Abstract
Women of color (WOC) are at increased risk of dying from HIV/AIDS, a disparity that may be partially explained by the care barriers they face. Based in a health care disparity model and the socio-ecological framework, the objective of this study was to identify the barriers and facilitators to HIV care at three points along the HIV continuum: HIV testing, entry/early care, and engagement. Two focus groups (n=11 women) and 19 semi-structured interviews were conducted with HIV-positive WOC in an academic medical setting in North Carolina. Content was analyzed and interpreted. We found barriers and facilitators to be present at multiple levels of the ecological framework, including personal-, provider-, clinic-, and community-levels. The barriers reported by women were aligned with the racial health care disparity model constructs and varied by stage of HIV. Identifying the salient barriers and facilitators at multiple ecological levels along the HIV care continuum may inform intervention development.
Introduction
Women account for approximately 27% of new human immunodeficiency virus (HIV) infections in the United States (US).1 In 2008, a year for which mortality data were available, HIV was the sixth leading cause of death among all US women aged 25–44 years.2 The factors that place women at increased risk for HIV infection include both younger and older age; a lack of awareness and recognition of her partner's risk factors; high-risk heterosexual contact, including the inability to negotiate safer sex practices; biologic vulnerability to HIV resulting from women's larger mucosal area exposed during vaginal intercourse and co-morbid sexually transmitted diseases.3 In addition, substance use, childhood or adult trauma, and mental health issues also combine to put women at increased risk of HIV and AIDS.1,4–6 The estimated percent of AIDS diagnoses among adult and adolescent females increased from 7% in 1985 to 25% in 2010.7
However, not all women are at equal risk for HIV infection and progression to AIDS. Over a 4-year period (2006–2009), an analysis of HIV data showed that among females, African American women had the highest rates of new HIV infections each year, followed by Latina women.8 Furthermore, among women of color (WOC), HIV infection was the leading cause of death for African American women aged 25–34 years, the third leading cause of death for African American women aged 35–44 years, the fourth leading cause of death for African American women aged 45–54 years, and the fourth leading cause of death for Hispanic women aged 35–44 years in the US.3 In 2010, the overall HIV infection diagnosis rate was 8.0 per 100,000, while the rate for African American women was 41.7.7 Because many of these WOC face racial or sexual discrimination, and suffer from poverty, low health literacy, and low access to health care, they may delay entry into HIV care.1 The consequence of this delay is the death rate differential experienced by African American compared with white women: in 2009, the death rate among adult and adolescent African American females with an HIV infection diagnosis was 23.8, compared with 1.1 for white women the same year.7 Patterns of care entry and engagement may help explain AIDS-related disparities.9
HIV care occurs along a continuum,10 beginning with the individual decision to get tested and culminating—hopefully—in the appropriate and long-term engagement in HIV care. Estimates of the total HIV population at each step of HIV care have been published.11,12 Due to a significant reduction in the proportion of all HIV-infected persons at each subsequent step in the care continuum, the graphic representation has been referred to as a “cascade.” The cascade of HIV care begins with the population of HIV-infected individuals (both known and unknown) and follows the national proportions down each step of the care continuum, from HIV-diagnosed to linked to care to retained in care to on antiretroviral therapy to suppressed viral load. The important thing to note about the care cascade is that within each step of the care process, smaller proportions of individuals are contained. For instance, while approximately 80% of suspected infections have been diagnosed, 62% are thought to be linked to care and only 28% of likely HIV-infected individuals are virally suppressed. These decreasing proportions of HIV-infected individuals engaged in appropriate HIV care adversely influence public health. It is likely that barriers to HIV care exist at each step of the HIV care cascade, which results in decreasing numbers of HIV-infected individuals being represented at the more advanced levels of HIV engagement and support.
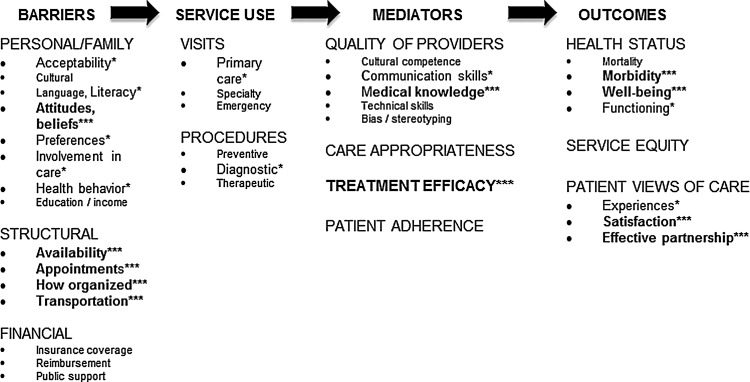
Barriers to engaging in care exist at every stage in the HIV care process and can be found at multiple levels of the socio-ecological framework,13 including personal (financial, attitudinal), provider (clinic structure, appointment availability), and community (stigma, lack of testing availability).1,9 The Cooper model of access to health resources was designed to organize the multiple factors that may contribute to health disparities,14 and is the conceptual model underlying this research. It describes barriers (personal/family, structural, financial) as contributing to individual's use of health services and mediators that influence the relationships between service usage and patient health outcomes that accrue (Fig. 1). Barriers are seen as events that occur prior to health care system contact, whereas mediators occur after entry into care. Together barriers and mediators lead to outcomes. The Cooper model is useful for describing how the accumulation of barriers may contribute to the disproportionately high morbidity and mortality from AIDS observed among WOC.
FIG. 1.
Key: Items in smaller font (8-point) not mentioned during focus groups/semi-structured interviews. Items in larger font (10point) with one * are items identified by participants. Items in bold with *** are items spontaneously offered by three or more women. Adapted and reprinted by permission from Ref. 14.
