Abstract
Self-determination theory examines the needs of people adopting new behaviors but has not been applied to the adoption of HIV healthcare behaviors. The current study applied self-determination theory to descriptions of healthcare behaviors adopted by ethnic minority women after an HIV diagnosis. Women of color were asked to describe their experiences with HIV testing, entry, and engagement-in-care in qualitative interviews and focus groups. Participants were mostly African-American (88%), over 40 years old (70%), had been diagnosed for more than 6 years (87%) and had disclosed their HIV infection to more than 3 people (73%). Women described unmet self-determination needs at different time points along the HIV Continuum of Care. Women experienced a significant loss of autonomy at the time of HIV diagnosis. Meeting competency and relatedness needs assisted women in entry and engagement-in-care. However, re-establishing autonomy was a key element for long-term engagement-in-care. Interventions that satisfy these needs at the optimal time point in care could improve diagnosis, entry-to-care, and retention-in-care for women living with HIV.
Introduction
Antiretroviral therapy (ART) almost completely prevents HIV transmission to uninfected heterosexual partners1 and adherence to ART is life-saving.2 Yet, 25–30% of HIV infected people in the United States are unaware of their infection, and each year over 50,000 new infections and 10,000 deaths occur.3–5 To use ART effectively to prevent either illness or HIV transmission, HIV-infected persons must be aware of their infection, engage in HIV care, and become adherent to medications. Ideally, movement through these steps, referred to as the HIV Continuum of Care,6 happens smoothly: the person is rapidly diagnosed through testing, is linked to and quickly enters in HIV care, efficiently receives ART, and promptly achieves long-term virologic suppression. Instead of this ideal Continuum, more than 50% of people with HIV either fail to enter care, receive sporadic care, or are lost to care for periods of time.5 HIV-infected black women experience twofold greater mortality7 compared with non-black women, suggesting that black women experience even greater delays in the movement into and through the Continuum of Care. Delays in linkage-to-care result in more advanced disease, higher risk of AIDS, and death, while poorer retention-in-care rates are associated with lower rates of HIV virologic suppression and survival.8,9 Thus, knowledge of HIV status alone will not achieve optimal health outcomes. Rather, achievement of optimal health outcomes requires full engagement in care, which in turn, requires directed personal and healthcare system efforts.
Becoming effectively engaged in care is not a simple act and it requires many new and modified health behaviors. The Self-Determination Theory is a model10 of behavior change that examines the concept of motivation. New behaviors may be changed in the presence of extrinsic motivators but will not be sustained until there is intrinsic motivation and the behavior has value and meaning. Behaviors gain value and meaning when persons feel competent, autonomous, and connected. Interventions designed to address these core needs11 have been used to assist people with exercise, smoking, and glucose control.11–18
Recent reports suggest that relationships with HIV medical providers are important, even critical.19 Yet, women report insufficient reproductive health information from their providers, leading to increased sexual risk behavior.20 A small survey of 37 HIV providers reported more “frustration” with women patients compared with men and rated women as less educated, rational, responsible, compliant, independent, and direct compared with male patients.21 The generalizability of these findings is unknown, but failure to recognize key information needs of women and having more frustrating interactions with women may reduce opportunities to provide relatedness support in the clinical setting. Low levels of relatedness support may help explain why women are less likely to effectively engage in HIV care than men, which would be consistent with Self-Determination Theory.10
We hypothesized that the core needs of self-determination are present in the experience of HIV testing, entry into and engagement in care, and to our knowledge, this hypothesis has not previously been explored. As part of a national initiative for HIV-infected women of color, “Enhancing Access to and Retention in Quality HIV Care for Women of Color”, we conducted a series of focus groups and qualitative interviews with HIV-infected women of color to understand women's experience with HIV care. Using these qualitative findings, this article will address the following research questions: (1) Are the core needs for self-determination (autonomy, relatedness /connectedness, and competency) experienced during the process of testing and engaging in HIV care? (2) Does the relative importance of the core needs vary during the three phases of the Continuum of Care, testing, entry-to-care and retention-in-care?
