Abstract
Background
Hip fracture patients have, in several studies, been shown to have excessive mortality. There is, however, a lack of mortality data, in comparison to incidence data, from the last decade in particular.
Objective
To study short- and long-term mortality in a population-based cohort of hip fracture patients over the last decade and compare it to the background population.
Patients and methods
Fragility hip fracture patients in the two most southern counties in Norway who experienced fractures in 2004 and 2005 were studied. For each patient, three controls were randomly recruited from the background population matched for age, sex, and residency. Overall, age-, gender-, and group-specific mortality rates were calculated.
Results
A total of 942 (267 male and 675 female) patients with a fragility hip fracture were identified. In the hip fracture patients, overall mortality rate after 1 year was 21.3% (males 30.7% and females 19.1%, P < 0.005) and, after 5 years, 59.0% (males 70.0% and females 54.6%, P < 0.005). The corresponding figures for matched controls were 5.6% (males 5.9%, females 5.4%, P = 0.6) and 24.9% (males 25.9%, females 24.5%, P = 0.4), respectively. A statistically significant difference was seen in the log-rank statistical analysis between hip fracture patients and controls, both in males (P < 0.0005) and females (P < 0.0005), and for age groups 50–80 years (P < 0.0005) and 80 years and older (P < 0.0005).
Conclusion
Mortality in males and females with hip fractures is high not only in the first year after fracture, but remains higher than in the background population during 5 years of follow-up. The high mortality in hip fracture patients remains a challenge both in middle-aged and elderly individuals. Optimization of post-fracture treatment and care could reduce mortality of hip fracture in middle-aged and elderly individuals.
Keywords: hip fracture, mortality, survival, population-based study
Introduction
Mortality in fragility hip fracture in middle-aged and elderly men and women has, in several studies, been reported to be higher compared to the general population and to be higher in men than in women.1,2 Whether or not the excess mortality of the fragility hip fracture persists over time is not yet clarified.1,3–8 In a recent published meta-analysis, researchers concluded that mortality in hip fracture patients remains increased over time.1
A decline in hip fracture incidence has been reported in parts of the Western world during the past decade.9,10 The exact reasons for the falling incidence are unknown. Recently, this tendency towards a lower incidence of hip fracture was also shown in Norway for females, but not for males.10 This decline is suggested, in part, to be explained by the increased use of bisphosphonates over the last 10–20 years.10 Interestingly, there is also some evidence of a beneficial effect on mortality in hip fracture patients treated with bisphosphonates.11–13 In general, there is a lack of updated, population-based, long-term (5 years and over) mortality data in hip fracture patients from the past decade. Thus, our aim was to study the short- and long-term mortality of fragility hip fractures in males and females in Norway over the last decade.
Patients and methods
Identification of fragility hip fracture patients
Patients aged 50 years or older with a fragility hip fracture were identified in 2004 and 2005 from four hospitals (Kristiansand, Arendal, Flekkefjord, and Mandal) located in the two most southern counties in Norway (Vest-Agder and Aust-Agder counties). The four hospitals are the only referral centers for orthopedic trauma in southern Norway. Data on incidence of hip fracture from this patient cohort have previously been described in detail.14 In short, the hospital electronic diagnosis registers were used to identify all hip fracture patients coded as S72.0-2 according to the International Classification of Diseases 10th Revision (ICD-10) in the 2-year period.15 For all individuals, data on sex, date of birth, date of hip fracture, and place of residency were collected. The identified patients’ medical records and X-ray records were examined, and the diagnosis of hip fracture was confirmed before being included in the study. We excluded pathological fractures, eg, those caused by tumor.
Each of the fragility hip fracture patients was matched to three controls of the same sex who were born near the same date (±15 days) and lived in the same municipality. The matching of each patient to controls was performed by the Norwegian National Register. The follow-up time for a patient was from the month the fracture occurred to death or to the censoring dates of January 1, 2010 or January 1, 2011; for a control, this was to death or to the censoring dates of January 1, 2010 or January 1, 2011.
