | 980 | 1,070 | +9 |
| VT | 90 | 80 | 80 | 0 |
| WA | 720 | 840 | 930 | +11 |
| WI | 600 | 710 | 690 | −3 |
| WV | 180 | 210 | 190 | −10 |
| WY | 60 | 60 | 60 | 0 |
| United States | 37,370 | 37,370 | 39,460 | +6 |
Supply–demand equilibrium: −5% to +5%.
Units: number of full-time clinical equivalents of obstetrician-gynecologists needed to meet demand.
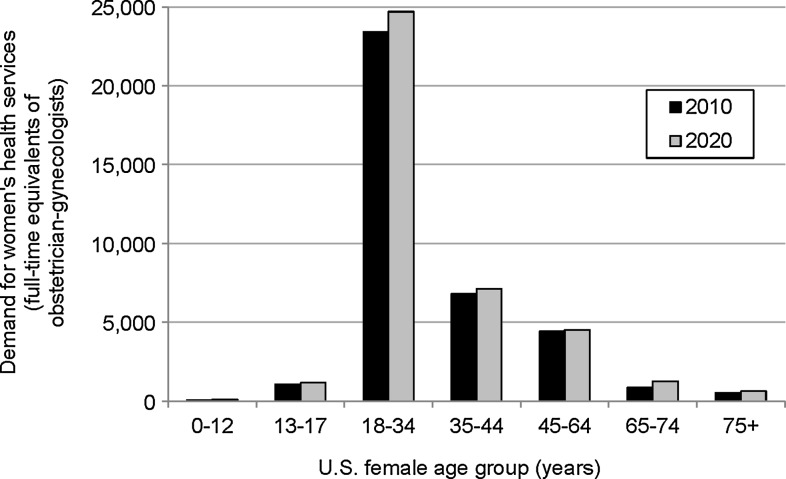
The overall patient demand for ob-gyn services in the United States is forecast to grow by 6% between 2010 and 2020 (Table 1). The female population age 14 and older is projected to increase by more than 10% between 2010 and 2020, but much of this growth will be among women age 65 and older (33% growth rate) who use relatively fewer ob-gyn related services. An estimated 81% of time for ob-gyn related services is currently devoted to women of reproductive age (18–44 years old), and this population is projected to grow in the United States by slightly less than 6% during this period (Fig. 1). If future patterns of care delivery remain similar to today's care delivery patterns, growth in demand for women's health care services between 2010 and 2020 will require the equivalent of an additional 2,090 clinical FTEs of ob-gyns at the national level.
FIG. 1.
Estimated demand for women's health care (full-time equivalents of obstetrician-gynecologists) by U.S. female population age group for years 2010 and 2020.
Projected growth in the demand for women's health care services was not found to be equally divided among the races. Over half (56%) of the growth in demand by 2020 will be associated with more needs of Hispanic women compared with 18% growth in service needs by the non-Hispanic white population. In 2010, approximately 17% of ob-gyn related service time was utilized by patients of Hispanic origin, which accounts for approximately 6,700 clinical FTEs to provide such services. By 2020, approximately 19% of ob-gyn service time will be dedicated to providing care to Hispanic women, which equates to approximately 8,200 clinical FTEs of ob-gyn physicians.
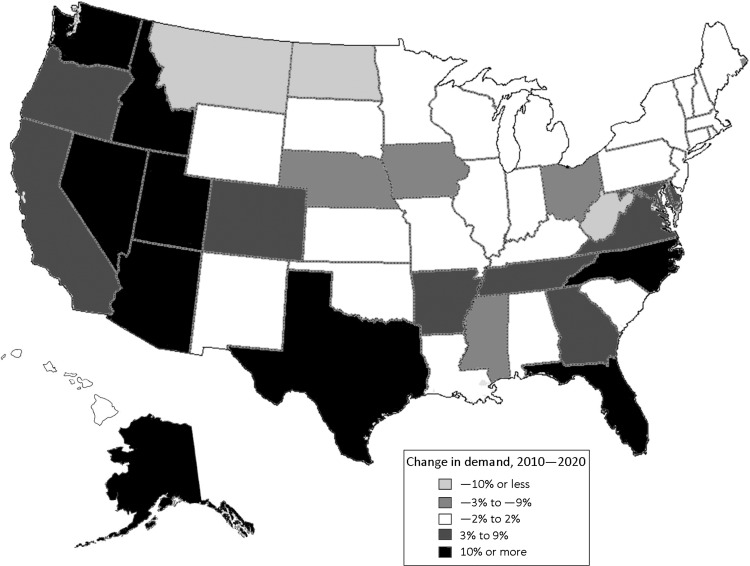
The estimated number of clinical FTEs of ob-gyns to meet the forecast women's health demand is shown in Table 1 for 2020. This change in demand (far right column) will vary substantially by state over the next 10-year period. It is forecast by 2020 to be highest in Nevada (27%), Arizona (24%), Florida (18%), and Texas (17%) but less than in 2010 in West Virginia (–11%), North Dakota (–10%), and Montana (–9%). Figure 2 displays graphically how growth in demand for ob-gyn services will change between 2010 and 2020 from state to state. Nearly half (24) of the states will likely show no growth in patient demand (±2%), while 18 (36%) will increase and 7 (14%) will decrease in demand.
