Abstract
Adults with better jobs enjoy better health: job title was, in fact, the social gradient metric first used to study the relationship between social class and chronic disease etiology, a core finding now replicated in most developed countries. What has been less well proved is whether this correlation is causal, and if so, through what mechanisms. During the past decade, much research has been directed at these issues.Best evidence in2009 suggests that occupation does affect health. Most recent research on the relationship has been directed at disentangling the pathways through which lower-status work leads to adverse health outcomes. This review focuses on six areas of recent progress: (1) the role of status in a hierarchical occupational system; (2) the roles of psychosocial job stressors; (3) effects of workplace physical and chemical hazard exposures; (4) evidence that work organization matters as a contextual factor; (5) implications for the gradient of new forms of nonstandard or “precarious” employment such as contract and shift work; and (6) emerging evidence that women may be impacted differently by adverse working conditions, and possibly more strongly, than men.
Keywords: occupational health, psycho-social stressors, work organization, women in the workplace, nonstandard work
Introduction
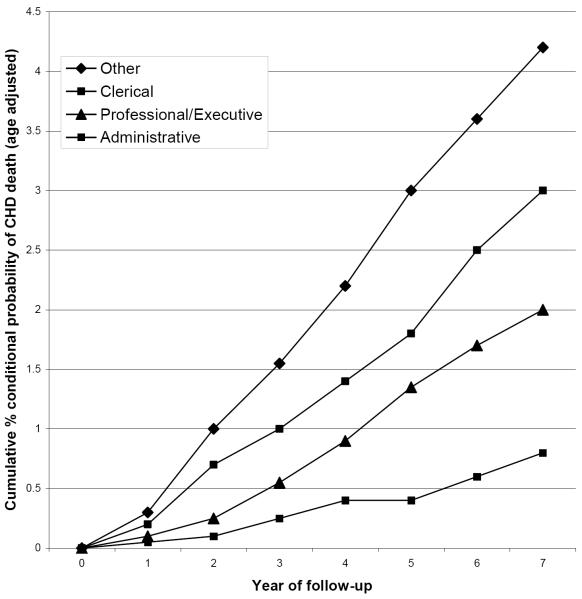
It has long been recognized adults with better jobs enjoy better health than do their counterparts. Indeed job, rather than other measures of wealth and education, was the social gradient metric first used to understand the relationship between social class in the UK and chronic disease etiology, in the landmark Whitehall studies of the 1970's (Figure 1) (Reid et al. 1974).
Figure 1.
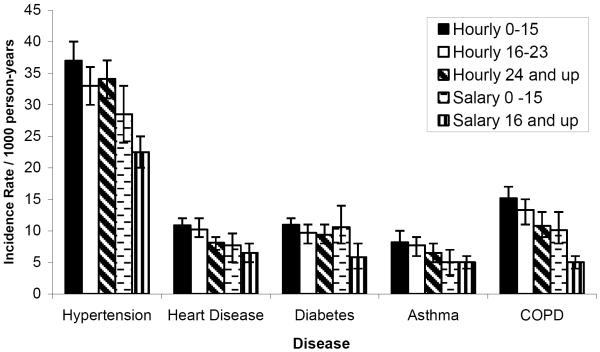
The core finding, an inverse association between job status and multiple measures of chronic disease incidence, prevalence and mortality, has been replicated in most developed countries (Mackenbach et al. 2008). For example, Figure 2 depicts incidence rates for six chronic illnesses in a large, diverse, and geographically dispersed employee population of a single U.S. corporation, for 1996–2003 (Cullen et al. 2006).
Figure 2.
These relationships hold even after adjustment for socioeconomic status (SES) and related factors (e.g., education, income), although these are highly correlated in most populations in developed countries (Mackenbach et al. 2008).
What has been less clear is whether this correlation is, causal, and if so, through what mechanisms. Much of the research undertaken during the past decade has been directed at these issues, although progress has been hampered for various reasons, especially in the important area of cardiovascular disease where interest is highest (Cullen (in press); MacDonald et al. (in press)). We will review the general evidence for causality here, and discuss possible pathways in the several sections that follow.
Two non-causal links between occupational status and health have been hypothesized. First, reverse causation would suggest that poorer health status, or adverse health risk profiles, lead to lower job status, through a compromised ability to work as effectively or consistently as healthier workers (Bartley 1988). There is some longitudinal evidence that poor childhood health leads to lower professional achievement in adulthood (Mensah and Hobcraft 2008), and some evidence of pre-existing health gradients by profession among young adults (Rabinowitz et al. 2006). Nevertheless, there is little evidence of measurable health differences among young adults strong enough to explain job attainment differences after adjustment for education. In fact, most lower–grade jobs in our society (e.g., mining, construction, farming manufacturing) require tremendous physical capabilities, especially in comparison to high-grade jobs, and employees in physically demanding jobs are typically screened for fitness at hire. These observations suggest that the reverse may actually be true — that significant physical incapacity can serve to exclude individuals from physical employment, and is the basis for well-described healthy worker selection effects among employees performing physical labor (Checkoway et al. 2004). Studies have attempted to apportion the job status-health association into causal and selective components using longitudinal data (Chandola et al. 2003; Claussen et al. 2005; Heponiemi et al. 2007), with limited success. Causal and selective components of job status are difficult to disentangle, in part, due to persistent confounding by social class and its associated risk factors. Blue-collar workers in competitive economies tend to be lower socioeconomic status (SES), with lesser education and fewer job options. In the U.S., blue-collar jobs are disproportionately performed by males and minorities, and may include a higher prevalence of smokers (Kivimaki et al. 2006).
Second, and more challenging to a causal link between occupational status and health, is persistent confounding by social class and omitted (unmeasured) variables; workers from more privileged backgrounds, already on a better health trajectory, are more likely to seek and achieve better jobs. As such, occupation may serve only as a surrogate measure for such selection effects. Since experimental data will never be available (comparable to, say, lottery winners for the study of income effects on health, or educational lotteries such as Moving to Opportunity (U.S. Department of Housing and Urban Development 2006), evidence for and against this argument is strictly observational. Studies of British birth cohorts have demonstrated that pre-hire factors explain some of the subsequent pattern of adult health (Mensah and Hobcraft 2008), but may act additively with subsequent occupation and income (Lidfeldt et al. 2007). Studies of the U.S. Alcoa aluminum manufacturing population, stratified by propensity scores of risk factors at hire, demonstrate added effects associated with duration of lower-status, but not higher status, work among men and women, suggesting that endogenous differences at onset don't explain the outcome entirely, but may indicate susceptibility to subsequent exposures (Clougherty et al. 2008; Clougherty et al. (under review)).
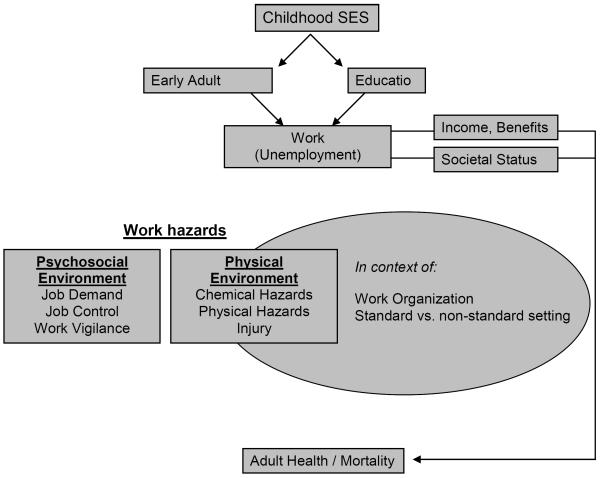
Thus, while the causal role of job in determining health outcomes remains far from fully established, and in particular its interplay with SES indicators such as education and wealth remains underexplored, the best evidence in 2009 suggests that occupation matters significantly for health. As such, much recent research on work and health has been directed at disentangling the multiple pathways through which lower status work may lead to adverse health outcomes. Figure A, below, depicts the conceptual framework from which we have examined the evidence linking work and adult health. Childhood SES may contribute to adult work roles via educational and/or direct (early adult) health pathways, as well as some “opportunity” pathways, less easily measured. In adulthood, additional benefits or hazards to health may be mediated in turn through multiple pathways including social ones—societal status, income, benefits, etc--and pathways linked more closely to the context and content of work itself. To capture job content, we include separate physical aspects (e.g., work load, chemical and physical environmental factors) from psycho-social aspects, such as job strain or a need for constant vigilance. The social context in which these exposures occur may modify their impact, especially the psycho-social stressors. Not depicted in the schema, but noteworthy, is the likelihood that each of the pathways, from childhood SES down, may operate differently in women than in men.
Figure A.
We devote the rest of this review to these mediating pathways, with a focus on five areas of recent progress. First, we discuss the role of status in a hierarchical system. Related to that is the role of psychosocial job stressors, and the role of physical and chemical hazard exposures in the workplace. Fourth, we review recent evidence that work organization as a contextual factor (as opposed to job-specific factors within a workplace) may significantly influence employee health. One specific aspect of that context relates to the changing nature of the work-employee contract, as non-standard work arrangements become increasingly common, raising new questions about the health impact of job insecurity, contract work, self-employment, and, increasingly, underemployment and unemployment, which many working adults will experience at some time in their working life, particularly if current patterns persist. Finally, as women increasingly perform work roles once almost exclusively male, new questions have arisen about persistent sex-stratification in the workforce, and possible modification in the health effects of work conditions on health by sex and gender.
(1) The Role of Status: Does position in an occupational hierarchy in and of itself confer health risks or benefits?
Occupational status, frequently used as one of the core components of the SES construct, includes a highly complex bundle of factors whose impact on health may be mediated through many alternate pathways. At the most obvious level, occupational status confers societal prestige (or the lack of it), unrelated to its actual day to day meaning at work. Professionals, for example, are more highly esteemed in our culture than laborers; executives than clericals. There is anthropologic and biologic evidence to suggest humans, like other primates, are naturally hierarchical, and that relative position, in and of itself, confers health benefit (or harm). Within the work setting, job status often translates to more tangible benefits or hazards as well, including income and benefit levels, as well as degree of control over work, support and, typically, likelihood of exposure to noxious physical environments. Teasing apart these components has been and remains a scientific challenge, especially given the implausibility of experimental or even quasi-experimental data sources: job status is inherently a non-random assignment.
Most research on job status has relied either on relatively coarse job classifications, or focused almost exclusively on administrative (i.e., “white-collar”) populations (Marmot and Smith 1991; Marmot et al. 1997; Calhoun et al. 1998; Barbini et al. 2005; Moller et al. 2005; Aboa-Eboule et al. 2007; Kivimaki et al. 2007). Across more diverse cohorts, job grade may reflect a host of social, economic and psychosocial risk factors varying with social class (Kaplan and Keil 1993; Warren et al. 2004; Erikson 2006), and the effect of job grade itself may vary within broader occupational classes and settings (Sparacino et al. 1982). Among white-collar workers, job grade may be mediated through status and decision-making authority; among blue-collar workers, job grade may capture differences in chemical exposures, physical demands, or work pace. Some factors, such as income and job security, can vary within both groups.
The use of broad occupational classifications
Occupational classifications used in many epidemiological studies (i.e. manual/ non-manual distinctions (Macleod et al. 2005), professional grade (Marmot and Smith 1991; Schaufelberger and Rosengren 2007), and census job classifications (Stevens and Cho 1985) have proven too coarse to capture fine-scale status differences most relevant to employee experiences within occupational settings. More recent work has attempted to understand health effects of status differentials within working classes, and to examine job grade effects among manufacturing and industrial workers, where job grade itself is confounded by (and may also, to some extent, consist of) a range of physical, chemical and psychosocial stressors, including noise, heat, chemical exposures, a rapid pace of work, job strain, and socioeconomic risks factors outside the occupational setting.
The complexity of “job grade” in the blue-collar setting
The association between job status and health has been difficult to interpret, as job status can represent many physical and psychosocial aspects of work, as well as socioeconomic risk factors and health behaviors outside of work (Kaplan and Keil 1993; Warren et al. 2004; Erikson 2006). With improved methods for measuring work-related stressors (e.g., noise, ergonomic demands), we can now achieve a more refined understanding of job grade effects independent of the physical demands and exposures of work, though the task remains challenging as such exposures are persistently correlated. Recent studies have attempted to disaggregate job grade into its physical and psychosocial components (MacDonald et al. 2001), including income (Lecluyse 2007), effort-reward imbalance (Merritt et al. 2004), perceived fairness (DeVogli et al. 2007), knowledge of job-related risks and behaviors (Niknian et al. 1991; Nourjah et al. 1994) and job strain (decision latitude vs. demands) (Blumenthal et al. 1995; Steptoe and Willemsen 2004; Kivimaki et al. 2006). Due to this complex exposure mix, most studies have focused on few industries or companies, in which working conditions can be measured and isolated (Kasl 1981; Matthews et al. 1987).