Considerable research has examined correlates of care singly, including psychosocial status,15,16 supportive relationships,17–19 and violence.20,21 While some research identifying a range barriers to HIV care exists,1 little has explored these barriers at various stages in the HIV-care engagement process specifically among one of the most vulnerable populations—women of color. In light of the need to reduce the health disparities associated with HIV care among WOC, and the recognition that barriers and facilitators occur at multiple structural levels, this article will report on the barriers and facilitators identified by HIV-positive WOC at three stages of the HIV care continuum: getting tested for HIV, entering HIV care, and remaining appropriately engaged in care.
Methods
Study description
Based on a model of racial health disparities,14 the Guide to Healing (G2H) project is framed around healing communication principles, including motivational interviewing and self-determination theory.22 To supplement the ongoing HIV care activities, including social support, on-site psychiatric and addiction services, three main interventions are being delivered to HIV-positive women of color (WOC) as part of the G2H project: (1) rapid linking into care, (2) strengths-based counseling, and (3) informational and support groups with health literacy, coping, life skills, and social support modules. It is within the G2H project that the research reported here was conducted.
Research setting
The research was conducted in an academic medical care clinic in North Carolina (NC). The medical clinic provided HIV care to 1700 HIV infected people in 2010, of whom 58% were African American, 10% were Hispanic or otherwise not white, and 31% were women. Of the women seen in the medical clinic, almost all were minority women (82%), of whom the majority (69%) was African American.
Instrument development
The qualitative research guide was developed to capture the potential barriers and facilitators to engaging with the HIV care system at three critical time points for engagement in HIV care. We asked about women's decision to get tested and their testing experience; the time period during which they were waiting for their HIV testing results and early experiences in HIV care; more regular experiences in their early HIV care; and contemporary care experiences. The interview instrument also contained questions designed to elicit feedback regarding specific planned intervention components. The research team was interested in understanding women's opinions about the feasibility, acceptability, and potential utility of possible care modifications. Finally, the instrument asked women to respond to a list of possible barriers or facilitators and rate their top five (Table 1). The qualitative guide was pilot-tested among a group of non-research participants and revised for use.
Table 1.
Participant Ratings of Barriers and Facilitators from Checklist and Number of “Top Five” Ratings for Items
|
How often do you agree with these statements? All or most of the time (1); some of the time (2); never or hardly ever (3) |
Average score |
|---|---|
| 37) Important people in my life want me to take care of myself | 1.07 |
| 22) I do things to take care of myself | 1.13 |
| 24) I can have a long life with HIV | 1.13 |
| 27) Going to my appointments will keep me well | 1.13 |
| 33) No one here will treat me badly because of my HIV | 1.13 |
| 34) I trust the providers here to take care of me | 1.13 |
| 21) Treatment for HIV is getting better every year | 1.17 |
| 1) A doctor, nurse, or counselor helped me get care | 1.23 |
| 23) I can get help getting to the clinic if I need it | 1.27 |
| 30) I need to take care of myself so I can take care of others (my family) | 1.30 |
| 44) The clinic staff help me to be brave when I think about my HIV | 1.30 |
| 20) I understand HIV and how it is treated | 1.33 |
| 48) When I am told when my next appointment is before I leave clinic, it is easier to be there | 1.34 |
| 16) I've been getting emotional support from others | 1.40 |
| 25) Appointments are scheduled at times that work for me | 1.40 |
| 5) I've been getting comfort and understanding from someone. | 1.43 |
| 8) My romantic partner provides me with love and care | 1.48 |
| 40) When I can get care for my other medical issues, it is easier to make my HIV appointments | 1.57 |
| 26) I know I won't wait too long during my appointment | 1.60 |
| 28) I know my way around the hospital and clinic | 1.60 |
| 4) Getting help with expenses makes it easier to come to my appointments | 1.63 |
| 42) Talking to a counselor makes it easier to take care of myself | 1.64 |
| 32) I take care of my HIV so I can keep going to work | 1.65 |
| 47) When I can talk to someone about my drug use, it is easier to keep my appointments | 2.32 |
| 11) I am worried about the cost of my appointment | 2.37 |
| 35) I worry that someone will find out about my clinic visits | 2.38 |
| 41) Some of my medications make me feel too ill to take | 2.55 |
| 36) I'm not sure I understand what the doctors and nurses tell me | 2.63 |
| 39) On days when I feel very sad, I do not like to come to the clinic | 2.63 |
| 49) I don't always have a working phone number. | 2.63 |
| 38) It is too hard to tell the doctors and nurses what is going on in my life | 2.67 |
| 9) I am not sure that the HIV medicine is good to take | 2.70 |
| 29) I missed appointments when I was drunk, high or hung-over | 2.72 |
| 18) Sometimes I am too sick to come to clinic | 2.73 |
| 2) If I don't come to clinic, I don't have to think about my HIV | 2.77 |
| 10) I am worried about missing a day of work | 2.77 |
| 13) I did not always get the appointment information | 2.77 |
| 14) I do not always have access to a car that works, so sometimes I skip appointments | 2.79 |
| 19) I had to wait a long time for my appointment here and I forgot it | 2.80 |
| 31) I sometimes miss appointments because I cannot tell anyone I am getting treated for HIV | 2.80 |
| 7) When I don't have enough food for my family, I don't come to my appointments | 2.83 |
| 12) I cannot get my questions answered in this clinic | 2.86 |
| 17) I have other people to take care of, so I cannot take care of myself | 2.86 |
| 45) The world would be better without me | 2.87 |
| 3) Everyone dies with AIDS, so what is the point of treatment? | 2.90 |
| 43) When my partner is angry with me I am afraid to come to appointments | 2.95 |
| 46) Things I have to do for my family keep me from coming to clinic | 2.97 |
| 15) I've been too worried about where I'm going to live, so I couldn't come to clinic | 2.90 |
| 6) Without child care, I cannot come to my appointments | 3.00 |
Participant recruitment and consent
Posters describing the qualitative study participation opportunity were posted in the medical care clinic. Social workers, nurses, and providers also informed potential participants about the opportunity to participate. Following the first recruitment period, during which 11 participants agreed to participate in two focus groups, we assessed the participants' socio-demographic characteristics and compared them to the overall clinic population based on age, number of years in care, and presence of young children in the home. In an effort to ensure we were capturing the heterogeneous perspectives of the clinic population, the second round of recruitment was targeted toward younger and more recently diagnosed women. Of those approached, 19 agreed to participate in the qualitative study. Both the UNC and the Duke University Institutional Review Boards approved consent and recruitment procedures. Informed consent occurred prior to the focus groups and individual interviews.