Methods
Study participants
The research was conducted in an academic Infectious Diseases clinic in North Carolina in 2010. During that year, the clinic provided HIV care to more than 1700 HIV-infected people, with 58% African-American (AA), 10% Hispanic and other minorities, and 31% women, consistent with the HIV epidemic in North Carolina. Women were recruited to participate by flyers or provider referral and eligible if they were: HIV-infected, women of color (AA, Native Americans, or Latinas), able to communicate in English, and 18 years of age or older. Following two focus groups (n=11), we then offered semi-structured qualitative interviews (in-person or by phone, n=19) to increase representation of those not represented in the focus groups (younger, more recently diagnosed, employed, or those who would not participate in a group). The final sample (n=30) falls within the recommended parameters for a qualitative research sample.22
Data collection procedures
We asked women to describe their experiences with the HIV care system at specific time points: diagnosis experiences (testing), the time period during which they were waiting for their HIV testing results and early experiences in HIV care (entry); and chronic HIV care (retention/engagement) using a semi-structured interview guide. An experienced facilitator with field note-takers conducted the focus groups (approximately 2 h)23 and an experienced interviewer conducted the 30–60 min semi-structured interviews. All interviews and focus groups were digitally recorded, transcribed verbatim, reviewed, and corrected. The University of North Carolina at Chapel Hill Institutional Review Board approved all procedures for the study. Since a breach of confidentiality from a signed consent form was the major potential risk for participants in the study, a waiver of written consent was obtained from the Institutional Review Board.
Data analysis
The approach to data analysis was informed by grounded theory methodology,24 in which specific themes and codes emerge during the first step of data collection. This approach was chosen to avoid imposing preconceived notions of what constituted relevant barriers on the data provided by the women. First, each transcript (focus group or interview) was independently read for overall meaning and content-coded by members of the analytic team using traditional systematic manual open-coding content analysis adapted from grounded theory strategies. A second review of the transcripts used a directed content analysis approach25 to identify content units that contained words (see below) that suggested a self-determination need. Next, the content units from the initial review were also examined for themes that represented a self-determination need that was expressed without use of the selected key words. Abstracted content units from both reviews were then coded to identify self-determination need, character of the need and reference time in the continuum of care. Following this, a content analysis summary of the expressions of self-determination needs in relationship to the continuum of care was created. The numerical data were used to provide additional information supporting the internal generalizability of the observations and to identify the patterns that were not discernible otherwise when looking at the content units.26 Finally, self-determination content units were re-read for sub-themes and commonalities, including high, low and intermediate levels of each self-determination need. At each step the coding authors (EBQ, LM) discussed the coding, identified areas of discrepancy, and discussed them to resolution. Trustworthiness of the data was established by discussing the data at interim analysis steps with the authorship group, all of whom had experience with the patient population and provided feedback on interpretations. Selecting quotations that represented the key ideas in the richest language was used to maximize the transferability of our findings. Dependability was established by record keeping of the coding processes and frequent returns to the original language in the transcripts.
Autonomy
According to self-determination theory, psychological autonomy refers to a sense of independent will or volition and implies the ability to make choices for one's self. Apathy and low levels of self-care autonomy occur in situations of powerlessness. Autonomy support includes having open dialogues with patients, encouraging questions, and participation in joint decision-making. Transcripts were reviewed for expressions of powerlessness (not wanting, not accepting, can't, giving up), empowerment/ autonomy (want, choose, chose, choice, enjoy, ask, decide, decision) and the provision of autonomy support by providers (listens, accepts me, answers questions) by reading for these concepts and searching for related words.
Competency
Competency and self-efficacy are related concepts where self-efficacy is the belief that one can complete a task and competency refers to the actual ability to do so. Transcripts were reviewed for words indicating competency (able, ability, willing, know, knowledge) and read for descriptions of experiences with competency or lack of competency.
Relatedness
Patients' sense of relatedness is met in healthcare settings where they feel welcomed and respected and time is taken to build a relationship. We searched for the terms “doctor,” “provider,” and “nurse” to look for relatedness needs. Positive descriptions of interactions with the provider or staff were interpreted as a proxy for a sense of relatedness; negative descriptions of interactions with providers or staff were interpreted as a sign of low-level relatedness with clinic staff.
Results
Participants
Eleven respondents participated in focus groups and 19 respondents participated in individual interviews using the same interview guide (Table 1). Four women, who were younger than 30 years old or recently diagnosed, received targeted invitations to participate in the study. Women who were employed full-time (n=11) were able to participate in interviews but not the focus groups. Two-thirds of the 30 participants were over 40 years old, and 88% were AA.27 Most women were diagnosed more than 6 years before the interview (87%), had disclosed their HIV infection to more than three people (73%), had a high school education or less (HS or <HS: 70%; >HS: 30%), were currently single (single/divorced/separated/widowed and not dating: 53%), and were unemployed (63%).
Table 1.