In our dataset of 15,000 aluminum manufacturing employees across eight U.S. states, we compared incident hypertension among full-time hourly (mainly production, or “blue-collar”) and salaried (production supervisors and administrative, largely “white-collar”) personnel in a large aluminum manufacturing company. We used propensity stratification to account for strong SES bias in job placement, and to distinguish selection from exposure effects. We found elevated hypertension risks among blue-collar employees, relative to white-collar, which persisted after adjustment for SES and age. The blue-collar effect increased with more stringent case criteria, suggesting greater illness severity or chronicity among blue-collar workers. Higher job grades were generally protective, particularly among hourly employees and men.
Tenure (years on the job) increased risks among blue-collar workers, and may indicate cumulative exposure to physical, chemical, or psychosocial exposures, including heat, noise, and job strain. Differences in chemical or physical exposures (e.g. closer proximity to smelting fumes among laborers than supervisors) may also account, in part, for some job grade effects within blue-collar groups. In addition, due to diminishing marginal returns, lower-grade employees may benefit more per increment, possibly explaining some job grade effects in women, who make up a larger portion of low-grade workers (Quinn et al. 2007).
Job status in social epidemiology
New phases in the study of job status and health, and particularly new interest in refined job grade, precarious employment, and multilevel effects, are emblematic of the principles that have shaped social epidemiology over the past 10 to 20 years. In particular, we are now developing a richer understanding of health effects across the full gradient of occupational class (rather than focusing on the extremes), a richer appreciation for the role of precarious employment (e.g., unstable resource access and social status), and developing methods to examine whether and how job-level effects on health vary by workplace context, using techniques from multilevel modeling. Perhaps most importantly, we are now considering how these combined stressors may affect individual health over the long term, and developing techniques and models for examining these related (and often correlated) stressors in tandem.
For example, in our cohort of blue-collar aluminum manufacturing personnel we found that low job grade increases risk of hypertension across the spectrum of grades, with some evidence of diminishing health returns to job grade at higher levels (Clougherty et al. 2008). Similarly, scholarship on SES and health in recent decades has demonstrated strong effects of SES on health across the SES gradient, and diminishing marginal health returns are known for income (Kawachi 2000; Mackenbach et al. 2004) and material well-being. Likewise, the growing appreciation for the complexity of job grade (Evans et al. 1994), and its varied risk factors, within the workplace setting and beyond, mirrors the growing multidisciplinary approach of epidemiology. For example, the relationship between SES and childhood asthma is increasingly recognized to be vastly complex, mediated by a host of multiplicative chronic factors, including environmental exposures, housing quality, healthcare access, and social stressors (Clougherty et al. 2007; Chen et al. 2008). For this reason, methods being developed in other areas of epidemiology may be invaluable towards disentangling the complex job grade-health association.
In summary, new evidence suggests caution in generalizing results from white-collar cohorts to blue-collar workers, and growing diversity among the modern workforce – across age, sex, and race/ ethnicity – may also mean greater opportunities to observe modification in the job status-health association.
(2) Psychosocial Job Stressors (Demand, control, reward): How do we understand and parameterize these constructs, and what do they contribute to the gradient?
Working life entails many types of demands -- some physical, some mental -- and many variants of “control”, or means of meeting those demands. As such, one of the greatest challenges in job strain research lies in accurately characterizing the nature of `job strain,' or work-related stress, and distinguishing its effects from those of concomitant physical, chemical, and financial stressors.
There is broad evidence linking psychosocial work characteristics to cardiovascular risk (Kuper and Marmot 2003; Barbini et al. 2005; Chandola et al. 2006). Increased risks of hypertension and elevated ambulatory blood pressure have been associated with chronic job strain (Landsbergis et al. 2003; Markovitz et al. 2004), low job control (Steptoe and Willemsen 2004), and stressful work conditions including low promotion potential, little participation in decision-making, communication difficulties, unsupportive co-workers and foremen, and overall job dissatisfaction (Matthews et al. 1987). Several biological and psychological pathways have been proposed to link psychosocial work conditions to hypertension (Chandola et al. 2008), including chronic stress, irritation (Folkow 1981), suppression of anger and problems (Cottington et al. 1986), and selection by personality type (Esler et al. 1977). More generally, chronic stress can produce cumulative wear and tear (allostatic load), potentially suppressing immune function over time, increasing general susceptibility, reducing systemic regulation, and increasing broad disease risk (McEwen and Seeman 1999).
In previous decades, most of what was known about `job strain' stemmed from the development and application of the demand-control model (Karasek et al. 1981; Karasek et al. 1998; Karasek and Theorell 2000), which defined job strain as the bi-dimensional interaction between (1) job demands (usually psychological, rather than physical) and (2) decision latitude allowing the individual to meet those demands, often referred to as control. As was the case for job grade, most early work using the Karasek model included only white-collar populations, and generally found that greater control conferred better health outcomes. Some more recent cross-sectional studies have demonstrated associations between job strain and blood pressure across men in various occupations, an effect which may be stronger among lower-SES persons (Landsbergis et al. 2003) and during working hours (Landsbergis et al. 2008). Using the demand-control model for their administrative cohort, Whitehall investigators concluded that much of the differential in IHD morbidity and mortality observed between job grades could be explained by control (Kuper and Marmot 2003).
Alternatively, the effort-reward imbalance model quantifies the lack of correspondence between job-related efforts (both physical and, more importantly, psychological) and rewards received for those efforts (including monetary remuneration, prestige, and career opportunities) (Siegrist 1996). A number of investigations, including cross-sectional and longitudinal results, though largely among men, support a link between effort-reward imbalance and cardiovascular outcomes (Belkic et al. 2000). There is additional evidence that the effort-reward imbalance model may be most informative in combination with results of the job strain model (Peter et al. 2002), as together the models capture “a broader range of stressful experience at work (Peter et al. 2002).” The models overlap significantly along the control dimension; according to some evidence, persons with high job control report more effort-reward imbalance (Bosma et al. 1998). It is important to note, however, that they emphasize very different types of control; job strain emphasizes control over task performance, while effort-reward imbalance emphasizes control over “macro-level” issues such as salary and career advancement (Belkic et al. 2004).
The nature of job stressors, and, accordingly the critical aspects of control, may differ dramatically by setting. In the manufacturing setting, where job strain has been less explored, greater decision latitude for a worker in a rapid-paced manual process can be highly stressful. Furthermore, the forms of control valued by the individual workers performing physical (rather than sedentary) labor may be very different; some workers may value having input on how their work is designed or performed, while others (particularly those performing physical work) may more greatly value the option to take a work break when needed. Perhaps not surprisingly, then, recent studies of the job strain model in the aluminum manufacturing sector have produced results that different dramatically from the Whitehall results; while both demand and control measures may predict injury risk (Kim et al. 2009; Cantley et al. (Submitted)), only demand appears to be associated with incident depression (Iennaco et al. (Submitted)), and neither demand nor control produces a continuous predictive relationship with cardiovascular outcomes (unpublished data).
Part of the discrepancy between these results may be derived from differences in the job strain measurement. Most studies over the past three decades have relied on subjective report of the major elements of strain (Karasek et al. 1981; Reed et al. 1989; Kuper and Marmot 2003). Due to concerns about conflation of predictors with outcomes, especially with mental health or other outcomes also measured by self-report (Landsbergis and Theorell 2000), many have proposed and utilized measures of strain associated with particular jobs or tasks, or external measures, rather than individual reports (Greiner and Krause 2000). These latter job-level strain assessments are often performed by external, presumably more objective, raters, though Kasl and others have argued that this approach introduces other measurement issues and biases (Kasl 1981). Importantly, in the few cases in which subjective and external ratings have both been obtained, as in Whitehall, the two measures correlate poorly (r < 0.2) (Rehkopf et al. (under review)). Recent analyses of absenteeism suggests that subjective measures add little to external ratings, and the latter has the advantage of representing “environmental” factors more amenable to intervention or modification (Rehkopf et al. (under review)). For this reason, external ratings have been relied upon in the previously cited Alcoa studies of job strain.
Finally, specific stressful characteristics of work have merited more involved study. Night shift work and threat avoidance vigilance have been associated with cardiovascular outcomes including hypertension and myocardial infarction (Winkleby et al. 1988; Belkic et al. 1998; Boggild and Knutsson 1999). Some physical stressors associated with job tasks (e.g., exposures to noise, vibration, heavy lifting, or chemicals such as carbon monoxide, carbon disulfide, and nitroglycerin (Fine 2000)) have shown similar results, though, importantly, distributions of these exposures are tightly correlated, such that their health effects can be difficult to disentangle. One such chronic stress conditions, threat avoidance vigilance, may help to explain elevated risks of hypertension co-occurring with injury risk in some manufacturing settings.
(3) Physical and Chemical Hazards: What do they contribute to the occupational gradient?
The study of occupational hazards and health dates back to the early 18th century, and remains a substantive discipline of research and practice in both clinical and public health (Ramazzini 1700; Rosenstock et al. 2005). In addition to widespread risks of work-related physical injury, hundreds of acute and chronic work-related disorders have been characterized, and risk profiles associated with exposure to thousands of common toxic materials have been established, many supported through toxicologic experiments in laboratory animals. Despite this body of knowledge, and the broad investment in the US and other developed countries to control and manage occupational risks, many social epidemiologists have argued that physical hazards contribute minimally to SES-health gradients at the societal level (are there any citations for this observation?). This perspective stems from the exemplary demonstration of the health and mortality gradients among the administrative white-collar Whitehall I and II populations, wherein to physical exposures such as heat, noise, and chemical hazards were negligible, and evidence that social gradients in health begin early in life, precluding any effect of work beyond that of parental occupation (again, status) or residual exposures to chemical exposures carried home on work clothes.
This evidence indicates that at-work exposures to physical agents are not a necessary component to social health gradients — indeed, SES-health gradients clearly can exist in the absence of physical hazards -- though this is not proof that work-related physical hazards are non-contributory. Moreover, it is widely believed that workers, in an earlier period of industrial development endured tremendous physical hazards, and that the modern post-development economy has all but eliminated “dangerous” sectors and nearly eliminated residual risks in the industrial sector through, modern regulations. In this section, we review the evidence suggesting that both presuppositions are false, while we acknowledge that robust quantitative estimates for the contribution of physical work hazards to the social gradient in health are yet unknown.
Exposures to physical environmental conditions at work, including trauma, chemicals, biologic agents and physical hazards (e.g., heat, noise, radiation), are still widely prevalent in the U.S. and other OECD countries, and thus may contribute substantively to the social gradient in health. Using the most recent U.S. data available, work in the formal manufacturing, construction, mining and agriculture sector continue to comprise roughly 25% percent of the total workforce, or 37.5 million men and women (Bureau of Labor Statistics 2006). Another 15% of jobs, mostly in health, transportation and food services, have substantial environmental exposures and among the highest injury rates of any sector. These BLS statistics do not include the far larger fraction of older adults moved from the shrinking sectors such as manufacturing into services or retirement, nor those working full or part time in the informal sector including very dangerous trades such as sex work, drug trade, personal, and domestic services, nor the very dangerous exposures incurred during military service. In sum, it is reasonable to estimate that 60% or more living U.S. adults are substantially exposed to hazardous physical, chemical or biologic hazards for some period of time during their working careers.
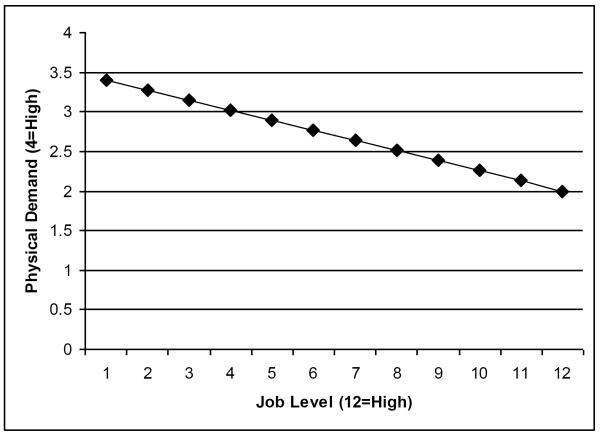
Is the distribution of hazardous exposures sufficiently parallel to the social gradient in health that a significant contribution is plausible? Or, are lower-SES workers more exposed to physical hazards than higher-SES workers, with such consistency as to explain a meaningful portion of the social gradient? Putting aside for the moment the varying efficacy of present-day controls and regulation of workplace physical exposures, this proposition of a social gradient in workplace exposures has been assumed so self-evident that empiric proof has not been broadly presented across industries, though indirect evidence and within-industry associations abound. Most jobs in the formal industrial sectors described above require a high school education or less, and many (with the possible exception of the relatively small trade-union middle class) are marginally compensated relative to higher status professions. Labor market theory would suggest that workers in hazardous industries might earn a hazard “premium,” or proportionately higher wages in exchange for accepting greater risks, but recent reevaluation suggests this may not generally be so (Leigh 1991). While such premiums have been identified within specific narrow social and geographic contexts (for example, underground miners in rural West Virginia earn more than workers in jobs supporting the mining industry) most evidence indicates that, overall, workers in larger workplaces are both better protected and better paid compared to those in smaller or more marginal workplaces (Haas and Buchan 1995; Suruda and Wallace 1996). Within workplaces, there is also evidence that higher-status workers enjoy better physical environmental conditions, as well as lower physical demands. For example, Figure 3 depicts the relationship between physical demand (1= sedentary, up to 5= extreme physical exertion) and job grade (here on a 12 point scale) within the hourly (blue-collar) workforce at a large aluminum smelting facility (unpublished data):
Figure 3.
