Abstract
In meta-analysis, between-study heterogeneity indicates the presence of effect-modifiers and has implications for the interpretation of results in cost-effectiveness analysis and decision making. A distinction is usually made between true variability in treatment effects due to variation in patient populations or settings and biases related to the way in which trials were conducted. Variability in relative treatment effects threatens the external validity of trial evidence and limits the ability to generalize from the results; imperfections in trial conduct represent threats to internal validity. We provide guidance on methods for meta-regression and bias-adjustment, in pairwise and network meta-analysis (including indirect comparisons), using illustrative examples. We argue that the predictive distribution of a treatment effect in a “new” trial may, in many cases, be more relevant to decision making than the distribution of the mean effect. Investigators should consider the relative contribution of true variability and random variation due to biases when considering their response to heterogeneity. In network meta-analyses, various types of meta-regression models are possible when trial-level effect-modifying covariates are present or suspected. We argue that a model with a single interaction term is the one most likely to be useful in a decision-making context. Illustrative examples of Bayesian meta-regression against a continuous covariate and meta-regression against “baseline” risk are provided. Annotated WinBUGS code is set out in an appendix.
Keywords: cost-effectiveness analysis, Bayesian meta-analysis, comparative effectiveness, systematic reviews
When combining results of different studies in a meta-analysis, heterogeneity (i.e., between-trials variation in relative treatment effects) has implications for the interpretation of results and decision making. We provide guidance on techniques that can be used to explore the reasons for heterogeneity, as recommended in the National Institute for Health and Clinical Excellence (NICE) Guide to Methods of Technology Appraisal.1 We focus particularly on the implications of different forms of heterogeneity, the technical specification of models that can estimate or adjust for potential causes of heterogeneity, and the interpretation of such models in a decision-making context. There is a considerable literature on the origins and measurements of heterogeneity,2 and this is beyond the scope of this article.
Heterogeneity in treatment effects is an indication of the presence of effect-modifying mechanisms—in other words, of interactions—between the treatment effect and the trial or trial-level variable. A distinction is usually made between 2 kinds of interaction effects: clinical variation in treatment effects, resulting from variation between treatment effects due to different patient populations, settings, or protocols across trials and deficiencies in the way the trial was conducted. The first type of interaction is said to represent a threat to the external validity of trials, limiting the extent to which one can generalize trial results from one situation to another. The second threatens the internal validity of trials: the trial delivers a biased estimate of the treatment effect in its target population, which may or may not be the same as the target population for decision. Typically, these biases are considered to vary randomly over trials and do not necessarily have a zero mean. For example, the biases associated with markers of poor trial quality, such as lack of allocation concealment or lack of double blinding, have been shown to be associated with larger treatment effects.3,4 A general model for heterogeneity that encompasses both types of interaction has been proposed,5 but it is seldom possible to determine what the causes of heterogeneity are and how much is due to true variation in clinical factors and how much is due to other unknown causes of biases.
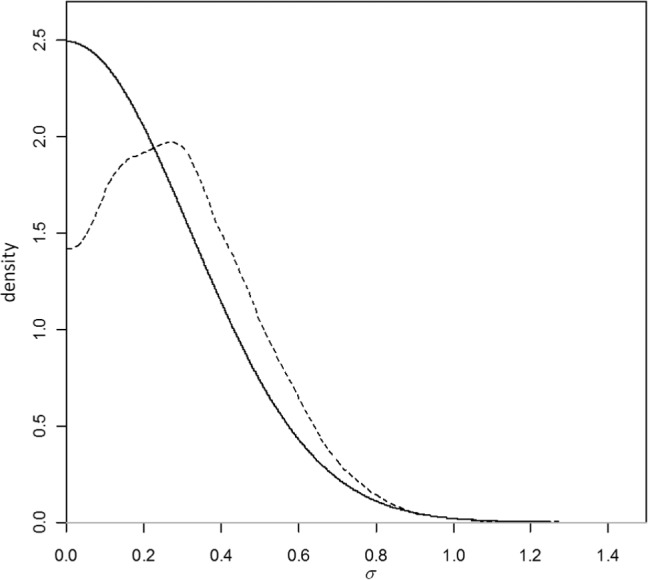
In a decision-making context, the response to high levels of heterogeneity is a critical issue. Investigators should compare the size of the treatment effect with the extent of between-trials variation. If the latter approximates the former, interpretation of mean treatment effects is difficult.6,7 Figure 1 portrays a situation in which a random effects (RE) model has been fitted. The posterior mean of the mean treatment effect is 0.70 with a posterior standard deviation (SD) of 0.2, making the mean effect clearly different from zero with a 95% credible interval (CrI) of (0.31, 1.09). However, the posterior mean of the between-trials standard deviation is σ = 0.68, comparable in size to the mean effect. What is a reasonable confidence interval for our prediction of the outcome of a future trial of infinite size? An approximate answer in classical statistics is found by adding the variance of the mean to the between-trials variance, which gives SD2+σ2 = 0.50, giving a predictive standard deviation of 0.71. Note that the 95% predictive interval is now (−0.69, 2.09), easily spanning zero effect, including a range of harmful effects. If we interpret these distributions in a Bayesian way, we would find that the probability that the mean effect is less than zero is only 0.0002, whereas the probability that a new trial would show a negative effect is much higher: 0.162 (Figure 1).
Figure 1.
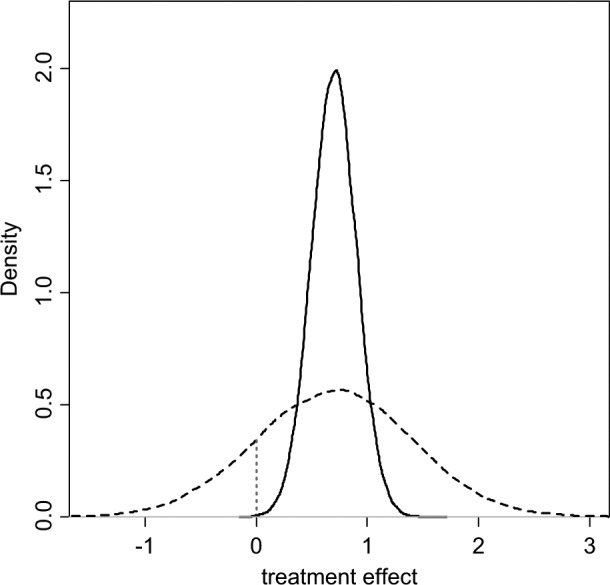
Posterior (solid) and predictive (dashed) densities for a treatment effect with mean = 0.7, standard deviation = 0.2, and heterogeneity (standard deviation) = 0.68. The area under the curve to the left of the vertical dotted line is the probability of a negative value for the treatment effect.
This issue has been discussed before,5–8 and it has been proposed that, in the presence of heterogeneity, the predictive distribution, rather than the distribution of the mean treatment effect, better represents our uncertainty about the comparative effectiveness of treatments in a future “rollout” of a particular intervention. In a Bayesian Markov chain Monte Carlo (MCMC) setting, a predictive distribution is easily obtained by drawing further samples from the distribution of effects:
where d is the estimated (common) mean treatment effect and σ2 the estimated between-trial heterogeneity variance.
Where there are high levels of unexplained heterogeneity, the implications of this recommendation for the uncertainty in a decision can be quite profound, and it is therefore important that the degree of heterogeneity is not exaggerated and that the causes of the heterogeneity are investigated.9,10 The variance term in the predictive distribution should consist only of true variation between trial populations,5 but at present, there is no clear methodology to distinguish between different sources of variation in treatment effect. Recent meta-epidemiological work on the determinants of between-study variation is beginning to shed some light on this.11
Meta-regression is used to relate the size of a treatment effect obtained from a meta-analysis to potential effect modifiers—covariates—that may be characteristics of the trial participants or connected with the trial setting or conduct. These covariates may be categorical or continuous. In common with other forms of meta-analysis, meta-regression can be based on aggregate (trial-level) outcomes and covariates, or individual patient data (IPD) and covariates when available. However, even if we restrict attention to randomized controlled trial (RCT) data, the study of effect-modifiers is inherently observational2,12 as it is not possible to randomize patients to one covariate value or another. As a consequence, meta-regression inherits all the difficulties of interpretation and inference that attach to nonrandomized studies: confounding, correlation between covariates, and, most important, the inability to infer causality from association.
We provide guidance on methods for meta-regression and bias-adjustment that can address the presence of heterogeneity using aggregate data and trial-level covariates and discuss the limitations of this approach and the potential advantages of meta-regression with IPD.
Subgroup Effects (Appendix: Example 1)
We start with the simplest form of meta-regression: adjusting for subgroup effects in a pairwise meta-analysis. The theory set out in this section is then generalized to other types of meta-regression and to multiple treatments. The methods outlined here can be seen as extensions to the common generalized linear modeling framework for pairwise and network meta-analysis.13
In the context of treatment effects in RCTs, a subgroup effect can be understood as a categorical trial-level covariate that interacts with the treatment. The hypothesis would be that the size of the treatment effect is different, for example, in male and female patients or that it depends on age group or previous treatment. Separate analyses can be carried out for each group and the relative treatment effects compared. However, if the models have random treatment effects, having separate analyses means having different estimates of between-trial variation. As there are seldom enough data to estimate the between-trial variation, it may make more sense to assume that it is the same for all subgroups. Furthermore, running separate analyses does not immediately produce the test of interaction that is required to reject the null hypothesis of equal effects. It is therefore preferable to have a single integrated analysis with a single between-trial variation term and an interaction term, β, introduced on the treatment effect, as follows:
| (1) |
where xi is the trial-level covariate for trial i, which can represent a subgroup, a continuous covariate, or baseline risk; θik is the linear predictor13 (e.g., the log-odds or mean) in arm k of trial i;µi are the trial-specific baseline effects in a trial i, treated as unrelated nuisance parameters; δi,1k are the trial-specific treatment effects of the treatment in arm k relative to the treatment in arm 1 in that trial, with k = 1, 2 and
| (2) |
We can rewrite equation (1) as
and note that the treatment and covariate interaction effects (δ and β) act only in the experimental arm, not in the control. For an RE model, the trial-specific log-odds ratios come from a common distribution: . For a fixed effect (FE) model, we replace equation (1) with . In the Bayesian framework d 12, β and σ will be given independent (noninformative) priors: for example, d 12, β ~ N(0, 1002) and σ ~ Uniform(0, 5).
Meta-Regression Models in Network Meta-Analysis
In a network meta-analysis (NMA) context, variability in relative treatment effects can also induce inconsistency14 across pairwise comparisons. The methods introduced here are therefore also appropriate for dealing with inconsistency. Unless otherwise stated, when we refer to heterogeneity in this context, this can be interpreted as heterogeneity and/or inconsistency.
A large number of meta-regression models can be proposed for NMA, each with very different implications. There are 3 main approaches: unrelated interaction terms for each treatment, exchangeable and related interaction terms, and one single interaction effect for all treatments. We argue that the third model is the most likely to have a useful interpretation in a decision-making context.