Statistical methods
Hip fracture mortality rates were calculated for the first year and for the entire 5-year period for all patients, separately for each sex and for the age subgroups 50–80 years and 80 years and older for each sex. Mortality in hip fracture patients and controls was analyzed by using Kaplan–Meier survival curves. The data for each sex were analyzed for all and for the two groups of the hip fracture population, ie, older and younger than 80 years old. This cutoff was chosen as it represented the main age of our patients. We compared differences in survival probabilities between fragility hip fracture patients and the control population and between patients living in rural and urban areas by logrank statistical analysis. The relative risk (RR) for hip fracture mortality was calculated for different time periods during the 5-year period by comparing mortality in hip fracture patients with controls. The association between mortality after 1 year as the dependent variable and hip fracture, sex, age, hospital, and urban/rural areas as the independent variables was tested in a multivariate regression model. All the analyses were performed using SPSS version 17.0 (SPSS, Chicago, IL, USA). Statistical significance was defined as P < 0.05.
Ethics
The study was approved by the Regional Committee for Medical Research Ethics for Southern and Eastern Norway, Oslo, Norway.
Funding
This work was supported and funded by the Competence Development Fund of Southern Norway and Hospital of Southern Norway Trust.
Results
Fragility hip fracture and age-and sex-specific mortality rates
As previously reported in our incidence study,14 of hip fracture, a total of 951 patients (271 males and 680 females) were identified with a hip fracture in the catchment area in the 2-year period.14 Nine hip fracture patients (four males and five females) could not be identified by the Norwegian National Register, which performed the matching of patients with controls. The 942 patients (267 males and 675 females) included in this study had a mean age of 81.2 years (males 80.0 years and females 81.8 years).