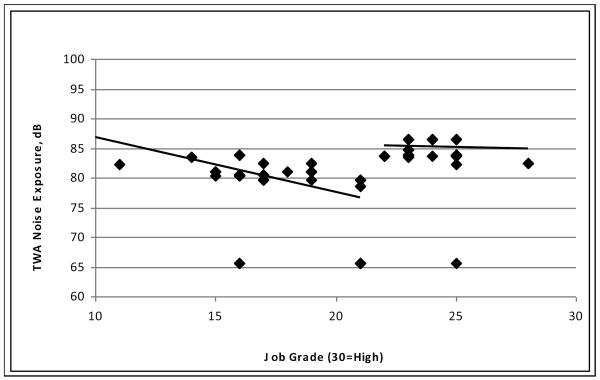
Similarly, in this dataset, dust exposures are also higher among lower-grade hourly employees. Noise exposures, however, distribute differently: higher-grade skilled tradesman (here, grades 22 and above on a 30-point scale) experience higher noise exposures, on average, than those in lower status jobs:
As noted, exposures to all of these agents are negligible among the better-educated salaried workforce, which comprises about 1/3 of all company employees.
By far the most salient hazard in the above workplaces is trauma and bodily injury. In 2007, almost 5,500 U.S. men and women died on the job. Another 122 per 10,000 workers (another 2 million) suffered injuries serious enough to require medical treatment and restricted or lost work time—heavily concentrated in the heaviest, lower SES jobs-- costing 1–2% of GDP annually (Institute of Medicine 2001). While these injuries cannot substantively account for health and mortality gradients, they do contribute significantly to differentials in individual's ability to work productively into late middle-age and beyond. Indeed, musculo-skeletal disorders far outweigh all other causes of social security and private disability claims except for mental impairments, constituting over 25% of the social security disability claims (Social Security Administration 2008). More importantly, and inadequately studied, is the potential of these physical injuries and disability to impair health and susceptibility, increasing mortality risk. One pathway, discussed already above but inadequately studied at work, is hyper-vigilance, which may be highly prevalent among those in dangerous jobs.
The contribution of workplace chemicals to chronic respiratory disease has been better examined, with studies following two key approaches. First, classical occupational epidemiology prospective cohort studies have followed cohorts exposed to various well-measured agents (e.g., coal dust, welding fumes) to estimate risks of “excess” chronic lung disease compared to less-exposed, but otherwise comparable, control populations. Extrapolation of risks to the larger population is then derived from the fraction of the population that is exposed and estimated exposure intensity. In this manner, risks associated with occupational exposures to hundreds of organic and inorganic chemicals have been established as major causes of asthma (Chan-Yeung and Malo 1999; Van Kampen et al. 2000). Likewise, longitudinal studies of lung function in workers exposed to various dusts and fumes have demonstrated excess reductions in airflow and risk of chronic obstructive pulmonary disease (COPD), outcomes normally associated with smoking (Seixas et al. 1993; Coggon and Taylor 1998; Nakadate et al. 1998). Second, the contribution of workplace airborne irritants and toxicants to chronic lung disease has been estimated by parsing risk factors observed in large heterogeneous populations to assess whether occupational exposures — generically defined from medical records, self-report, or questionnaires — can explain differences in lung function or disease rates (Kauffmann et al. 1982; Kryzyzanowski et al. 1986; Xu et al. 1992). Gratifyingly, this latter approach, which applies relatively weaker case-control methods in the occupational setting, has been corroborated by prospective results, yielding relatively consistent estimates of approximately 15% of adult asthma cases and 15–20% of the COPD burden (American Thoracic Society 2003). The contribution to lung fibrosis has historically been higher but is dropping with control of the most prevalent causal agents, asbestosis and silica dust.
The contribution of workplace chemicals to the total cancer burden has been estimated by similar study designs. Malignant mesothelioma, an otherwise uncommon cancer, is largely attributed to asbestos exposure among workers in western countries (Bianchi and Bianchi 2007). Lung and bladder cancers, much more common, are also closely associated with workplace chemicals, with upwards of 20% of cases attributable to established causal agents in the workplace, including asbestos, petroleum combustion products, and arsenic (Barone-Adesi et al. 2005). Some leukemias, liver and skin cancers (other than highly lethal melanoma) are less common, and occupational causes are well established (Rosenstock et al. 2005). For many other cancers and tumors, associations with workplace hazards are hypothesized but unestablished. Overall estimates, using forward and backward approaches—studying cancer outcomes in cohorts of workers exposed to varying doses, or using broad patterns in the larger population to estimate attribution-- range from 4 to 5% of the total cancer burden, with little change over the past three decades (Doll and Peto 1981; Rushton et al. 2008). The implication of these observations towards explaining the social gradient in health, however, is that most of the attributable cancer burden is borne by the most-exposed workers, typically in manufacturing, construction or mining—only 20–25% of all workers – with lower-grade workers experiencing longer and more intensive exposures.
Evidence of a causal association between workplace physical exposures and cardiovascular disease remains far less well understood, but, due to the high prevalence of cardiovascular illness in developed countries, may be extremely important, even if the attributable fraction of cases is relatively small (Cullen (in press); MacDonald et al. (in press)). Three nearly ubiquitous physical hazards in the industrial setting (noise, heat, and exertion) have each been linked to ischemic heart disease (IHD). For noise, the presumptive pathway is via elevated blood pressure, though evidence of a direct link remains limited (Kristal-Boneh et al. 1995) despite elegant physiologic models of adrenomedullary responses to noise in laboratory and animal experiments (Ortiz et al. 1974). Heat stress, a potent stimulus for increased cardiovascular demand, has been long recognized as a risk for myocardial infarction (MI) or sudden death in workers with existing heart disease (Redmond et al. 1979; Wild et al. 1995). For this reason, most workers with heart disease and those taking vasoactive drugs for hypertension are excluded from working in hot environments. Due to screening and self-selection away from such jobs, the impact of hot work on IHD morbidity and mortality has been difficult to assess. For high-exertion activity, the data are mixed; Paffenbarger famously showed that physical activity among longshoreman reduces IHD risk (Paffenbarger et al. 1970), but the role of selection and the `healthy worker effect' in these estimates remains problematic, and heavy physical exertion may, with or without other environmental risks, be harmful (Kales et al. 2007).
As globalization and other economic transformations increase the proportion of work performed at non-traditional hours, concern for the health consequences of work-shift have intensified, with cardiovascular diseases and its antecedents the area of greatest concern (Boggild and Knutsson 1999; Knuttson 2003). Methodological problems, most notably endogenous differences between those who do and do not end up working non-day shifts, have complicated study of this issue, but cohorts studies in Denmark (Boggild et al. 1999) and Finland (Tenkanen et al. 1997) have found excess CVD outcomes in men, while Kawachi and colleagues found a risk in female nurses proportional to the number of years the women worked alternative shifts (Kawachi et al. 1995). Others have failed to find such excesses, though there is also data linking increased BMI and insulin resistance to shift work (Knuttson 2003), rendering this concern highly plausible given present knowledge.
Perhaps more worrisome still, evidence from many environmental studies of outdoor air pollution consistently show that inhaled fine particulates (aerodynamic diameter less than 2.5 microns, or PM2.5) increases risk of respiratory and cardiovascular mortality, with moderately elevated relative risks on the order of 1.2, and attributed annual excess mortality of 60,000 U.S. deaths/ year (Miller and Chen 2007; Pope et al. 2009). The data supports the attribution of a significant fraction of cardiovascular deaths to ambient air pollution, and an extensive literature has emerged exploring possible mechanistic pathways, including inflammatory effects in the lung, affecting vascular endothelium via circulating cytokines (Brook et al. 2004). Some recent studies attempt to differential ambient PM2.5 into source-attributable components (Clougherty et al. (under review)), and some new evidence indicates that ischemia and ST segment depression may be more responsive to PM2.5 from traffic and PM with high carbon content (Lanki et al. 2006). As such, ambient air pollution may account for some portion of the SES gradient in health, and these data raise serious implications about the role of workplace particulates, which can be present in concentrations an order of magnitude or more above ambient levels. As such, occupational PM exposures should contribute to markedly increased IHD mortality among workers in heavy industry, transportation, construction, and related fields. Dusts in these industries, however, have long been considered a nuisance rather than a risk factor—and cardiovascular effects have been largely ignored among young, relatively health working populations —as such, evidence to inform this proposition remains limited, though several studies are progress. In summary, while physical hazards in the work environment may prove a major contributor to high rates of cardiovascular illness among lower social class workers, evidence at this time remains more limited than that for respiratory diseases and cancer.
(4) Healthy Work Organization: Is there a “neighborhood” effect in the workplace?
In recent years, social epidemiologists have reinvigorated investigation into the socioeconomic causes of poor health, and have demonstrated the necessity of disentangling proximal individual risk factors from more distal or `structural' risk factors. Occupational health researchers, in turn, have attempted to estimate the influence of the workplace environment and some of its structural characteristics – variously conceived of and named `workplace culture', `work organization', and `workplace social capital', for example. Several workplace characteristics have been extensively measured and studied, towards understanding how workplace context, as distinct from workforce composition, contributes to ill health. Results of research point to the importance of the work environment to workers' health, and saliently, to the need for appropriate methods for examining and quantifying these separate contributions.
`Safety culture', a commitment to safety that is expressed in appropriate policies and practices (Guldenmund 2000), has long been championed by human resources and safety professionals as integral to safe working environments. The construct of `safety culture', however, has not been easily or adequately measured. Nowhere perhaps has the culture of the work environment been more studied than in the pressure- and hazard- filled health care setting. The culture of the healthcare organization has shown to be relevant both for the health/safety of patients and that of its workers. Abundant patient safety research demonstrates that safety culture and organizational factors are interdependent; patients well-being depends upon the success of `system', more so than individual-oriented measures (Clark 2002). Analogously, research in the health care setting, particularly among nurses, points to the contribution of job design and organizational interventions to injury and illness outcomes, including needle-stick injuries (Clarke et al. 2002; Stone and Gershon 2006).
Another area of research that focuses on organizational factors, though does not always include the measurement of exposures at the organizational level, is the area of workplace psychosocial exposures. The workplace presents psychological exposures associated with various somatic and mental health outcomes. For example, studies of the impact of downsizing provide a window into the effect of psychosocial environment on worker health. A 2001 review of the evidence for the health impacts of work organization reported that 90% of 25 downsizing studies reviewed found a negative association with workers' health and safety outcomes (Quinlan et al. 2001). Another well-known area of study is the analysis of job demand and control (and their `mismatch', job strain) on worker health. Job strain is usually measured at the individual level, though it is argued that job strain is a social construct, reflecting qualities of the work environment. The manner in which work is organized dictates the demand and control associated with the performance of jobs, thus researchers have recently identified the need to analyze demand/control at the aggregate work-unit level (Soderfeldt et al. 1997; Leyland and Groenewegen 2003; Eloivainio et al. 2004). By modeling individual's responses to questions about job demand, control, and other exposures both at the level of the individual and, aggregated, at the level of the work unit (eg., department, work group, plant), researchers observe that variation in individuals' health outcomes draws from both differences in individual responses and work unit aggregates.
As with job control, demand and job strain, the effects of most working conditions, have been examined at the individual level, by comparing predictors such as individuals' working hours or perceived safety climate against individual health outcomes. These constructs can vary importantly across job settings, however; for example, Amick (Amick 1998), showed higher strain indices and poorer self-reported health across women employed in healthcare settings. Many workplace psychological processes likely operate on multiple levels: both the individual-level, and that of the work unit(s), departments, or plants, where presumably at least some fraction of the exposure originates. Newer modeling techniques allow for the estimation of effects at multiple levels (e.g., the individual and the plant).
The methodology behind studying workplace-level factors has been sharpened by social epidemiologists, under the rubric of multilevel (or hierarchical) analysis and modeling.