Consider a binary between-trial covariate (e.g., primary v. secondary prevention trials) in a case where s treatments are being compared.15,16 We take treatment 1 (e.g., a placebo or standard treatment) as the reference treatment in the NMA. Following the approach to consistency models adopted previously,13 we have (s– 1) basic parameters for the relative treatment effects d 12, d 13, . . ., d 1s of each treatment relative to treatment 1. The remaining (s– 1)(s– 2)/2 treatment contrasts are expressed in terms of these parameters using the consistency equations: for example, the effect of treatment 4 compared with treatment 3 is written as d 34 = d 14–d 13.13 We set out a range of fixed treatment effect interaction models, which are later extended to random treatment effects.
1. Unrelated Treatment-Specific Interactions
If there is an interaction effect between, say, primary/secondary prevention and treatment, but these interactions are different for every treatment, the model will have as many interaction terms as there are basic treatment effects (e.g., β12, β13, . . ., β1s), each representing the additional (interaction) treatment effect in secondary prevention (compared with primary) in comparisons of treatments 2, 3, . . ., s to treatment 1. These terms are exactly parallel to the main effects d 12, d 13, . . ., d 1s, which now represent the treatment effects in primary prevention populations. As with the main effects, for trials comparing, say, treatments 3 and 4, the interaction term is the difference between the interaction terms on the effects relative to treatment 1, so that β34 = β14–β13. The fixed treatment effects model for the linear predictor is
| (3) |
with tik representing the treatment in arm k of trial i, xi the covariate/subgroup indicator, and I defined in equation (2). In all models, we set d 11 = β11 = 0. The remaining interaction terms are given unrelated vague prior distributions in a Bayesian analysis.
The relative treatment effects in secondary prevention are d 12+β12, d 13+β13, . . ., d 1s+β1s. The interpretation is that the relative efficacy of each of the s treatments in primary prevention populations is entirely unrelated to their relative efficacy in secondary prevention populations.
2. Exchangeable and Related Treatment-Specific Interactions
This model has the same structure as the model above, but now the (s– 1) “basic” interaction terms are drawn from a random distribution with a common mean and between-treatment variance: , for treatment k = 2, . . ., s. The mean interaction effect and its variance are estimated from the data, although informative priors that limit how similar or different the interaction terms are can be used. The interpretation is that there are real differences between the relative treatment effects, although these are centered on a common mean, with a common variance.
3. Same Interaction Effect for All Treatments
In this case, there is a single interaction term b that applies to the relative effects of all the treatments relative to treatment 1, so that for k = 2, . . ., s. The treatment effects relative to treatment 1, d12, d 13…d 1s in primary prevention, are all higher or lower by the same amount, b in secondary prevention: d 12+b, d 13+b . . . d 1s+b. However, the effects of treatments 2, 3, . . ., s relative to each other in primary and secondary prevention populations are the same because the interaction terms cancel out. For example, consider the effect of treatment 4 relative to treatment 3 in secondary prevention: , which is the same as in primary prevention. This means that the choice of reference treatment becomes important, and results for models with covariates are sensitive to this choice.
Note that although we have presented the models in the context of subgroup effects, models for meta-regression with continuous covariates, including baseline risk, have the same structure.
If an unrelated interactions model is being considered (model 1), this requires 2 connected networks (one for each subgroup), including all the treatments, that is, with at least (s– 1) trials in each. With related interaction effects (model 2), it may not be necessary to have 2 complete networks, but a substantial number of trials are needed to identify both random treatment effects and random interactions. However, to use such a model, there needs to be a clear rationale for exchangeability of interactions with a common mean and variance. One rationale could be to allow for different covariate effects for different treatments within the same class. Thus, treatment 1 is a standard or placebo treatment, whereas some of the treatments 2, . . ., s belong to a “class.” For example, one might imagine one set of exchangeable interaction terms for aspirin-based treatments for atrial fibrillation relative to placebo and a second set of interactions for warfarin-based treatments relative to placebo.17
Although exchangeable and related interactions seem an attractive model in theory, they could lead to situations where the relative efficacy or the relative cost-effectiveness of a set of active treatments in the same class, and hence optimal treatment decisions, will depend on covariate values. However, differences between interaction terms are unlikely to be robust, and treatment decisions could then be driven by statistically insignificant interaction terms. Therefore, although these more complex models can be fitted,17,18 their best role may be in exploratory analyses. Here we explore only model 3, which assumes an identical interaction effect across all treatments with respect to the reference treatment.
Network Meta-Regression with a Continuous Covariate
When dealing with a continuous covariate, we will use centered covariate values.19 This is achieved by subtracting the mean covariate value, , from each xi. To fit a random treatment effects model that assumes a common interaction effect for all treatments with covariate centering, we rewrite equation (3) as
| (4) |
where β11 = 0, β1k = b (k = 2, . . . ,7) and .
We retain the treatment-specific interaction effects but set them all equal to b, so that the terms cancel out in comparisons not involving the reference treatment. To produce treatment effect estimates at covariate value z, the outputs from this model should be “uncentered”: , k = 2, . . ., s.
Example: Certolizumab Meta-Regression on Mean Disease Duration (Appendix: Example 2)
Data are available from a review of trials of certolizumab pegol (CZP) for the treatment of rheumatoid arthritis in patients who had failed on disease-modifying antirheumatic drugs, including methotrexate (MTX).20 Twelve MTX controlled trials were identified, comparing 6 different treatments with placebo (Figure 2).
Figure 2.
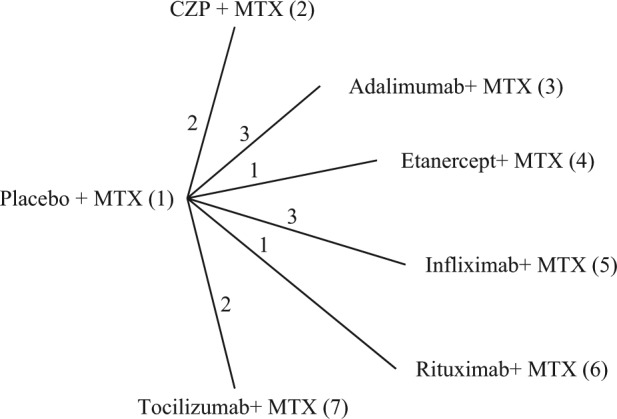
Certolizumab example20: treatment network. Lines connecting 2 treatments indicate that a comparison between these treatments has been made. The numbers on the lines indicate how many randomized controlled trials compare the 2 connected treatments. CZP, certolizumab pegol; MTX, methotrexate.
Table 1 shows the number of patients who have improved by at least 50% on the American College of Rheumatology scale (ACR50) at 6 months, rik, out of all included patients, nik, for each arm of the included trials, along with the mean disease duration in years for patients in each trial, xi (i = 1, . . ., 12; k = 1, 2). The crude odds ratios (ORs) from Table 1 are plotted (on a log-scale) against mean disease duration in Figure 3, with the numbers 2 to 7 representing the OR of that treatment relative to placebo plus MTX (chosen as the reference treatment). Example 1 in the Appendix gives details of priors and the WinBUGS21 code for the model in equation (4).
Table 1.
Certolizumab Example20: Number of Patients Achieving ACR50 at 6 Months,a r, Out of the Total Number of Patients, n, in Arms 1 and 2 of the 12 Trials and Mean Disease Duration (in Years) for Patients in Trial i, xi
| Arm 1 |
Arm 2 |
||||||
|---|---|---|---|---|---|---|---|
| Study Name | Treatment in Arm 1, ti 1 | Treatment in Arm 2, ti 2 | No. Achieving ACR50, ri 1 | Total No. of Patients, ni 1 | No. Achieving ACR50, ri 2 | Total No. of Patients, ni 2 | Mean Disease Duration (Years), xi |
| RAPID 1 | Placebo | CZP | 15 | 199 | 146 | 393 | 6.15 |
| RAPID 2 | Placebo | CZP | 4 | 127 | 80 | 246 | 5.85 |
| Kim 2007 | Placebo | Adalimumab | 9 | 63 | 28 | 65 | 6.85 |
| DE019 | Placebo | Adalimumab | 19 | 200 | 81 | 207 | 10.95 |
| ARMADA | Placebo | Adalimumab | 5 | 62 | 37 | 67 | 11.65 |
| Weinblatt 1999 | Placebo | Etanercept | 1 | 30 | 23 | 59 | 13 |
| START | Placebo | Infliximab | 33 | 363 | 110 | 360 | 8.1 |
| ATTEST | Placebo | Infliximab | 22 | 110 | 61 | 165 | 7.85 |
| Abe 2006b | Placebo | Infliximab | 0 | 47 | 15 | 49 | 8.3 |
| Strand 2006 | Placebo | Rituximab | 5 | 40 | 5 | 40 | 11.25 |
| CHARISMAb | Placebo | Tocilizumab | 14 | 49 | 26 | 50 | 0.915 |
| OPTION | Placebo | Tocilizumab | 22 | 204 | 90 | 205 | 7.65 |
All trial arms had methotrexate in addition to the placebo or active treatment. CZP, certolizumab pegol.
Three months was used when this was not available.
ACR50 at 3 months.
Figure 3.
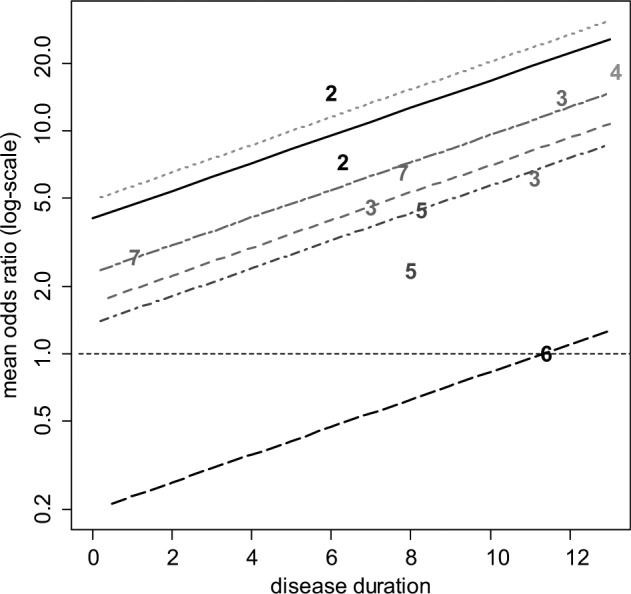
Certolizumab example20: plot of the crude odds ratio (OR) (on a log-scale) of the 6 active treatments relative to placebo plus methotrexate (MTX) against mean disease duration (in years). For plotting purposes, the odds of response on placebo plus MTX for the Abe 2006 study were assumed to be 0.01. The plotted numbers refer to the treatment being compared with placebo plus MTX, and the lines represent the relative effects of the following treatments compared with placebo plus MTX based on a random effects meta-regression model (from top to bottom): etanercept plus MTX (treatment 4, dotted green line), certolizumab pegol (CZP) plus MTX (treatment 2, solid black line), tocilizumab plus MTX (treatment 7, short-long dash purple line), adalimumab plus MTX (treatment 3, dashed red line), infliximab plus MTX (treatment 5, dot-dashed dark blue line), and rituximab plus MTX (treatment 6, long-dashed black line). Odds ratios above 1 favor the plotted treatment, and the horizontal line (thin dashed) represents no treatment effect.