Data collection procedures
Based on prior experience with the clinic population, the investigators knew some women would be willing to participate in focus groups, while others would be more likely to respond to some of these sensitive questions in a more private setting. Therefore, we conducted both focus groups (two focus groups comprised of 11 participants total) and semi-structured individual interviews (19 interviews). The final sample falls within acceptable parameters for a qualitative research sample.23
The focus groups occurred over two months (January–February, 2010) and were conducted by an experienced facilitator who was also a woman of color; each took approximately 2 h to complete. Note-takers recorded field observations during the focus groups and expanded upon these notes following each session.24 The semi-structured interviews were completed between February and May (2010); six were in-person interviews and 13 occurred by telephone. These semi-structured interviews were facilitated by an experienced interviewer and took about 1 h to complete. All interviews were digitally recorded and transcribed verbatim. The transcripts were compared to the audio recordings and corrected for discrepancies when necessary.
Data analysis
The approach to data analysis was informed by grounded theory methodology, for which the first step is data collection from which specific themes and codes emerged. We took this approach because we did not want to impose preconceived notions of what constituted relevant barriers on the data women were providing, but at the same time recognized the project was informed by behavioral theories and investigators anticipated some number of topics that might be disclosed by participants. Data were analyzed using a systematic, manual open-coding approach adapted from grounded theory strategies 25 to identify barriers and facilitators to patient care and themes relevant to the socio-ecological model13 and recurring themes were identified, discussed and modified until thematic saturation was achieved. This modified grounded theory approach to analysis employed both inductive and deductive reasoning to inform the analysis.26 Each transcript (focus group or interview) was independently read and content-coded by three members of the analytic team,27 using traditional open-coding content analysis. At each step, team members discussed the coding, identified areas of discrepancy and resolved them. Overall, inter-rater reliability was high. Sharing the identified codes and themes with the larger authorship group, all of whom had experience with the patient population and were able to provide feedback on interpretations, helped ensure data validity. Data dependability was further established by careful recording of the coding processes and frequent returns to the original language in the transcripts. In a non-qualitative format, responses to the barriers and facilitators list were collected following the focus group or individual interview, averaged and each item was ranked.
Results
Participants
Most of the 30 participants were over 40 years of age (Table 2) and had not gone beyond a high school education. Approximately 20% of the women were married, and most women had either child or adult caregiving responsibilities, including eight women who reported caring for both. Only 17% of all women had private insurance, 63% were not employed, and the largest percentage of women earned between $5,000 and $14,900 annually. The women who participated in the qualitative study had been diagnosed with HIV for more than 6 years and had disclosed their diagnosis to multiple people. Fewer than half had independent transportation to clinic, and a fifth allowed more than 3 hours for a clinic visit (due to distance traveled and transportation limitations). Women who participated in individual interviews were more likely to be younger, employed, and live farther away from clinic and have higher incomes and education than focus group participants.
Table 2.
Focus Group and Semi-Structured Interview Participant Description
| Focus group membernumber (%) | Intervieweenumber (%) | |
|---|---|---|
| Sociodemographic characteristics | ||
| Main race/ethnicity | ||
| African American | 10 (91%) | 15 (85%) |
| Puerto-Rican Hispanic | 1 (9%) | 1 (5%) |
| Multi-racial | 0 (0%) | 2 (10%) |
| Age | Mean age: 49.5 | Mean age: 42.1 |
| Twenties | 0 (0 %) | 3 (16%) |
| Thirties | 1 (9%) | 5 (26%) |
| Forties | 5 (45%) | 7 (37%) |
| Fifties or sixties | 5 (45%) | 4 (21%) |
| Education | ||
| Less than high school | 4 (36%) | 5 (26%) |
| High school | 3 (27%) | 9 (47%) |
| More than high school | 4 (36%) | 5 (26%) |
| Relationship status (multiple) | ||
| Single | 5 (45%) | 8 (42%) |
| Married, living with | 2 (18%) | 6 (32%) |
| Not datinga | 1 (9%) | 2 (11%) |
| Dating | 3 (27%) | 3 (16%) |
| Caregiving responsibilities | ||
| Children | 5 (45%) | 8 (42%) |
| Adults | 3 (27%) | 3 (16%) |
| Both | 1 (9%) | 2 (11%) |
| Income/financial support characteristics | ||
| Insurance status | ||
| Private | 0 (0%) | 5 (26%) |
| Public | 10 (91%) | 8 (42%) |
| None | 1 (9%) | 6 (32%) |
| Employment status | ||
| Full-time (no part-time workers) | 0 (0%) | 11 (58%) |
| No employment | 11 (100%) | 8 (42%) |
| Income | ||
| Less than $5000 | 4 (36%) | 4 (21%) |
| $ 5000–$14,900 | 6 (54%) | 9 (47%) |
| $15,000+ | 1 (9%) | 6 (32%) |
| HIV-related characteristics | ||
| Time since HIV diagnosis | ||
| 6+ years ago | 10 (91%) | 16 (84%) |
| 4–6 years ago | 1 (9%) | 2 (11%) |
| 1–3 years ago | 0 (0%) | 1 (5%) |
| HIV disclosure | ||
| No one | 0 (0%) | 1 (5%) |
| 1–3 people | 2 (18%) | 5 (26%) |
| 4–9 people | 2 (18%) | 3 (16%) |
| 10+ people | 7 (64%) | 10 (53%) |
| Transportation to clinic | ||
| Drove self | 5 (45%) | 8 (42%) |
| Got ride from someone else | 1 (9%) | 4 (21%) |
| Took bus or van | 5 (45%) | 6 (32%) |
| How much time do you budget | ||
| <2 h | 4 (36%) | 6 (32%) |
| 2–3 h | 7 (64%) | 7 (37%) |
| >3 h | 0 (0%) | 6 (32%) |
Not dating includes separated, divorced, widowed, and otherwise not dating.
