Abstract
This study measured reading workstation monitors and the viewing environment currently available within BreastScreen New South Wales (BSNSW) centres to determine levels of adherence to national and international guidelines. Thirteen workstations from four BSNSW service centres were assessed using the American Association of Physicists in Medicine Task Group 18 Quality Control test pattern. Reading workstation monitor performance and ambient light levels when interpreting screening mammographic images were assessed using spectroradiometer CS-2000 and chroma meter CL-200. Overall, radiologic monitors within BSNSW were operating at good acceptable levels. Some non-adherence to published guidelines included the percentage difference in maximum luminance between pairs of primary monitors at individual workstations (61.5 % or 30.8 % of workstations depending on specific guidelines), maximum luminance (23.1 % of workstations), luminance non-uniformity (11.5 % of workstations) and minimum luminance (3.8 % of workstations). A number of ambient light measurements did not comply with the only available evidence-based guideline relevant to the methodology used in this study. Larger ambient light variations across sites are shown when monitors were switched off, suggesting that differences in ambient lighting between sites can be masked when a standard mammogram is displayed for photometric measurements. Overall, BSNSW demonstrated good adherence to available guidelines, although some non-compliance has been shown. Recently updated United Kingdom and Australian guidelines should help reduce confusion generated by the plethora and sometimes dated nature of currently available recommendations.
Keywords: Mammography, Monitor performance, Ambient light, BreastScreen, 5 M-pixel monitor
Introduction
Imaging modalities require high-quality electronic display devices to convey precise and accurate information for diagnostic interpretation, clinical review, consultation or guidance during surgical procedures. Suboptimal or inconsistent performance of reading workstation monitors can prolong viewing times, increase reader fatigue, reduce detection of abnormalities and affect diagnostic performance [1–5]. Good displays are of particular importance in the interpretation of mammograms where subtle malignancies demonstrate little grey level difference from normal breast tissues [6], and whilst much emphasis is placed on innovations that maximise pathology visualisation, the effectiveness of these developments rely on high-quality image presentation.
The electronic era has introduced many benefits to medical imaging such as rapid access to images at sites remote from acquisition, through the use of picture archiving and communication system (PACS) and other network systems [7]. With this wide access, however, certain challenges are presented including ensuring that images, wherever they are reported, are displayed at consistently high quality and that the luminance limitations of widely available monitors (as compared with the traditional transilluminators) do not compromise diagnostic efficacy. These quality issues not only rely on the display but also dictate that the viewing environment, in particular, ambient lighting is set so that visual adaptation and perception is promoted [8–14].
The importance of these above-mentioned features is well acknowledged within the Australian BreastScreen network where state of the art display devices are evident within locations that are designed for dedicated mammographic reading. However, monitor performance and viewing condition can change over time, and without appropriate quality assurance (QA) procedures in place, reduction in performance may be noted, regardless of manufacturer specifications. The Australasian College of Physical Scientists and Engineers in Medicine (ACPSEM) has recently published an excellent position paper on digital mammography QA [15], within which various recommendation levels similar to the UK National Health Service Breast Screening Programme (NHSBSP) equipment report 0604 [16] are shown (Table 1). However, the largest challenge lies in the lack of scientific publications upon which to base the available recommendations. Therefore, the purpose of this study was to explore if monitors and viewing environment currently available within BreastScreen New South Wales (BSNSW) centres are operating at consistent levels and adhere to guidelines available within national and international literature.
Table 1.
Summary of recommended QA schedule for LCD monitors
| Daily | Weekly/monthly/quarterly/half-yearly | Annually | |
|---|---|---|---|
| BSNSW [17] | Monitor cleanliness | Weekly | |
| Monitor cleanliness, overall visual assessment including artefact and contrast resolution | |||
| AAPM [18] | Overall visual assessment | Monthly for the first quarter of operation and subsequently on a quarterly basis if the system is proven to be stable. | Reflections, luminance measures, resolution, noise, veiling glare, chromaticity |
| Reflections, luminance measures, resolution | |||
| EIZO [19] | Overall visual assessment | Every 3–6 months | |
| Luminance measures, greyscale | |||
| BARCO [20] | Manual: monitor cleanliness | Weekly | Overall visual assessment |
| Manual: image quality | |||
| Inbuilt software: automatic I–guard check, calibration setting, measure display white, display test, mammo-compliance test | |||
| Monthly | |||
| Inbuilt software: measure quality level, compliance test | |||
| NHSBSP [16] | Luminance measures, visual assessment including resolution, artefact, overall imaging performance | ||
| EUREF [21] | Visual assessment including contrast visibility, artefacts | Half-yearly | |
| Resolution, luminance measures, greyscale display function | |||
| ACPSEM [15] | Weekly | Luminance measures, overall visual assessment including artefact and resolution | |
| Monitor cleanliness, overall visual assessment including artefact and resolution | |||
| ACRIN DMIST [22] | Monitor cleanliness | Weekly | Luminance measures, display quality, resolution |
| Overall visual assessment including contrast visibility |
BSNSW BreastScreen NSW, AAPM American Association of Physicists in Medicine, NHSBSP National Health Service Breast Screening Programme, EUREF European Reference Organisation for Quality Assured Breast Screening and Diagnostic Services, ACPSEM Australasian College of Physical Scientists and Engineers in Medicine, ACRIN DMIST American College of Radiology Imaging Network Digital Mammographic Imaging Screening Trial
Methods and Materials
Thirteen workstations (nine pairs of Eizo Radiforce GS520 and four pairs of Barco MFGD-5621 HD; Table 2) from four BSNSW service centres (referred to as A, B, C and D) were assessed in this study by the same radiographer between the period of October 2011 and March 2012. The sample assessed in this study, whilst not necessarily representative, provides a preliminary overview of the entire BSNSW network which consists of a total of 37 workstations and 35 BSNSW service centres. The reporting monitor performance and ambient light levels used for interpreting screening mammographic images were measured. Each workstation comprised of a pair of 5 M-pixels primary reporting monitors, and each was warmed-up for at least 30 min before any measurements were taken to allow the monitor output to stabilise [26]. Details of the date of assessment, date of monitor manufacture, most recent QA performed, as well as results and actions taken by the physicist based on the most recent QA are outlined in Table 3.