Table 2 shows the results of fitting fixed and random treatment effects NMA13 and interaction models with disease duration as the covariate. The estimated ORs for different durations of disease are represented by the parallel lines in Figure 3. Note that the treatment effects obtained are the estimated log-odds ratios at the mean covariate value ( years in this case) and that credible interval lines have not been included in Figure 3.
Table 2.
Certolizumab Example20: Posterior Mean, SD, and 95% CrI for the Interaction Estimate (b) and Log-Odds Ratios dXY of Treatment Y relative to Treatment X
| No Covariate |
Covariate “Disease Duration” |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| FE |
REa
|
FE | REa
|
|||||||||
| Mean | SD | CrI | Mean/ Median | SD | CrI | Mean | SD | CrI | Mean/ Median | SD | CrI | |
| b | NA | NA | NA | NA | NA | NA | 0.14 | 0.06 | (0.01, 0.26) | 0.14 | 0.09 | (−0.03, 0.32) |
| d 12 | 2.21 | 0.25 | (1.73, 2.72) | 2.27 | 0.39 | (1.53, 3.10) | 2.50 | 0.29 | (1.96, 3.08) | 2.57 | 0.42 | (1.79, 3.44) |
| d 13 | 1.93 | 0.22 | (1.52, 2.37) | 1.97 | 0.33 | (1.33, 2.64) | 1.66 | 0.25 | (1.19, 2.16) | 1.71 | 0.34 | (1.04, 2.41) |
| d 14 | 3.47 | 1.34 | (1.45, 6.74) | 3.46 | 1.41 | (1.26, 6.63) | 2.82 | 1.34 | (0.71, 5.96) | 2.77 | 1.42 | (0.42, 6.01) |
| d 15 | 1.38 | 0.17 | (1.06, 1.72) | 1.48 | 0.33 | (0.90, 2.21) | 1.40 | 0.17 | (1.08, 1.74) | 1.48 | 0.30 | (0.95, 2.15) |
| d 16 | 0.00 | 0.71 | (−1.40, 1.39) | 0.01 | 0.82 | (−1.61, 1.63) | −0.42 | 0.73 | (−1.86, 1.04) | −0.44 | 0.84 | (−2.08, 1.21) |
| d 17 | 1.65 | 0.22 | (1.22, 2.10) | 1.56 | 0.38 | (0.77, 2.28) | 1.98 | 0.28 | (1.45, 2.53) | 2.00 | 0.45 | (1.12, 2.93) |
| σ | NA | NA | NA | 0.34 | 0.20 | (0.03, 0.77) | NA | NA | NA | 0.28 | 0.19 | (0.02, 0.73) |
| b | 37.6 | 30.9 | 33.8 | 30.2 | ||||||||
| pD | 18.0 | 21.2 | 19.0 | 21.3 | ||||||||
| DIC | 55.6 | 52.1 | 52.8 | 51.4 | ||||||||
Posterior median, standard deviation (SD), and 95% credible interval (CrI) of the between-trial heterogeneity (σ) for the number of patients achieving ACR50 for the fixed effects (FE) and random effects (RE) models with and without covariate “disease duration” and measures of model fit: posterior mean of the residual deviance (), effective number of parameters (pD), and deviance information criterion (DIC). Results are based on 100,000 iterations from 3 independent chains after a burn-in of 40,000 iterations. Treatment codes are given in Figure 2. NA, not applicable.
Using informative prior for σ (for details, see Appendix).
Compare with 24 data points.
The deviance information criterion (DIC) provides a measure of model fit that penalizes model complexity22—lower values of the DIC suggest a more parsimonious model. We calculate the DIC as the sum of the posterior mean of the residual deviance, , and the leverage, pD.13 The DIC and posterior means of the residual deviances in Table 2 do not decisively favor a single model (differences less than 3 or 5 are not considered meaningful). The fit of the FE model is improved by including the covariate interaction term b, which also has a CrI that does not include zero. Addition of the covariate to the RE model reduces the heterogeneity from a posterior median of 0.34 to 0.28, but the CrI for the interaction parameter b includes zero. In this example, the meta-regression models are all reasonable but not strongly supported by the evidence, although the finding of smaller treatment effects with a shorter disease duration has been reported previously.18
Should the use of biologics be confined to patients whose disease duration was above a certain threshold? This seems reasonable, but it would be difficult to determine this threshold on the basis of this evidence alone. The slope is largely determined by treatments 3 and 7 (adalimumab and tocilizumab), which are the only treatments trialed at more than 1 disease duration and appear to have different effects at each duration (Figure 3). However, the linearity of relationships is highly questionable, and the prediction of negative effects for treatment 6 (rituximab) is not plausible. This suggests that other explorations of the causes of heterogeneity in this network should be undertaken (see below).
Network Meta-Regression on Baseline Risk
The meta-regression model presented above can be extended to use the baseline risk in each trial as a covariate, taking into account the error in the estimation of baseline risk and its correlation to the OR. The model is the same as in equation (4) but now xi = µi, the trial-specific baseline for the control arm in each trial. An important property of this Bayesian formulation is that it takes the “true” baseline (as estimated by the model) as the covariate and automatically takes the uncertainty in each µi into account.23,24 Naive approaches, which regress against the observed baseline risk, fail to take the correlation between the treatment effect and baseline risk, as well as the consequent regression to the mean phenomenon, into account.
Example: Certolizumab Meta-Regression on Baseline Risk (Appendix: Example 3)
Both FE and RE models with a common interaction term were fitted. Due to covariate centering, the treatment effects in Table 3 for the models with covariate adjustment are the effects for patients with a baseline log-odds ACR50 of −2.421, the mean of the observed log-odds on treatment 1. This corresponds to a baseline ACR50 probability of 0.082.
Table 3.
Certolizumab Example20: Posterior Mean, SD, and 95% CrI for the Interaction Estimate (b) and Log-Odds Ratios dXY of Treatment Y Relative to Treatment X
| FE |
RE |
|||||
|---|---|---|---|---|---|---|
| Mean | SD | CrI | Mean/Median | SD | CrI | |
| b | −0.93 | 0.09 | (−1.03, −0.69) | −0.95 | 0.10 | (−1.10, −0.70) |
| d 12 | 1.85 | 0.10 | (1.67, 2.06) | 1.83 | 0.24 | (1.35, 2.29) |
| d 13 | 2.13 | 0.11 | (1.90, 2.35) | 2.18 | 0.22 | (1.79, 2.63) |
| d 14 | 2.08 | 0.34 | (1.47, 2.80) | 2.04 | 0.46 | (1.19, 2.94) |
| d 15 | 1.68 | 0.10 | (1.49, 1.86) | 1.71 | 0.22 | (1.30, 2.16) |
| d 16 | 0.36 | 0.50 | (−0.72, 1.27) | 0.37 | 0.59 | (−0.86, 1.45) |
| d 17 | 2.20 | 0.14 | (1.93, 2.46) | 2.25 | 0.27 | (1.75, 2.79) |
| σ | NA | NA | NA | 0.19 | 0.19 | (0.01, 0.70) |
| a | 27.3 | 24.2 | ||||
| pD | 19.0 | 19.4 | ||||
| DIC | 46.3 | 43.6 | ||||
Posterior median, standard deviation (SD), and 95% credible interval (CrI) of the between-trial heterogeneity (σ) for the number of patients achieving ACR50 for the fixed effects (FE) and random effects (RE) models with covariate “baseline risk” and measures of model fit: posterior mean of the residual deviance (), number of parameters (pD), and deviance information criterion (DIC). Results are based on 100,000 iterations from 3 independent chains after a burn-in of 60,000 iterations. Treatment codes are given in Figure 2. NA, not applicable.
Compare with 24 data points.
In both models, the 95% CrIs for covariate term exclude zero, suggesting a strong interaction effect between the baseline risk and the treatment effects. The estimated RE model is shown in Figure 4: the differences between the lines represent treatment differences controlling for baseline risk. However, note that there is considerable uncertainty around these lines, which is not represented in Figure 4. The DIC statistics and the posterior means of the residual deviance also marginally favor the RE model with the covariate. In interpreting the results of this model, it should be noted that treatment effect is being defined on a percent change scale: the extent of change is therefore automatically increased as the baseline is lowered. Hence, the observed interaction may to some extent be an artifact of the measurement scale.
Figure 4.
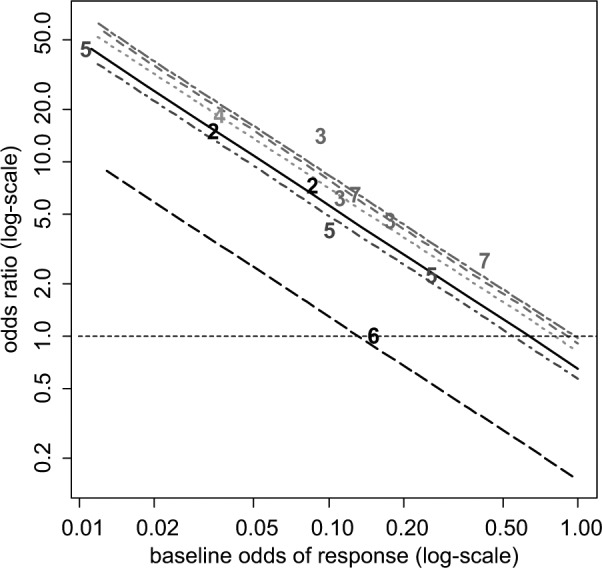
Certolizumab example20: plot of the crude odds ratio (OR) of the 6 active treatments relative to placebo plus methotrexate (MTX) against odds of baseline response on a log-scale. For plotting purposes, the odds of response on placebo plus MTX for the Abe 2006 study were assumed to be 0.01. The plotted numbers refer to the treatment being compared with placebo plus MTX, and the lines represent the relative effects of the following treatments (from top to bottom) compared with placebo plus MTX based on a random effects meta-regression model: tocilizumab plus MTX (treatment 7, short-long dash purple line), adalimumab plus MTX (treatment 3, dashed red line), etanercept plus MTX (treatment 4, dotted green), certolizumab pegol (CZP) plus MTX (treatment 2, solid black line), infliximab plus MTX (treatment 5, dot-dashed dark blue line), and rituximab plus MTX (treatment 6, long-dashed black line). Odds ratios above 1 favor the plotted treatment, and the horizontal line (dashed) represents no treatment effect.