Global barriers and facilitators to HIV care
Women were asked to respond to a list of 49 barriers and facilitators to HIV care (see Table 1). The most women agreed “all or most of the time” to the statement, “Important people want me to take care of myself.” Tied for the second most consistently agreed upon statements were the following five items: “I do things to take care of myself,” “I can have a long life with HIV,” “Going to my appointments will keep me well,” “No one here (clinic) will treat me badly because of my HIV,” and “I trust the providers here to take care of me.” Contained within these six statements are the beliefs that women can live with HIV, they are powerful to affect their own health, that HIV care is effective, and that the providers will respectfully partner with them in their HIV care.
Attitudes representing defeatism (e.g., “Everyone dies with AIDS, so what is the point of treatment”) and personal barriers (e.g., “When my partner is angry with me I am afraid to come to appointments,” “Things I have to do for my family keep me from coming to clinic,” “I've been too worried about where I am going to live, so I couldn't come to clinic,” and “Without childcare, I can not come to my appointments”) were almost always listed as “Never or hardly ever” suggesting these items do not represent substantial current barriers to HIV care for the WOC who participated in this work.
Barriers and facilitators across the continuum of HIV care
Getting tested for HIV
Women reported getting HIV tested for personal reasons (Table 3). Some were already sick and scared, while others had become pregnant and did not want to risk transmitting HIV to their child. Other facilitators included getting paid for testing, having a sexual or drug partner who had already tested positive, and wanting to get tested with a new sexual partner:
Table 3.
Participant-Identified Barriers and Facilitators for Three Stages of HIV Treatment: Getting Tested for HIV, Entry into Care for HIV, and Engagement in HIV Care
|
Getting tested for HIV | ||
|---|---|---|
| Facilitators | Barriers | |
| Patient-level | • Already sick and scared | • Personal ignorance of risk factors / behavioral risk |
| • Pregnant–not wanting to infect fetus | • Drug addiction | |
| • Partner/drug-partner testing | • Don't really want to know | |
| • Partner tested positive | • Fear and stigma | |
| • Getting paid to be tested | ||
| Provider-level | • Good relationship with doctor | • No barriers identified because no pre-existing relationship with doctor |
| • Should include testing in annual exam | ||
| Clinic-level | • Counseling to let woman know she is competent to care for self | • Didn't choose to get tested; tested while incapacitated in health care setting |
| • Testing should be part of annual care | ||
| Community-level | • Communal awareness of HIV seriousness and risk factors | • Testing facility not discreet |
| • Testing availability | ||
| • Prison testing | ||
| Entry into HIV care/early care | ||
| Patient-level | • Know it is the right thing to do | • Drug addiction |
| • Want to get educated | • Fatalism; depression / trauma | |
| • Family / good friends support | • Adverse medication reactions | |
| • Want to stay healthy, general | • Shame, guilt, embarrassment | |
| • Want to stay healthy for children | • Family does not know | |
| Provider-level | • Caseworker/counselor support Positive provider attention • Taken care of by hospital coworkers | • No HIV education provided by MD • Having to change to HIV doctor • Being “lectured” to by doctor |
| Clinic-level | • Positive clinic attributes | • Lack of privacy / clinic not discreet |
| • Someone with you at diagnosis | • Travel inconvenient | |
| • Someone guide you through process | • Many complicated steps to get into care | |
| • Clinic in discreet location | ||
| • Help paying for medicine / services | ||
| • Specialized programs for women | ||
| Community-level | • Prison—supportive environment for diagnosis and treatment | • Community-level stigma |
| • Support groups / group home | ||
| Engagement in care | ||
| Patient-level | • Knowledge that HIV care works | • Appointment system failed |
| • Knowing not going to die | • Medicine makes sick/feel ill | |
| • Personal system for keeping appointments | • Sick; didn't feel like coming in | |
| • Family support | • Other family responsibilities | |
| • Getting off/staying off drugs | • Addiction; hopelessness; depression | |
| • Faith/religion | • Other medical needs trumped HIV care | |
| • Becoming familiar with routine care | • Felt too good to come in | |
| • Missed last appointment; personal sense needed to come to this one | • God taking care of health | |
| • Dislike blood work | ||
| • Personal forgetfulness | ||
| Provider-level | • Positive relationship with provider | • No barriers identified |
| • Positive relationship with clinic staff | ||
| Clinic-level | • Clinic conveniently located | • No clinic-provided reminder |
| • Clinic co-located with other services | • Clinic changed appointment time | |
| • Clinic provides reminders | • Appointment at inconvenient time | |
| • Support groups / therapy | • No child care | |
| Community-level | • Caseworker support • Had help with transportation | • Lack of transportation; transportation very inconvenient; no money for gas |
| • Bad weather | ||
Bold text indicates three or more women spontaneously offered same factor.