In occupational health, multilevel modeling is increasingly being used to distinguish and quantify variability in effects of individual-level predictors from those of the workplace, department, or other organizational unit, with specific attentions to potential “cross-level” interactions between individual factors (e.g., age, sex) and aggregate characteristics (e.g., workplace size, type, region) (Soderfeldt et al. 1997). Multilevel analysis, applied to occupational cohorts, accounts for clustering among workers in the same unit, rather than treating each subject (worker) as an independent observation, thus better accounting for autocorrelation in occupational datasets. Importantly, most occupational datasets are inherently hierarchical, with workers nested within organizational units; as such, multilevel modeling offers advantages for improved validity and efficiency over previous strategies, such as including binary indicators for each organizational unit into a single-level multivariate regression model, which accounts for a mean effect by plant, but does not allow for worker “fit” though interactions between individual and workplace characteristics.
Soderfeldt et al (1997) first applied multilevel modeling to study the demand–control model in an occupational cohort, and concluded that the job variables in the demand-control model drew a significant portion of their variation from organizational level factors. Later, results from the prospective Finnish Public Sector Study of over 25,000 public sector employees found, using intra-class correlations, that 21% and 15% of the variability in job strain and job demand, respectively, occurred at the work unit level. The study reported that higher-strain jobs (assessed by self-report or aggregate measure) conferred increased risk of disability, relative low-strain jobs (Laine et al. 2008). In a separate Finnish cohort of 2,969 hospital personnel, both individual- and unit-level decision latitude (i.e., control) and `organizational justice' predicted certified sickness absence (Eloivainio et al. 2004). Multilevel methods should, where appropriate (these methods require minimum numbers of `clusters' or work units), be applied to studies of occupational exposures.
In summary, the context of the workplace (and/or other work unit) has been increasingly revealed to be an important predictor of health. Variation in the work environment – safety culture, work organization, etc – may be more salient to occupational health outcomes, though research will reveal more. More work must be done to determine the relationship and interdependence of organizational- and individual- level exposures, and their contributions to observed socio-economic gradients in health.
(5) The New Employment “Contract” and Worker Health: What are the implications for the gradient?
Despite the work-related health and safety risks elucidated above, there is compelling evidence that work may confer important health advantages as well. Many studies have documented that stably employed adults experience better health and survival than those who are less stably or never employed. Recent evidence of the health benefits of work are documented in Finnish studies and strong evidence is provided by many occupational cohorts, in which those who retire early — even from hazardous occupations — have consistently worse outcomes than those who continue working, with large increases in adverse lifestyle, accidental death, and homicide (Kivimaki et al. 2003; Virtanen et al. 2008). For this reason, short-term workers are generally excluded from cohort studies, as their inclusion may mask detrimental effects of work exposures. Much of this disparity has been attributed to selection effects, i.e., that men and women with stable habits and lifestyle are more likely to be stably employed, and also to enjoy better health. Alternatively, there is some suggestion, including studies of non-voluntary changes in workforce participation (e.g., eastern European males after the fall of communism) (Kopp et al. 2007), that work itself may confer positive health benefits, though it has been difficult to establish what aspects of stable work (e.g., regular activity, sense of responsibility, efficacy, role) may confer benefits beyond those attributable to income and material well-being.
Better understanding these non-economic health aspects of work becomes even more salient as the older order of work is rapidly disappearing. Historically, most workers spent long stretches of their careers working for a single employer, under a covenant in which employers were generally expected to provide continued employment and security, in return for allegiance and continued efforts, for the common benefit of both parties—with or without the intercession of a union. This venerated arrangement has begun to erode as a newer one is developing, wherein workers sell their portions of their labor effort in the marketplace. While the erosion of the old “contract” may confer benefits to some employees (e.g., flexibility, mobility, competitive pricing for relatively scarce skills). It likely also confers new hazards (e.g., economic insecurity, loss of social support networks, transfer of responsibility for retirement planning from employers to individuals). Unemployment, once only a risk to employees with less marketable or over-supplied skills, or workers in economically marginal sectors, has increasingly become a reality for many, if not most employees; many will experience periods of relative underemployment as market conditions fluctuate. While for many workers, especially in lower status occupations, chronic risk of unemployment or underemployment is not new, the diffusion of un- and underemployment into the more highly educated workers has increased the overall prevalence of related risks, and created a compelling urgency to understand the health consequences of these economic and societal transformations.
While the health risks associated with unemployment per se has been studied (reviewed below), the impact of these other aspects have only recently been seriously examined as a contribution to social gradients in health. In this chapter we shall review what has been learned so far, as its importance may grow as the economy continues to change.
Unemployment
Macroeconomic studies of the societal effect of increases and decreases in employment rates as occur through business cycles have yielded, perhaps surprisingly, little clear indication that growth, with its attendant increases in the rate of employment, results in short-term gains in mortality or self-rated health, except psychologically; more surprisingly, modern studies of recession have shown either minimal (ref: Indonesian studies) or positive impacts on overall mortality, cardiovascular and accidental death rates, infant mortality, and self-rated health; only mental health and suicide appear “procyclical” (Ruhm 2003; Granados 2005; Ruhm 2005). Stated reasons include demonstrated decreases in adverse health behaviors during recessions, as well as less overall driving, risky-behaviors and the like. What is less clear from these reports is upon which segments of the population this “benefit” of unemployment is conferred, all the more vexing I light of multiple studies showing that unemployed individuals do poorly. Because of the important methodological issues raised by persistent selection effects and SES confounding associated with employment insecurity, the best studies of the health effects caused by unemployment are assessments of larger plant closings, wherein individual selection is minimized. Kasl (Kasl et al. 1975) found worse self-reported health and increased adverse health behaviors after job loss, and similar observations were reported in more recent studies (Hamilton et al. 1990; Keefe et al. 2002) though longer-term consequences have been less well explored. There are many longitudinal studies of men and women who have become unemployed for various reasons, though these studies are often confounded by other factors, including SES and education, which may themselves augur poor health outcomes. Jin et al. reviewed the health impacts of unemployment (Jin et al. 1995), and documented excess mortality among individuals who had ever been unemployed, compared with those who had not. Swedish twin registry studies, comparing mortality 10 and 24 years later among young adults unemployed in 1973, found broad mortality excess compared both to their siblings and to the general population; these differences were not explained by prior smoking, drinking or chronic disease status (Nylén et al. 2001; Voss et al. 2004). The U.S. Health and Retirement Study found both short- and long-term effects of involuntary job loss on physical function and cardiovascular disease among older workers, after accounting for smoking and income (Gallo et al. 2005; Gallo et al. 2006). Census studies in the UK and Denmark have also documented that cancer rates and mortality were higher among those previously unemployed, after controlling for tobacco use (Lynge 1997). Mathers and Schofield (Mathers and Schofield 1998), likewise, showed the effects of unemployment to be greater than those of economic loss alone, suggesting that stable work may confer benefits beyond income and material well-being. Efforts to explain these negative health effects have focused on loss of social support (Roberts et al. 1997) and psychological stressors including lowered self-esteem and depression (Feather and O'Brien 1986; Kessler et al. 1988). Some physical effects may be mediated through inflammatory pathways, as suggested by recent data from the CARDIA study, which showed elevated C-reactive protein (CRP) levels 15 years after baseline among men who had been unemployed five years previously, after adjustment for health behaviors and SES (Janicki-Deverts et al. 2008).
Work Insecurity
Several recent studies of perceived stress have suggested that prolonged fear of losing a job may be more damaging than job loss itself (Heaney et al. 1994; Aronsson 1999), particularly for mental health and self-reported health status (Ferrie et al. 1998; De Witte 1999). More worrisomely, Mattiasson (Mattiasson et al. 1990) showed direct effects of job-loss threat on cardiovascular risk factors, including blood pressure and serum cholesterol, though the associated longer-term health outcomes and mortality gradients remain unestablished. Likewise, the elevated cardiovascular risk factors reported (Arnetz 1991) among Swedish factory workers, and British civil servants in Whitehall II (Ferrie et al. 1998), do not establish longer-term health outcomes. These studies focused primarily on the impact of fear of job loss occurring in the context of feared lay-offs and firm closings. Whether similar impacts will develop in workers for whom the old notion of job security itself no longer exists in the newer environment remains an open question, but an urgent one.
Non-Traditional, Non-Standard, and Contingent Work
It is not surprising that unemployment, or fear of unemployment, should confer a loss of both tangible and intangible health benefits of steady work. In economic recessions, these effects certainly become more widespread, though deeper structural changes in the nature of work, brought about by globalization, technological change, and economic restructuring may prove more intractable and, potentially, more consequential over the long term. For example, most working adults in developed countries since the end of World War II have been working under a “contract”—formal or otherwise—conferring relatively predictable, and generally rising, wages and benefits in exchange for continued work and corporate fidelity. Work has traditionally been conducted at the employer's place of business, during regular business hours. These traditional characteristics of work have shifted in recent decades, with the rise of telecommuting, enabled by modern technologies, and changing family structures demanding greater flexibility in work hours and location. In 1995, the BLS estimated that 30% of all US workers are on-call or day laborers, involuntarily part-time, self-employed, work for a contract labor firm, or work from home. A follow-up survey is not available, though evidence points to an increase in these non-traditional, non-standard, contingent, or precarious forms of work, the health effects of which are now under scrutiny. Two thorough reviews (Quinlan et al. 2001; Price and Burgard 2008) emphasize potential health risks from these forms of work, which include material and income loss, greater work stress, enhanced work-family conflict due to irregular scheduling and high work demands; poorer regulation of the physical work environment, and adverse social effects including isolation.
The work categories described above, while sharing some common features, are very different, and it is probably inappropriate to lump self-employment by choice with involuntary part-time work, or combine forms of full-time employment with on-call or temporary work. Indeed, some efforts have been made to distinguish the health effects of these varying work structures (Price and Burgard 2008), particularly as many non-traditional job structures exist by choice, by men and women needing flexible hours to meet family-care demands, because these structures may confer opportunities for economic and personal growth not available in the traditional labor market. As such, health studies of `precarious employment' can suffer from extreme heterogeneity in the populations included, and the applicability of the results to particular industries past or future should be interpreted with caution. In addition, data on the SES distribution of precariously employed workers is limited, although Hipple (Hipple 2001) has shown non-traditional work structures to be more prevalent among women, minorities, and poorer groups. It has also been assumed that such jobs within each broad social class may be less desirable in the aggregate, and thus more likely held by relatively disadvantaged workers (Quinlan et al. 2001), which in turn makes distinguishing employment consequences from unmeasured selection effects problematic (Benach et al. 2000; Benach et al. 2002).
Many studies attempt to relate irregular employment conditions with various health outcomes most, but not all, report adverse effects on injury rates, self-reported mental and physical health, or poorer health and safety performance (Quinlan et al. 2001). One consistent finding is that workers in non-traditional settings experience more injuries, and more severe injury (e.g., fatality) (Blank 1995; Silverstein 1998; Mayhew and Quinlan 1999; Meyer and Muntaner 1999; Morris 1999). While the contribution of precarious employment to the health gradient is not immediately transparent, it underscores the likelihood that these job conditions may be consistently worse than in traditional work settings, even after adjusting for the nature of the work. A few of these studies substantiate these claims using self-reported depression and fatigue (Aronsson and Goransson 1999), musculo-skeletal symptoms (Johansson 1995), and physical and psychological health (Dooley et al. 1994; Friedland and Price 2003; Benach et al. 2004), though objective and long-term measures are lacking. Finally, while the demonstration of adverse health and safety conditions and work culture associated with these jobs must be viewed more as process than outcome measure (Aronsson and Goransson 1999; Kalleberg et al. 2000), the importance of these factors to deteriorating health and mortality suggests that such links will become manifest, perhaps justifying the use of the term “precarious” to describe these work-types preferred by many investigators (Quinlan et al. 2001).
(6) Sex, Gender and Occupation: How have dramatic changes in the roles of women in workplaces affected the health of women?
The gendered landscape of work is rapidly changing. Despite greater numbers of women in traditionally `male' roles, gender stratification in job assignment persists overall, and is well documented (Alexanderson and Ostlin 2001; United States Department of Labor 2002). Accordingly, men and women have historically differed, on average, in job-related chemical exposures (London et al. 2002), ergonomic demands (Silverstein et al. 1986), accidents (Salminen et al. 1992), and psychosocial stressors (Hall 1989).