Table 2.
Information and specifications of monitors in four BSNSW service centres
| Monitor information | Service centres | |||
|---|---|---|---|---|
| A | B | C | D | |
| Number of reading workstations | 3 | 1 | 5 | 4 |
| Monitor type and model | Eizo Radiforce GS520 | Eizo Radiforce GS520 | Eizo Radiforce GS520 | Barco MFGD-5621 HD |
| Screen size (cm) | 54 | 54 | 54 | 54 |
| Display resolution | 2,048 × 2,560 | 2,048 × 2,560 | 2,048 × 2,560 | 2,048 × 2,560 |
| Screen type | Monochrome LCD | Monochrome LCD | Monochrome LCD | Monochrome LCD |
| Maximum luminance (cd/m2) | 700 | 700 | 700 | 800 |
| Maximum contrast ratio | 800:1 | 800:1 | 800:1 | 900:1 without PPUa 700:1 with PPUa |
| Self-calibrating | No | No | No | Yes (I-guard technology) |
Table 3.
Details of the date of assessment, date of monitor manufacture, most recent QA performed as well as result and action taken by the physicist based on the most recent QA
| Location and workstation | Date of assessment (current study) | Date of monitor manufacture | Most recent QA performed by physicist | Result/action taken by physicist based on the most recent QA |
|---|---|---|---|---|
| A1 | 16/3/2012 | 1/11/2008 | 21/9/2011 | Fail on Lmax matching between two primary monitors due to wrong setting selected (CAL instead of DICOM); settings adjusted and locked |
| A2 | 16/3/2012 | 1/11/2008 | 21/9/2011 | Pass |
| A3 | 16/3/2012 | 1/10/2008 | – | – |
| B1 | 21/10/2011 | 19/5/2009 | – | – |
| C1 | 9/3/2012 | 1/8/2008 | 6/12/2011 | Pass |
| C2 | 9/3/2012 | 12/6/2008 | 6/12/2011 | Fail on Lmax of right monitor; recalibrated by Eizo |
| C3 | 9/3/2012 | 5/10/2010 | 6/12/2011 | Fail on Lmax matching between two primary monitor; recalibrated by Eizo |
| C4 | 9/3/2012 | 18/3/2009 | 6/12/2011 | Pass |
| C5 | 9/3/2012 | 1/2/2011 | 6/12/2011 | Pass |
| D1 | 16/3/2012 | 1/7/2006 | 16/8/2012 | Pass |
| D2 | 16/3/2012 | 1/12/2007 | 11/2/2010 | Pass |
| D3 | 16/3/2012 | 1/12/2008 | 11/2/2010 | Lmax matching failed; Barco informed |
| D4 | 16/3/2012 | 1/1/2009 | 11/2/2010 | Pass |
CAL calibration, DICOM Digital Imaging and Communications in Medicine, en dash indicates information not available
Measurement of Monitors
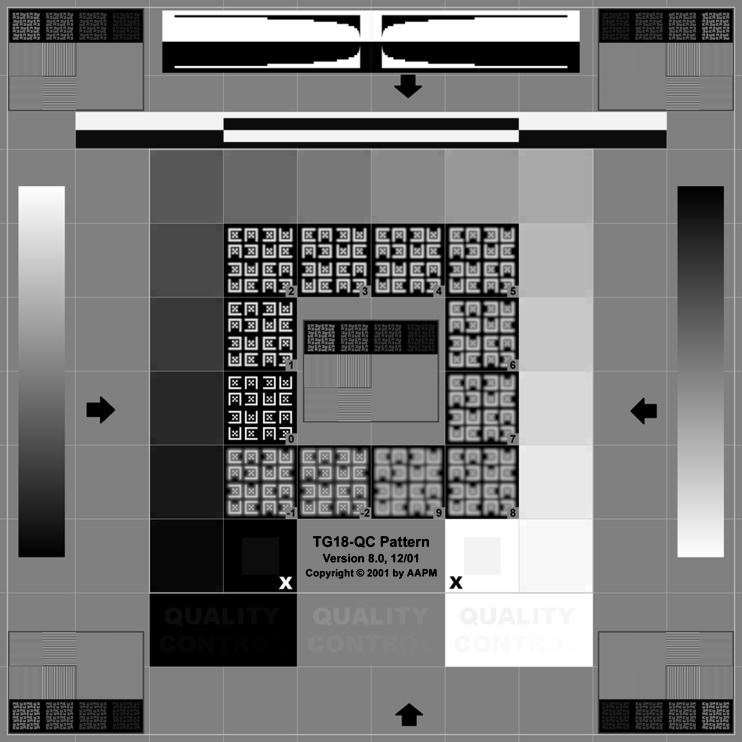
The American Association of Physicists in Medicine (AAPM) Task Group 18 Quality Control (TG18-QC) test pattern (Fig. 1), available in the PACS (Sectra Imtec AB, Sweden) and accessed from all investigated workstations, was used to assess monitor performance [18].