“Found somebody that, you know, that I knew I—At the time I wanted to spend the rest of my life with. And we both made the choice to go get tested at the same time. He came up negative, I came up positive.”
The individual-level barriers to HIV testing included ignorance as to the risk factors/behaviors associated with HIV acquisition, not really wanting to know if she is HIV-positive, active drug addiction, and fear/stigma.
“Don't say, don't just ‘do the test.’ Do the test because you're gonna have treatment. Because this treatment gonna help you. Because we gonna help you. Because this is the first step, the second step. But they goes, ‘Just do the test.’ So you get scared.”
This participant noted that messages to get tested for HIV alone were not helpful, and without additional information about HIV treatment and support, actually contributed to fear among women who were not aware of their HIV status.
No provider-level barriers to testing were identified by women, because most of the women interviewed did not have a pre-existing relationship with a physician at the time of HIV testing. Of those with physicians, having a good relationship was described as facilitating HIV testing.
At the clinic level, women wanted guidance in getting through the testing process and more preparation for what to expect. They also noted that they wanted testing to be part of their annual exam:
“I think it should be a part of your yearly physical, just general blood work that they do. You know what I'm saying? When you go for your yearly physical or whatever, they check your glucose, your cholesterol, blood pressure, sugar level, things of that nature. I think that should be one of the tests that is just a part of the norm.”
Knowledge of testing importance and opportunities at the community levels were considered facilitators to getting tested. Women suggested that advertising community-testing sites would promote testing among HIV-positive WOC. They also noted that a lack of discretion of the testing facility was a barrier to HIV testing.
“See, where I got tested at, everybody knew if you go to that place, you were—you had some kinda…. It was a clinic. The health department. Because I'm from a small town…I still went, but it was hard for me to go. I would lie and if I see somebody in there, I would leave before they called me. It didn't make sense—now it don't, but then, it did.”
The availability of testing sites was important, but the attributes of these testing facilities, including discretion and convenience, are perhaps equally important.
Entry into HIV care
In general, respondents indicated they knew becoming engaged in HIV care was the “right thing to do” and they wanted to become healthy and educated about the disease in order to stay healthy for themselves and for their children. One woman noted:
“I thought my life was over, but him [my husband] doing his research and stuff, he assured me like ‘no, they have people who have been living with this for years, and they still around, and you're young, you're going to be able to live with it years too.’ So my husband, he played like a big major role in my accepting it and being able to live with it easier I should say.”
Awareness of these motivations, and support for them during early engagement, may help facilitate appropriate HIV care for women of color. However, patient-level barriers to HIV care were also present. Women who attempted to become engaged in treatment, but found themselves intolerant of the HIV medication, reported difficulty remaining in care. Depression, addiction, and fatalism formed powerful barriers to entering HIV care, especially following trauma.
“It was hard for me. It was never easy from the first appointment because of the shame and the guilt and embarrassment. So it was hard to go for me to go to my second and third appointment.”
This sentiment was expressed by one of three women who described being raped prior to becoming diagnosed with HIV.
At the provider level, having a supportive provider, caseworker, or counselor helped women attend their early HIV appointments. But not all provider interactions were seen as supportive during early care. If early interactions with providers did not convey optimism about the efficacy of treatment and how to go about seeking treatment, entry to care was delayed.
“Actually, the doctor that spoke with me when I first found out was the OB/GYN doctor [name] down in [county name]. And he sent me to see his nurse, if she would've just followed up with me because she told me, but she didn't give me any information about clinics or anything, I'd never found out about clinics. It wasn't until I went to treatment to [town name], I went to a drug and alcohol treatment center, and it wasn't until then I found out about treatment for HIV and the Ryan White Foundation and the different things that was in place for people that were HIV positive.”
This was the information received by one woman who reported she delayed seeking treatment because she was not aware of the care options available to her. After being tested and while considering engagement in care, women reported it was critical that they heard optimism for their future longevity and received information about the effectiveness of treatment; this proved to be a defining moment for many women that shaped their care trajectories for years.
“When I first found out I had HIV, I didn't accept it. I didn't want to accept it. I used to come to appointments. I used to walk out. I didn't see the doctors or anything because I didn't want to accept it. And now, I finally accepted it and they explained it to me. I can live a long time.”
Women reported that providing care-related information early and often can help facilitate women's successful engagement in HIV treatment.
Clinic-level factors could facilitate or impede care engagement as well. Positive clinic attributes, such as friendliness, professionalism, warmth, and discretion were helpful for women of color as they entered care.
“I started to just leave the clinic, but they made me feel comfortable. That's why I kept coming. And then, talking with the doctors, and the social workers, and everybody.”
Clinic representatives, including front desk staff, social workers, nurses, and providers all play an important role in encouraging care entrance. Conversely, a lack of privacy or discretion kept some women from wanting to return to future appointments.
“Oh Lord, I'm up in here in [city's name], and all my family will come to [city's name], ‘cause they're gonna see me sitting here in this thing, say, ‘ID clinic. Why was you in the ID clinic? What does that stand for?’ and all like that.”
Clinic-level attributes could both facilitate and discourage women's successful entrance into and engagement in care.
Relatively few community-level factors were noted for entry into HIV care. Having community support services for HIV-positive women of color, including group homes, was considered helpful for early HIV-care. Community-level, HIV-related stigma was widely cited as a barrier to becoming engaged in care.
Engagement in care
Women reported the key to staying in care was their experience with treatment effectiveness and their profound belief that if they stayed in treatment, they would not die prematurely from HIV.
“I guess because I'm used to being HIV positive…and I want to get better. My health, as long as you take the medicine, you have a longer chance of living. It's just more of a chance, you have a greater chance to than if you're not taking the medicine and stuff.”