Bias and Bias-Adjustment
If it is thought that heterogeneity is due to bias in some of the included studies, models for bias-adjustment can be used. The difference between “bias-adjustment” and the meta-regression models described above is slight but important. In meta-regression, we concede that even within the formal scope of the decision problem, there are distinct differences in relative treatment efficacy. In bias-adjustment, we have in mind a target population for decision making, but the evidence available, or at least some of the evidence, provides biased, or potentially biased, estimates of the target parameter, perhaps because the trials have internal biases, they concern different populations or settings, or both.
Adjustment for Bias Based on Meta-Epidemiological Data
Confronted by trial evidence of mixed quality, investigators have 3 options: 1) to restrict attention to studies of high quality, ignoring what may be a substantial proportion of the evidence; 2) to include trials of both high and low quality in a single analysis, which risks delivering a biased estimate of the treatment effect; or 3) to use all the data but simultaneously adjust and down-weight the evidence from studies at risk of bias.25 The latter uses information on the expected bias, as well as between-study variation in bias, derived from statistical analysis of meta-epidemiological data. The analysis assumes that the study-specific biases in the data set of interest are exchangeable with those in the meta-epidemiological data used to provide the prior distributions used for adjustment. This approach can form the basis for sensitivity analyses to show whether the presence of studies at risk of bias, with potentially over-optimistic results, has an impact on the decision.25
It is expected that this bias-adjustment method will be used more when more data are available on how the degree of bias depends on the nature of the outcome measure and the clinical condition.4 In principle, the same form of bias-adjustment could be extended to other types of bias or to mixtures of RCTs and observational studies. Each of these extensions, however, depends on the applicability of analyses of very large meta-epidemiological data sets that are starting to become available.11,26
Estimation and Adjustment for Bias in Network Meta-Analysis
In NMA, if we assume that the mean and variance of the study-specific biases are the same for each treatment, it is possible to simultaneously estimate the treatment effects and the bias effects in a single analysis and to produce treatment effects that are based on the entire body of data and also adjusted for bias.27 If A is placebo or standard treatment and B, C, and D are all active treatments, it would be reasonable to expect the same bias distribution to apply to the AB, AC, and AD trials. But it is less clear what the direction of the bias should be in BC, BD, and CD trials. Assuming that the average bias is always in favor of the newer treatment, this becomes a model for novelty bias.28,29 Another approach might be to propose a separate mean bias term for active v. active comparisons.27
This method can in principle be extended to include syntheses that are mixtures of trials and observational studies, and it can also be extended to any form of “internal” bias. A particularly interesting application is to “small-study bias,” which is one interpretation of “publication bias.” The idea is that smaller studies have greater bias. The “true” treatment effect can therefore be conceived as the effect that would be obtained in a study of infinite size, which is taken to be the intercept in a regression of the treatment effect against the study variance.30,31
Elicitation of Bias Distributions
This method32 is conceptually the simplest of all bias-adjustment methods, applicable to trials and observational studies alike, but it is also the most difficult and time-consuming. One of its advantages is that it can be used when the number of trials is insufficient for meta-regression approaches. Each study is considered by several independent experts using a predetermined protocol that itemizes a series of potential internal and external biases. Each expert is asked to provide information that is used to develop a combined bias distribution. The mean and variance of the bias distributions are statistically combined with the original study estimate and its variance to create a new, adjusted estimate of the treatment effect in each study. The final stage is a conventional synthesis of the adjusted study-specific estimates using standard pairwise or network meta-analysis methods.
Discussion
We have detailed methods to explore or explain heterogeneity in pairwise and network meta-analyses using study-level covariates, including baseline risk (variation in “baseline” natural history is dealt with in another tutorial in this series33), although we have not covered the closely related topic of outlier detection.16,34,35
However, meta-regression based on aggregate data and study-level covariates suffers from several bias and confounding problems as well as typically having low power. When a categorical covariate is considered, one can contrast a within-trial comparison (e.g., treatment effects reported separately for males and females) and a between-trial comparison where different trials are run on male and female patients. The contrast is similar to the difference between a paired and an unpaired t test. With between-trial comparisons, a given covariate effect (i.e., interaction) will be harder to detect as it has to be distinguishable from the “random noise” created by the between-trial variation. However, for within-trial comparisons, the between-trial variation is controlled for, and the interaction effect needs only to be distinguishable from sampling error. A further drawback of between-trial comparisons is that, because the number of observations (trials) may be very low while the precision of each trial may be relatively high, it is quite possible to observe a highly statistically significant relation between the treatment effect and the covariate that is entirely spurious.36 Furthermore, between-trial comparisons are more vulnerable to ecologic bias or ecologic fallacy,37 where, for example, a linear regression coefficient of treatment effect against the covariate in the between-trial case can be entirely different from the coefficient for the within-trial data.
With continuous covariates and IPD, not only does the within-trial comparison avoid ecological bias, but it also has far greater statistical power to detect a true covariate effect. This is because the variation in patient covariate values will be many times greater than the variation between the trial means,38,39 and the precision in any estimated regression coefficient depends directly on the variance in covariate values. For these reasons, IPD meta-analyses and meta-regression are taken to be the “gold standard,”40 although IPD is not available in most situations.
Two broad approaches to IPD meta-regression have been considered.41 In the 2-step approach, the analyst first estimates the interaction effect sizes and their standard errors from each study and then conducts a standard meta-analysis on these summaries. This is appropriate for inference on the existence of an interaction, but for decision making, we recommend a 1-step method in which main effects and interaction are estimated simultaneously. This is because the parameter estimates of the main effects and interaction terms will be correlated, and their joint uncertainty can most easily be propagated through the decision model by estimating them simultaneously. IPD RE pairwise meta-analysis models have been developed for continuous,42,43 binary,44 survival,45 and ordinal46 variables. Although most of the models are presented in the single pairwise comparison context, it is possible to extend them to an NMA context.42,47–51 Criteria for determining the potential benefits of IPD to assess patient-level covariates have recently been outlined.52
When IPD is available only in a subset of studies, it is possible to incorporate both types of data in the same analysis using dual effect models.48,50,53–55 This makes the best possible use of all available data, but a decision has to be made on whether between-study variability is to be included in the estimation of effects. Statistical tests are unlikely to have sufficient power to inform a decision. In an NMA with IPD, we would recommend use of models with a single interaction term for each covariate, at least within a class of treatments, for decision making, but more complex structures have been attempted.49
Finally, it needs to be appreciated that in cases where the covariate does not interact with the treatment effect but modifies the baseline risk, the effect of pooling data over the covariate is to bias the estimated treatment effect toward the null effect. This is a form of ecologic bias known as aggregation bias,37 which does not affect strictly linear models, where pooling data across such covariates will not create bias. Usually, it is significant only when both the covariate effect on baseline risk and the treatment effect are quite strong. It is a particular danger in survival analysis because the effect of covariates such as age on cancer risk can be particularly marked and because the log-linear models routinely used are highly nonlinear. When covariates that affect risk are present, even if they do not modify the treatment effect, the analysis must be based on pooled estimates of treatment effects from a stratified analysis for group covariates and regression for continuous covariates and not on treatment effects estimated from pooled data.
Bias-adjustment methods are another form of accounting for differences between studies. These methods should be considered semi-experimental as there is a need for further experience with applications and for further meta-epidemiological data on the relationships between the many forms of internal bias that have been proposed.29 However, they represent reasonable and valid methods for bias-adjustment and are likely to be superior to no bias-adjustment in situations where data are of mixed quality. At the same time, caution is required as the method is essentially a meta-regression based on “between-studies” comparisons, with no certainty of a causal mechanism.
We have suggested that choice between models with and without the covariate or bias-adjustment coefficients should be based on examining the DIC and the CrI of the regression coefficient. However, in general, the DIC is not able to inform choice between RE models with and without covariates as both will tend to fit equally well and have a similar effective number of parameters. Other considerations, such as a reduction in the heterogeneity, will play a greater role in choosing between RE models. For FE models with and without covariates, the DIC is suitable for model choice.
Acknowledgments
We thank Jenny Dunn at NICE DSU and Julian Higgins, Jeremy Oakley, and Catrin Tudor-Smith for reviewing previous versions of this article.
Appendix
Heterogeneity and Meta-Regression—Illustrative Examples and WinBUGS Code
This appendix gives illustrative WinBUGS code for all the examples presented in the main article. All programming code is fully annotated. The program codes are printed here but are also available as WinBUGS system files from http://www.nicedsu.org.uk. Users are advised to download the WinBUGS files from the website instead of copying and pasting from this document. We have provided the codes as complete programs. However, the majority of each meta-regression program is identical to the programs in Dias and others.13,56 We have therefore highlighted the main differences in blue and bold, to emphasize the modular nature of the code. The code presented is completely general and will be suitable for fitting pairwise or network meta-analyses with any number of treatments and multiarm trials. We also provide an indication of the relevant parameters to monitor for inference and model checking for the various programs. The nodes to monitor for the FE models are the same as those for the RE models, except that there is no heterogeneity parameter.
Table A1 gives an index of the programs and their relation to the examples in the main text. Note that for each example, there are RE and FE versions of the code. All FE code can be run using the same data structure described for RE.
Table A1.
Index of WinBUGS Code with Details of Examples and Sections Where They Are Described.
| Program | Fixed or Random Effects | Example Name | Model Specification | |
|---|---|---|---|---|
| 1 | (a) | RE | Statins (subgroups) | Meta-regression with subgroups |
| (b) | FE | |||
| 2 | (a) | RE | Certolizumab (mean disease duration) | Meta-regression with continuous covariate |
| (b) | FE | |||
| 3 | (a) | RE | Certolizumab (baseline risk) | Meta-regression with adjustment for baseline risk |
| (b) | FE | |||
FE, fixed effects; RE, random effects.
Example 1. Statins: Meta-Regression with Subgroups
A meta-analysis of 19 trials of statins for cholesterol lowering v. placebo or usual care3 included some trials on which the aim was primary prevention (patients included had no previous heart disease) and others on which the aim was secondary prevention (patients had previous heart disease). Note that the subgroup indicator is a trial-level covariate. The outcome of interest was all-cause mortality, and the data are presented in Table A2. The potential effect-modifier, primary v. secondary prevention, can be considered a subgroup in a pairwise meta-analysis of all the data, or 2 separate meta-analyses can be conducted on the 2 types of study.
Table A2.