Fig. 1.
AAPM TG18-QC test pattern [18]. Maximum luminance and minimum luminance measured over region denoted by black “X” and white “X”, respectively. Luminance non-uniformity was assessed over areas identified by arrows
A spectroradiometer CS-2000 (Konica Minolta, Japan) was used to measure luminance in candela per metres squared (cd/m2) [27]. All measurements were taken using a 0.2° aperture with the front edge of the metal lens barrel at a distance of 50 cm from the display monitor [27]. Measurements were taken for the left (L) and right (R) reporting monitor with all room lighting switched off. All investigated parameters were measured four times, and a mean value was calculated.
The following parameters were assessed:
Luminance response
Luminance response refers to “the relationship between displayed luminance and the input values of a standardized display system” [18] and is comprised of several components including: maximum luminance (Lmax), minimum luminance (Lmin), contrast ratio, Just-Noticeable-Difference (JND), percentage difference between two primary monitors, and luminance non-uniformity.
Lmax, Lmin, and Contrast ratio
Lmax is the highest and Lmin the lowest luminance level measured at the 100 % and 0 % regions on the TG18-QC pattern denoted by black “X” and white “X”, respectively (Fig. 1).
Contrast ratio, describing the ratio of maximum and minimum luminance, was calculated for each monitor (L and R) using the following formula [18]:
 |
-
b.
JND
A JND is defined as the difference in luminance of a target that the average human observer can perceive under a given viewing condition [28]. The Lmax and Lmin of each monitor were mapped to the JND index which converts the luminance values to JND integers, and the achievable JNDs of each monitor was subsequently obtained with the difference between the JND integers of Lmax and Lmin [28].
-
c.
Maximum luminance difference between two primary monitors in each workstation
Percentages difference between the maximum luminance of the two primary reporting monitors at each workstation was calculated using the following formula:
 |
-
d.
Luminance non-uniformity
This refers to the maximum deviation of luminance across a monitor displaying a uniform pattern [18]. Luminance non-uniformity was assessed by comparing the luminance of four regions on the monitor screen (see arrows in Fig. 1) and expressed as a percentage using the following formula [18]:
 |
where Lmax and Lmin in this instance is the maximum brightness value and lowest brightness value respectively amongst the four regions assessed.
-
2.
Measurement of spatial resolution
This refers to the ability of a monitor to display and separate small details, and a visual evaluation approach was taken for this assessment. The Cx patterns on four regions of the TG18-QC pattern was assessed and given a score through the comparison of its appearance with the scale at the test pattern centre, with a score of 0 being most desirable and 4 being the maximum limit before the monitor would be deemed unacceptable [18].
Measurement of Ambient Lighting
Ambient lighting of each screen reading workstation was measured using a chroma meter (Konica Minolta, Japan) at a typical reading distance of 70 cm from the monitor under normal working conditions with the monitor either displaying a standard mammogram or switched off. As all workstations assessed in this study have an integrated lighting system (Planilux® Eltrono, Germany) which allows adjustment to ambient light level as well as a sensor-controlled automatic light function that varies light level depending on brightness of the reporting monitors, measurements were made under four different desk light levels: automatic, brightest, dimmest, and switched off.
Results
An evaluation of data produced in this study was made with reference to currently available guidelines [12, 13, 15, 16, 18, 21, 22, 29] as shown in Tables 4 and 5.
Table 4.