Demographic Characteristics of Participants
| Focus groupnumber (%) | Interviewnumber (%) | |
|---|---|---|
| Race/ethnicity | ||
| African American | 10 (91%) | 15 (85%) |
| Puerto-Rican, Hispanic | 1 (9%) | 2 (10%) |
| Other, multiracial | 0 (0%) | 2 (10%) |
| Age (years) | Mean age: 49.5 | Mean age: 42.1 |
| 20–39 | 1 (9%) | 8 (42%) |
| 40–49 | 5 (45%) | 7 (37%) |
| 50–69 | 5 (45%) | 4 (21%) |
| Education | ||
| Less than a high school degree | 4 (36%) | 5 (26%) |
| High school degree | 3 (27%) | 9 (47%) |
| More than a high school degree | 4 (36%) | 5 (26%) |
| Relationship status (multiple) | ||
| Single, not dating | 5 (45%) | 8 (42%) |
| Separated/divorced/widowed, not dating | 1 (9%) | 2 (11%) |
| Married, living with partner | 2 (18%) | 6 (32%) |
| Dating | 3 (27%) | 3 (16%) |
| Employment status | ||
| Full-time (no part-time workers) | 0 (0%) | 11 (58%) |
| No employment | 11 (100%) | 8 (42%) |
| Time since HIV diagnosis | ||
| > 6 years ago | 10 (91%) | 16 (84%) |
| 4–6 years ago | 1 (9%) | 2 (11%) |
| 1–3 years ago | 0 (0%) | 1 (5%) |
| HIV disclosure | ||
| No one | 0 (0%) | 1 (5%) |
| 1–3 people | 2 (18%) | 5 (26%) |
| 4–9 people | 2 (18%) | 3 (16%) |
| ≥ 10 people | 7 (64%) | 10 (53%) |
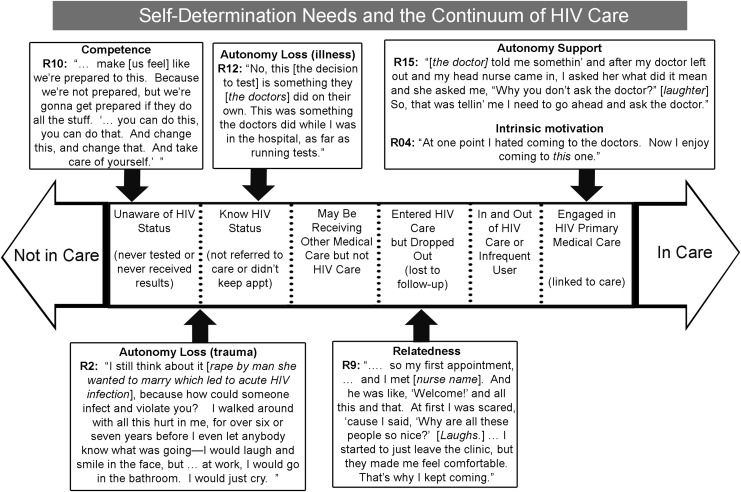
HIV Continuum of Care and the self-determination needs
To identify relationships between the continuum of care and the expression of self-determination needs that might not be apparent when examining only content, and to enhance the generalizability of the observations, a numerical content summary was performed. Each description of a core need was assigned to one of the three phases of care (testing, entry, and retention) based on what aspect of HIV was being described by the speaker (Table 2). Overall, 172 descriptions of core needs were expressed, and at each of the three phases, more than three-fourths (n=23 or more) of the interviewees described one or more of the core needs. When describing testing experiences, 22 and 24 women expressed competency and autonomy needs, respectively, whereas very few women discussed relatedness (n=3). At entry to care, competency (n=24) and relatedness needs (n=24) predominated. When responding to questions about staying in care, autonomy (n=28), and relatedness (n=17) were more commonly described than a competency need (n=14).
Table 2.
Number of Women Who Reported Self-Determination Needs During Testing, Entry-to-Care, and Retention-in-Care
| |
Self-determination needs |
||
|---|---|---|---|
| Continuum of Care | Autonomy | Competency | Relatedness |
| 1. Testing | 24 | 22 | 3 |
| 2. Entry | 16 | 24 | 24 |
| 3. Engagement | 28 | 14 | 17 |
Testing
To understand the self-determination needs through the Continuum of Care Model, we examined the content of the women's statements by three key phases in this Continuum: testing, entry-to-care, and retention-in-care (Fig. 1). Competency was especially important when women first learned of their HIV diagnosis; it helped them accept a referral to care and begin learning to manage their illness. In the absence of competency, women reported, “all I knew is that people were dying.” and “… make [us feel] like we're prepared to do this [take an HIV test]. Because we're not prepared [to manage our HIV], but we're gonna get prepared if they do all the stuff.” HIV competency has the power to be life-saving at times. One woman's inability to educate her family members about the safety of non-sexual interactions put her at risk of committing suicide. She required hospitalization for suicidal thoughts when her children isolated her from her grandchildren: “[They said] ‘my kids can't be around you, because they said this is gonna catch.’ ”. Participants also reported that providers failed to counsel them about care, prognosis and treatment and sent them away without education, “sent me on my merry way.” Another woman, who had been trained as an HIV educator, used her knowledge to seek testing in an alternative medical location after being given the diagnosis of influenza. She became ill after being raped, and this prompted her to seek the assistance of an HIV specialist.