Research on gender and health, in recent decades, has called for improved access to traditionally `male' jobs for women and, relatedly, improved data and analysis of the health effects of working conditions on women's health. Generally, it remains true that greater accessibility allows individuals the freedom to make appropriate working decisions as meet their individual needs. The altered gendered space of work also poses new challenges and offers new opportunities for occupational health research, as a wider range of individuals performing any specific job offers better opportunities to separate job effects from individual health risk characteristics. There remains, however, relatively little research on the effect of `male' work roles on women's health, and some studies show greater health risks associated with blue-collar work for women than men (Hall et al. 1993; LaCroix 1994; Baigi et al. 2002; Clougherty et al. (under review)). These results have been surprising as, in most prior adult cohorts, women's risk of chronic illness, including cardiovascular illness, diabetes, and COPD, has been notably lower than men's, until relatively late in life. Thus, the observation that illness should actually be higher for blue-collar women than men suggests strong workplace risk factors, to which women may be particularly responsive (e.g., possibly some chemical exposures), or prevalent factors which specifically affect women (e.g., adverse social environments).
Beyond this elevated chronic disease risk, hourly work appears to pose additional risks to women's health. Controlling for work tasks themselves, women get injured 40–60% more often, with greater injury severity (Pollack et al. 2007). Likewise, rates of absenteeism, and time to return to work after illness, are consistently worse in blue-collar women than their male counterparts (Hill et al. 2008; Hill et al. (Submitted)).
It remains unknown what portion of these elevated risks among women may be attributable to differences in sex-linked biological susceptibility, or to culturally-derived gender differences, such as gendered selection into job roles, workplace harassment, or personal life circumstances. This critical distinction between sex (i.e., biological differences by chromosomal complement, including reproductive organs and hormonal composition) and gender (i.e., self-representation, socially-derived behaviors and roles, and response by social institutions) is needed towards accurately disaggregating work-related health risks for both sexes, and for designing effective workplace interventions (Wizemann and Pardue 2001; Krieger 2003; Messing and Stellman 2006).
Socioeconomics and selection into job roles
It is important to recognize that, even as sanctioned sex-stratification in work is reducing, women and men continue to live and work within a gendered society, and evidence indicates that women & men `choose' blue-collar work for very different reasons. In our dataset of 15,000 aluminum manufacturing employees across eight U.S. states, we found a greater likelihood of blue-collar work among lower-educated, African-American, and single parent women than men (Clougherty et al. (under review)). We observed that the women in hourly jobs tended to be from lower SES background, have greater financial need (e.g., single mothers), and were more likely to hold lower-grade (e.g., lower-skilled) hourly jobs, than were hourly men. These observations suggest that most of the hourly women had not planned to be so, but rather were drawn towards manufacturing jobs out of financial necessity. More of the hourly men in our dataset, comparatively, were skilled individuals in higher-rank hourly jobs, or were hired by the company later in their careers.
Sex, gender, and causal effects
If blue-collar work shows a different causal effect on women's health than on men's, we must carefully pose the question of why this is the case: Is this a difference of sex, or biological susceptibility to common workplace exposures, or of gender, influencing job placement, workplace stress, or other life demands?
To examine gender influences on job assignment in our data, we used propensity score models to examine the effect of pre-hire sociodemographic characteristics and personal life factors (e.g., marital status, parity) on men's and women's employment decisions. After adjustment using propensity scores, hourly work conferred greater risks of hypertension, a broad marker of cardiovascular risk, among women than men. The effect proved stronger using more stringent case criteria. Tenure, a surrogate for cumulative exposure, conferred greater risks among women likely to be hourly, suggesting greater susceptibility to workplace risk factors with lower SES. In addition, higher job grades reduced risks more consistently among men than women. Finally, men in blue-collar jobs with higher physical demands displayed the protective effect of lower BMI, which was not observed in women, while women showed stronger negative health effects with physical strain.
Possible explanations may include sex-linked differential susceptibility to workplace contaminants, or gender differences in the manufacturing environment experience. The same worksite and task may be experienced differently by women and men; for example, differences in anthropomorphic measurements and work equipment designed for male bodies can increase women's task burden (Courville et al. 1991; Stevenson et al. 1996; Punnett and Bergqvist 1999). Women are still a tiny fraction of the blue-collar working population, and are more likely to experience harassment, discrimination (Arcand et al. 2000; Gutek 2001), and low job control (Hall 1989; Bourbonnais et al. 2000). Finally, non-workplace factors, including family roles and domestic responsibilities, may influence susceptibility to employment-related health effects; women's greater average time on household tasks (Blau et al. 2002) may affect fatigue, non-occupational stress (Bergqvist et al. 1995; Brisson et al. 1999), response to workplace stressors, and return to work following illness or injury (Feeney et al. 1998; Katz et al. 1998; Islam et al. 2001).
Women and job grade
Women still comprise a small proportion of blue-collar workers, but are overly represented in low-grade jobs (Statistics Canada 2001; Catalyst 2002), and earn less than men in the same job category (United States Department of Labor 2002). This gendered stratification is important because low job grade has been linked to heart disease (Marmot et al. 1997), hypertension (Calhoun et al. 1998), and injury (Houtman et al. 1994; Wilkins and Mackenzie 2007). As much job grade research has focused on largely male, “white-collar” populations (e.g., (Marmot and Smith 1991)), it remains unclear whether job status operates similarly among women or blue-collar workers. Finally, `job grade' is associated with many chemical, physical, and psychosocial stressors, thus its `causal components' for health remain unknown, and may vary by age, gender, and setting (Sparacino et al. 1982). Together, these observations suggest that, currently, blue-collar work settings may not be healthy workplaces for women. It is less clear, however, why this is so. The negative effect of blue-collar work on women's health, combined with higher risks associated with job tenure among women predicted to be hourly, together raise important questions about the nature of manufacturing work which may differently affect men and women. Why employment duration increases risks more among women than men is unclear, and may indicate different responses to cumulative physical, chemical, or psychosocial exposures at work. Finally, the heightened effects observed among women and men predicted to be hourly may suggest interaction effects between SES and job-related exposures, possibly suggesting a heightened susceptibility with lower SES.
Summary
Weighing the evidence, it is generally apparent that work contributes to the adult SES-health gradient, despite the varied limitations to our current knowledge. The status and social benefits that work confers are likely important, but it is also probable that psychosocial and physical stressors play a role, as well as organizational structure and person-environment fit. The limited data available at this stage to assess the effects of traditionally `male' roles (generally physical labor and manufacturing jobs) on women's health point to greater risks among women, likely modified by those social factors which predict women's likelihood to work in manufacturing positions. Likely, but far from proven by the extant analyses, is that these multiple factors likely work additively and multiplicatively to shape worker health, though a cumulative-risk-factor perspective, as described by Evans and Kim (CITE: MacArthur Chapter X), may prove a useful approach. However, because strategies to reduce health risks from work will require a multi-faceted approach, expanding knowledge of each aspect remains the primary challenge, even as multi-level and more nuanced models will be needed to develop closure in this stage of the research.
References
- Aboa-Eboule C, Brisson C, et al. Job strain and risk of acute recurrent coronary heart disease events. Journal of the American Medical Association. 2007;298(14):1652–1660. doi: 10.1001/jama.298.14.1652. [DOI] [PubMed] [Google Scholar]
- Alexanderson K, Ostlin P. Worklife and health in Sweden. National Institute for Working Life; M. S. Stockholm: 2001. Work and ill-health among men and women in Sweden. [Google Scholar]
- American Thoracic Society American Thoracic Society Statement: Occupational contribution to the burden of airway disease. Am J Respir Crit Care Med. 2003;167:787–797. doi: 10.1164/rccm.167.5.787. [DOI] [PubMed] [Google Scholar]
- Amick B. Relationship of job strain and iso-strain to health status in a cohort of women in the U.S. Scand. J Work Environ Health. 1998;24:54–61. doi: 10.5271/sjweh.278. [DOI] [PubMed] [Google Scholar]
- Arcand R, Labreche F, et al. enquete sociale et de sante 1998 (Social and Health Survey 1998) Institute de la statistique du Quebec; Quebec: 2000. Work environment and health. (environnement de travail et santé) pp. 525–570. [Google Scholar]
- Arnetz B. Neuroendocrine and immunologic effects of unemployment and job insecurity. PsychotherPsychosom. 1991;55:76–80. doi: 10.1159/000288412. [DOI] [PubMed] [Google Scholar]
- Aronsson G. Contingent workers and health and safety. Work Employment Society. 1999;13:439–460. [Google Scholar]
- Aronsson G, Goransson S. Permanent employees but not in a preferred occupation: Psychological and medical aspects. J Occup Health Psychol. 1999;4:152–163. doi: 10.1037//1076-8998.4.2.152. [DOI] [PubMed] [Google Scholar]
- Baigi A, Fridlund B, et al. Cardiovascular mortality focusing on socio-economic influence: the low-risk population of Halland compared to the population of Sweden as a whole. Public Health. 2002;116(5):285–288. doi: 10.1038/sj.ph.1900877. [DOI] [PubMed] [Google Scholar]
- Barbini N, Gorini G, et al. Analysis of arterial hypertension and work in the epidemiologic study “Aging, Health, and Work. Epidemiologia E Prevenzione. 2005;29(3–4):160–165. [PubMed] [Google Scholar]
- Barone-Adesi F, Richiardi L, et al. Population attributable risk for occupational cancer in Italy. Int J Occup Environ Health. 2005;11(1):23–31. doi: 10.1179/oeh.2005.11.1.23. [DOI] [PubMed] [Google Scholar]
- Bartley M. Unemployment and health: selection or causation – a false antithesis? Sociology of Health and Illness. 1988;10(1):41–67. [Google Scholar]
- Belkic K, Emdad R, et al. Occupational profile and cardiac risk: possible mechanisms and implications for professional drivers. Int J Occup Environ Health. 1998;11:37–57. [PubMed] [Google Scholar]
- Belkic K, Lansbergis P, et al. Psychosocial factors: review of the empirical data among men. In: Schnall PL, Belkic K, Landsbergis PA, Baker D, editors. The workplace and cardiovascular disease. Vol. 15. Hanley & Belfus, Inc.; Philadelphia: 2000. pp. 24–46. [Google Scholar]
- Belkic KL, Landsbergis PA, et al. Is job strain a major source of cardiovascular disease risk? Scan J Work Environ Health. 2004;30(2):85–128. doi: 10.5271/sjweh.769. [DOI] [PubMed] [Google Scholar]
- Benach J, Amable M, et al. The consequences of flexible work for health. J Epidem Commun Health. 2002;56:405–406. doi: 10.1136/jech.56.6.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benach J, Benavides FG, et al. The health damaging potential of new types of flexible employment: A challenge to public health researchers. Am J Pub Health. 2000;90:1316–1317. doi: 10.2105/ajph.90.8.1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benach J, Gimeno D, et al. Types of emplyment and health in the European Union: Changes from 1995–2000. Eur J Public Health. 2004;14:314–321. doi: 10.1093/eurpub/14.3.314. [DOI] [PubMed] [Google Scholar]
- Bergqvist U, Wolgast E, et al. Musculoskeletal disorders among visual display terminal workers: Individual, ergonomic and work organizational factors. Ergonomics. 1995;38:763–776. doi: 10.1080/00140139508925148. [DOI] [PubMed] [Google Scholar]
- Bianchi C, Bianchi T. Malignant mesothelioma: global incidence and relationship with asbestos. Industrial Health. 2007;45(3):379–387. doi: 10.2486/indhealth.45.379. [DOI] [PubMed] [Google Scholar]
- Blank V. Hidden accident rates and patterns in the Swedish mining industry due to the involvement of contract workers. Safety Sci. 1995;21:23–35. [Google Scholar]
- Blau F, Ferber M, et al. The economics of women, men, and work. Prentice Hall; Upper Saddle River, NY: 2002. [Google Scholar]
- Blumenthal J, Thyrum E, et al. Contribution of job strain, job status, and marital status to laboratory and ambulatory blood pressure in patients with mild hypertension. Journal of Psychosomatic Research. 1995;39(2):133–144. doi: 10.1016/0022-3999(94)00087-l. [DOI] [PubMed] [Google Scholar]
- Boggild H, Knutsson A. Shift work, risk factors and cardiovascular disease. Scan J Work Environ Health. 1999;25:85–99. doi: 10.5271/sjweh.410. [DOI] [PubMed] [Google Scholar]
- Boggild H, Knutsson A. Shift work, risk factors and cardiovascular disease [review] Scand J Work Environ Health. 1999;25(2):85–99. doi: 10.5271/sjweh.410. [DOI] [PubMed] [Google Scholar]
- Boggild H, Saudicani P, et al. Shift work, social class and ischaemic heart disease in middle aged and elderly men; a 22 year follow-up in the Copenhagen male study. Occup Environ Med. 1999;56:45–64. doi: 10.1136/oem.56.9.640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosma H, Peter R, et al. Two alternative job stress models and the risk of coronary heart disease. Am J Pub H. 1998;88:68–74. doi: 10.2105/ajph.88.1.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourbonnais R, Larocque B, et al. environnement psychosocial du travail (The psychosocial environment of work) In: Daveluy C, Audet R, Lapointe F, editors. Enquete sociale et de sante. Institut de la statistique; Quebec: 2000. pp. 571–583. [Google Scholar]
- Brisson C, Laflamme N, et al. Effect of family responsibilities and job strain on ambulatory blood pressure among white-collar women. Psychosomatic Medicine. 1999;61:205–213. doi: 10.1097/00006842-199903000-00013. [DOI] [PubMed] [Google Scholar]
- Brook RD, Franklin B, et al. Air pollution and cardiovascular disease. A statement for healthcare professionals from the expert panel on population and prevention science of the American Heart Association. Circulation. 2004;109:2655–2671. doi: 10.1161/01.CIR.0000128587.30041.C8. [DOI] [PubMed] [Google Scholar]
- Bureau of Labor Statistics 2006.