Although depression, hopelessness, and addiction continued to plague many of our respondents, those who were able to get mental health and addiction treatment found themselves able to remain continuously engaged in care. Many women also cited family support, a personal organization system, and faith as facilitators to appropriate care engagement. Engagement in care was harmed when personal organizational systems broke down or when other conditions, such as family responsibilities or other health needs, were prioritized over HIV care. Women also noted they were challenged to attend their HIV appointments when they felt sick or their HIV medicines made them feel bad. And while many women credited faith and religion for helping them stay engaged in HIV care, some used their faith to justify not coming in for appointments:
“The medicine and the doctors, that's not my main priority of keeping me well. It's God. That's for me. You know, I have to come to that point.”
Provider relationships were uniformly cited as one key to remaining engaged in care. Virtually all women who participated in the qualitative data collection, and were engaged in care, identified the importance of the provider-patient relationship for care engagement.
“Yeah. My doctor(s)…Like I could talk to them about anything, any questions I have, I get an answer, it being medical or personal—they're like always there. So it's like I always have a shoulder and an ear.”
Once women are engaged in care, and were in an ongoing partnership with a provider and clinic, provider-level barriers cease to be noteworthy. No provider-level barriers to care engagement were identified by these women.
Many women noted that care engagement was facilitated by a conveniently located clinic, either along transportation routes or near other services/amenities, along with the clinic providing appointment reminders, being co-located with other relevant services (e.g., pharmacy) and providing support groups/therapy. Clinic-level barriers to care engagement occurred when appointment reminder systems failed, appointment times were changed or were scheduled for inconvenient times, childcare was unavailable, or clinic scheduling failed to account for patient flow.
“Because if your appointment is at 9:30, and they said come fifteen minutes early, you left fifteen minutes early, but yet you still got to wait to get checked in, because the people that's coming out, to check out, they're standing there. And then all of a sudden, you late for your appointment.”
Community-level facilitators were not very important for the HIV-positive WOC during engagement-in-care. A few were mentioned (e.g., caseworker support and help with transportation) but none by more than a couple of women each. The biggest barrier cited by women at the community level was the lack of transportation for HIV appointments.
“I'd say it was my transportation, because I have to come from [city name]. And then my thing is, I mean with public transportation,…I have to get on the [bus name] bus. And then from the (bus name) bus I have to get on the [different bus name]….Let me say today, like since I had to get here at twelve…I had to leave the house at eight o'clock.”
While lack of transportation can be considered an individual-level barrier, the lack of efficient, accessible public transportation represents a community-level barrier to heath care.
In revisiting the conceptual model that underlies the research presented here (Fig. 1), we found our participants' reported barriers and facilitators at four socio-ecological structural levels, patient-, provider-, clinic-, or community-level, which correspond well to the categories employed by Cooper in her model of health disparities.14 The individual-level barriers and facilitators map quite cleanly to the patient-level factors identified by the qualitative research participants and many of Cooper's barriers were also cited by our WOC, including their prior involvement in care, health behaviors, attitudes and beliefs, and literacy levels. The mediators in Cooper's model, including provider quality and treatment efficacy, were identified by the HIV-positive WOC as “provider-level” barriers and facilitators to care. The structural level barriers in Cooper's models look remarkably similar to the clinic-level barriers and facilitators that women identified, while the financial barriers can be translated into the community-level barriers and facilitators.
Discussion
In this qualitative study, we found barriers and facilitators at multiple levels of the socio-ecological framework, including patient-, provider-, clinic-, and community-levels. Further, women reported that the important barriers and facilitators to HIV care differed by their stage of HIV care. Important facilitators to getting tested for HIV, for which “important” is defined as multiple women offering the same factor independently, occurred at the patient- and community- levels, indicating communities can play important roles in both facilitating and impeding HIV testing. The important facilitators for entry into and early HIV care occurred at all four levels, but the bulk of both barriers and facilitators occurred at the individual and provider levels. These findings suggest that individual support and building a good provider relationship can influence women's entry into and early HIV care. By the time women were engaged in care, the nature of both the barriers and facilitators were different from early testing and care experiences. Individual-level facilitators to engagement in care continued to be important, as were provider-level factors. It was interesting to note that no provider-level barriers to engagement were noted by these women for this stage of HIV care, suggesting that by the time women are engaged, they found providers with whom they are comfortable working. The community-level barriers to care also changed from fear of community-stigma to more community structural (lack of transportation) issues.
Despite many barriers and facilitators being specific to an individual's location on the continuum of care, some were important across time and stage of diagnosis. One facilitator that was apparent across the care continuum was a woman's attention and focus on her health. During the testing phase, this focus may have begun with awareness that she was sick and needed to be cared for, but following testing, the desire to stay healthy became and remained an important facilitator for HIV care. A second important facilitator was having a positive relationship with a provider. The provider role was slightly different at different stages of the continuum; for instance, the positive provider role at the testing stage was one of encouraging the women to get tested. In the early care stage, it was one of reassurance and knowledge, while during engagement it transitioned to one of partnership in care. Despite its morphing over time, a positive relationship with a provider remained an important facilitator for HIV care. The importance of the patient–provider relationship has been noted in other work,28 including qualitative work conducted in the U.S. South.29 Barriers to HIV engagement were also evident across the HIV care continuum. Drug addiction was a force capable of derailing women and their care regardless of where they were in the HIV care process. Women also reported depression or other related psychosocial attributes (fear, stigma) as being barriers to both getting into and staying in HIV care. Another important barrier over time was clinic discretion. Women reported the importance of protecting their privacy at all stages of HIV care. Clinic location and overt naming could impair the ability to become engaged in HIV care. The barriers and facilitators that appear to transcend stage of care are important to be aware of because supporting these cross-stage facilitators to care or intervening on the constant barriers can support HIV care across a woman's lifespan with greater impact.