Measured values from 13 pairs of monitors in four BSNSW service centres
| Measurement of luminance response | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Lmax (cd/m2) | Lmin (cd/m2) | Contrast ratio | Just-noticeable-difference (JND) | Percentage difference between two primary monitors (%) | Luminance non-uniformity (%) | ||||||
| Location and workstation | Left | Right | Left | Right | Left | Right | Left | Right | Between Lmax of both monitorsa | Left | Right |
| A1 | 424.63 | 462.00 | 1.19 | 1.19 | 356.98 | 387.34 | 603 | 616 | 8.09 [R] | 13.14 | 20.50 |
| A2 | 497.50 | 476.53 | 1.18 | 1.22 | 423.40 | 391.96 | 627 | 620 | 4.22 [L] | 10.41 | 7.33 |
| A3 | 425.00 | 453.95 | 1.22 | 1.24 | 347.44 | 365.79 | 599 | 608 | 6.38 [R] | 19.21 | 9.13 |
| B1 | 442.03 | 534.00 | 1.19 | 1.30 | 372.70 | 411.24 | 611 | 632 | 17.22 [R] | 23.08 | 24.35 |
| C1 | 481.43 | 485.55 | 1.14 | 1.20 | 421.38 | 403.28 | 623 | 624 | 0.85 [R] | 8.27 | 10.46 |
| C2 | 431.83 | 385.78 | 1.21 | 1.22 | 356.59 | 316.79 | 607 | 588 | 10.66 [L] | 16.66 | 25.11 |
| C3 | 469.53 | 479.60 | 1.52 | 1.16 | 309.36 | 412.47 | 607 | 620 | 2.10 [R] | 10.61 | 17.74 |
| C4 | 516.15 | 469.58 | 1.39 | 1.30 | 371.53 | 360.59 | 623 | 616 | 9.02 [L] | 20.08 | 20.38 |
| C5 | 491.18 | 470.08 | 1.19 | 1.12 | 411.97 | 420.93 | 627 | 620 | 4.30 [L] | 16.68 | 19.31 |
| D1 | 490.20 | 470.10 | 1.01 | 0.91 | 483.67 | 515.45 | 627 | 632 | 4.10 [L] | 37.75 | 24.39 |
| D2 | 499.00 | 442.40 | 1.05 | 1.02 | 475.58 | 434.79 | 631 | 612 | 11.34 [L] | 31.61 | 31.99 |
| D3 | 574.75 | 535.05 | 1.36 | 1.19 | 423.62 | 451.52 | 639 | 640 | 6.91 [L] | 21.75 | 21.41 |
| D4 | 541.98 | 480.25 | 1.17 | 1.08 | 465.21 | 444.78 | 639 | 624 | 11.39 [L] | 22.33 | 11.71 |
| Mean | 483.48 | 472.68 | 1.22 | 1.17 | 401.49 | 409.00 | 620.23 | 619.38 | 7.43 | 19.35 | 18.75 |
| Max/min ratio | 1.35 | 1.39 | 1.50 | 1.43 | 1.56 | 1.63 | 1.07 | 1.05 | 20.26 | 4.56 | 4.36 |
| Current guidelines | ≥170 [18] | ≤1.5 [16] | ≥250 [18,21] | b | ≤5 % [15,16,21,29] | ≤30 % [15,16,18,21] | |||||
| ≥450 [15,16] | ≥300 [16] | ≤10 % [18] | |||||||||
Independent values for left and right monitors are presented for Lmax, Lmin, contrast ratio, JND and luminance non-uniformity. Current guidelines indicated in table for LCD monitors. Brackets indicate reference for the specific guideline
aMonitor with greater Lmax value indicated by left [L] or right [R]
bNo available guideline
Table 5.