FIG. 1.
Self-determination and the HIV continuum of care. Reprinted with permission from Cheever (2007).
“… Three days after [I was raped], I got so sick.…[My doctor said] ‘Oh [Name], it's the flu.’ So I went to…an HIV specialist. He said, ‘I don't know what you've been into,’ he said, ‘but the HIV's just entered your body.’ ”
Education also reduced passive suicidal thoughts. “At first I had to get educated…then I became more willing to want to live.” The most requested educational message was that testing led to treatment and a reasonable expectation for a normal lifespan.
Testing was a time when many women first experienced profound helplessness. Hearing a diagnosis of HIV-infection without a plan for treatment could lead to a sense of fatality. HIV testing during acute illness, although potentially life-saving, may create a perception of powerlessness. One woman described the experience:
“Because as I start coming back to myself, out of something like a coma state, that's when I was hit with it that I was HIV.…And then when I kind of sorted it out, I said, “Well, I'm going to die with something,” so when I did get out of the hospital, I went right back to street drugs.”
Experiences of trauma (rape and betrayal by partners, etc.) exacerbated feelings of powerlessness and loss of autonomy. When infected after partner violence and a sexual assault, women said:
“ ‘cause I was in denial like ten years, first. Like I don't have it, and didn't want to take no pills.”
Another woman reported on the association between being tired of taking medications and depression:
“I still think about it [rape], because how could someone infect and violate you? I walked around with all this hurt in me, for over six or seven years…—I would laugh and smile in the face, but…at work, I would go in the bathroom. I would just cry.”
Receiving an HIV diagnosis after a partner's presumed infidelity, another woman said:
“It probably would have been easier if I had went on my own to have it tested but…The guy that I was dating just up and told me he was HIV-positive and that I needed to go be tested. I had been with him for ten years.”
These betrayals contributed to powerlessness and women linked these experiences with subsequent delayed entry into or failure to engage in care. Low health literacy (unawareness of the benefits of treatment) contributed to hopelessness (“I automatically took that frame of mind of death, so I continued on to do the things that I was doing ”). Many women reported being pushed by events such as pregnancy, betrayal, or illness that suggested the need for HIV testing. Thus, at a time when empowerment is critically needed, women experience HIV testing as just the opposite–an experience that reinforces powerlessness.
Fear of accidental disclosure of HIV infection was an additional source of stress that left women feeling helpless and unable to access care.
“… I just refused to go. And then what made me start coming regular and stuff is I had got real bad sick, and then I had to be hospitalized for a good three months.…[because]…if it was my mom taking me I didn't mind, but anyone else I didn't want them taking me there.”
Despite her description of these actions as “crazy,” this woman was unable to act differently. Other women described similar feelings of paralysis. Stigma and a fear of being stigmatized were powerful negative external factors that overwhelmed women's abilities to make autonomous decisions about medical care.
However, proactive decisions to seek help that would lead to engagement in care were also described.
“And I had time to think while I was in [prison], so that's what made me come to the situation and…I wanted to live.”
and
“… then when I decided to get help, and I started talking [in therapy]. And that's one of the reasons why I'm in this clinic today.“
These decisions, motivated by personal intrinsic values and goals, were critical points in obtaining HIV care and led to long term retention-in-care.
The testing and diagnosis phase was marked by descriptions of powerlessness, loss of autonomy, and a need for competency. Participants reported that knowledge of testing opportunities in their community facilitated testing for them and indicated that advertising testing sites and offering routine annual testing would promote testing competency among women.
Entry-to-care
Women rarely described a relationship that influenced the testing process. However, when entering care, the relationship with provider or knowledgeable staff was described as very important. Stigma influenced many of the experiences but one of the most profound was the physical act of entering the clinic. This was very difficult for women: they left without being seen, wanted to whisper, hid their face behind newspapers, books, and doors. One woman pantomimed this painful interaction while all the focus group members laughed heartily in acknowledgement of their shared painful experiences.