While providing a critical perspective on the barriers and facilitators to HIV care across the HIV care continuum, the research reported here is not without limitations. These qualitative data asked women to recall historic events and their responses may be subject to recall bias. In addition, participants may have sought to please the interviewer through their responses, so their responses may also be biased for this reason. Importantly, despite efforts made at relationship- and trust-building during the conversations, there may still be critical barriers (or facilitators) that women were reluctant to talk about in these settings; therefore, we may be missing salient barrier or facilitator information. One important barrier noted in Cooper's model that did not spontaneously arise from research participants was poverty. This is undoubtedly a major barrier that contributes both directly and indirectly to difficulties. We were able to capture this and other demographic characteristics through a survey in order to provide the context in which to review women's qualitative responses. The final limitation to this research reported here is our discussion of the extent to which depression plays a critical role in women's HIV care engagement. Through both focus groups and quantitative findings we have learned that depression colors women's engagement along the entire care continuum; thus, we have opted to address it in a separate article. While underexplored in this article, we recognize that depression is a critical co-morbidity that functions as a barrier to care engagement, which warrants more research.
We believe the limitations reported above are more than offset by the overall findings and strengths of this study. We obtained broad representativeness in our qualitative sample. We also employed skilled and experienced focus group and individual-interview facilitators. The consistency of themes across participants suggests that the salient items were identified and we approached saturation for many of our themes. We also obtained thematic consistency across two data collection approaches (focus group and semi-structure individual interviews), which indicated the themes we identified were independent of data collection method. The congruence of findings across both qualitative data collection methods and the more quantitative check list also indicates the themes we identified through this research are robust to methodological approach and consistent with other published work employing different methods.30 While Cooper's thinking has been previously applied to HIV work,31 her model of health disparities has been more widely applied. We view the expansion of this model into HIV to be an important contribution this article makes to the larger literature on HIV and health disparities.
The National HIV/AIDS strategy, written by the Office of AIDS Policy in 2010 outlines the public health goals for a national approach to HIV.32 The policy acknowledges that women carry a significant portion of the health care burden of HIV and states that HIV is a disease with profound health care disparities. The research reported here has expanded on prior barrier and facilitator literature by identifying the levels at which barriers exist (individual-, provider-, clinic-, and community-levels) across multiple points of the HIV care continuum (testing, entry into and early care, engagement in care) for HIV-positive women of color. Understanding these barriers can also help inform where along the HIV cascade women of color fall out of care.11,12 These findings provide important information to policymakers seeking to construct effective strategies for combatting the differential burden of HIV among women of color and suggest possible points of intervention.33 We believe medical care and HIV support systems will be more successful recruiting and retaining HIV-positive women of color in care if we attend to some of these critical barriers and facilitators.
Acknowledgments
This research was supported by funds from HRSA's Special Projects of National Significance program (HA15148), UNC Centers for AIDS Research (P30-AI50410), and the Clinical and Translational Science Award program of the Division of Research Resources, National Institutes of Health (UL1RR025747). We thank Kimberly Walker and the Southeastern AIDS Education and Training Center, the UNC HIV Cohort Database team, especially Brant Stalzer and Sonia Napravnik, for assistance with clinical data retrieval, and J Seay for assistance with data collection. The authors also acknowledge the clinic staff, providers, and patients for their invaluable contributions to this research.
Author Disclosure Statement
EB Quinlivan, LC Messer, N DeSousa, N Bowditch, A Adimora, K Roytburd, and H Parnell have no conflicts of interest to report. This study was conducted with the approval of the University of North Carolina–Chapel Hill and Duke University Institutional Review Boards.
References
- 1.Aziz M. Smith K. Challenges and successes in linking HIV-infected women to care in the United States. Clin Infect Dis. 2011;52:S231–237. doi: 10.1093/cid/ciq047. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention [CDC] Leading causes of death by age group, all females-United States, 2007-2012. http://www.cdc.gov/women/lcod/2008/08_all_women.pdf. [Oct 21;2012 ]. http://www.cdc.gov/women/lcod/2008/08_all_women.pdf
- 3.Centers for Disease Control and Prevention [CDC] HIV/AIDS among women. Atlanta, GA: Centers for Disease Control and Prevention [CDC] 2008. http://www.cdc.gov/hiv/topics/women/resources/factsheets/pdf/women.pdf. [Oct 21;2012 ]. http://www.cdc.gov/hiv/topics/women/resources/factsheets/pdf/women.pdf
- 4.Whetten K. Lesserman J. Whetten R, et al. Exploring lack of trust in care providers and the government as a barrier to health service use. Am J Public Health. 2006;96:716–21. doi: 10.2105/AJPH.2005.063255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pence B. Mugavero M. Carter T, et al. Childhood trauma and health outcomes in HIV-infected patients: An exploration of causal pathways. J Acquir Immune Defic Syndr. 2012;59:409–416. doi: 10.1097/QAI.0b013e31824150bb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Whetten K. Leserman J. Low K, et al. Prevalence of childhood sexual abuse and physical trauma in an HIV-positive sample from the deep south. Am J Public Health. 2006;96:1028–1030. doi: 10.2105/AJPH.2005.063263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention [CDC] HIV surveillance in women. Atlanta, GA: Centers for Disease Control and Prevention. 2012. http://www.cdc.gov/hiv/topics/surveillance/resources/slides/women/index.htm. [Oct 21;2012 ]. http://www.cdc.gov/hiv/topics/surveillance/resources/slides/women/index.htm
- 8.Prejean J. Song R. Hernandez A, et al. Estimated HIV incidence in the United States, 2006–2009. PLoS One. 2011;6:e17502. doi: 10.1371/journal.pone.0017502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Swejda D. Scofield J. Directors NAoSaTA. The landscape of HIV/AIDS among African American women in the United States. 2008.