Meta-Analysis of Statins v. Placebo for Cholesterol Lowering in Patients with and without Previous Heart Disease3: Number of Deaths Due to All-Cause Mortality in the Control and Statin Arms of 19 Randomized Controlled Trials.
| Placebo/Usual Care |
Statin |
||||
|---|---|---|---|---|---|
| Trial ID | No. of Deaths, ri 1 | No. of Patients, ni 1 | No. of Deaths, ri 2 | No. of Patients, ni 2 | Type of Prevention, xi |
| 1 | 256 | 2223 | 182 | 2221 | Secondary |
| 2 | 4 | 125 | 1 | 129 | Secondary |
| 3 | 0 | 52 | 1 | 94 | Secondary |
| 4 | 2 | 166 | 2 | 165 | Secondary |
| 5 | 77 | 3301 | 80 | 3304 | Primary |
| 6 | 3 | 1663 | 33 | 6582 | Primary |
| 7 | 8 | 459 | 1 | 460 | Secondary |
| 8 | 3 | 155 | 3 | 145 | Secondary |
| 9 | 0 | 42 | 1 | 83 | Secondary |
| 10 | 4 | 223 | 3 | 224 | Primary |
| 11 | 633 | 4520 | 498 | 4512 | Secondary |
| 12 | 1 | 124 | 2 | 123 | Secondary |
| 13 | 11 | 188 | 4 | 193 | Secondary |
| 14 | 5 | 78 | 4 | 79 | Secondary |
| 15 | 6 | 202 | 4 | 206 | Secondary |
| 16 | 3 | 532 | 0 | 530 | Primary |
| 17 | 4 | 178 | 2 | 187 | Secondary |
| 18 | 1 | 201 | 3 | 203 | Secondary |
| 19 | 135 | 3293 | 106 | 3305 | Primary |
The number of deaths in arm k of trial i, rik, is assumed to have a binomial likelihood , i = 1, . . ., 19; k = 1, 2. Defining xi as the trial-level subgroup indicator such that
our interaction model is , where is the linear predictor (see Dias and others13,56). In this setup, represent the log-odds of the outcome in the “control” treatment (i.e., the treatment indexed 1), and are the trial-specific log-odds ratios of success on the treatment group compared with control for primary prevention studies. See the main text for further details of the model.
WinBUGS code to fit 2 separate fixed or random effects models is given in the appendix to Dias and others.13,56 The WinBUGS code for a single analysis with an interaction term for subgroup with RE is given in program 1(a), and the FE code is given in program 1(b). Although this example includes only 2 treatments, the code presented below can also be used for subgroup analysis with multiple treatments and including multiarm trials.
Program 1(a): Binomial Likelihood, Logit Link, Random Effects, Meta-Regression with Subgroups (Statins Example)
# Binomial likelihood, logit link, subgroup
# Random effects model for multi-arm trials
model{ # *** PROGRAM STARTS
for(i in 1:ns){ # LOOP THROUGH STUDIES
w[i,1] <- 0 # adjustment for multi-arm trials is zero for control arm
delta[i,1] <- 0 # treatment effect is zero for control arm
mu[i] ~ dnorm(0,.0001) # vague priors for all trial baselines
for (k in 1:na[i]) { # LOOP THROUGH ARMS
r[i,k] ~ dbin(p[i,k],n[i,k]) # binomial likelihood
# model for linear predictor, covariate effect relative to treat in arm 1
logit(p[i,k]) <- mu[i] + delta[i,k] +(beta[t[i,k]]-beta[t[i,1]]) * x[i]
rhat[i,k] <- p[i,k] * n[i,k] # expected value of the numerators
dev[i,k] <- 2 * (r[i,k] * (log(r[i,k])-log(rhat[i,k])) #Deviance contribution
+ (n[i,k]-r[i,k]) * (log(n[i,k]-r[i,k]) - log(n[i,k]-rhat[i,k])))
}
resdev[i] <- sum(dev[i,1:na[i]]) # summed residual deviance contribution for this trial
for (k in 2:na[i]) { # LOOP THROUGH ARMS
delta[i,k] ~ dnorm(md[i,k],taud[i,k]) # trial-specific LOR distributions
md[i,k] <- d[t[i,k]] - d[t[i,1]] + sw[i,k] # mean of LOR distributions (with multi-arm trial correction)
taud[i,k] <- tau *2*(k-1)/k # precision of LOR distributions (with multi-arm trial correction)
w[i,k] <- (delta[i,k] - d[t[i,k]] + d[t[i,1]]) # adjustment for multi-arm RCTs
sw[i,k] <- sum(w[i,1:k-1])/(k-1) # cumulative adjustment for multi-arm trials
}
}
totresdev <- sum(resdev[]) # Total Residual Deviance
d[1]<-0 # treatment effect is zero for reference treatment
beta[1] <- 0 # covariate effect is zero for reference treatment
for (k in 2:nt){ # LOOP THROUGH TREATMENTS
d[k] ~ dnorm(0,.0001) # vague priors for treatment effects
beta[k] <- B # common covariate effect
}
B ~ dnorm(0,.0001) # vague prior for covariate effect
sd ~ dunif(0,5) # vague prior for between-trial SD
tau <- pow(sd,-2) # between-trial precision = (1/between-trial variance)
} # *** PROGRAM ENDS
To obtain posterior summaries for other parameters of interest, the nodes d, B, and sd need to be monitored. To obtain the posterior means of the parameters required to assess model fit and model comparison, dev, totresdev, and the DIC (from the WinBUGS DIC tool) need to be monitored.
Additional code can be added before the closing brace to estimate all the pairwise log-odds ratios and odds ratios and to produce estimates of absolute effects, given additional information on the absolute treatment effect on one of the treatments, for given covariate values. For further details on calculating other summaries from the results and on converting the summaries onto other scales, refer to the appendix in Dias and others.13,56
###################################### ##########################################
# Extra code for calculating all odds ratios and log odds ratios, and absolute effects, for covariate
# values in vector z, with length nz (given as data)
####################### ############################ #############################
for (k in 1:nt){
for (j in 1:nz) { dz[j,k] <- d[k] + (beta[k]-beta[1])*z[j] } # treatment effect when covariate = z[j]
}
# pairwise ORs and LORs for all possible pair-wise comparisons
for (c in 1:(nt-1)) {
for (k in (c+1):nt) {
# when covariate is zero
or[c,k] <- exp(d[k] - d[c])
lor[c,k] <- (d[k]-d[c])
# at covariate=z[j]
for (j in 1:nz) {
orz[j,c,k] <- exp(dz[j,k] - dz[j,c])
lorz[j,c,k] <- (dz[j,k]-dz[j,c])
}
}
}
# Provide estimates of treatment effects T[k] on the natural (probability) scale
# Given a Mean Effect, meanA, for ‘standard’ treatment 1, with precision (1/variance) precA, and covariate value z[j]
A ~ dnorm(meanA,precA)
for (k in 1:nt) {
for (j in 1:nz){
logit(T[j,k]) <- A + d[k] + (beta[k]-beta[1]) * z[j]
}
}
For a meta-regression with 2 subgroups, vector z would be added to the list data statement as list(z=c(1), nz=1).
The data structure is identical to that presented in Dias and others13,56 but now has an added column x[] that represents the value of the covariate (taking values 0 or 1) for each trial. The remaining variables represent the number of treatments, nt, and the number of studies, ns; r[,1] and n[,1] are the numerators and denominators for the first treatment, r[,2] and n[,2] are the numerators and denominators for the second listed treatment, t[,1] and t[,2] are the treatment number identifiers for the first and second listed treatments, and na[] is the number of arms in each trial. Text is included after the hash symbol (#) for ease of reference to the original data source. Note that the data are provided as a list and a table component. Both components need to be loaded into WinBUGS for the program to run.
# Data (Statins example)
list(ns=19, nt=2)
t[,1] t[,2] na[] r[,1] n[,1] r[,2] n[,2] x[] # ID name
1 2 2 256 2223 182 2221 1 # 1 4S
1 2 2 4 125 1 129 1 # 2 Bestehorn
1 2 2 0 52 1 94 1 # 3 Brown
1 2 2 2 166 2 165 1 # 4 CCAIT
1 2 2 77 3301 80 3304 0 # 5 Downs
1 2 2 3 1663 33 6582 0 # 6 EXCEL
1 2 2 8 459 1 460 1 # 7 Furberg
1 2 2 3 155 3 145 1 # 8 Haskell
1 2 2 0 42 1 83 1 # 9 Jones
1 2 2 4 223 3 224 0 # 10 KAPS
1 2 2 633 4520 498 4512 1 # 12 LIPID
1 2 2 1 124 2 123 1 # 13 MARS
1 2 2 11 188 4 193 1 # 14 MAAS
1 2 2 5 78 4 79 1 # 15 PLAC 1
1 2 2 6 202 4 206 1 # 16 PLAC 2
1 2 2 3 532 0 530 0 # 17 PMSGCRP
1 2 2 4 178 2 187 1 # 18 Riegger
1 2 2 1 201 3 203 1 # 19 Weintraub
1 2 2 135 3293 106 3305 0 # 20 Wscotland
END
# Initial values
# Initial values for delta can be generated by WinBUGS.
#chain 1
list(d=c( NA, 0), mu=c(0,0,0,0,0, 0,0,0,0,0, 0,0,0,0,0, 0,0,0,0), B=0, sd=1)
#chain 2
list(d=c( NA, -1), mu=c(-3,-3,3,-3,3, -3,3,-3,3,-3, -3,-3,3,3,-3, 3,-3,-3,3), B=-1, sd=3)
#chain 3
list(d=c( NA, 2), mu=c(-3,5,-1,-3,7, -3,-4,-3,-3,0, 5,0,-2,-5,1, -2,5,3,0), B=1.5, sd=0.5)
Program 1(b): Binomial Likelihood, Logit Link, Fixed Effects, Meta-Regression with Subgroups (Statins Example)
# Binomial likelihood, logit link, subgroup
# Fixed effects model with one covariate
model{ # *** PROGRAM STARTS
for(i in 1:ns){ # LOOP THROUGH STUDIES
mu[i] ~ dnorm(0,.0001) # vague priors for all trial baselines
for (k in 1:na[i]) { # LOOP THROUGH ARMS
r[i,k] ~ dbin(p[i,k],n[i,k]) # binomial likelihood
# model for linear predictor, covariate effect relative to treat in arm 1
logit(p[i,k]) <- mu[i] + d[t[i,k]] - d[t[i,1]] + (beta[t[i,k]]-beta[t[i,1]]) * x[i]
rhat[i,k] <- p[i,k] * n[i,k] # expected value of the numerators
dev[i,k] <- 2 * (r[i,k] * (log(r[i,k])-log(rhat[i,k])) #Deviance contribution
+ (n[i,k]-r[i,k]) * (log(n[i,k]-r[i,k]) - log(n[i,k]-rhat[i,k])))
}
resdev[i] <- sum(dev[i,1:na[i]]) # summed residual deviance contribution for this trial
}
totresdev <- sum(resdev[]) # Total Residual Deviance
d[1] <- 0 # treatment effect is zero for reference treatment
beta[1] <- 0 # covariate effect is zero for reference treatment
for (k in 2:nt){ # LOOP THROUGH TREATMENTS
d[k] ~ dnorm(0,.0001) # vague priors for treatment effects
beta[k] <- B # common covariate effect
}
B ~ dnorm(0,.0001) # vague prior for covariate effect
} # *** PROGRAM ENDS
# Initial values
#chain 1
list(d=c( NA, 0), mu=c(0,0,0,0,0, 0,0,0,0,0, 0,0,0,0,0, 0,0,0,0), B=0)
#chain 2
list(d=c( NA, -1), mu=c(-3,-3,3,-3,3, -3,3,-3,3,-3, -3,-3,3,3,-3, 3,-3,-3,3), B=-1)
#chain 3
list(d=c( NA, 2), mu=c(-3,5,-1,-3,7, -3,-4,-3,-3,0, 5,0,-2,-5,1, -2,5,3,0), B=1.5)
The results (including the model fit statistics introduced in Technical Support Document 256) of the 2 separate analyses and the single analysis using the interaction model for fixed and random treatment effects models are shown in Table A3. For the FE models, convergence was achieved after 10,000 burn-in iterations for separate analyses (20,000 iterations for the joint analysis), and results are based on 50,000 samples from 3 independent chains. For the RE models, 40,000 burn-in iterations were used for the separate analyses, 50,000 burn-in iterations were used for the joint analysis, and results are based on 100,000 samples from 3 independent chains. Note that in an FE context, the 2 analyses deliver the same results for the treatment effects in the 2 groups, whereas in the RE analysis, due to the shared variance, treatment effects are not quite the same: they are more precise in the single analysis, particularly for the primary prevention subgroup, where there was less evidence available to inform the variance parameter, leading to very wide CrIs for all estimates in the separate RE meta-analysis. However, within the Bayesian framework, only the joint analysis offers a direct test of the interaction term β, which, in both cases, has a 95% CrI that includes the possibility of no interaction, although the point estimate is negative, suggesting that statins might be more effective in secondary prevention patients.