In both sexes, elevated mortality rates in hip fracture patients were observed compared with the controls (Table 1). In the hip fracture patients, overall mortality after the first year was 21.3% (males 30.7% and females 19.1%, P < 0.005) and, after 5 years, 59.0% (males 70.0% and females 54.6%, P < 0.005). The overall mortality rates for the age group 50–80 years for the first year after fracture was 10.7% (95% confidence interval [CI]: 7.6–13.7 [males 15.0 and females 8.7, P < 0.2]) and after 5 years 38.5% (95% CI: 33.6–43.3 [males 46.0 and females 34.9, P < 0.03]). The overall mortality rate for patients older than 80 years with a fragility hip fracture at the end of the first year was 28.7% (95% CI: 24.9–32.4 [males 44.6 and females 23.3, P < 0.005]) and, at the end of the fifth year, 73.4% (95% CI: 69.7–77.0 [males 91.4 and females 67.2, P < 0.005]).
Table 1.
Outcome, mortality rates, and relative risk of fragility hip fracture patients compared to controls at the first and fifth years after hip fracture in southern Norway in 2004–2005
| Age at the time of injury | Patients, n | Controls, n | Number of deceased
|
|
Mortality rate per 100 patient-years (95% CI)
|
Relative risk (95% CI)
|
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1st year
|
5th year
|
||||||||||
| Patients, n | Controls, n | Patients, n | Controls, n | 1 st year | 5th year | 1 st year | 5th year | ||||
| Males | 50–80 years | 126 | 351 | 19 | 10 | 58 | 45 | 15.0(8.7–21.2) | 46.0* (37.3–54.7) | 5.2(2.5–11.0) | 3.5 (2.5–5.0) |
| 80+ years | 141 | 450 | 63 | 38 | 129 | 163 | 44.6* (36.4–52.8) | 91.4* (86.7–96.0) | 3.9 (2.7–5.7) | 2.5 (2.2–2.8) | |
| All | 267 | 801 | 82 | 48 | 187 | 208 | 30.7(26.8–38.1) | 70.0 (64.5–75.5) | 4.1 (2.9–5.8) | 2.0(1.7–2.3) | |
| Females | 50–80 years | 263 | 723 | 23 | 14 | 92 | 65 | 8.7(5.3–12.1) | 34.9* (29.1–40.6) | 4.5(2.2–8.1) | 3.1 (2.3–4.2) |
| 80+ years | 412 | 1302 | 96 | 96 | 277 | 431 | 23.3* (19.2–27.3) | 67.2* (62.6–71.7) | 2.7(2.1–3.6) | 2.0(1.8–2.2) | |
| All | 675 | 2025 | 119 | 110 | 369 | 496 | 19.1 (16.1–22.0) | 54.6 (50.8–58.3) | 2.9 (2.3–3.7) | 1.8(1.6–2.0) | |
| All | 50–80 years | 389 | 1074 | 42 | 24 | 150 | 110 | 10.7(7.6–13.7) | 38.5 (33.6–43.3) | 4.8 (2.9–7.8) | 3.7 (3.0–4.6) |
| 80+ years | 553 | 1752 | 159 | 134 | 406 | 594 | 28.7 (24.9–32.4) | 73.4 (69.7–77.0) | 3.7 (3.0–4.6) | 2.1 (1.9–2.3) | |