- 10.Cheever L. Lubinski C. Horberg M, et al. Ensuring access to treatment for HIV infection. Clin Infect Dis. 2007;45:S266–274. doi: 10.1086/522549. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention [CDC] Clinical and behavioral characteristics of adults receiving medical care for HIV infection. Medical monitoring project, United States. 2007. http://www.cdc.gov/mmwr/preview/mmwrhtml/ss6011a1.htm. [Oct 21;2012 ]. http://www.cdc.gov/mmwr/preview/mmwrhtml/ss6011a1.htm [PubMed]
- 12.Marks G. Gardner L. Craw J, et al. Entry and retention in medical care among HIV-diagnosed persons: A meta-analysis. AIDS. 2010;24:2655–2678. doi: 10.1097/QAD.0b013e32833f4b1b. [DOI] [PubMed] [Google Scholar]
- 13.McLeroy K. Bibeau D. Steckler A, et al. An ecologic perspective on health promotion programs. Health Educ Q. 1988;15:351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 14.Cooper L. Hill M. Powe N. Designing and evaluating interventions to eliminate racial and ethnic disparities in health care. J Gen Intern Med. 2002;17:477–486. doi: 10.1046/j.1525-1497.2002.10633.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bing E. Burnam M. Longshore D, et al. Psychiatric disorders and drug use among human immunodeficiency virus-infected adults in the United States. Arch Gen Psychiatry. 2001;58:721–728. doi: 10.1001/archpsyc.58.8.721. [DOI] [PubMed] [Google Scholar]
- 16.Pence B. Reif S. Whetten K, et al. Minorities, the poor, and survivors of abuse: HIV-infected patients in the US deep south. South Med J. 2007;100:1114–1122. doi: 10.1097/01.smj.0000286756.54607.9f. [DOI] [PubMed] [Google Scholar]
- 17.Catz S. Mcclure J. Jones G, et al. Predictors of outpatient medical appointment adherence among persons with HIV. AIDS Care. 1999;11:361–373. doi: 10.1080/09540129947983. [DOI] [PubMed] [Google Scholar]
- 18.Gardner L. Marks G. Metsch L, et al. Psychological and behavioral correlates of entering care for HIV infection: The antiretroviral treatment access study (ARTAS) AIDS Patient Care STDS. 2007;21:418–425. doi: 10.1089/apc.2006.0115. [DOI] [PubMed] [Google Scholar]
- 19.Knowlton A. Hua W. Latkin C. Social support networks and medical service use among HIV-positive injection drug users: Implications for intervention. AIDS Care. 2005;17:479–492. doi: 10.1080/0954012051233131314349. [DOI] [PubMed] [Google Scholar]
- 20.Lichenstein B. Domestic violence in barriers to care for HIV-positive women. AIDS Patient Care STDS. 2006;20:122–132. doi: 10.1089/apc.2006.20.122. [DOI] [PubMed] [Google Scholar]
- 21.Siemieniuk R. Krentz H. Gish J, et al. Domestic violence screening: Prevalence and outcomes in a Canadian HIV population. AIDS Patient Care STDS. 2010;24:763–770. doi: 10.1089/apc.2010.0235. [DOI] [PubMed] [Google Scholar]
- 22.Johnson V. Promoting behavior change: Making healthy choices in wellness and healing choices in illness. Use of self-determination theory in nursing practice. Nurs Clin North Am. 2007;42:229–241. doi: 10.1016/j.cnur.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 23.Morse J. Designing funded qualitative research. In: Denzin N, editor; Lincoln Y, editor. Handbook of Qualitative Research. Sage Publications; Thousand Oaks, CA: 1994. pp. 220–235. [Google Scholar]
- 24.Spradley J. Participant Observation. Holt, Rinehart & Winston; New York, NY: 1980. [Google Scholar]
- 25.Strauss A. Corbin J. Grounded theory methodology. In: Denzin N, editor; Lincoln Y, editor. Handbook of Qualitative Research. Sage Publications; Thousand Oaks, CA: 1994. pp. 273–285. [Google Scholar]
- 26.Hennink M. Hunter I. Bailey A. Qualitative Research Methods. Sage Publications; London: 2011. [Google Scholar]
- 27.Hsieh H. Shannon S. Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 28.Squires KE. Hodder SL. Feinberg J, et al. Health needs of HIV-infected women in the United States: Insights from the women living positive survey. AIDS Patient Care STDS. 2011;25:279–285. doi: 10.1089/apc.2010.0228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kempf M. McLeod J. Boehme A, et al. A qualitative study of the barriers and facilitators to retention-in-care among HIV-positive women in the rural southeastern United States: Implications for targeted interventions. AIDS Patient Care STDS. 2010;24:515–520. doi: 10.1089/apc.2010.0065. [DOI] [PubMed] [Google Scholar]
- 30.Smith L. Fisher J. Cunningham C, et al. Understanding the behavioral determinants of retention in HIV care: A qualitative evaluation of a situated information, motivation, behavioral skills model of care initiation and maintenance. AIDS Patient Care STDS. 2012;26:344–355. doi: 10.1089/apc.2011.0388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Deviuex J. Malow R. Jean-Gilles M, et al. Reducing health disparities through culturally sensitive treatment for HIV+adults in Haiti. ABNF J. 2004;15:109–115. [PMC free article] [PubMed] [Google Scholar]
- 32.Office of National AIDS Policy. National HIV/AIDS Strategy for the United States of America. Office of the White House. 2010 [Google Scholar]
- 33.Rao D. Desmond M. Andrasik M, et al. Feasibility, acceptability, and preliminary efficacy of the unity workshop: An internalized stigma reduction intervention for African American women living with HIV. AIDS Patient Care STDS. 2012;26:614–620. doi: 10.1089/apc.2012.0106. [DOI] [PMC free article] [PubMed] [Google Scholar]