Table A3.
Statins Example15: Posterior Mean, SD, and 95% Credible Interval (CrI) for the Log-Odds Ratio (LOR) and Odds Ratio (OR) for All-Cause Mortality When Using Statins for Primary and Secondary Prevention Groups
| Fixed Effects |
Random Effects |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Primary Prevention |
Secondary Prevention |
Primary Prevention |
Secondary Prevention |
|||||||||
| Separate Analyses |
Separate Analyses |
|||||||||||
| Mean | SD | CrI | Mean | SD | CrI | Mean/Median | SD | CrI | Mean/Median | SD | CrI | |
| LOR | −0.11 | 0.10 | (−0.30, 0.09) | −0.31 | 0.05 | (−0.42, −0.21) | −0.18 | 0.74 | (−2.01, 1.12) | −0.36 | 0.16 | (−0.72, −0.06) |
| OR | 0.90 | 0.09 | (0.74, 1.09) | 0.73 | 0.04 | (0.66, 0.81) | 1.12 | 3.65 | (0.13, 3.07) | 0.71 | 0.11 | (0.49, 0.94) |
| σ | — | — | — | — | — | — | 0.79 | 0.98 | (0.06, 3.90) | 0.16 | 0.23 | (0.01, 0.86) |
| resdev | 16.9a | 29.0b | 11.9a | 28.3b | ||||||||
| pD | 6.0 | 15.0 | 9.3 | 16.8 | ||||||||
| DIC | 22.9 | 44.0 | 21.1 | 45.1 | ||||||||
| Single Analysis with Interaction Term, β, for Subgroup |
Single Analysis with Interaction Term, β, for Subgroup |
|||||||||||
| Mean | SD | CrI | Mean | SD | CrI | Mean/Median | SD | CrI | Mean/Median | SD | CrI | |
| β | −0.21 | 0.11 | (−0.42, 0.01) | −0.29 | 0.26 | (−0.86, 0.20) | ||||||
| LOR | −0.11 | 0.10 | (−0.30, 0.09) | −0.31 | 0.05 | (−0.42, −0.21) | −0.07 | 0.20 | (−0.48, 0.36) | −0.36 | 0.16 | (−0.72, −0.07) |
| OR | 0.90 | 0.09 | (0.74, 1.09) | 0.73 | 0.04 | (0.66, 0.81) | 0.95 | 0.21 | (0.62, 1.43) | 0.70 | 0.11 | (0.49, 0.94) |
| σ | — | — | — | — | — | — | 0.19 | 0.20 | (0.01, 0.76) | |||
| resdevc | 45.9 | 42.6 | ||||||||||
| pD | 21.0 | 24.2 | ||||||||||
| DIC | 66.9 | 66.8 | ||||||||||
Posterior median, standard deviation (SD), and 95% credible interval (CrI) of the between-trial heterogeneity (σ) for All-Cause Mortality When Using Statins for the fixed and random effects models and measures of model fit: posterior mean of the residual deviance (resdev), number of parameters (pD), and deviance information criterion (DIC). LOR <0 and OR <1 Favor Statins. NA, not applicable.
Compare with 10 data points.
Compare with 28 data points.
Compare with 38 data points.
Example 2. Certolizumab: Continuous Covariate
This example and results are described in the main text. The WinBUGS code for RE meta-regression model with a continuous covariate and noninformative priors is given in program 2(a), and the FE code is given in program 2(b). The relevant nodes to monitor are the same as in program 1.
Program 2(a): Binomial Likelihood, Logit Link, Random Effects, Meta-Regression with a Continuous Covariate (Certolizumab Continuous Covariate Example)
# Binomial likelihood, logit link, continuous covariate
# Random effects model for multi-arm trials
model{ # *** PROGRAM STARTS
for(i in 1:ns){ # LOOP THROUGH STUDIES
w[i,1] <- 0 # adjustment for multi-arm trials is zero for control arm
delta[i,1] <- 0 # treatment effect is zero for control arm
mu[i] ~ dnorm(0,.0001) # vague priors for all trial baselines
for (k in 1:na[i]) { # LOOP THROUGH ARMS
r[i,k] ~ dbin(p[i,k],n[i,k]) # binomial likelihood
# model for linear predictor, covariate effect relative to treat in arm 1 (centring)
logit(p[i,k]) <- mu[i] + delta[i,k] + (beta[t[i,k]]-beta[t[i,1]]) * (x[i]-mx)
rhat[i,k] <- p[i,k] * n[i,k] # expected value of the numerators
dev[i,k] <- 2 * (r[i,k] * (log(r[i,k])-log(rhat[i,k])) #Deviance contribution
+ (n[i,k]-r[i,k]) * (log(n[i,k]-r[i,k]) - log(n[i,k]-rhat[i,k])))
}
resdev[i] <- sum(dev[i,1:na[i]]) # summed residual deviance contribution for this trial
for (k in 2:na[i]) { # LOOP THROUGH ARMS
delta[i,k] ~ dnorm(md[i,k],taud[i,k]) # trial-specific LOR distributions
md[i,k] <- d[t[i,k]] - d[t[i,1]] + sw[i,k] # mean of LOR distributions (with multi-arm trial correction)
taud[i,k] <- tau *2*(k-1)/k # precision of LOR distributions (with multi-arm trial correction)
w[i,k] <- (delta[i,k] - d[t[i,k]] + d[t[i,1]]) # adjustment for multi-arm RCTs
sw[i,k] <- sum(w[i,1:k-1])/(k-1) # cumulative adjustment for multi-arm trials
}
}
totresdev <- sum(resdev[]) # Total Residual Deviance
d[1]<-0 # treatment effect is zero for reference treatment
beta[1] <- 0 # covariate effect is zero for reference treatment
for (k in 2:nt){ # LOOP THROUGH TREATMENTS
d[k] ~ dnorm(0,.0001) # vague priors for treatment effects
beta[k] <- B # common covariate effect
}
B ~ dnorm(0,.0001) # vague prior for covariate effect
sd ~ dunif(0,5) # vague prior for between-trial SD
tau <- pow(sd,-2) # between-trial precision = (1/between-trial variance)
} # *** PROGRAM ENDS
The data structure is the same as in program 1, but now we have more than 2 treatments being compared and need to add the mean covariate value mx to the list data, for centering.
# Data (Certolizumab example – covariate is disease duration)
list(ns=12, nt=7, mx=8.21)
t[,1] t[,2] na[] n[,1] n[,2] r[,1] r[,2] x[] # ID Study name
1 3 2 63 65 9 28 6.85 # 1 Kim 2007 (37)
1 3 2 200 207 19 81 10.95 # 2 DE019 Trial (36)
1 3 2 62 67 5 37 11.65 # 3 ARMADA Trial (34)
1 2 2 199 393 15 146 6.15 # 4 RAPID 1 Trial (40)
1 2 2 127 246 4 80 5.85 # 5 RAPID 2 Trial (41)
1 5 2 363 360 33 110 8.10 # 6 START Study (57)
1 5 2 110 165 22 61 7.85 # 7 ATTEST Trial (51)
1 5 2 47 49 0 15 8.30 # 8 Abe 2006 (50)
1 4 2 30 59 1 23 13.00 # 9 Weinblatt 1999 (49)
1 6 2 40 40 5 5 11.25 # 11 Strand 2006 (62)
1 7 2 49 50 14 26 0.92 # 12 CHARISMA Study (64)
1 7 2 204 205 22 90 7.65 # 13 OPTION Trial (67)
END
To estimate all the pairwise log-odds ratios, odds ratios, and absolute effects, for covariate values 0, 3, and 5, vector z could be added to the list data as list(z=c(0,3,5), nz=3).
# Initial values
# Initial values for delta can be generated by WinBUGS.
#chain 1
list(d=c( NA, 0,0,0,0,0,0), mu=c(0, 0, 0, 0, 0, 0, 0, 0, 0, 0,0,0), sd=1, B=0)
#chain 2
list(d=c( NA, -1,1,-1,1,-1,1), mu=c(-3, -3, -3, -3, -3, -3, -3, -3, -3, -3, -3, -3), sd=0.5, B=-1)
#chain 3
list(d=c( NA, 2,-2,2,-2,2,-2), mu=c(-3, 5, -1, -3, 7, -3, -4, -3, -3, 0, 5, 0), sd=3, B=5)
An RE model with Uniform(0, 5) prior for σ, the heterogeneity parameter is not identifiable. This is because there is a trial with a zero cell and not many replicates of each comparison. Due to the paucity of information from which the between-trial variation can be estimated, in the absence of an informative prior on σ, the relative treatment effect for this trial will tend toward infinity. We have therefore used an informative half-normal prior, represented by the solid line in Figure A1, which ensures stable computation: .
This prior distribution was chosen to ensure that, a priori, 95% of the trial-specific ORs lie within a factor of 2 from the median OR for each comparison. Under this prior, the mean σ is 0.26. To fit the RE meta-regression model with this prior distribution, the line of code annotated as “vague prior for between-trial SD” in program 2(a) should be replaced with the following 2 lines:
sd ~ dnorm(0,prec)I(0,) # prior for between-trial SD
prec <- pow(0.32,-2)
This prior should not be used unthinkingly. Informative prior distributions allowing wider or narrower ranges of values can be used by changing the value of prec in the code above.
In this example, the posterior distribution obtained for σ is given by the dotted line in Figure A1 and shows that the range of plausible values for σ has not changed much, but the probability that σ will have values close to zero has decreased.