… I was vexed, ‘cause I don't want nobody to see me [inaudible]. And then when I come out, I would stick my head out. And then just run on out. They're like, ‘Oh girl, where you been?’ …“I went around there to the bathroom, and got lost.’ ”
Despite the emotional stress experienced when entering the clinic, efforts by staff to be supportive made a difference. When relatedness was communicated, women described a strong connection to clinic with statements of trust and affection for staff, nurses, and providers. Staff at the front desk were named as resources. Nurses were consistently described as sources of information, autonomy support (“she ain't gonna look at me like it's a stupid question.”), encouragement (“don't be weary,”), acceptance (“she's seen my bad side and she's seen my good side,”), and respect (“they're so willing to help me and despite of what I've been doing,”). They saw the work that the healthcare personnel performed as an expression of caring.
“The doctors did care and the nurses and they just wasn't helping me to be helping me.…They was helping me when I wasn't helping myself, and they cared more about me than what I cared about myself. And after I seen that they cared and they was doing all they could to help me, I started caring about myself and start helping myself.”
When care for the women was effectively expressed and women were able to trust that the providers and staff genuinely cared, the women could then begin to care for themselves, knowing that they had the support of the clinic staff.
This relatedness had to be sufficiently strong to overcome the stigma most women experienced. In general, respondents indicated they knew becoming engaged in HIV care was the “right thing to do” and they wanted to become knowledgeable about the disease in order to stay healthy for themselves and for their children. However, the need to establish new health care relationships was particularly difficult at a time when many women were very vulnerable. Family members (if told of the diagnosis) were often able to provide support: “My mother helped me…took like, feel like a burden off me” and “My family was like, ‘Hey, look…It's time to get it right, whether you want help or not’ ”. Positive clinic attributes, such as friendliness, professionalism, warmth, and discretion were helpful, whereas a lack of privacy or discretion would keep women from wanting to return to future appointments. One woman described the memorable first impression her nurse made on her and his expression of “Welcome!” directed at her specifically and his ability to make her feel comfortable. This ultimately changed her mind about leaving clinic. These were very simple, yet powerful methods for providing relatedness support for patients who are entering in care; moreover, this support extended into the engagement phase.
Retention-in-care
Competency needs related to HIV were expressed with less emphasis during the engagement phase, suggesting that the needed knowledge and skills to manage HIV infection had been acquired. However, women described a significant need for logistical skills for balancing personal, economic, transportation and clinic resources and the need to have them all working simultaneously in order to get care. One woman described the interplay between her motivation and the timing of available resources when she stated that the transportation van comes when she does not feel like going but when she wants to go and be on time, the van is late. Participants described many obstacles to using the healthcare system: navigating labs, parking decks, construction and traffic and logistical skills required to work around these obstacles required practice (“… knowing your blood draws and where to get ‘em done…And then learning the parking deck and not getting lost. [It took] roughly about a year.”) and a routine (“It's like a routine part of my life now.”). Increasing HIV-specific knowledge and general healthcare navigation skills enabled some women to engage in HIV care.
Relationships with providers were strongly expressed as critical for retention but more likely to be discussed in the context of autonomy support than during testing and entry-to-care. Autonomy descriptions emphasized the need for autonomy support from providers or the acquisition of personal autonomy around HIV care rather than describing the loss of autonomy expressed during discussion of the testing and diagnosis phase. Health behavior autonomy was reflected in expressions of independence and the motivations for these behaviors were influenced by positive values (pride, happiness, satisfaction). Women who were engaged in care with intrinsic motivation to care for themselves, articulated this motivation with statements such as “decided to take care of [myself ]”, “I want to live” (12 women), “I want to be healthy”, (6 women). Engaged women no longer viewed HIV care as a burden. Instead, it was perceived as something that relieved their worry; they felt good and proud of the work they did to stay healthy.
“I feel good that I've been following this regimen, and doing what she asks of me. You know. And see the progress.”
and
“I wanted to live, so my appointments are very important to me because it lets me know what my prognoses are and how I am doing with my counts and my viral load and all of this stuff.”
and
“Yeah, I had own motivation: stay healthy.”
When women saw their clinical progress as an accomplishment of which they were proud, this complemented their sense of an autonomous partnership with their provider and internalized the motivation to stay engaged in care.
Not all women achieve this autonomy independently. Some women required specific coaching before they were comfortable acting autonomously:
“Yeah, if they tell me something, I'd leave it alone, but if I don't understand something now, I ask questions. They told me somethin’ and after my doctor left out and my head nurse came in, I asked her what did it mean and she asked me, ‘Why, you don't ask the doctor?’ So, that was tellin’ me I need to go ahead and ask the doctor.”
The expressions of “she motivates me” and “she is easy to talk to” represent a provider who supports the patient's autonomy in addition to being “sincere about helping”
“I mean, they help you out, they tell you to learn about your sickness and everything, so that's why I chose to come back here.”