- Calhoun H, Hemingway H, et al. Socio-economic status and blood pressure: an overview analysis. Journ Human Hypertens. 1998;12:91–110. doi: 10.1038/sj.jhh.1000558. [DOI] [PubMed] [Google Scholar]
- Cantley L, Iennaco J, et al. An externally rated job demand survey to assess physical and psychological job stress in relation to injury risk in aluminum manufacturing jobs. Occup Environ Med. Submitted. [Google Scholar]
- Catalyst 2002 Retrieved January 15, 2008, from www.catalystwomen.org.
- Chan-Yeung M, Malo J-L. Tables of major inducers of occupational airways disease. In: Bernstein IL, Chan-Yeung M, Malo J-L, Bernstein DI, editors. Asthma in the workplace. Marcel Dekker; New York: 1999. [Google Scholar]
- Chandola T, Bartley M, et al. Health selection in the Whitehall II study, UK. Soc Sci Med. 2003;56:2059–72. doi: 10.1016/s0277-9536(02)00201-0. [DOI] [PubMed] [Google Scholar]
- Chandola T, Britton A, et al. Work and coronary heart disease: what are the mechanisms? Eur Heart J. 2008 doi: 10.1093/eurheartj/ehm584. [DOI] [PubMed] [Google Scholar]
- Chandola T, Brunner E, et al. Chronic stress at work and the metabolic syndrome: prospective study. BMJ (Clin Res) 2006 doi: 10.1136/bmj.38693.435301.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Checkoway H, Pearce N, et al. Research Methods in Occupational Epidemiology. Monographs in epidemiology and statistics. Oxford University Press; New York: 2004. [Google Scholar]
- Chen E, Schreier HMC, et al. Chronic traffic-related air pollution and stress interact to predict biological and clinical outcomes in asthma. Env Health Perspec. 2008 doi: 10.1289/ehp.11076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark G. Organizational culture and safety: an interdependent relationship. Aust Health Rev. 2002;25(6):181–189. doi: 10.1071/ah020181. [DOI] [PubMed] [Google Scholar]
- Clarke SP, Sloane DM, et al. Needlestick injuries to nurses, in context. LDI Issue Brief. 2002;8(1):1–4. [PubMed] [Google Scholar]
- Claussen B, Smits J, et al. Intragenerational mobility and mortality in Oslo: Social selection versus social causation. Soc Sci Med. 2005;61:2513–2520. doi: 10.1016/j.socscimed.2005.04.045. [DOI] [PubMed] [Google Scholar]
- Clougherty J, Eisen E, et al. Workplace status and risk of hypertension among hourly and salaried aluminum manufacturing employees. Soc Sci Med. 2008 doi: 10.1016/j.socscimed.2008.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clougherty JE, Eisen EA, et al. Gender and sex differences in job placement, and in effects of workplace status and work tenure on hypertension. Soc Sci Med. under review. [Google Scholar]
- Clougherty JE, Houseman EA, et al. Examining intra-urban variation in fine particle mass constituents using GIS and constrained factor analysis. Atmos Environ. under review. [Google Scholar]
- Clougherty JE, Levy JI, et al. Synergistic effects of traffic-related air polliton and exposure to violence on urban asthma etiology. Environ Health Perspect. 2007;115(8):1140–1146. doi: 10.1289/ehp.9863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coggon D, Taylor AN. Coal mining and chronic obstructive pulmonary disease: a review of the evidence. Thorax. 1998;53:398–407. doi: 10.1136/thx.53.5.398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cottington EM, Matthews KA, et al. Occupational stress, suppressed anger, and hypertension. Psychosomatic Medicine. 1986;48:249–260. doi: 10.1097/00006842-198603000-00010. [DOI] [PubMed] [Google Scholar]
- Courville J, Vezina N, et al. Comparison of the work activity of two mechanics: a woman and a man. Int J Ind Ergon. 1991;7:163–174. [Google Scholar]
- Cullen M, Vegso S, et al. Use of Medical Insurance Claims Data for Occupational Health Research. J Occup Environ Med. 2006;48(10):1054–1061. doi: 10.1097/01.jom.0000241049.23093.a4. [DOI] [PubMed] [Google Scholar]
- Cullen MR. The Search for Preventable Causes of Cardiovascular Disease: Whither Work? Am J Epid. doi: 10.1093/aje/kwp078. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Witte H. Job insecurity and psychological well being: Review of the likterature and exploration of some unresolved issues. Eur J Work Org Psych. 1999;8:155–177. [Google Scholar]
- DeVogli R, Ferrie J, et al. Unfairness and health: evidence from the Whitehall II study. J Epidem Comm Health. 2007;61(6):513–518. doi: 10.1136/jech.2006.052563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doll R, Peto R. The causes of cancer. Oxford University Press; Oxford: 1981. [Google Scholar]
- Dooley D, Catalano R, et al. Depression and unemployment: Panel findings from the epidemiologic catchment area study. Am J Commun Psychol. 1994;22:745–765. doi: 10.1007/BF02521557. [DOI] [PubMed] [Google Scholar]
- Eloivainio M, Kimivaki M, et al. Job decision latitude, organizational justice and health: multivariate covariance structure analysis. Soc Sci Med. 2004;58:1659–1669. doi: 10.1016/S0277-9536(03)00366-6. [DOI] [PubMed] [Google Scholar]
- Erikson R. Social class assignment and mortality in Sweden. Soc Sci Med. 2006;62:2151–2160. doi: 10.1016/j.socscimed.2005.09.009. [DOI] [PubMed] [Google Scholar]
- Esler M, Julius S, et al. Mild high-renin essential hypertension: neurogenic human hypertension? N Engl J Med. 1977;296:405–411. doi: 10.1056/NEJM197702242960801. [DOI] [PubMed] [Google Scholar]
- Evans GW, Johansson G, et al. Psychosocial factors and the physical environment: Inter-relations in the workplace. Internat Rev Indust Organ Psychol. 1994:1–29. [Google Scholar]
- Feather NT, O'Brien GE. A longitudinal study of the effects of employment and unemployment on school-leavers. J Occup Psych. 1986;59:121–144. doi: 10.1111/j.2044-8295.1986.tb02211.x. [DOI] [PubMed] [Google Scholar]
- Feeney A, North F, et al. Socioeconomic and sex differentials in reason for sickness absence from the Whitehall II study. Occup Environ Med. 1998;55:91–98. doi: 10.1136/oem.55.2.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrie J, Shipley MJ, et al. Health effects of anticipation of job change and non-employment: Longitudinal data from the Whitehall II study. Brit Med J. 1998;311:1264–1269. doi: 10.1136/bmj.311.7015.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fine LJ. Chemical and physical factors. In: Schnall PL, Belkic K, Landsbergis PA, Baker D, editors. The workplace and cardiovascular disease. Vol. 15. Hanley & Belfus Inc.; Philadelphia: 2000. pp. 18–24. [Google Scholar]
- Folkow B. Physiological aspects of primary hypertension. Physiology Review. 1981;62:347–504. doi: 10.1152/physrev.1982.62.2.347. [DOI] [PubMed] [Google Scholar]
- Friedland DS, Price RH. Underemployment: Consequences for the health and well-being of workers. Am J Commun Psych. 2003;32:33–45. doi: 10.1023/a:1025638705649. [DOI] [PubMed] [Google Scholar]
- Gallo WT, Bradley EH, et al. Health effects of involuntary job loss among older workers: Findings from the health and retirement survey. J Geront Series B: Psych Sci Soc Sci. 2005;55:S131–S140. doi: 10.1093/geronb/55.3.s131. [DOI] [PubMed] [Google Scholar]
- Gallo WT, Teng HM, et al. The impact of late career job loss on myocardial infarction and stroke: A 10 year follow up using the health and retirement survey. Occup Environ Med. 2006;63:683–687. doi: 10.1136/oem.2006.026823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granados JAT. Increasing mortality during the expansions of the US economy 1900–96. Intern J Epid. 2005;34:1194–1202. doi: 10.1093/ije/dyi141. [DOI] [PubMed] [Google Scholar]
- Greiner BA, Krause N. Expert-observer assessment of jobcharacteristics. In: Schnall PL, Belkic K, Landsbergis PA, Baker D, editors. The workplace and cardiovascular disease. Vol. 15. Hanley & Belfus Inc.; Philadelphia: 2000. pp. 175–183. [Google Scholar]
- Guldenmund FW. The nature of safety culture: a review of theory and research. Safety Sci. 2000;34:215–257. [Google Scholar]
- Gutek BA. Women and paid work. Psychol Women Q. 2001;25(4):379–393. [Google Scholar]
- Haas J, Buchan R. Occupational health and safety hazards in Colorado small industry. Appl. Occup. Environ. Hyg. 1995;10:151–155. [Google Scholar]
- Hall E, Johnson J, et al. Women, occupation, and risk of cardiovascular morbidity and mortality. Occup Med. 1993;8(4):709–719. [PubMed] [Google Scholar]
- Hall EM. Gender, work control, and stress: A theoretical discussion and an empirical test. Int J Health Serv. 1989;19:725–745. doi: 10.2190/5MYW-PGP9-4M72-TPXF. [DOI] [PubMed] [Google Scholar]
- Hamilton VL, Broman CL, et al. Hard times and vulnerable people: Initial effects of plant closings on autoworkers' mental health. J Health Soc Behav. 1990;31:123–140. [PubMed] [Google Scholar]
- Heaney CA, Israel BA, et al. Chronic job insecurity among automobile workers: Effects on job satisfaction and health. Soc Sci Med. 1994;38:1431–1437. doi: 10.1016/0277-9536(94)90281-x. [DOI] [PubMed] [Google Scholar]
- Heponiemi T, Elovainio M, et al. Relationship between unemployment and health among health care professionals: Health selection of health effect? Journ Psychosom Res. 2007;63:425–431. doi: 10.1016/j.jpsychores.2007.04.005. [DOI] [PubMed] [Google Scholar]
- Hill JJ, Slade MD, et al. The relationship between lost work time and duration of absence spells. Proposal for a payroll driven measure of absenteeism. J Occup Environ Med. 2008;50:840–851. doi: 10.1097/JOM.0b013e31816b44dd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill JJ, Slade MD, et al. The Impact of Short- Term Disability Benefits on Employment Status after Acute Hospitalization in a Large Manufacturing Workforce. Health Services Research. Submitted. [Google Scholar]
- Hipple S. Contingent work in the late 1990's. Monthly Labor Rev. 2001;124:3–27. [Google Scholar]
- Houtman I, Bongers P, et al. Psychosocial stressors at work and musculoskeletal problems. Scand J Work Environ Health. 1994;20(2):139–145. doi: 10.5271/sjweh.1419. [DOI] [PubMed] [Google Scholar]
- Iennaco J, Cullen MR, et al. Effects of Externally Rated Job Demand and Control on Depression Diagnosis Claims in an Industrial Cohort. AJE. doi: 10.1093/aje/kwp359. Submitted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine . Musculoskeletal Disorders and the Workplace: Low Back and Upper Extremities. National Academy Press; Washington DC: 2001. [PubMed] [Google Scholar]
- Islam SS, Velilla AM, et al. Gender differences in work-related injury/illness: Analysis of workers' compensation claims. Am J Ind Med. 2001;39:84–91. doi: 10.1002/1097-0274(200101)39:1<84::aid-ajim8>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- Janicki-Deverts D, Cohen S, et al. History of unemployment predicts future elevations in C-reactive protein among male participants in CARDIA. Annals Behav Med. 2008 doi: 10.1007/s12160-008-9056-5. [DOI] [PubMed] [Google Scholar]
- Jin RL, Shah CP, et al. The impact of unemployment on health: A review of the evidence. Can Med Assoc J. 1995;153:529–540. [PMC free article] [PubMed] [Google Scholar]
- Johansson J. Psychosocial work factors, physical work load and associated musculoskeletal symptoms among home care workers. Scand J Psychol. 1995;36(2):113–129. doi: 10.1111/j.1467-9450.1995.tb00973.x. [DOI] [PubMed] [Google Scholar]
- Kales SN, Soteriades ES, et al. Emergency duties and deaths from heart disease among firefighters in the United States. New Engl J Med. 2007;356:1207–1215. doi: 10.1056/NEJMoa060357. [DOI] [PubMed] [Google Scholar]
- Kalleberg AL, Reskin BF, et al. Bad jobs in America: Standard and nonstandard employment relations and job quality in the United States. Am Sociological Rev. 2000;65:256–278. [Google Scholar]