Ambient light levels of 13 workstations in four BSNSW service centres
| Workstation | Standard mammographic image displayed on monitor | Monitor switched off | ||||||
|---|---|---|---|---|---|---|---|---|
| Workstation desk lighting (lux) | Workstation desk lighting (lux) | |||||||
| Auto | Brightest | Dimmest | Off | Auto | Brightest | Dimmest | Off | |
| A1 | 11.10 | 39.65 | 10.33 | 10.05 | 3.05 | 36.63 | 1.70 | 1.33 |
| A2 | 14.40 | 53.50 | 13.33 | 10.90 | 3.75 | 42.43 | 2.55 | 1.73 |
| A3 | 41.13 | 55.48 | 12.08 | 11.93 | 35.10 | 41.35 | 3.80 | 2.85 |
| B1 | 28.95 | 73.23 | 18.25 | 18.10 | 12.18 | 61.15 | 10.33 | 9.55 |
| C1 | 27.53 | 58.13 | 10.90 | 9.78 | 7.78 | 47.15 | 4.95 | 0.60 |
| C2 | 20.18 | 51.78 | 13.13 | 13.05 | 35.09 | 44.85 | 4.37 | 3.43 |
| C3 | 13.98 | 30.95 | 11.68 | 9.03 | 3.69 | 29.17 | 2.53 | 1.75 |
| C4 | 13.85 | 41.98 | 12.38 | 12.08 | 4.90 | 32.63 | 3.88 | 2.93 |
| C5 | 19.65 | 41.08 | 18.15 | 15.34 | 10.09 | 36.48 | 9.15 | 8.95 |
| D1 | 10.38 | 43.73 | 9.65 | 9.25 | 4.20 | 34.40 | 2.90 | 2.38 |
| D2 | 10.10 | 46.40 | 10.05 | 9.53 | 3.53 | 36.48 | 3.00 | 2.70 |
| D3 | 11.75 | 43.83 | 11.28 | 10.40 | 3.23 | 38.00 | 2.43 | 1.88 |
| D4 | 18.75 | 44.19 | 10.58 | 9.75 | 12.08 | 37.95 | 2.55 | 2.18 |
| Median | 14.40 | 44.19 | 11.68 | 10.40 | 4.90 | 37.95 | 3.00 | 2.38 |
| Max/min ratio | 3.70 | 2.37 | 1.89 | 1.96 | 11.51 | 2.10 | 6.07 | 15.92 |
| Current guidelines | 2–10 [18]; <10 [16a,21,22]; <20 [15]; 25–40 [12,13] | |||||||
aGuideline depends on reflection characteristics. Brackets indicate reference for the specific guideline
Measurement of Luminance Response
Values describing luminance response of each monitor assessed in this study are demonstrated in Table 4 with the mean and maximum/minimum ratios along with current guidelines [15, 16, 18, 21, 29].
Whilst 20 out of 26 tested monitors shown good compliance to even the strictest available guidelines [15, 16], six monitors did not provide sufficient maximum luminance as indicated by recommendation published by ACPSEM [15] and NHSBSP [16]. In addition, one out of 26 tested monitors had an excessive minimum luminance, and three out of 26 monitors failed to comply with the luminance non-uniformity recommendation [15, 16, 18, 21]. The percentage difference between primary monitors at individual workstations was above recommended levels in eight out of the 13 workstations setups when reference was made to several standards published [15, 16, 21, 29] and four out of the 13 workstations according to AAPM guidelines [18].
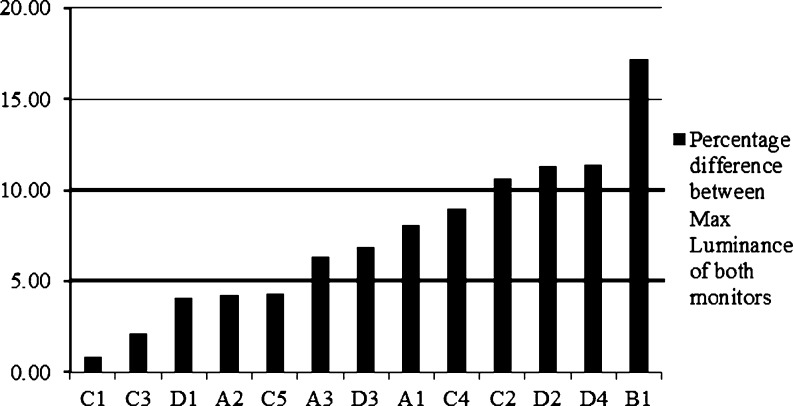
Although all other tested monitors demonstrated compliance to current guidelines (wherever available), some variations across monitors were observed for all parameters measured, with the largest demonstrated for percentage difference between monitors (at each workstation as described above) and luminance non-uniformity with maximum/minimum ratio of 20.3 and 4.6, respectively (Table 4 and Fig. 2).
Fig. 2.
Percentage difference between coupled primary monitors from 13 workstations. Horizontal bolded reference lines indicate the 5 % and 10 % luminance response limit between two primary monitors
Measurement of Spatial Resolution
Spatial resolution of all workstations reached the highest achievable score (Cx = 0) within the standards given by AAPM [18].
Measurement of Ambient Lighting
Variations were demonstrated amongst workstations with 86.5 % of the ambient light measurements not complying with the only available evidence-based guideline for our methodology (albeit for a different type of examination) of 25–40 lx [12, 13], with 81.1 % of these non-adherent values being lower than the stated range (Table 5). The measurements demonstrated a lower level of variation when a standard mammogram was displayed (maximum/minimum ratio 1.89–3.7) as opposed to when it was switched off (maximum/minimum ratio 2.1–15.92).
Discussion
Poor performance of reporting monitors can affect radiologic interpretation [30], therefore acceptance procedures must be rigorous, and with regular quality assurance tests carried out to ensure optimal display. This is particularly relevant in breast imaging where small changes in the brightness characteristics of a display may have a significant impact on the visibility of a subtle lesion in a dense region of the breast or on the contrast required to identify an asymmetric density [31]. In the current work, whilst it was reassuring that most tested monitors demonstrated adherence to current guidelines (wherever available), some inconsistent features were observed, most notably the luminance difference between primary monitors positioned at the same workstation.