Here, the availability of autonomy support from staff and providers translated into retention-in-care.
Discussion
HIV-infected women of color readily expressed the core needs of self-determination theory: autonomy, relatedness, and competency. Further, different needs were especially salient at different phases of the HIV Continuum of Care. Narratives about testing experiences consistently included the need for knowledge, such as perceptions of risk and awareness of the benefits of care. An additional important area of competency was system navigation skills. Relatedness did not appear important for testing, perhaps because participants did not have an established healthcare provider in this phase. Most importantly, for many women, testing and HIV diagnosis were done within the setting of partner betrayal or profound illness. A loss of personal autonomy occurred with HIV diagnosis in these situations, creating an experience of powerlessness, a core element of illness.28 This may make women particularly sensitive to the effects of barriers to their entry and engagement to care. Entry into care was profoundly influenced by the testing experience. Knowledge alone was rarely sufficient to bring a woman into care unless coupled with relatedness support. Stigma29,30 was a strong barrier to care entry, as it reduced social connectedness and paralyzed some women until they became severely ill. Therefore, entry into care was facilitated when relatedness needs were met by family, friends and/or healthcare staff and this stigma was overcome. The third phase, retention-in-care, was characterized by strong personal connections with providers, but long-term engagement required development of autonomy. Women experienced pride in their self-motivation and autonomy when they fully engaged in care. This suggests that recovery from the testing-related loss of autonomy occurred before engagement.
The data presented here contribute to the literature in several ways. First, this qualitative study asked women specifically about experiences and needs at different points in the HIV Continuum of Care. Most prior qualitative studies have asked women about key issues (such as stigma,24 provider relationship,31 self-management,32) without referencing the Continuum of Care, or have examined a single point on the Continuum of Care (retention-in-care or entering care19,33). Investigators have examined the constructs of the information-motivation-behavior theory of behavior change for both care initiation and retention.34 In this study, motivation was present in 92% of the response segments from patients discussing barriers and facilitators of HIV care. Anchoring the needs of women to the time frame of the Continuum of Care will allow interventions to be appropriately timed for maximum effectiveness. Second, we examined the specific phases of care in a real-world clinical care setting as opposed to examining the phases of care within a clinical trial. A prior study reported differences in entry-to-care and retention-in-care within the context of a clinical trial.35 Third, we examined the continuum of HIV care in the context of the core needs of Self-Determination Theory. Self-determination and intrinsic motivation have been examined in studies of antiretroviral adherence, including ART adherence.36,37 However, the core needs were not examined in these prior studies. This study adds to these findings by examining the role of Self-Determination Theory concepts in engagement in HIV medical care rather than medication adherence. Fourth, the Continuum of Care has been examined nationally at a population level to assess the effectiveness of current HIV care systems in the USA; however, information about specific demographic groups has not been published. The current study examined the Continuum of Care experiences of minority women and highlighted the vulnerability of HIV-infected minority women to healthcare disparities. To address the higher mortality of minority women compared with other demographic groups with HIV, the national HIV/AIDS Strategy38 will need qualitative and quantitative information about minority women's experiences in care.
While contributing to the literature in important ways, this study is not without limitations. The recall of women may have been limited by the length of time since these events occurred in their lives or biased by participants' desire to please the interviewer or other members of the group. We addressed the potential for social desirability bias by using a skilled group facilitator who was a member of the demographic community but unrelated to the clinic where the women received care. Second, because the focus groups and interviews recruited women who were attending clinic, we did not include anyone who was currently out of care or who left the clinic completely. However with probing, most women were readily able to describe periods of time when they were not engaged in care and articulated reasons for re-entry into care.
Women described unmet needs for relatedness, competence, and autonomy when navigating the healthcare system to receive care for HIV infection. The needs varied as patients moved through the Continuum of Care. Fear, compounded by a significant loss of autonomy, was experienced at the time of HIV diagnosis, while meeting competency and relatedness needs assisted women in entry and engagement in care. However, re-establishing autonomy was a key element for long-term engagement in care. Understanding the needs and designing interventions that improve the degree to which the needs are satisfied at the optimal time point has the potential to improve diagnosis, entry-to-care and retention-in-care, which are the current challenges in combating the HIV epidemic.