| All | 942 | 2826 | 201 | 158 | 556 | 704 | 21.3(18.7–23.9) | 59.0(55.8–62.1) | 3.8(3.1–4.6) | 2.3(2.1–2.5) | |
Note:
Statistically significant difference between the sexes (P < 0.05).
Abbreviation: CI, confidence interval.
RR of dying for the fragility hip fracture group
The overall RR for males and females with a fragility hip fracture compared to the control group for the first year was 4.1 and 2.9, respectively and, after 5 years, 2.0 and 1.8, respectively. For the age group 50–80 years, the RR for the first year was 5.2 for males and 4.5 for females and, after 5 years, 3.5 and 3.1 for males and females, respectively. For the age group 80+ years, the RR for the first year was 3.9 and 2.7 for males and females, respectively, and, for the fifth year, 2.5 and 2.0 for males and females, respectively (Table 1).
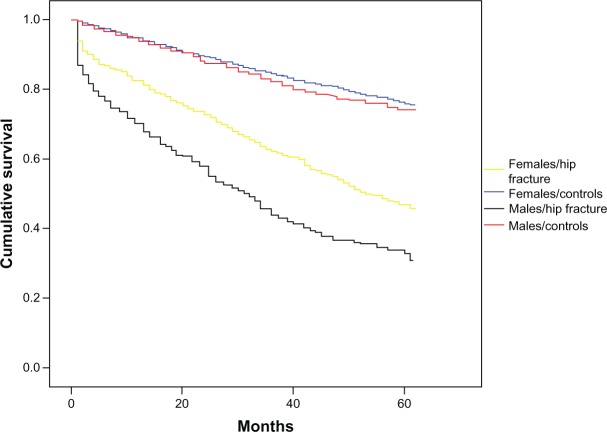
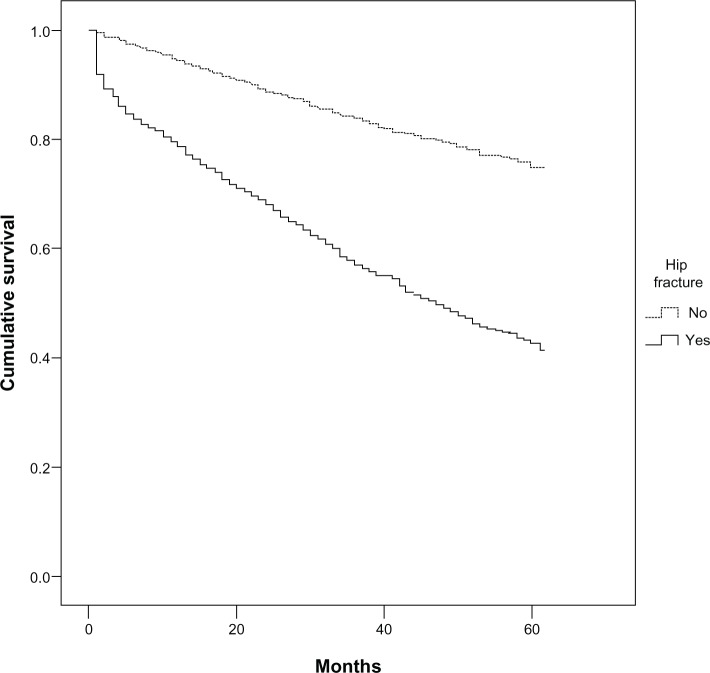
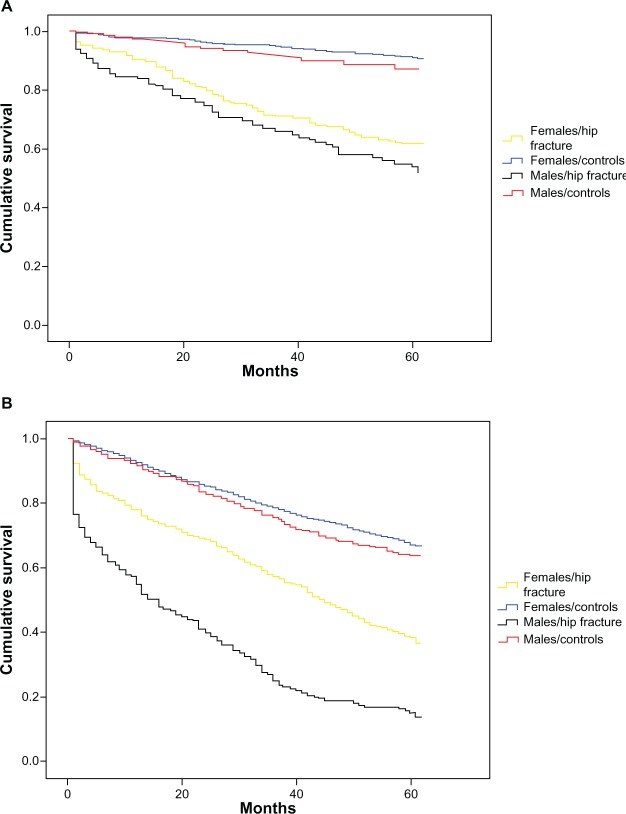
Kaplan–Meier survival curves
Cumulative survival for the fragility hip fracture patient group was lower compared to the matched controls for all patients with hip fracture, including both males and females and the two age subgroups (50–80 years and 80+ years), with more striking differences in males than in females (Figures 1–3). A statistically significant difference was seen in the log-rank statistical analysis between hip fracture patients and controls, both in males (P < 0.0005) and in females (P < 0.0005), and for the two age subgroups (50–80 years, P < 0.0005 and 80+ years, P < 0.0005) in both sexes.
Figure 1.
Kaplan–Meier survival analysis in males and females with a fragility hip fracture in 2004–2005 in southern Norway compared to matched controls.
Figure 3.
Kaplan–Meier survival analysis in patients with a fragility hip fracture in 2004–2005 in southern Norway (indicated with Yes) compared to matched controls (indicated with No).
Mortality odds ratio (OR)
In Table 2, an estimation of OR after hip fracture according to the time after fracture, is presented. The OR is highest in the first 3 months after fracture for both males (10.5) and females (6.5). After the first 3 months, the OR for mortality seemed to stabilize, but remained higher than the background population for the whole 5-year period.
Table 2.