FIG. 2.
Estimated change in demand for women's health services by 2020.
Discussion
Demand for women's health care services must be considered when exploring the supply of physicians or nonphysician clinicians (advance care providers, midwives, physician assistants). This study confirms that substantial geographic imbalances exist in the current supply of ob-gyn physicians in the United States, with several Central and Mountain West states having substantially less supply than required to meet patient demands.16 Results from the present study suggest that over the next decade, this demand for services will grow nationally at a modest 6% rate. Forecasted demand will vary geographically from a 27% increase in Nevada to an 11% decrease in West Virginia. States especially vulnerable are Arizona, Washington, Utah, and Idaho, since there is already an insufficient supply of ob-gyns coupled with projected large percentage increases in demand. In addition, Florida, Texas, North Carolina, and Nevada will be vulnerable due to projected increases in the adult female population that would partially explain the increased overall demand for women's health care services.
A strength of this novel simulation analysis was that it used a combination of several recent national databases to consider geographic variations in patient demographic, economic, and health risk factors. This multivariable approach provided a more accurate estimate of demand for women's health services rather than by simply projecting provider-to-adult female population ratios. This analysis takes into account trends in patient demographics as well as projected modest growth in household income. Another feature of this simulation analysis was consideration of ob-gyn service related demand in separate states that would have more meaning in regional healthcare decision making. Compared with a longer study time, this 10-year period allowed for greater accuracy and timelier adjustments of our forecast equations according to changes. At this time, it remains unclear how health care reform and expanded insurance coverage will affect demand for services in each region.
Findings from this report have important policy implications at both national and state levels. Our results support a need to increase the supply of providers for women's health services. Financial support to offset the considerable cost of training additional ob-gyn residents is highly improbable unless well justified in regions with the greatest need. Without increases in the number of ob-gyns trained, the nation will rely more heavily on services by nonphysician clinicians. In addition, other physicians trained to address many of the general health care needs of women are ob-gyn subspecialists and adult primary care physicians in family medicine or ambulatory general internal medicine. Forecasted shortfalls in clinical equivalents of physicians, as reported in this study, also suggest that ob-gyns in certain locations may have to limit their practice more and not assume expanded roles in addressing women's primary care needs. Growth in demand for ob-gyn related services is anticipated to be highest among minority populations (especially Hispanics), thereby highlighting a need for greater diversity within the provider workforce.
Information from this investigation for the higher-level, broader health policy community would offer a context within which to develop targeted policies and programs in women's health care. While national policies may not exist about a shortage in many medical specialties, state-level initiatives could respond where there are predicted to be shortages of specific women's health specialists. Addressing any predicted shortfall of women's health services in a state would require considerations about an analysis of local or regional health conditions, the involvement of local provider agencies, and the rational construction of service areas focusing especially on access to care and minimizing additional cost. It is likely that competition will exist between hospitals for shortages of those providers. In the same way that hospitals compete feverishly for new businesses, they could act more assertively in physician and nonphysician clinician recruitment.
Institution of the Affordable Care Act will likely increase demand for ob-gyns and other women's health care providers.17 To the best of our limited knowledge, we feel that women's health care needs will increase, but not sizably. Our projected 6% increase in demand by 2020 is conservative, yet we speculate that any additional increase will be only 1%–2% more. As a first step, findings from this study will better determine the projected training of additional physicians and nonphysician clinicians. Unfortunately, there are no good data in women's health care alone about nurse practitioners and physician assistants. Furthermore, a challenge for certified nurse midwives (CNMs) is the lack of state level data, including those CNMs who are self-employed versus those in a physician-led group practice. This issue about training the future supply of women's health care providers is important for future research as the data become available in the next few years.
Certain limitations exist about our simulation model to forecast demand for women's health care. Our scenario does not consider the extent of any changes in care delivery attributable to technological innovation or to more emphasis on evidence-based medicine. Such scenarios could increase or decrease demand for services and providers and can be incorporated into future simulations. Secondly, changes in access to care may encourage more visits to primary care providers at patient-centered medical homes. Whether primary care providers could assume such an expanded role in women's health is unclear—especially because many of the areas with ob-gyn shortfalls also experience shortfalls of other physicians.1 Lastly, we did not consider providers at county levels. These efforts to “drill down” to smaller geographic areas would require more precision and be subject to more misinterpretation.
Our analysis was based on certain assumptions such as the current ob-gyn physician supply being adequate at the national level. There are insufficient data to either support or refute this assumption. This analysis forecasted demand, not the future supply of ob-gyns and non-physician clinicians. Such forecasts are an area for future research but would require taking into account the current demographics of the provider workforce, numbers and characteristics of graduates, and patterns for retirement and hours worked. To the extent that supply of nonphysician clinicians of women's health services grows faster than 6%, then demand for ob-gyn physicians could be less than the projected 6% growth between 2010 and 2020.