- Kaplan G, Keil J. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation. 1993;88(4 Pt 1):1973–1998. doi: 10.1161/01.cir.88.4.1973. [DOI] [PubMed] [Google Scholar]
- Karasek R, Baker D, et al. Job decision latitude, job demands, and cardiovascular disease: a prospective study of Swedish men. Am J Pub H. 1981;71:694–705. doi: 10.2105/ajph.71.7.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karasek R, Brisson C, et al. The Job Content Questionnaire (JCQ): an instrument for internationally comparative assessments of psycho-social job characteristics. J Occup Health Psychol. 1998;3:322–355. doi: 10.1037//1076-8998.3.4.322. [DOI] [PubMed] [Google Scholar]
- Karasek R, Theorell T. The demand-control-support model and CVD. In: Schnall PL, Belkic K, Landsbergis PA, Baker D, editors. The workplace and cardiovascular disease. Vol. 15. Hanley & Belfus, Inc.; Philadelphia: 2000. pp. 78–83. [Google Scholar]
- Kasl SV. The challenge of studying the disease effects of stressful work conditions. Am J Pub H. 1981;71:682–684. doi: 10.2105/ajph.71.7.682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasl SV, Gore S, et al. The experience of losing a job: Reported changes in hedalth, symptoms and illness behavior. Psychosom Med. 1975;37:106–122. doi: 10.1097/00006842-197503000-00002. [DOI] [PubMed] [Google Scholar]
- Katz JN, Lew RA, et al. Prevalence and predictors of long-term work disability due to carpal tunnel syndrome. Am J Ind Med. 1998;33(6):543–550. doi: 10.1002/(sici)1097-0274(199806)33:6<543::aid-ajim4>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- Kauffmann F, Drouet D, et al. Occupational exposure and 12 year spirometric changes among Paris area workers. Br J Indus Med. 1982;39:221–232. doi: 10.1136/oem.39.3.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I. Income inequality and health. In: Berkman L, Kawachi I, editors. Social Epidemiology. Oxford University Press; New York: 2000. [Google Scholar]
- Kawachi I, Colditz GA, et al. Prospective study of shift work and risk of coronary heart disease in women. Circulation. 1995;92:3178–3182. doi: 10.1161/01.cir.92.11.3178. [DOI] [PubMed] [Google Scholar]
- Keefe V, Papaarangi R, et al. Serious health events following involuntary job loss in New Zealand meat processing workers. Int J Epidem. 2002;31:1155–1161. doi: 10.1093/ije/31.6.1155. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Turner JB, et al. Effects of unemployment on health in a community survey: Main, modifying, and mediating effects. J Soc Issues. 1988;44:69–85. [Google Scholar]
- Kim C, Min JY, et al. Job strain and the risk for occupational injury in small-to-mediumsized manufactruring enterprises: a prospective study of 1,209 Korean employees. AJIM. 2009;52:322–330. doi: 10.1002/ajim.20673. [DOI] [PubMed] [Google Scholar]
- Kivimaki M, Head J, et al. Why is evidence on job strain and coronary heart disease mixed? An illustration of measurement challenges in the Whitehall II Study. Psychosom Med. 2006;68:398–401. doi: 10.1097/01.psy.0000221252.84351.e2. [DOI] [PubMed] [Google Scholar]
- Kivimaki M, Head J, et al. Work stress, weight gain and weight loss: evidence for bidirectional effects of job strain on body mass index in the Whitehall II study. Internat J Obesity. 2006;30:982–987. doi: 10.1038/sj.ijo.0803229. [DOI] [PubMed] [Google Scholar]
- Kivimaki M, Head J, et al. Hypertension is not the link between job strain and coronary heart disease in the Whitehall II study. Amer J Hypertension. 2007;20(11):1146–1153. doi: 10.1016/j.amjhyper.2007.06.006. [DOI] [PubMed] [Google Scholar]
- Kivimaki M, Vahtera J, et al. Temporary employment and risk of overall and cause-specific mortality. Am J Epidem. 2003;158:663–668. doi: 10.1093/aje/kwg185. [DOI] [PubMed] [Google Scholar]
- Knuttson A. Health disorders of shift workers. Occup Med. 2003;53:103–108. doi: 10.1093/occmed/kqg048. [DOI] [PubMed] [Google Scholar]
- Kopp MS, Skrabski A, et al. Chronic stress and social changes: socioeconomic determination of chronic stress. Annals of the New York Academy of Sciences. 2007;1113:325–338. doi: 10.1196/annals.1391.006. [DOI] [PubMed] [Google Scholar]
- Krieger N. Genders, sexes, and health: what are the differences, and why does it matter? International Journal of Epidemiology. 2003;32:652–657. doi: 10.1093/ije/dyg156. [DOI] [PubMed] [Google Scholar]
- Kristal-Boneh E, Melamen S, et al. Acute and chronic effects of noise exposure on blood pressure and heart rate among industrial employees: The Cordis study. Arch Environ Health. 1995;50:298–304. doi: 10.1080/00039896.1995.9935958. [DOI] [PubMed] [Google Scholar]
- Kryzyzanowski M, Jedrychowski W, et al. Factors associated with the change in ventilatory function and the development of chronic obstructive pulmonary disease in a 13-year follow-up of the Cracow study. Am Rev Resp Dis. 1986;134:1101–1019. doi: 10.1164/arrd.1986.134.5.1011. [DOI] [PubMed] [Google Scholar]
- Kuper H, Marmot M. Job strain, job demands, decision latitude, and risk of coronary heart disease within the Whitehall II study. J Epidem Commun Health. 2003;57:147–153. doi: 10.1136/jech.57.2.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuper H, Marmot M. Job strain, job demands, decision latitude, and risk of coronary heart disease within the Whitehall II study. J Environ Commun Health. 2003;57:147–153. doi: 10.1136/jech.57.2.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaCroix A. Psychosocial factors and risk of coronary heart disease in women: an epidemiologic perspective. Fertility and Sterility. 1994;62(6 Suppl 2):133S–139S. [PubMed] [Google Scholar]
- Laine S, Gimeno D, et al. Job strain as a predictor of disability pension: the Finnish Public Sector Study. J Epidemiol Community Health. 2008;63:24–30. doi: 10.1136/jech.2007.071407. [DOI] [PubMed] [Google Scholar]
- Landsbergis PA, Schnall PL, et al. Work conditions and masked (hidden) hypertension -- insights into the global epidemic of hypertension. Scand J Work Environ Health. 2008;(Suppl(6)):41–51. [Google Scholar]
- Landsbergis PA, Schnall PL, et al. Lower socioeconomic status among men in relation to the association between job strain and blood pressure. Scand J Work Environ Health. 2003;29(3):206–215. doi: 10.5271/sjweh.723. [DOI] [PubMed] [Google Scholar]
- Landsbergis PA, Schnall PL, et al. Life-Course exposure to job strain and ambulatory blood pressure in Men. Am J Epidem. 2003;157(11):998–1006. doi: 10.1093/aje/kwg095. [DOI] [PubMed] [Google Scholar]
- Landsbergis PA, Theorell T. Self-report questionnaires. In: Schnall PL, Belkic K, Landsbergis PA, Baker D, editors. The workplace and cardiovascular disease. Vol. 15. Hanley & Belfus Inc.; Philadelphia: 2000. pp. 163–171. [Google Scholar]
- Lanki T, de Hartog JJ, et al. Can we identify sources of fine particles responsible for exercise-induced ischemia on days with elevated air pollution? The ULTRA Study. Environ Health Perspec. 2006;114(5):655–660. doi: 10.1289/ehp.8578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lecluyse A. Income-related health inequality in Belgium: a longitudinal perspective. Euro J Health Econ. 2007;8(3):237–243. doi: 10.1007/s10198-006-0024-3. [DOI] [PubMed] [Google Scholar]
- Leigh JP. No evidence of compensating wages for occupational fatalities. Indust.Relations. 1991;30:382–395. [Google Scholar]
- Leyland AH, Groenewegen Multilevel modeling and public health policy. Scand J Public Health. 2003;31:267–274. doi: 10.1080/14034940210165028. [DOI] [PubMed] [Google Scholar]
- Lidfeldt J, Li TY, et al. A Prospective Study of Childhood and Adult Socioeconomic Status and Incidence of Type 2 Diabetes in Women. Am J Epidem. 2007;165(8):882–888. doi: 10.1093/aje/kwk078. [DOI] [PubMed] [Google Scholar]
- London L, de Grosbois S, et al. Pesticide usage and health consequences for women in developing countries: Out of sight, out of mind? Int J Occup Environ Health. 2002;8(1):46–59. doi: 10.1179/oeh.2002.8.1.46. [DOI] [PubMed] [Google Scholar]
- Lynge E. Unemployment and cancer: A literature review. IARC Scientific Publications. 1997;138:343–351. [PubMed] [Google Scholar]
- MacDonald L, Karasek R, et al. Covariation between workplace physical and psychosocial stressors: evidence and implications for occupational health research and prevention. Ergonomics. 2001;44(7):696–718. doi: 10.1080/00140130119943. [DOI] [PubMed] [Google Scholar]
- MacDonald LA, Cohen A, et al. Occupation as socioeconomic status or environmental exposures: A survey of practice among population-based cardiovascular studies in the United States. Am J Epidem. doi: 10.1093/aje/kwp082. (in press) [DOI] [PubMed] [Google Scholar]
- Mackenbach J, Martikainen P, et al. The shape of the relationship between income and self-assessed health: an international study. Internat J Epid. 2004 doi: 10.1093/ije/dyh338. [DOI] [PubMed] [Google Scholar]
- Mackenbach JP, Stirbu I, et al. Socioeconomic Inequalities in Health in 22 European Countries. N Engl J Med. 2008;358:2468–2483. doi: 10.1056/NEJMsa0707519. [DOI] [PubMed] [Google Scholar]
- Macleod J, Smith GD, et al. Is subjective social status a more important determinant of health than objective social status? Evidence from a prospective observational study of Scottish men. Soc Sci Med. 2005;61:1916–1929. doi: 10.1016/j.socscimed.2005.04.009. [DOI] [PubMed] [Google Scholar]
- Markovitz J, Matthews K, et al. Increases in job strain are associated with incident hypertension in the CARDIA study. Ann Behav Med. 2004;28:4–9. doi: 10.1207/s15324796abm2801_2. [DOI] [PubMed] [Google Scholar]
- Marmot M, Bosma H, et al. Contribution of job control and other risk factors to social variations in coronary heart disease incidence. Lancet. 1997;350:235–239. doi: 10.1016/s0140-6736(97)04244-x. [DOI] [PubMed] [Google Scholar]
- Marmot M, Smith G. Health inequalities among British civil servants: The Whitehall II study. Lancet. 1991;337(8754):1387–1394. doi: 10.1016/0140-6736(91)93068-k. [DOI] [PubMed] [Google Scholar]
- Mathers CD, Schofield DJ. The health consequences of unemployment: The evidence. Med J Australia. 1998;168:178–182. doi: 10.5694/j.1326-5377.1998.tb126776.x. [DOI] [PubMed] [Google Scholar]
- Matthews K, Cottington E, et al. Stressful work conditions and diastolic blood pressure among blue collar factory workers. Am J Epidemiol. 1987;126(2):280–291. doi: 10.1093/aje/126.2.280. [DOI] [PubMed] [Google Scholar]
- Mattiasson I, Lindegarde F, et al. Threat of unemployment and cardiovascular risk factors: Longitudinal study of quality of sleep and serum cholesterol in men threatened with redundancy. Brit Med J. 1990;301:461–466. doi: 10.1136/bmj.301.6750.461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayhew C, Quinlan M. The effects of outsourcing on occupational health and safety: A comparative study of factory-based and outworkers in the Australian clothing industry. Int J Health Serv. 1999;29:83–107. doi: 10.2190/71L1-KRFN-P5QJ-XCNX. [DOI] [PubMed] [Google Scholar]
- McEwen BS, Seeman TE. Protective and damaging effects of mediators of stress. Elaborating and testing the concepts of allostasis and allostatic load. Ann NY Acad Sci. 1999;896:30–47. doi: 10.1111/j.1749-6632.1999.tb08103.x. [DOI] [PubMed] [Google Scholar]
- Mensah FK, Hobcraft J. Childhood deprivation, health and development: associations with adult health in the 1958 and 1970 British prospective birth cohort studies. J Epidem Commun Health. 2008;62:599–606. doi: 10.1136/jech.2007.065706. [DOI] [PubMed] [Google Scholar]