Program 2(b): Binomial Likelihood, Logit Link, Fixed Effects, Meta-Regression with a Continuous Covariate (Certolizumab Continuous Covariate Example)
# Binomial likelihood, logit link
# Fixed effects model with continuous covariate
model{ # *** PROGRAM STARTS
for(i in 1:ns){ # LOOP THROUGH STUDIES
mu[i] ~ dnorm(0,.0001) # vague priors for all trial baselines
for (k in 1:na[i]) { # LOOP THROUGH ARMS
r[i,k] ~ dbin(p[i,k],n[i,k]) # binomial likelihood
# model for linear predictor, covariate effect relative to treat in arm 1
logit(p[i,k]) <- mu[i] + d[t[i,k]] - d[t[i,1]] + (beta[t[i,k]]-beta[t[i,1]]) * (x[i]-mx)
rhat[i,k] <- p[i,k] * n[i,k] # expected value of the numerators
dev[i,k] <- 2 * (r[i,k] * (log(r[i,k])-log(rhat[i,k])) #Deviance contribution
+ (n[i,k]-r[i,k]) * (log(n[i,k]-r[i,k]) - log(n[i,k]-rhat[i,k])))
}
resdev[i] <- sum(dev[i,1:na[i]]) # summed residual deviance contribution for this trial
}
totresdev <- sum(resdev[]) # Total Residual Deviance
d[1] <- 0 # treatment effect is zero for reference treatment
beta[1] <- 0 # covariate effect is zero for reference treatment
for (k in 2:nt){ # LOOP THROUGH TREATMENTS
d[k] ~ dnorm(0,.0001) # vague priors for treatment effects
beta[k] <- B # common covariate effect
}
B ~ dnorm(0,.0001) # vague prior for covariate effect
} # *** PROGRAM ENDS
# Initial values
#chain 1
list(d=c( NA, 0,0,0,0,0,0), mu=c(0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0, 0), B=0)
#chain 2
list(d=c( NA, -1,1,-1,1,-1,1), mu=c(-3, -3, -3, -3, -3, -3, -3, -3, -3, -3, -3, -3), B=-2)
#chain 3
list(d=c( NA, 2,-2,2,-2,2,-2), mu=c(-3, 5, -1, -3, 7, -3, -4, -3, -3, 0, 5, 0), B=5)
Example 3. Certolizumab: Baseline Risk
This example and results are described in the main text. The WinBUGS code for the meta-regression model with adjustment for baseline risk for random and fixed treatment effects is similar to programs 2(a) and 2(b), respectively, but now x[i] is replaced with mu[i] in the definitions of the linear predictor. The variability of the normal prior distribution needs to be reduced to avoid numerical errors (this only minimally affects the posterior results). The relevant nodes to monitor are the same as in program 1.
Program 3(a): Binomial Likelihood, Logit Link, Random Effects, Meta-Regression with Adjustment for Baseline Risk (Certolizumab Baseline Risk Example)
# Binomial likelihood, logit link
# Random effects model for multi-arm trials
model{ # *** PROGRAM STARTS
for(i in 1:ns){ # LOOP THROUGH STUDIES
w[i,1] <- 0 # adjustment for multi-arm trials is zero for control arm
delta[i,1] <- 0 # treatment effect is zero for control arm
mu[i] ~ dnorm(0,.001) # vague priors for all trial baselines
for (k in 1:na[i]) { # LOOP THROUGH ARMS
r[i,k] ~ dbin(p[i,k],n[i,k]) # binomial likelihood
# model for linear predictor, covariate effect relative to treat in arm 1
logit(p[i,k]) <- mu[i] + delta[i,k] + (beta[t[i,k]]-beta[t[i,1]]) * (mu[i]-mx)
rhat[i,k] <- p[i,k] * n[i,k] # expected value of the numerators
dev[i,k] <- 2 * (r[i,k] * (log(r[i,k])-log(rhat[i,k])) #Deviance contribution
+ (n[i,k]-r[i,k]) * (log(n[i,k]-r[i,k]) - log(n[i,k]-rhat[i,k])))
}
resdev[i] <- sum(dev[i,1:na[i]]) # summed residual deviance contribution for this trial
for (k in 2:na[i]) { # LOOP THROUGH ARMS
delta[i,k] ~ dnorm(md[i,k],taud[i,k]) # trial-specific LOR distributions
md[i,k] <- d[t[i,k]] - d[t[i,1]] + sw[i,k] # mean of LOR distributions (with multi-arm trial correction)
taud[i,k] <- tau *2*(k-1)/k # precision of LOR distributions (with multi-arm trial correction)
w[i,k] <- (delta[i,k] - d[t[i,k]] + d[t[i,1]]) # adjustment for multi-arm RCTs
sw[i,k] <- sum(w[i,1:k-1])/(k-1) # cumulative adjustment for multi-arm trials
}
}
totresdev <- sum(resdev[]) # Total Residual Deviance
d[1]<-0 # treatment effect is zero for reference treatment
beta[1] <- 0 # covariate effect is zero for reference treatment
for (k in 2:nt){ # LOOP THROUGH TREATMENTS
d[k] ~ dnorm(0,.0001) # vague priors for treatment effects
beta[k] <- B # common covariate effect
}
B ~ dnorm(0,.0001) # vague prior for covariate effect
sd ~ dunif(0,5) # vague prior for between-trial SD
tau <- pow(sd,-2) # between-trial precision = (1/between-trial variance)
} # *** PROGRAM ENDS
The data structure is the same as example 1, but without variable x[].
# Data (Certolizumab, baseline risk)
list(ns=12, nt=7, mx=-2.421)
t[,1] t[,2] na[] n[,1] n[,2] r[,1] r[,2] # ID Study name
1 3 2 63 65 9 28 # 1 Kim 2007 (37)
1 3 2 200 207 19 81 # 2 DE019 Trial (36)
1 3 2 62 67 5 37 # 3 ARMADA Trial (34)
1 2 2 199 393 15 146 # 4 RAPID 1 Trial (40)
1 2 2 127 246 4 80 # 5 RAPID 2 Trial (41)
1 5 2 363 360 33 110 # 6 START Study (57)
1 5 2 110 165 22 61 # 7 ATTEST Trial (51)
1 5 2 47 49 0 15 # 8 Abe 2006 (50)
1 4 2 30 59 1 23 # 9 Weinblatt 1999 (49)
1 6 2 40 40 5 5 # 11 Strand 2006 (62)
1 7 2 49 50 14 26 # 12 CHARISMA Study (64)
1 7 2 204 205 22 90 # 13 OPTION Trial (67)
END
# Initial values
# Initial values for delta and other variables can be generated by WinBUGS.
#chain 1
list(d=c( NA, 0,0,0,0,0,0), mu=c(0, 0, 0, 0, 0, 0, 0, 0, 0, 0,0,0), sd=1, B=0)
#chain 2
list(d=c( NA, -1,1,-1,1,-1,1), mu=c(-3, -3, -3, -3, -3, -3, -3, -3, -3, -3, -3, -3), sd=0.5, B=-1)
#chain 3
list(d=c( NA, 2,-2,2,-2,2,-2), mu=c(-3, 5, -1, -3, 7, -3, -4, -3, -3, 0, 5, 0), sd=3, B=5)
Program 3(b): Binomial Likelihood, Logit Link, Fixed Effects, Meta-Regression with Adjustment for Baseline Risk (Certolizumab Baseline Risk Example)
# Binomial likelihood, logit link
# Fixed effects model with one covariate (independent covariate effects)
model{ # *** PROGRAM STARTS
for(i in 1:ns){ # LOOP THROUGH STUDIES
mu[i] ~ dnorm(0,.001) # vague priors for all trial baselines
for (k in 1:na[i]) { # LOOP THROUGH ARMS
r[i,k] ~ dbin(p[i,k],n[i,k]) # binomial likelihood
# model for linear predictor, covariate effect relative to treat in arm 1
logit(p[i,k]) <- mu[i] + d[t[i,k]] - d[t[i,1]] + (beta[t[i,k]]-beta[t[i,1]]) * (mu[i]-mx)
rhat[i,k] <- p[i,k] * n[i,k] # expected value of the numerators
dev[i,k] <- 2 * (r[i,k] * (log(r[i,k])-log(rhat[i,k])) #Deviance contribution
+ (n[i,k]-r[i,k]) * (log(n[i,k]-r[i,k]) - log(n[i,k]-rhat[i,k])))
}
resdev[i] <- sum(dev[i,1:na[i]]) # summed residual deviance contribution for this trial
}
totresdev <- sum(resdev[]) # Total Residual Deviance
d[1] <- 0 # treatment effect is zero for reference treatment
beta[1] <- 0 # covariate effect is zero for reference treatment
for (k in 2:nt){
d[k] ~ dnorm(0,.0001) # vague priors for treatment effects
beta[k] <- B # common covariate effect
}
B ~ dnorm(0,.0001) # vague prior for covariate effect
} # *** PROGRAM ENDS
# Initial values
#chain 1
list(d=c( NA, 0,0,0,0,0,0), mu=c(0, 0, 0, 0, 0, 0, 0, 0, 0, 0,0,0), B=0)
#chain 2
list(d=c( NA, -1,1,-1,1,-1,1), mu=c(-3, -3, -3, -3, -3, -3, -3, -3, -3, -3, -3, -3), B=-2)
#chain 3
list(d=c( NA, 2,-2,2,-2,2,-2), mu=c(-3, 5, -1, -3, 7, -3, -4, -3, -3, 0, 5, 0), B=5)
Footnotes
This series of tutorial papers were based on Technical Support Documents in Evidence Synthesis (available from http://www.nicedsu.org.uk), which were prepared with funding from the NICE Decision Support Unit. The views, and any errors or omissions, expressed in this document are of the authors only.