Mortality OR estimates in relation to time since fracture in males and females compared to controls
| Time after hip fracture | OR (95% CI)
|
||
|---|---|---|---|
| Males | Females | All | |
| 0–3 months | 10.5 (5.7–19.5) | 6.5 (4.2–10.0) | 8.6 (6.0–12.2) |
| 3–6 months | 2.5 (1.2–5.2) | 2.3 (1.3–4.0) | 2.7 (1.7–4.2) |
| 6–12 months | 3.1 (1.7–5.7) | 1.8 (1.2–2.8) | 2.2 (1.5–3.2) |
| 1–2 years | 2.5 (1.6–3.7) | 2.0 (1.5–2.7) | 2.3 (1.8–2.9) |
| 2–3 years | 3.2 (2.1–5.0) | 2.4 (1.8–3.2) | 2.9 (2.3–3.7) |
| 3–4 years | 2.3 (1.3–3.8) | 2.5 (1.8–3.5) | 2.6 (2.0–3.4) |
| 4–5 years | 2.4 (1.2–4.8) | 2.1 (1.5–2.9) | 2.3 (1.7–3.1) |
Abbreviations: CI, confidence interval; OR, odds ratio.
Rural/urban areas
No statistical significant differences in mortality rates were seen using the log-rank statistical analysis between rural and urban areas (63.5% versus [vs] 57.0%, P = 0.07), neither for males (74.5% vs 67.4%, P = 0.13) nor for females (59.1% vs 52.9%, P = 0.20).
Associations with mortality 1 and 5 years after fracture
In the performed multivariate analysis, the mortality risk at the end of the first year was significantly associated with male sex (OR 1.7 [1.3–2.1], P < 0.005), older age 80+ years (OR 3.3 [2.4–4.3], P < 0.005), and the event of hip fracture (OR 4.7 [3.7–6.0], P < 0.005). At the end of the fifth year, the mortality risk was significantly associated with male sex (OR 2.2 [1.6–3.1], P < 0.005), older age 80+ years (OR 3.4 [2.5–4.5], P < 0.005), and the event of hip fracture (OR 4.0 [3.4–4.8], P < 0.005). No significant differences in mortality risk between rural and urban areas or between hospitals were observed, neither 1 nor 5 years after the event of hip fracture. The Nagelkerke R2 for the 1-year multivariate analysis was 0.15 and 0.22 for the 5-year multivariate analysis.
Discussion
To our knowledge, this study is the first to display the longstanding burden of mortality (5 years) of fragility hip fracture in the past decade. In our population-based hip fracture study, patients suffered an exceptionally high mortality in the first 3 months after the event compared to the control group. During follow-up, the mortality rates dropped, but continued to be higher than the control group for both sexes (Tables 1 and 2). Our observation is in agreement with previous studies2,4,16–21 and a recent meta-analysis,1 and highlights the fact that hip fracture in the past decade remains a serious threat to life expectancy in the middle-aged and elderly population.
Compared to the general population, the relative mortality risk was higher in the age group 50–80 years than in those aged 80 years and older after 1 year, both for males and for females (Table 1). This has also been reported by others.4,8 However, a higher mortality risk after the first year was associated with the older age group (80+ years) in the multivariate analysis, reflecting the frailty of the older population.22,23
The excess mortality during the first 3 months after fracture is most likely explained by a higher rate of preexisting comorbidities in a subgroup of fragile patients. However, data also suggest that the hip fracture event itself and the subsequent treatment (eg, fracture repair) are causes of mortality.21 The use of antibiotics and medications that affect the digestive, cardiovascular, and nervous systems in female hip fracture patients, and the use of medications affecting the digestive and nervous systems in male hip fracture patients, have been reported to be associated with lower survival rates.17 Osteoporosis itself, which is common in the age group above 50 years old,24 appears also to be an independent risk factor of mortality.25,26 In our study, we did not distinguish between femoral neck and intertrochanteric fractures. It is noteworthy that intertrochanteric fractures have been reported to have a worse prognosis concerning mortality compared to femoral neck fractures, with regard to long-term prognosis.27
For the first year of follow-up, the mortality rates as displayed in Table 1 were significantly higher in males than in females. A higher mortality rate in males than in females in the first year after hip fracture has also been reported in other studies.1,4,28,29 The poor prognosis for males in the first year after fracture is also reflected in the multivariate analysis. In this analysis, male sex was found to be an independent risk factor for higher mortality in the first year after hip fracture.17,19,27 The incidence rates of fragility hip fracture in Norway10 and USA9 have been reported to be in decline; however, mortality rates remain high, as shown in our study. We have, in a previous study,14 shown that incidence rates of fragility hip fracture are comparable both for males and females in southern and central Norway. A study from central Norway conducted between 1986 and 1995 revealed increased mortality rates in fragility hip fracture patients during the first year after fracture for all age groups;4 however, after 5 years, the mortality rates were at the same level as in the background population. A recently published study from central Norway regarding female patients prospectively recruited from 1995–1997 and followed for up to five years showed comparable results to our study. Hence, the OR for mortality for female patients 3 months after fracture is 6.5 (present study 6.5) and, from 3–6 months after fracture, 2.6 (present study 2.3).30
Taking into account the above data, it seems that the mortality rate of hip fracture is not decreasing, but remains high. However, during the past few decades, some evidence was found of a reduction in hip fracture mortality. In a study examining the US Medicare population with hip fracture aged 65 years and older, a decline in mortality rates was observed between the periods 1986–1988 and 2003–2005.9 Our findings demonstrate the need for awareness of the continuing high mortality of fragility hip fracture in middle-aged and elderly populations.