Acknowledgments
We thank Kimberly Walker and the Southeastern AIDS Education and Training Center for lending the focus groups, and the UNC HIV Cohort Database team, especially Brant Stalzer and Sonia Napravnik, for assistance with clinical data retrieval. The authors also acknowledge the clinic staff, providers, and patients for their invaluable contributions to this research. This research was supported by funds from HRSA's Special Projects of National Significance program (HA15148), UNC Centers for AIDS Research (P30-AI50410), and the Clinical and Translational Science Award program of the Division of Research Resources, National Institutes of Health (UL1RR025747). This study was conducted with the approval of the University of North Carolina–Chapel Hill Institutional Review Board.
Author Disclosure Statement
EB Quinlivan, LC Messer, N Bowditch, AA Adimora, K Roytburd, H Parnell, J Seay, L Bell, and J Pierce have no conflicts of interest to report.
References
- 1.Cohen MS. Chen YQ. McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365:493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Walensky RP. Paltiel A. Losina E, et al. The survival benefits of AIDS treatment in the United States. J Infect Dis. 2006;194:11–19. doi: 10.1086/505147. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. HIV surveillance—Epidemiology of HIV infection (through 2009) 2011. http://www.cdc.gov/hiv/topics/surveillance/resources/slides/general/ [Sep 22;2012 ]. http://www.cdc.gov/hiv/topics/surveillance/resources/slides/general/
- 4.Prejean J. Song R. Hernandez A, et al. Estimated HIV incidence in the United States, 2006–2009. PLoS One. 2011;6:e17502. doi: 10.1371/journal.pone.0017502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marks G. Crepaz N. Janssen RS. Estimating sexual transmission of HIV from persons aware and unaware that they are infected with the virus in the USA. AIDS. 2006;20:1447–1450. doi: 10.1097/01.aids.0000233579.79714.8d. [DOI] [PubMed] [Google Scholar]
- 6.Cheever LW. Engaging HIV-infected patients in care: Their lives depend on it. Clin Infect Dis. 2007;44:1500–1502. doi: 10.1086/517534. [DOI] [PubMed] [Google Scholar]
- 7.Murphy K. Hoover D. Shi Q. The association of race with death from AIDS in continuous HAART users: WIHS. 19th Conference on Retroviruses and Opportunistic Infections; Seattle. 2012. [Abstract 1045]. [Google Scholar]
- 8.Giordano TP. Gifford AL. White AC, Jr., et al. Retention in care: A challenge to survival with HIV infection. Clin Infect Dis. 2007;44:1493–1499. doi: 10.1086/516778. [DOI] [PubMed] [Google Scholar]
- 9.Mugavero MJ. Davila JA. Nevin CR, et al. From access to engagement: Measuring retention in outpatient HIV clinical care. AIDS Patient Care STDS. 2010;24:607–613. doi: 10.1089/apc.2010.0086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Deci EI. Why We Do What We Do: Understanding Self-Motivation. Penguin; New York City: 1995. [Google Scholar]
- 11.Ryan RM. Lynch MF. Vansteenkiste M, et al. Motivation and autonomy in counseling, psychotherapy, and behavior change: A look at theory and practice. Counsel Psychol. 2011;39:193. [Google Scholar]
- 12.Russell KL. Bray SR. Promoting self-determined motivation for exercise in cardiac rehabilitation: The role of autonomy support. Rehabil Psychol. 2010;55:74–80. doi: 10.1037/a0018416. [DOI] [PubMed] [Google Scholar]
- 13.Williams GC. McGregor HA. Sharp D, et al. Testing a self-determination theory intervention for motivating tobacco cessation: Supporting autonomy and competence in a clinical trial. Health Psychol. 2006;25:91–101. doi: 10.1037/0278-6133.25.1.91. [DOI] [PubMed] [Google Scholar]
- 14.Silva MN. Markland D. Carraca EV, et al. Exercise autonomous motivation predicts 3-yr weight loss in women. Med Sci Sports Exerc. 2011;43:728–737. doi: 10.1249/MSS.0b013e3181f3818f. [DOI] [PubMed] [Google Scholar]
- 15.Williams GC. Freedman ZR. Deci EL. Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care. 1998;21:1644–1651. doi: 10.2337/diacare.21.10.1644. [DOI] [PubMed] [Google Scholar]
- 16.Williams GC. Minicucci DS. Kouides RW, et al. Self-determination, smoking, diet and health. Health Educ Res. 2002;17:512–521. doi: 10.1093/her/17.5.512. [DOI] [PubMed] [Google Scholar]
- 17.Julien E. Senecal C. Guay F. Longitudinal relations among perceived autonomy support from health care practitioners, motivation, coping strategies and dietary compliance in a sample of adults with type 2 diabetes. J Health Psychol. 2009;14:457–470. doi: 10.1177/1359105309102202. [DOI] [PubMed] [Google Scholar]