According to the current guidelines [15, 16, 18, 21, 29], it is recommended that the percentage difference between two primary monitors at the same workstation should not exceed 5 % [15, 16, 21, 29] or 10 % [18]. However, results from the current study demonstrate that 61.5 % (when reference made to UK and Australian guidelines [15, 16]) or 30.8 % (when referring to AAPM guidelines [18]) of the workstations assessed did not provide a sufficiently consistent luminance response between adjacent displays. In mammography where careful and precise diagnostic interpretation requires a constant comparison between the radiographic images of both breasts as well as between current and prior mammographic images, luminance discrepancies of up to 17 % between monitors appears sizeable. In addition, some tested monitors failed to demonstrate compliance for maximum luminance (23.1 % when reference made to 450 lx), luminance non-uniformity (11.5 %) and minimum luminance (3.8 %) guidelines [15, 16, 18, 21]. It is interesting to note that amongst the tested monitors, the oldest monitors (D1 and D2) were the ones demonstrating non-adherence to the luminance non-uniformity guidelines (Tables 3 and 4), which had otherwise shown compliance to the majority of the remaining parameters. Whilst all other tested monitors adhered to the available guidelines, some variations between maximum and minimum values were recorded across monitors for all parameters measured, particularly for the aforementioned percentage differences as well as luminance non-uniformity (maximum/minimum ratio 4.56). The impact of variations similar to that described here remains unclear and further work is required to evaluate the clinical relevance.
In addition to the performance of reporting monitors, previous literature has also shown that inappropriate ambient lighting under which radiologic images are interpreted affects diagnostic performance [4, 9, 10, 13]. Bright lighting affects visualization of normal and abnormal structures on radiologic images [8–11] through increased monitor reflection, resulting in higher luminance in dark areas of the images [14] and thus lower contrast ratios. At the opposite end, low levels of ambient lighting can cause visual adaptation difficulties between brighter monitor surface and darker surroundings [32]. Visual acuity is highest at the level of light to which the eyes are adapted, and if ambient lighting is too low, then the eye will adapt to a level below the brightness of the image since the visual field is substantially larger than the image display [33]. Whilst this concept is well proven, this is rarely considered by clinicians and authors of guidelines and is not considered in the recent UK and ACPSEM guidelines [15, 16]. The 81.1 % of non-adherent values which are lower than the evidence-based guideline of 25–40 lx (using our methodological approach) [12, 13], may be an affirmation to this although this guideline is based on orthopaedic images. It should be acknowledged, however, that applying the mammographic-specific guidelines of 2–10 lx [18], less than 10 lx [16, 21, 22] and less than 20 lx [15] could significantly change the interpretation of ambient light results; however, without clear instruction on methodology approaches supporting a number of the existing recommendations, it is sometimes difficult to state which values in Table 5 should be used. The importance of having a standardised methodological approach to ambient light measurements as described in the UK NHSBSP equipment report 0604 [16] is shown by the large variations across sites, particularly when the monitors were switched off, suggesting that differences in ambient lighting between sites can be masked when a standard mammogram is displayed for photometric measurements.
The aim of regular high-quality QA programs is to ensure optimal monitor and ambient light conditions in the reporting environment and reduce performance discrepancies between centres. Whilst results obtained from the sites assessed in this study do not provide any evidence of non-adherence to the BSNSW QA guideline (Table 1), it only included weekly QA on monitor cleanliness and overall visual assessment, and therefore, it is recommended for measurements of luminance response (as assessed in Table 4) to be built into the BSNSW QA schedule and performed at least once a year to ensure the adherence to other existing recommendations [15, 16, 18, 21, 29]. National and international recommendations however for QA scheduling are inconsistent as can be seen from the guidelines issued by bodies across the US, Europe, UK and Australia (Table 1). These variations in guidelines may at least in part contribute to some of the non-adherence and variations reported in this work. In addition, even when our values demonstrated good adherence for a variety of parameters for the majority of tested monitors such as Lmax, Lmin, contrast ratio and luminance non-uniformity, the relevance of some available recommendations to modern technology is unclear. AAPM guidelines [18] were last revised in 2005, and the minimum recommendation for maximum luminance for example appears to be quite low for current monitors, the capabilities of which have advanced substantially over the last 7 years. This issue is well addressed by two latest publications in the UK and Australia [15, 16]; however, the importance of regular updating of recommendations to reflect technological advancements is emphasised.