References
- 1. National Institute for Health and Clinical Excellence (NICE) Guide to the Methods of Technology Appraisal. London, UK: NICE; 2008 [PubMed] [Google Scholar]
- 2. Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.0 [updated February 2008]. Chichester, UK: The Cochrane Collaboration, Wiley; 2008 [Google Scholar]
- 3. Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias: dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA. 1995;273(5):408–12 [DOI] [PubMed] [Google Scholar]
- 4. Wood L, Egger M, Gluud LL, et al. Empirical evidence of bias in treatment effect estimates in controlled trials with different interventions and outcomes: meta-epidemiological study. BMJ. 2008;336:601–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Higgins JPT, Thompson SG, Spiegelhalter DJ. A re-evaluation of random-effects meta-analysis. J R Stat Soc Ser A. 2009;172:137–59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ades AE, Lu G, Higgins JPT. The interpretation of random effects meta-analysis in decision models. Med Decis Making. 2005;25(6):646–54 [DOI] [PubMed] [Google Scholar]
- 7. Welton NJ, White I, Lu G, Higgins JPT, Ades AE, Hilden J. Correction: interpretation of random effects meta-analysis in decision models. Med Decis Making. 2007;27:212–4 [DOI] [PubMed] [Google Scholar]
- 8. Spiegelhalter DJ, Abrams KR, Myles J. Bayesian Approaches to Clinical Trials and Health-Care Evaluation. New York: John Wiley; 2004 [Google Scholar]
- 9. Thompson SG. Why sources of heterogeneity in meta-analyses should be investigated. BMJ. 1994;309:1351–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Thompson SG. Why and how sources of heterogeneity should be investigated. In: Egger M, Davey Smith G, Altman D, eds. Systematic Reviews in Health Care: Meta-Analysis in Context. 2nd ed. London, UK: BMJ Books; 2001. p 157–75 [Google Scholar]
- 11. Turner RM, Davey J, Clarke MJ, Thompson SG, Higgins JPT. Predicting the extent of heterogeneity in meta-analysis, using empirical data from the Cochrane Database of Systematic Reviews. Int J Epidemiol. 2012;41:818–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to Meta-Analysis. Chichester, UK: John Wiley; 2009 [Google Scholar]
- 13. Dias S, Sutton AJ, Ades AE, Welton NJ. Evidence synthesis for decision making 2: a generalized linear modeling framework for pairwise and network meta-analysis of randomized controlled trials. Med Decis Making. 2013;33(5):2013;33(5):607-617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Dias S, Welton NJ, Sutton AJ, Caldwell DM, Lu G, Ades AE. Evidence synthesis for decision making 4: inconsistency in networks of evidence based on randomized controlled trials. Med Decis Making. 2013;33(5):641-656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sutton AJ. Meta-Analysis Methods for Combining Information from Different Sources Evaluating Health Interventions. Leicester, UK: University of Leicester; 2002 [Google Scholar]
- 16. Dias S, Sutton AJ, Welton NJ, Ades AE. NICE DSU Technical Support Document 3: Heterogeneity: subgroups, meta-regression, bias and bias-adjustment. 2011. Available from: http://www.nicedsu.org.uk [PubMed]
- 17. Cooper NJ, Sutton AJ, Morris D, Ades AE, Welton NJ. Addressing between-study heterogeneity and inconsistency in mixed treatment comparisons: application to stroke prevention treatments in individuals with non-rheumatic atrial fibrillation. Stat Med. 2009;28:1861–81 [DOI] [PubMed] [Google Scholar]
- 18. Nixon R, Bansback N, Brennan A. Using mixed treatment comparisons and meta-regression to perform indirect comparisons to estimate the efficacy of biologic treatments in rheumatoid arthritis. Stat Med. 2007;26(6):1237–54 [DOI] [PubMed] [Google Scholar]
- 19. Draper NR, Smith H. Applied Regression Analysis. 3rd ed. New York: John Wiley; 1998 [Google Scholar]
- 20. National Institute for Health and Clinical Excellence Certolizumab pegol for the treatment of rheumatoid arthritis. 2010. Report No. TA186. Available from: http://guidance.nice.org.uk/TA186
- 21. Lunn DJ, Thomas A, Best N, Spiegelhalter D. WinBUGS—a Bayesian modelling framework: concepts, structure, and extensibility. Stat Comput. 2000;10:325–37 [Google Scholar]
- 22. Spiegelhalter DJ, Best NG, Carlin BP, van der Linde A. Bayesian measures of model complexity and fit. J R Stat Soc Ser B. 2002;64(4):583–616 [Google Scholar]
- 23. McIntosh MW. The population risk as an explanatory variable in research synthesis of clinical trials. Stat Med. 1996;15:1713–28 [DOI] [PubMed] [Google Scholar]
- 24. Thompson SG, Smith TC, Sharp SJ. Investigating underlying risk as a source of heterogeneity in meta-analysis. Stat Med. 1997;16:2741–58 [DOI] [PubMed] [Google Scholar]
- 25. Welton NJ, Ades AE, Carlin JB, Altman DG, Sterne JAC. Models for potentially biased evidence in meta-analysis using empirically based priors. J R Stat Soc Ser A. 2009;172(1):119–36 [Google Scholar]
- 26. Savovic J, Harris RJ, Wood L, et al. Development of a combined database for meta-epidemiological research. Res Synthesis Methods. 2010;1:212–25 [DOI] [PubMed] [Google Scholar]
- 27. Dias S, Welton NJ, Marinho VCC, Salanti G, Higgins JPT, Ades AE. Estimation and adjustment of bias in randomised evidence by using mixed treatment comparison meta-analysis. J R Stat Soc Ser A. 2010;173(3):613–29 [Google Scholar]
- 28. Salanti G, Dias S, Welton NJ, et al. Evaluating novel agent effects in multiple treatments meta-regression. Stat Med. 2010;29:2369–83 [DOI] [PubMed] [Google Scholar]
- 29. Dias S, Welton NJ, Ades AE. Study designs to detect sponsorship and other biases in systematic reviews. J Clin Epidemiol. 2010;63:587–8 [DOI] [PubMed] [Google Scholar]
- 30. Moreno SG, Sutton AJ, Ades AE, et al. Assessment of regression-based methods to adjust for publication bias through a comprehensive simulation study. BMC Med Res Methodol. 2009;9:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Moreno SG, Sutton AJ, Turner EH, et al. Novel methods to deal with publication biases: secondary analysis of antidepressant trials in the FDA trial registry database and related journal publications. BMJ. 2009;339:b2981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Turner RM, Spiegelhalter DJ, Smith GCS, Thompson SG. Bias modelling in evidence synthesis. J R Stat Soc Ser A. 2009;172:21–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Dias S, Welton NJ, Sutton AJ, Ades AE. Evidence synthesis for decision making 5: the baseline natural history model. Med Decis Making. 2013;33(5):657-670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Madan J, Stevenson MD, Ades AE, Cooper KL, Whyte S, Akehurst R. Consistency between direct and indirect trial evidence: is direct evidence always more reliable? Value Health. 2011;14:953–60 [DOI] [PubMed] [Google Scholar]
- 35. Welton NJ, Sutton AJ, Cooper NJ, Abrams KR, Ades AE. Evidence Synthesis for Decision Making in Healthcare. New York: John Wiley; 2012 [Google Scholar]
- 36. Higgins JPT, Thompson SG. Controlling the risk of spurious findings from meta-regression. Stat Med. 2004;23:1663–82 [DOI] [PubMed] [Google Scholar]
- 37. Rothman KJ, Greenland S, Lash TL. Modern Epidemiology. 3rd ed. Philadelphia, PA: Lippincott, Williams & Wilkins; 2008 [Google Scholar]
- 38. Lambert PC, Sutton AJ, Abrams KR, Jones DR. A comparison of summary patient-level covariates in meta-regression with individual patient data meta-analysis. J Clin Epidemiol. 2002;55:86–94 [DOI] [PubMed] [Google Scholar]
- 39. Berlin JA, Santanna J, Schmid CH, Szczech LA, Feldman HI. Individual patient- versus group-level data meta-regressions for the investigation of treatment effect modifiers: ecological bias rears its ugly head. Stat Med. 2002;21:371–87 [DOI] [PubMed] [Google Scholar]
- 40. Stewart LA, Clarke MJ. Practical methodology of meta-analyses (overviews) using updated individual patient data. Stat Med. 1995;14:2057–79 [DOI] [PubMed] [Google Scholar]
- 41. Simmonds MC, Higgins JPT, Stewart LA, Tierney JF, Clarke MJ, Thompson SG. Meta-analysis of individual patient data from randomized trials: a review of methods used in practice. Clin Trials. 2005;2:209–17 [DOI] [PubMed] [Google Scholar]
- 42. Higgins JPT, Whitehead A, Turner RM, Omar RZ, Thompson SG. Meta-analysis of continuous outcome data from individual patients. Stat Med. 2001;20:2219–41 [DOI] [PubMed] [Google Scholar]
- 43. Goldstein H, Yang M, Omar RZ, Turner RM, Thompson SG. Meta-analysis using multilevel models with an application to the study of class size effects. Appl Stat. 2000;49:399–412 [Google Scholar]
- 44. Turner RM, Omar RZ, Yang M, Goldstein H, Thompson SG. A multilevel model framework for meta-analysis of clinical trials with binary outcomes. Stat Med. 2000;19:3417–32 [DOI] [PubMed] [Google Scholar]
- 45. Tudor Smith C, Williamson PR, Marson AG. Investigating heterogeneity in an individual patient data meta-analysis of time to event outcomes. Stat Med. 2005;24:1307–19 [DOI] [PubMed] [Google Scholar]
- 46. Whitehead A, Omar RZ, Higgins JPT, Savaluny E, Turner RM, Thompson SG. Meta-analysis of ordinal outcomes using individual patient data. Stat Med. 2001;20:2243–60 [DOI] [PubMed] [Google Scholar]
- 47. Tudor Smith C, Marson AG, Chadwick DW, Williamson PR. Multiple treatment comparisons in epilepsy monotherapy trials. Trials. 2007;8:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Achana FA, Cooper NJ, Dias S, et al. Extending methods for investigating the relationship between treatment effect and baseline risk from pairwise meta-analysis to network meta-analysis. Stat Med. 2013;32:752–71 [DOI] [PubMed] [Google Scholar]
- 49. Saramago P, Sutton AJ, Cooper NJ, Manca A. Mixed treatment comparisons using aggregate and individual participant level data. Stat Med. 2012;31:3516–36 [DOI] [PubMed] [Google Scholar]
- 50. Donegan S, Williamson P, D’Alessandro U, Garner P, Tudor Smith C. Combining individual patient data and aggregate data in mixed treatment comparison meta-analysis: individual patient data may be beneficial if only for a subset of trials. Stat Med. 2013;32:914–30 [DOI] [PubMed] [Google Scholar]
- 51. Donegan S, Williamson P, D’Alessandro U, Tudor Smith C. Assessing the consistency assumption by exploring treatment by covariate interactions in mixed treatment comparison meta-analysis: individual patient-level covariates versus aggregate trial-level covariates. Stat Med. 2012;31:3840–57 [DOI] [PubMed] [Google Scholar]
- 52. Simmonds MC, Higgins JPT. Covariate heterogeneity in meta-analysis: criteria for deciding between meta-regression and individual patient data. Stat Med. 2007;26:2982–99 [DOI] [PubMed] [Google Scholar]
- 53. Riley RD, Abrams KR, Lambert PC, Sutton AJ, Thompson JR. An evaluation of bivariate random-effects meta-analysis for the joint synthesis of two correlated outcomes. Stat Med. 2007;26:78–97 [DOI] [PubMed] [Google Scholar]
- 54. Riley RD, Lambert PC, Staessen JA, Wang J, Gueyffier F, Boutitie F. Meta-analysis of continuous outcomes combining individual patient data and aggregate data. Stat Med. 2008;27:1870–93 [DOI] [PubMed] [Google Scholar]
- 55. Sutton AJ, Kendrick D, Coupland CAC. Meta-analysis of individual- and aggregate-level data. Stat Med. 2008;27:651–69 [DOI] [PubMed] [Google Scholar]
- 56. Dias S, Welton NJ, Sutton AJ, Ades AE. NICE DSU Technical Support Document 2: A generalised linear modelling framework for pair-wise and network meta-analysis of randomised controlled trials. 2011. Available from: http://www.nicedsu.org.uk [PubMed]