- 18.Johnson VD. Promoting behavior change: Making healthy choices in wellness and healing choices in illness—Use of self-determination theory in nursing practice. Nurs Clin North Am. 2007;42:229–241. doi: 10.1016/j.cnur.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 19.Kempf MC. McLeod J. Boehme AK, et al. A qualitative study of the barriers and facilitators to retention-in-care among HIV-positive women in the rural southeastern United States: Implications for targeted interventions. AIDS Patient Care STDS. 2010;24:515–520. doi: 10.1089/apc.2010.0065. [DOI] [PubMed] [Google Scholar]
- 20.Finocchario-Kessler S. Mabachi N. Dariotis JK, et al. “We weren't using condoms because we were trying to conceive”: The need for reproductive counseling for HIV-positive women in clinical care. AIDS Patient Care STDs. 2012;26:700–707. doi: 10.1089/apc.2012.0232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Blackstock OJ. Beach MC. Korthuis PT, et al. HIV providers' perceptions of and attitudes toward female versus male patients. AIDS Patient Care STDs. 2012;26:582–588. doi: 10.1089/apc.2012.0159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morse J. Handbook of Qualitative Research. Sage Publications; Thousand Oaks: 1994. Designing funded qualitative research; pp. 220–235. [Google Scholar]
- 23.Spradley J. Participant Observation. Holt, Rinehart & Winston; New York City: 1980. [Google Scholar]
- 24.Logie CH. James L. Tharao W, et al. HIV, gender, race, sexual orientation, and sex work: A qualitative study of intersectional stigma experienced by HIV-positive women in Ontario, Canada. PLoS Med. 2011;8:e1001124. doi: 10.1371/journal.pmed.1001124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hsieh HF. Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15:12771288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 26.Maxwell JA. Using numbers in qualitative research. Qual Inq. 2012;16:475. [Google Scholar]
- 27.Messer LC. Quinlivan EB. Parnell H, et al. Barriers and facilitators to testing, treatment entry, and engagement in care by HIV-positive women of color. In press. [DOI] [PMC free article] [PubMed]
- 28.Margaretha Strandmark K. Ill health is powerlessness: A phenomenological study about worthlessness, limitations and suffering. Scand J Caring Sci. 2004;18:135. doi: 10.1111/j.1471-6712.2004.00275.x. [DOI] [PubMed] [Google Scholar]
- 29.Earnshaw VA. Chaudoir SR. From conceptualizing to measuring HIV stigma: A review of HIV stigma mechanism measures. AIDS Behav. 2009;13:1160–1177. doi: 10.1007/s10461-009-9593-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Goffman E. Gornick V. Stigma: Notes on the Management of Spoiled Identity. Prentice- Hall, Inc.; 1963. [Google Scholar]
- 31.Boehme AK. Moneyham L. McLeod J, et al. HIV-infected women's relationships with their health care providers in the rural deep south: An exploratory study. Health Care Women Int. 2012;33:403–419. doi: 10.1080/07399332.2011.610533. [DOI] [PubMed] [Google Scholar]
- 32.Webel AR. Dolansky MA. Henry AG, et al. A qualitative description of women's HIV self-management techniques: Context, strategies, and considerations. J Assoc Nurses AIDS Care. 2012;23:281–293. doi: 10.1016/j.jana.2011.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moneyham L. McLeod J. Boehme A, et al. Perceived barriers to HIV care among HIV-infected women in the Deep South. J Assoc Nurses AIDS Care. 2010;21:467–477. doi: 10.1016/j.jana.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 34.Smith LR. Fisher JD. Cunningham CO, et al. Understanding the behavioral determinants of retention in HIV care: A qualitative evaluation of a situated information, motivation, behavioral skills model of care initiation and maintenance. AIDS Patient Care STDs. 2012;26:344–355. doi: 10.1089/apc.2011.0388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Falcon R. Bridge DA. Currier J, et al. Recruitment and retention of diverse populations in antiretroviral clinical trials: Practical applications from the gender, race and clinical experience study. J Womens Health (Larchmt) 2011;20:1043–1050. doi: 10.1089/jwh.2010.2504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lynam I. Catley D. Goggin K, et al. Autonomous regulation and locus of control as predictors of antiretroviral medication adherence. J Health Psychol. 2009;14:578–586. doi: 10.1177/1359105309103577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Houston E. McKirnan DJ. Cervone D, et al. Assessing treatment motivation among patients receiving antiretroviral therapy: A multidimensional approach. Psychol Health. 2012;27:674–687. doi: 10.1080/08870446.2011.618536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Office of National AIDS Policy. National HIV/AIDS Strategy for the United States of America. Office of the White House. 2010 [Google Scholar]