Previously, there has been no published review of monitor standards in BSNSW, and therefore, the information provided in this work would be useful as it demonstrated gross acceptability and areas that require further improvement. Similarly, the authors of this study would encourage other workers to publish findings obtained from their QA data in order to improve existing knowledge as well as to increase the number of papers from which recommendations could be made. Whilst all parameters assessed in this work were found to be important, the appropriateness of tolerances set in guidelines is worth considering, especially for the 5 % limit in place between two primary monitors at the same workstation [15, 16, 21, 29]. Whilst the tolerance limit is achievable, there should be a balance between what is achievable on a system and what actually makes a difference in clinical practice. Therefore, further work should be performed to assess the level of difference between monitors at the same workstation to determine the actual difference that would actually affect radiologists’ ability to detect breast abnormalities. In addition, further work should also be done to assess how long before reporting monitors go out of calibration so that the appropriateness of existing QA schedules may be revisited.
It should be acknowledged that the three main limitations to this work relate to the fact that firstly, the full range of QA tests recommended for LCD monitors were unable to be performed due to the lack of resources such as unavailability of other dedicated TG18 test patterns and specialized equipment. Secondly, equipment used in this study (spectroradiometer and chroma meter) is not commonly available, and therefore results from this study may be difficult to replicate in future studies. Lastly, it is not known whether monitors assessed in this study were in calibration at the most recent QA due to unavailability of information, or whether it was even in calibration at installation since medical physicists were only employed in BSNSW after December 2009.
Conclusion
This work has demonstrated that, for the majority of tested monitors, the Breast Screen service in New South Wales demonstrated good adherence to available guidelines, although some non-compliance has been shown. Recent published guideline documents in the UK and Australia will contribute importantly to the optimisation of radiologic viewing conditions.
Acknowledgement
We would like to thank all the BreastScreen NSW screening centres who took part in this study and members of staff who helped facilitate all measurement processes.
References
- 1.Herron JM, Bender TM, Campbell WL, Sumkin JH, Rockette HE, Gur D. Effects of luminance and resolution on observer performance with chest radiographs. Radiology. 2000;215:169–174. doi: 10.1148/radiology.215.1.r00ap34169. [DOI] [PubMed] [Google Scholar]
- 2.Krupinski E, Roehrig H, Furukawa T. Influence of film and monitor display luminance on observer performance and visual search. Acad Radiol. 1999;6:411–418. doi: 10.1016/S1076-6332(99)80191-3. [DOI] [PubMed] [Google Scholar]
- 3.Hidano S, Ikeda M, Ishigaki T, Usami H, Shimamoto K, Kato K. Effects of monitor luminance change on observer detection performance. Comput Med Imaging Graph. 2005;29:35–41. doi: 10.1016/j.compmedimag.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 4.Dreyer KJ, Mehta A, Thrall JH. PACS: a guide to digital revolution. 1. New York: Springer; 2002. [Google Scholar]
- 5.Siegel E, Reiner B. Radiology reading room design: the next generation. Appl Radiol. 2002;4:11–16. [Google Scholar]
- 6.Mello-Thoms C, Hardesty L, Sumkin J, Ganott M, Hakim C, Britton C, Stalder J, Maitz G. Effects of lesion conspicuity on visual search in mammogram reading. Acad Radiol. 2005;12:830–840. doi: 10.1016/j.acra.2005.03.068. [DOI] [PubMed] [Google Scholar]
- 7.Hayt DB, Alexander S, Drakakis J, Berdebes N. Filmless in 60 days: the impact of picture archiving and communications systems within a large urban hospital. J Digit Imaging. 2001;14:62–71. doi: 10.1007/s10278-001-0004-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Balter S. A preliminary investigation of ambient light in the interventional fluoroscopy laboratory. Proc SPIE. 2005;5749:348. doi: 10.1117/12.593701. [DOI] [Google Scholar]
- 9.Fuchsjager MH, Schaefer-Prokop CM, Eisenhuber E, Homolka P, Weber M, Funovics MA, Prokop M. Impact of ambient light and window settings on the detectability of catheters on soft-copy display of chest radiographs at bedside. AJR Am J Roentgenol. 2003;181:1415–1421. doi: 10.2214/ajr.181.5.1811415. [DOI] [PubMed] [Google Scholar]
- 10.Goo JM, Choi JY, Im JG, Lee HJ, Chung MJ, Han D, Park SH, Kim JH, Nam SH. Effects of monitor luminance and ambient light on observer performance in soft-copy reading of digital chest radiographs. Radiology. 2004;232:762–766. doi: 10.1148/radiol.2323030628. [DOI] [PubMed] [Google Scholar]
- 11.Kimme-Smith C, Haus AG, DeBrehl N, Bassett LW. Effects of ambient light and view box luminance on the detection of calcifications in mammography. AJR Am J Roentgenol. 1997;168:775–778. doi: 10.2214/ajr.168.3.9057533. [DOI] [PubMed] [Google Scholar]
- 12.McEntee M, Brennan P, Evanoff M, Philips P, O Connor WT, Manning D. Optimum ambient lighting conditions for the viewing of softcopy radiological images. Proc SPIE. 2006;6146:260–268. [Google Scholar]
- 13.Brennan PC, McEntee M, Evanoff M, Philips P, O’Connor WT, Manning DJ. Ambient lighting: effect of illumination on soft-copy viewing of radiographs of the wrist. AJR Am J Roentgenol. 2007;188:177–180. doi: 10.2214/AJR.05.2048. [DOI] [PubMed] [Google Scholar]
- 14.Uffmann M, Prokop M, Kupper W, Mang T, Fiedler V, Schaefer-Prokop C. Soft-copy reading of digital chest radiographs: effect of ambient light and automatic optimization of monitor luminance. Invest Radiol. 2005;40:180–185. doi: 10.1097/01.rli.0000153658.15272.91. [DOI] [PubMed] [Google Scholar]
- 15.Australasian College of Physical Scientists & Engineers in Medicine. Available at http://www.acpsem.org.au/~acpsem/index.php/nmdocuments/cat_view/334-groups/187specialty-groups/189-radiology/201-reports. Accessed 5 September 2012.