Conclusions
This report used standard national data sources to analyze the current healthcare demand by women seeking ob-gyn related services in order to forecast future demands. We project that if current trends continue, then demand for services will grow by 6% during the next decade. A lower limit of forecasted demand would primarily result from either less growth of the population or expanded use of nonphysician clinicians. An upper limit on demand would occur if there is a major impact from instituting the Affordable Care Act in 2014 and if providers assume more responsibility for the outpatient care of more women with a resultant increase in procedures. This increase in demand for providers will likely be somewhere in-between these two extremes, suggesting a need for women's health services to be delivered more by either qualified nonphysician providers or other adult primary care physicians. Strategies are needed to collect ongoing data about the geographical demands for women's healthcare to encourage more qualified providers to be recruited and retrained in underserved communities.
Acknowledgments
This research was supported by IHS Global Inc., Washington, DC; American Congress of Obstetricians and Gynecologists, Washington, DC; and the Randolph V. Seligman Research Endowment, University of New Mexico School of Medicine, Albuquerque, NM.
Disclosure Statement
No competing financial interests exist.
References
- 1.Rayburn WF. The obstetrician-gynecologist workforce in the United States. Washington DC: American Congress of Obstetricians and Gynecologists; 2011. pp. 119–135. [Google Scholar]
- 2.Dall TM. Zhang Y. Zhang S, et al. Weight loss and lifetime medical expenditures: a case study with TRICARE Prime beneficiaries. Am J Prev Med. 2011;40:338–344. doi: 10.1016/j.amepre.2010.11.020. [DOI] [PubMed] [Google Scholar]
- 3.Yang W. Dall TM. Zhang Y. Zhang S. Arday DR. Dorn PW. Jain A. Simulation of quitting smoking in the military shows higher lifetime medical spending more than offset by productivity gains. Health Affairs. 2012;31:2717–2726. doi: 10.1377/hlthaff.2010.1048. [DOI] [PubMed] [Google Scholar]
- 4.Klagholz J. Strunk AL. Washington DC: American College of Obstetricians and Gynecologists; 2012. [Sep 1;2012 ]. Overview of the 2012 ACOG survey on professional liability (electronic) pp. 1–6. [Google Scholar]
- 5.United States Census Bureau. American community survey. 2010. www.census.gov/acs/www/ [Sep 1;2012 ]. www.census.gov/acs/www/
- 6.Centers for Disease Control and Prevention (CDC) Atlanta, Georgia: US Department of Health and Human Services; 2010. [Sep 1;2012 ]. Behavioral risk factor surveillance system survey data. [Google Scholar]
- 7.U.S. Census Bureau. Interim state population projections 2000–2030 based on Census 2000. 2005. www.census.gov/population/www/projections/projectionsagesex.html. [Sep 1;2012 ]. www.census.gov/population/www/projections/projectionsagesex.html
- 8.U.S. Census Bureau. National population projections. 2008. www.census.gov/population/www/projections/2008projections.html. [Sep 1;2012 ]. www.census.gov/population/www/projections/2008projections.html
- 9.Agency for Healthcare Research and Quality (AHRQ) Medical expenditure panel survey. 2009. http://meps.ahrq.gov/mepsweb. [Jun 1;2012 ]. http://meps.ahrq.gov/mepsweb [PubMed]
- 10.AHRQ. Nationwide inpatient sample. 2009. www.hcup-us.ahrq.gov/nisoverview.jsp. [Sep 1;2012 ]. www.hcup-us.ahrq.gov/nisoverview.jsp
- 11.American Congress of Obstetricians and Gynecologists (ACOG) Washington, DC: ACOG; 2004. [May 1;2012 ]. Profile of ob-gyn practice. [Google Scholar]
- 12.Association of American Medical Colleges (AAMC) Washington, DC: AAMC; 2008. [Sep 1;2012 ]. The complexities of physician supply and demand: Projections through 2025. [Google Scholar]
- 13.National Heart, Lung, and Blood Institute (NHLBI) NHLBI Obesity Education Initiative Expert Panel on the Identification, Evaluation, and Treatment of Obesity in Adults (US) Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: The evidence report. 1998. www.ncbi.nlm.nih.gov/books/NBK2003. [Sep 1;2012 ]. www.ncbi.nlm.nih.gov/books/NBK2003
- 14.ACOG Committee on Coding and Nomenclature. ICD-9-CM Abridged. Washington, DC: ACOG; 2010. [Google Scholar]
- 15.AMA; 2012. [Sep 1;2012 ]. American Medical Association Masterfile, 2010. [Google Scholar]
- 16.Rayburn WF. Klagholz JC. Murray-Krezan C. Dowell LE. Strunk AL. Distribution of American Congress of Obstetricians and Gynecologists fellow and junior fellows in practice in the United States. Obstet Gynecol. 2012;119:1017–1022. doi: 10.1097/AOG.0b013e31824cfe50. [DOI] [PubMed] [Google Scholar]
- 17.Gee RE. Rosenbaum S. The Affordable Care Act: An overview for obstetricians and gynecologists. Obstet Gynecol. 2012;120:1263–1266. doi: 10.1097/aog.0b013e3182756118. [DOI] [PubMed] [Google Scholar]