In our study, there were no differences in either the cumulative survival rates between urban and rural areas or in the mortality risk in the performed multivariate analysis. This is in agreement with a recently published study from the USA.31 This demonstrates the fact that mortality rates after fragility hip fracture are universal and not associated to the area of residence.
Strengths and limitations
The strengths of our study include the investigation of a stable population, which enabled identification of all individuals with hip fractures and deaths over the 2-year period in a well-defined geographic region. Further, for each fracture patient we aimed to recruit three controls randomly selected from the population matched for age, sex, and living area. However, our findings should be interpreted within the context of a number of limitations. The population studied was mainly white; hence, these results should not be generalized to other ethnic populations. A higher number of examined patients with hip fractures would also have given us the opportunity to estimate mortality in more detail for specific age groups, especially among those aged 80 years and younger. Information on comorbidities and other risk factors associated with mortality, as well as causes of death, were not available in this cohort of patients or controls. Thus, our study does not identify if hip fracture is, in itself, a risk factor independent of other risk factors or a marker for excess death in this patient group. We acknowledge the above as an important limitation of our study. Furthermore, the study sample, especially of males, is limited, thus presenting a major weakness of our study.
Conclusion
Our study confirms that hip fracture patients have an excess mortality, especially in the first 3 months after fracture, compared to the general population, which remains higher than the background population during the entire 5 years after fracture. In males, the mortality rates were higher than in females during the first year. The excess mortality in hip fracture patients documented in the past decade should encourage health care professionals, bureaucrats, and politicians to increase disease awareness and increase efforts to reduce the burden and consequences of fragility hip fracture.
Figure 2.
Kaplan–Meier survival analyses in males and females with a fragility hip fracture in 2004–2005 in southern Norway.
Notes: (A) Age group 50–80 years; (B) age group 80+ years.