- 16.NHS Breast Screening Programme. Available at http://www.cancerscreening.nhs.uk/breastscreen/publications/nhsbsp-equipment-report-0604.pdf. Accessed 5 September 2012.
- 17.BreastScreen New South Wales: Mammography quality assurance program—guidelines for routine quality control testing for digital mammography (CR & DR), version 1. New South Wales: Cancer Institute NSW, 2010.
- 18.American Association of Physicists in Medicine. Available at http://deckard.mc.duke.edu/~samei/tg18_files/tg18.pdf. Accessed 15 Auguest 2012.
- 19.EIZO. Available at http://www.radiforce.nl/pool/files/nl/WP_QualityControl.pdf. Accessed 15 July 2012.
- 20.Barco: recommended quality assurance for Barco Coronis 5MP Mammo, version 10, Belgium: Barco, 2010
- 21.European Reference organisation for quality assured breast screening and diagnostic services (EUREF). Available at http://ec.europa.eu/health/ph_projects/2002/cancer/fp_cancer_2002_ext_guid_01.pdf. Accessed 15 August 2012.
- 22.Yaffe MJ, Bloomquist AK, Mawdsley GE, Pisano ED, Hendrick RE, Fajardo LL, Boone JM, Kanal K, Mahesh M, Fleischman RC, Och J, Williams MB, Beideck DJ, Maidment AD. Quality control for digital mammography: part II, recommendations from the ACRIN DMIST trial. Med Phys. 2006;33:737–752. doi: 10.1118/1.2164067. [DOI] [PubMed] [Google Scholar]
- 23.Barco. Available at http://www.barco.com/en/products-solutions/5mp-medical-flat-grayscale-display-for-digital-mammography_1.aspx?tab=specs. Accessed 5 April 2012.
- 24.EIZO. Available at http://www.radiforce.nl/pool/spec/GS520/1_uk_GS520.pdf. Accessed 5 April 2012.
- 25.Barco. Available at http://www.barco.com/en/Specsheets/0c0481a9-223a-4023-a97d-a685399610c9/mfgd-5621-hd.pdf. Accessed 5 April 2012.
- 26.Jung H, Kim HJ, Kang WS, Yoo SK, Fujioka K, Hasegawa M, Samei E. Assessment of flat panel LCD primary class display performance based on AAPM TG 18 acceptance protocol. Med Phys. 2004;31:2155–2164. doi: 10.1118/1.1764946. [DOI] [PubMed] [Google Scholar]
- 27.Konica Minolta. Available at http://www5.konicaminolta.eu/fileadmin/CONTENT/Measurement_Instruments/Download/NEU_Owners_Manuals/CS-2000_2000A_E_OM.pdf. Accessed 6 June 2012.
- 28.Digital Imaging and Communications in Medicine (DICOM). Available at http://medical.nema.org/dicom/2004/04_14PU.PDF. Accessed 11 July 2012.
- 29.Samei E. New developments in display quality control. Great Falls: Society for Computer Applications in Radiology; 2002. [Google Scholar]
- 30.Krupinski E, Roehrig H. Recent developments in evaluating soft-copy displays for medical images. Recent Res Devel Optical Eng. 2000;3:35–49. [Google Scholar]
- 31.Majid AS, de Paredes ES, Doherty RD, Sharma NR, Salvador X. Missed breast carcinoma: pitfalls and pearls. Radiographics. 2003;23:881–895. doi: 10.1148/rg.234025083. [DOI] [PubMed] [Google Scholar]
- 32.Chawla AS, Samei E. Ambient illumination revisited: a new adaptation-based approach for optimizing medical imaging reading environments. Med Phys. 2007;34:81–90. doi: 10.1118/1.2402583. [DOI] [PubMed] [Google Scholar]
- 33.Brennan JA, Brennan P, Haygood TM. Ambient lighting in the reading room: theoretical concepts and practical outcomes. Curr Med Imaging Rev. 2010;6:156–164. doi: 10.2174/157340510791636246. [DOI] [Google Scholar]