- Merritt M, Bennett G, et al. Low educational attainment, John Henryism, and cardiovascular reactivity to and recovery from personally relevant stress. Psychosom Med. 2004;66(1):49–55. doi: 10.1097/01.psy.0000107909.74904.3d. [DOI] [PubMed] [Google Scholar]
- Messing K, Stellman JM. Sex, gender, and women's occupational health: The importance of considering mechanism. Environ Res. 2006;101:146–162. doi: 10.1016/j.envres.2005.03.015. [DOI] [PubMed] [Google Scholar]
- Meyer J, Muntaner C. Injuries in home health care workers: An analysis of occupational morbidity from a state compensation database. Am J Indust Med. 1999;35:295–301. doi: 10.1002/(sici)1097-0274(199903)35:3<295::aid-ajim10>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- Miller G, Chen E. Unfavorable socioeconomic conditions in early life presage expression of proinflammatory phenotype in adolescence. Psychosom Med. 2007;69(5):402–409. doi: 10.1097/PSY.0b013e318068fcf9. [DOI] [PubMed] [Google Scholar]
- Moller J, Theorell T, et al. Work related stressful life events and the risk of myocardial infarction. Case-control and case-crossover analyses within the Stockholm heart epidemiology program (SHEEP) J Environ Commun Health. 2005;59:23–30. doi: 10.1136/jech.2003.019349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris J. Injury experience of temporary workers in a manufacturing setting: Factors that increase vulnerability. Am Assoc Occup Health Nurses J. 1999;47:470–478. [PubMed] [Google Scholar]
- Nakadate T, Aizawa Y, et al. Change in obstructive pulmonary function as a result of cumulative exposure to welding fumes as determined by magnetopneumonography in Japanese arc welders. Occup Environ Med. 1998;55:673–677. doi: 10.1136/oem.55.10.673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niknian M, Linnan L, et al. Use of population-based data to assess risk factor profiles of blue and white collar workers. J Occup Med. 1991;33(1):29–36. doi: 10.1097/00043764-199101000-00010. [DOI] [PubMed] [Google Scholar]
- Nourjah P, Wagener D, et al. Knowledge of risk factors and risk behaviors related to coronary heart disease among blue and white collar males. J Pub H Pol. 1994;15(4):443–459. [PubMed] [Google Scholar]
- Nylén L, Voss M, et al. Mortality among women and men relative to unemployment, part time work, overtime work, and extra work: a study based on data from the Swedish twin registry. Occup Environ Med. 2001;58:52–57. doi: 10.1136/oem.58.1.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortiz GA, Arguelles AE, et al. Modification of epinephrine, norepinephrine, blood lipd fractions and the cardiovascular system produced by noise in an industrial medium. Horm Res. 1974;5:57–64. doi: 10.1159/000178619. [DOI] [PubMed] [Google Scholar]
- Paffenbarger RSJ, Laughlin ME, et al. Work activity of longshoremen as related to death from coronary heart disease and stroke. New Engl J Med. 1970;282:1109–1114. doi: 10.1056/NEJM197005142822001. [DOI] [PubMed] [Google Scholar]
- Peter R, Siegrist J, et al. Psychosocial work environment and myocardial infarction: improving risk estimation by combining two complementary job stress models in the SHEEP study. J Epidem Commun Health. 2002;56:294–300. doi: 10.1136/jech.56.4.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollack KS, Sorock GS, et al. The association of body mass index and acute traumatic workplace injury in hourly manufacturing workers. AJE. 2007;166:204–211. doi: 10.1093/aje/kwm058. [DOI] [PubMed] [Google Scholar]
- Pope CA, Ezzati M, et al. Fine-particulate air pollution and life expectancy in the United States. New Eng J Med. 2009;360:376–386. doi: 10.1056/NEJMsa0805646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price RH, Burgard SA. The new employment contract and worker health in the Unites States. Making Americans Healthier. In: Schoeni RF, House JS, Kaplan GA, Pollack H, editors. Social and Economic policy as Health Policy. Russle Sage Press; New York: 2008. pp. 201–207. [Google Scholar]
- Punnett L, Bergqvist U. Musculoskeletal disorder in visual display unit work: Gender and work demands. Occup Med State Art Rev. 1999;14(1):113–124. [PubMed] [Google Scholar]
- Quinlan M, Mayhew C, et al. The global expansion of precarious emplyment, work disorganization, and the consequences for occupational health: A review of the recent literature. Int J Health Serv. 2001;31:335–341. doi: 10.2190/607H-TTV0-QCN6-YLT4. [DOI] [PubMed] [Google Scholar]
- Quinn MM, Sembajwe G, et al. Social disparities in the burden of occupational exposures: results of a cross-sectional study. AJIM. 2007;50(12-861-75) doi: 10.1002/ajim.20529. [DOI] [PubMed] [Google Scholar]
- Rabinowitz PM, Slade MD, et al. Trends in the prevalence of hearing loss among young adults entering an industrial workforce 1985–2004. Ear and Hearing. 2006;27(4):369–375. doi: 10.1097/01.aud.0000224125.12338.9a. [DOI] [PubMed] [Google Scholar]
- Ramazzini B. De Morbis Artificum. 1700 doi: 10.2105/ajph.91.9.1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redmond CK, Emes JJ, et al. Mortality of steelworkers employed in hot jobs. J Environ Pathol Toxicol. 1979;2:75–96. [PubMed] [Google Scholar]
- Reed DM, LaCroix AZ, et al. Occupational strain and the incidence of coronary heart disease. Am J Epid. 1989;129:495–502. doi: 10.1093/oxfordjournals.aje.a115160. [DOI] [PubMed] [Google Scholar]
- Rehkopf DH, Kuper H, et al. Discrepancy between objective and subjective measures of job stress and sickness absence. doi: 10.5271/sjweh.3081. (under review) [DOI] [PubMed] [Google Scholar]
- Reid DD, Brett GZ, et al. Cardiorespiratory disease and diabetes among middle aged civil servants. Lancet. 1974;7856:469–73. doi: 10.1016/s0140-6736(74)92783-4. [DOI] [PubMed] [Google Scholar]
- Roberts H, Pearson JCG, et al. Unemployment and health: The quality of social support among residents in the Trent region of England. J Epidem Commun Health. 1997;51:41–45. doi: 10.1136/jech.51.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenstock L, Cullen MR, et al. Textbook of Clinical Occupational and Environmental Medicine. Elsevier, Ltd; W.B.Saunders; Philadelphia: London: 2005. [Google Scholar]
- Ruhm CJ. Good times make you sick. J Health Econ. 2003;22:637–658. doi: 10.1016/S0167-6296(03)00041-9. [DOI] [PubMed] [Google Scholar]
- Ruhm CJ. Healthy living in hard times. J Health Econ. 2005;24:341–363. doi: 10.1016/j.jhealeco.2004.09.007. [DOI] [PubMed] [Google Scholar]
- Rushton L, Hutchings S, et al. The burden of cancer at work: estimation as the first step to prevention. Occup Environ Med. 2008;65:789–800. doi: 10.1136/oem.2007.037002. [DOI] [PubMed] [Google Scholar]
- Salminen S, Saari J, et al. Risk factors for women in serious occupational accidents. Occup Health Safety (Australia New Zealand) 1992;8(4):341–347. [Google Scholar]
- Schaufelberger M, Rosengren A. Heart failure in different occupational classes in Sweden. Eur Heart J. 2007;28:212–218. doi: 10.1093/eurheartj/ehl435. [DOI] [PubMed] [Google Scholar]
- Seixas NS, Roins TG, et al. Longitudinal and cross-sectional analyses of coal mine dust and pulmonary function in new miners. Brit J INdust Med. 1993;50:929–937. doi: 10.1136/oem.50.10.929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegrist J. Adverse health effects of high-effort/low-reward conditions. J Occup Health Psychol. 1996;1:27–41. doi: 10.1037//1076-8998.1.1.27. [DOI] [PubMed] [Google Scholar]
- Silverstein B. Claims incidence of work-related disorders of the upper extremities: Washington state 1987 through 1995. Am J Public Health. 1998;88:1827–1833. doi: 10.2105/ajph.88.12.1827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverstein BA, Fine LJ, et al. Hand wrist cumulative trauma disorders in industry. Br J Ind Med. 1986;43:779–784. doi: 10.1136/oem.43.11.779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Social Security Administration 2008.
- Soderfeldt B, Soderfeldt M, et al. Does organization matter? A multilevel analysis of the demand-control model applied to human services. Soc Sci Med. 1997;44(4):527–534. doi: 10.1016/s0277-9536(96)00179-7. [DOI] [PubMed] [Google Scholar]
- Sparacino J, Ronchi D, et al. Blood pressure of municipal employees: effects of job status and worksite. Perception and Motor Skills. 1982;55(2):563–578. doi: 10.2466/pms.1982.55.2.563. [DOI] [PubMed] [Google Scholar]
- Statistics Canada Labour force 15 years and over by detailed occupation. 2001 [Google Scholar]
- Steptoe A, Willemsen G. The influence of low job control on ambulatory blood pressure and perceived stress over the working day in man and women from the Whitehall II cohort. J Hypertens. 2004;22(5):915–20. doi: 10.1097/00004872-200405000-00012. [DOI] [PubMed] [Google Scholar]
- Stevens G, Cho JH. Socioeconomic indexes and the new 1980 census occupational classification scheme. Soc Sci Res. 1985;14:142–168. [Google Scholar]
- Stevenson JM, Greenhorn DR, et al. Selection test fairness and the incremental lifting machine. Appl Ergon. 1996;27:45–52. doi: 10.1016/0003-6870(95)00053-4. [DOI] [PubMed] [Google Scholar]
- Stone PW, Gershon RR. Nurse work environments and occupational safety in intensive care units. Policy Polit Nurs Pract. 2006;7(4):240–247. doi: 10.1177/1527154406297896. [DOI] [PubMed] [Google Scholar]
- Suruda A, Wallace DF. Fatal work-related injuries in the US chemical industry 1984–89. Int. Arch. Occup. Environ. Health. 1996;68:425–428. doi: 10.1007/BF00377864. [DOI] [PubMed] [Google Scholar]
- Tenkanen L, Sjoblom T, et al. Shift work, occupation and coronary heart disease over six years of follow-up in the Helsinki Heart Study. Scand Work Environ Health. 1997;23:257–265. doi: 10.5271/sjweh.218. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Housing and Urban Development 2006.
- United States Department of Labor 2002 http://www.dol.gov.
- Van Kampen V, Merget R, et al. Occupational airway sensitizers: an overview of the respective literature. Am J Indus Med. 2000;38:164–218. doi: 10.1002/1097-0274(200008)38:2<164::aid-ajim7>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- Virtanen P, Vahtera J, et al. Employment trajectory as determinant of change in health-related lifestyle: the prospective HeSSup study. Eur J Pub Health. 2008;18:504–508. doi: 10.1093/eurpub/ckn037. [DOI] [PubMed] [Google Scholar]
- Voss M, Nylen L, et al. Unemployment and early cause-specific mortality: A study based on the Swedish twin registry. Am J Pub Health. 2004;94:2155–2161. doi: 10.2105/ajph.94.12.2155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warren J, Hoonaker P, et al. Job characteristics as mediators in SES-health relationships. Soc Sci Med. 2004;59:1367–1378. doi: 10.1016/j.socscimed.2004.01.035. [DOI] [PubMed] [Google Scholar]
- Wild P, Moulin JJ, et al. Mortality from cardiovascular diseases among potash workers exposed to heat. Epidemiol. 1995;6:243–247. doi: 10.1097/00001648-199505000-00009. [DOI] [PubMed] [Google Scholar]
- Wilkins K, Mackenzie S. Work injuries. Health Report. 2007;18(3):25–42. [PubMed] [Google Scholar]
- Winkleby MA, Ragland DR, et al. Excess risk of sickness and disease in bus drivers: a review and synthesis of epidemiological studies. Int J Epidemiol. 1988;17:255–262. doi: 10.1093/ije/17.2.255. [DOI] [PubMed] [Google Scholar]
- Wizemann TM, Pardue ML. Exploring the biological contributions to human health: Does sex matter? National Academy Press; Washington DC: 2001. [PubMed] [Google Scholar]
- Xu X, Christiani DC, et al. Exposure-response relationships between occupational exposures and chronic respiratory illness: a community based study. Am Rev Resp Dis. 1992;146:413–418. doi: 10.1164/ajrccm/146.2.413. [DOI] [PubMed] [Google Scholar]