Acknowledgments
We gratefully appreciate the expert technical assistance and help with data collection from the osteoporosis nurses Lillann Krüger Hæstad, Hanne Vestaby, Tove Kjøstvedt, and Åse Birkedal, as well as statistical support from Are Hugo Pripp. This work was supported and funded by The Competence Development Fund of Southern Norway and the Hospital of Southern Norway Trust.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Haentjens P, Magaziner J, Colón-Emeric CS, et al. Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med. 2010;152(6):380–390. doi: 10.1059/0003-4819-152-6-201003160-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abrahamsen B, van Staa T, Ariely R, Olson M, Cooper C. Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int. 2009;20(10):1633–1650. doi: 10.1007/s00198-009-0920-3. [DOI] [PubMed] [Google Scholar]
- 3.Magaziner J, Lydick E, Hawkes W, et al. Excess mortality attributable to hip fracture in white women aged 70 years and older. Am J Public Health. 1997;87(10):1630–1636. doi: 10.2105/ajph.87.10.1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Forsen L, Sogaard AJ, Meyer HE, Edna T, Kopjar B. Survival after hip fracture: short- and long-term excess mortality according to age and gender. Osteoporos Int. 1999;10(1):73–78. doi: 10.1007/s001980050197. [DOI] [PubMed] [Google Scholar]
- 5.Empana JP, Dargent-Molina P, Bréart G, EPIDOS Group Effect of hip fracture on mortality in elderly women: the EPIDOS prospective study. J Am Geriatr Soc. 2004;52(5):685–690. doi: 10.1111/j.1532-5415.2004.52203.x. [DOI] [PubMed] [Google Scholar]
- 6.Clayer MT, Bauze RJ. Morbidity and mortality following fractures of the femoral neck and trochanteric region: analysis of risk factors. J Trauma. 1989;29(12):1673–1678. doi: 10.1097/00005373-198912000-00016. [DOI] [PubMed] [Google Scholar]
- 7.Tosteson AN, Gottlieb DJ, Radley DC, Fisher ES, Melton LJ., 3rd Excess mortality following hip fracture: the role of underlying health status. Osteoporos Int. 2007;18(11):1463–1472. doi: 10.1007/s00198-007-0429-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.LeBlanc ES, Hillier TA, Pedula KL, et al. Hip fracture and increased short-term but not long-term mortality in healthy older women. Arch Intern Med. 2011;171(20):1831–1837. doi: 10.1001/archinternmed.2011.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302(14):1573–1579. doi: 10.1001/jama.2009.1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stoen RO, Nordsletten L, Meyer HE, Frihagen JF, Falch JA, Lofthus CM. Hip fracture incidence is decreasing in the high incidence area of Oslo, Norway. Osteoporos Int. 2012;23(10):2527–2534. doi: 10.1007/s00198-011-1888-3. [DOI] [PubMed] [Google Scholar]
- 11.Lyles KW, Colón-Emeric CS, Magaziner JS, et al. HORIZON Recurrent Fracture Trial Zoledronic acid in reducing clinical fracture and mortality after hip fracture. N Engl J Med. 2007;357:nihpa40967. doi: 10.1056/NEJMoa074941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beaupre LA, Morrish DW, Hanley DA, et al. Oral bisphosphonates are associated with reduced mortality after hip fracture. Osteoporos Int. 2011;22(3):983–991. doi: 10.1007/s00198-010-1411-2. [DOI] [PubMed] [Google Scholar]
- 13.Sambrook PN, Cameron ID, Chen JS, et al. Oral bisphosphonates are associated with reduced mortality in frail older people: a prospective five-year study. Osteoporos Int. 2011;22(9):2551–2556. doi: 10.1007/s00198-010-1444-6. [DOI] [PubMed] [Google Scholar]
- 14.Diamantopoulos AP, Rohde G, Johnsrud I, et al. Incidence rates of fragility hip fracture in middle-aged and elderly men and women in southern Norway. Age Ageing. 2012;41(1):86–92. doi: 10.1093/ageing/afr114. [DOI] [PubMed] [Google Scholar]
- 15.International Statistical Classification of Diseases and Related Health Problems 10th Revision [webpage on the Internet] Geneva: World Health Organization; 2010Available from: http://apps.who.int/classifications/icd10/browse/2010/enAccessed Apr 2013 [Google Scholar]
- 16.Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA. 2009;301(5):513–521. doi: 10.1001/jama.2009.50. [DOI] [PubMed] [Google Scholar]
- 17.Kannegaard PN, van der Mark S, Eiken P, Abrahamsen B. Excess mortality in men compared with women following a hip fracture. National analysis of comedications, comorbidity and survival. Age Ageing. 2010;39(2):203–209. doi: 10.1093/ageing/afp221. [DOI] [PubMed] [Google Scholar]
- 18.Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA. Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet. 1999;353(9156):878–882. doi: 10.1016/S0140-6736(98)09075-8. [DOI] [PubMed] [Google Scholar]
- 19.Panula J, Pihlajamäki H, Sävelä M, et al. Cervical hip fracture in a Finnish population: incidence and mortality. Scand J Surg. 2009;98(3):180–188. doi: 10.1177/145749690909800310. [DOI] [PubMed] [Google Scholar]
- 20.Tsuboi M, Hasegawa Y, Suzuki S, Wingstrand H, Thorngren KG. Mortality and mobility after hip fracture in Japan: a ten-year follow-up. J Bone Joint Surg Br. 2007;89(4):461–466. doi: 10.1302/0301-620X.89B4.18552. [DOI] [PubMed] [Google Scholar]
- 21.Vestergaard P, Rejnmark L, Mosekilde L. Increased mortality in patients with a hip fracture-effect of pre-morbid conditions and post-fracture complications. Osteoporos Int. 2007;18(12):1583–1593. doi: 10.1007/s00198-007-0403-3. [DOI] [PubMed] [Google Scholar]
- 22.Pioli G, Barone A, Giusti A, et al. Predictors of mortality after hip fracture: results from 1-year follow-up. Aging Clin Exp Res. 2006;18(5):381–387. doi: 10.1007/BF03324834. [DOI] [PubMed] [Google Scholar]
- 23.Jiang HX, Majumdar SR, Dick DA, et al. Development and initial validation of a risk score for predicting in-hospital and 1-year mortality in patients with hip fractures. J Bone Miner Res. 2005;20(3):494–500. doi: 10.1359/JBMR.041133. [DOI] [PubMed] [Google Scholar]
- 24.McClung MR, Geusens P, Miller PD, et al. Hip Intervention Program Study Group Effect of risedronate on the risk of hip fracture in elderly women. Hip Intervention Program Study Group. N Engl J Med. 2001;344(5):333–340. doi: 10.1056/NEJM200102013440503. [DOI] [PubMed] [Google Scholar]
- 25.Browner WS, Seeley DG, Vogt TM, Cummings SR. Non-trauma mortality in elderly women with low bone mineral density. Study of Osteoporotic Fractures Research Group. Lancet. 1991;338(8763):355–358. doi: 10.1016/0140-6736(91)90489-c. [DOI] [PubMed] [Google Scholar]
- 26.Johansson C, Black D, Johnell O, Odén A, Mellström D. Bone mineral density is a predictor of survival. Calcif Tissue Int. 1998;63(3):190–196. doi: 10.1007/s002239900513. [DOI] [PubMed] [Google Scholar]
- 27.Karagiannis A, Papakitsou E, Dretakis K, et al. Mortality rates of patients with a hip fracture in a southwestern district of Greece: ten-year follow-up with reference to the type of fracture. Calcif Tissue Int. 2006;78(2):72–77. doi: 10.1007/s00223-005-0169-6. [DOI] [PubMed] [Google Scholar]
- 28.Pande I, Scott DL, O’Neill TW, Pritchard C, Woolf AD, Davis MJ. Quality of life, morbidity, and mortality after low trauma hip fracture in men. Ann Rheum Dis. 2006;65(1):87–92. doi: 10.1136/ard.2004.034611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kang HY, Yang KH, Kim YN, et al. Incidence and mortality of hip fracture among the elderly population in South Korea: a population-based study using the national health insurance claims data. BMC Public Health. 2010;10:230. doi: 10.1186/1471-2458-10-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Grønskag AB, Romundstad P, Forsmo S, Langhammer A, Schei B. Excess mortality after hip fracture among elderly women in Norway. The HUNT study. Osteoporos Int. 2012;23(6):1807–1811. doi: 10.1007/s00198-011-1811-y. [DOI] [PubMed] [Google Scholar]
- 31.Miller BJ, Cai X, Cram P. Mortality rates are similar after hip fractures for rural and urban patients. Clin Orthop Relat Res. 2012;470(6):1763–1770. doi: 10.1007/s11999-011-2140-3. [DOI] [PMC free article] [PubMed] [Google Scholar]