Abstract
Background
The crossover sign is a radiographic finding associated with cranial acetabular retroversion and has been associated with pincer-type femoroacetabular impingement (FAI) in patients with hip pain. Variable morphology, location, and size of the anterior inferior iliac spine (AIIS) may contribute to the crossover sign even in the absence of retroversion. Thus, the sign may overestimate the incidence of acetabular retroversion.
Questions/purposes
We asked: Can the crossover sign appear on standardized, well-positioned AP pelvis radiographs despite the absence of acetabular retroversion? And what is the contribution of variable size and morphology of the AIIS to a crossover sign?
Methods
We evaluated radiographs of 53 patients with symptomatic FAI in the absence of substantial chondral degenerative changes (< Tönnis Grade 2). Forty-one radiographs met the appropriate criteria of neutral tilt and obliquity. Three independent reviewers determined presence and location of the crossover sign. Acetabular version was defined using high-resolution three-dimensional CT. CT reconstructions were used to define three AIIS types addressing AIIS morphology.
Results
Nineteen of 38 radiographs with a crossover sign on AP radiographs had focal or global acetabular retroversion on three-dimensional CT (positive and negative predictive values = 50%). In contrast, the AIIS extended to or below the level of the anterior superior acetabular rim and was partially or completely responsible for the appearance of a radiographic crossover sign in all 19 hips with an anteverted acetabulum. High interobserver reliability (kappa > 0.8) was found for AIIS types.
Conclusions
A crossover sign is frequently present on well-positioned AP pelvis radiographs in the absence of acetabular retroversion. Variable AIIS morphology may explain the appearance of this sign in the presence or absence of acetabular retroversion.
Level of Evidence
Level III, diagnostic study. See Instructions for Authors for a complete description of levels of evidence.
Introduction
Cranial (cephalad) retroversion of the acetabulum is a specific morphologic variation of acetabular anatomy in which the acetabular opening is situated in a more posterolateral direction in the sagittal plane relative to a more normal, anterolateral opening [9, 10]. This morphology has been associated with a dynamic focal rim impingement between the anterolateral head-neck junction of the femur and the retroverted acetabular rim. This type of impingement has been termed pincer impingement in the literature and results in an impaction injury pattern to the acetabular labrum with resulting mechanical hip pain. Treatment is typically directed at rim recession with either focal labral débridement or labral refixation to eliminate the retroversion and zone of mechanical conflict and to restore the normal suction seal effect of the labrum [6]. True acetabular retroversion is characterized by global anterior overcoverage with corresponding posterior undercoverage and may result in isolated anterior impingement or combined anterior impingement with posterior coverage deficiency, leading to posterior instability. This morphology is different from focal cranial retroversion, which is characterized by anterior overcoverage only at the cranial aspect of the acetabulum with normal posterior wall coverage. The presence of a posterior wall sign (the posterior wall of the acetabulum sits medial to the center of the femoral head) and an ischial spine sign (exaggerated size of the ischial spine on the AP radiograph medial to the pelvic brim) are radiographic findings of true acetabular retroversion.
A major limitation in distinguishing focal from true acetabular retroversion, however, remains the unreliability of plain radiographs. The crossover sign is associated with focal cranial retroversion and on AP pelvis radiographs is characterized by the anterior rim of the acetabulum projecting more laterally than the posterior rim proximally but correcting more distally with progressive medial projection [8]. Unfortunately, the reliability of these signs in identifying focal cranial retroversion is affected by small changes in pelvic tilt and rotation [1, 4, 5, 8, 10, 13]. The potentially high false-positive rate of focal cranial retroversion of the acetabulum indicated by the presence of a crossover sign may errantly lead to the surgical resection of portions of the acetabular rim, and in cases of true acetabular retroversion with posterior wall deficiency, resection of the anterior acetabular wall can lead to iatrogenic dysplasia and structural instability.
Even with properly positioned and aligned pelvic radiographs, variable morphology, size, and location of the anterior inferior iliac spine (AIIS) may contribute to the appearance of a radiographic crossover sign [12]. A prominent AIIS at the anterior superior acetabular rim level has been reported as another contributing factor for hip impingement [11]. In these cases, the caudad prominence of the AIIS impinged against the femoral head-neck junction during hip flexion and the impingement was relieved after partial resection of the impinging portion of the AIIS. Dandachli et al. [2] reported on radiographs and CT scans of 64 hips in 33 patients with symptomatic femoroacetabular impingement (FAI). The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) for the crossover sign were 92%, 55%, 59%, and 91%, respectively [2]. Given the relatively low specificity of the crossover sign, the potential for errant rim resection based on a presumption of focal cranial retroversion is a major concern in the treatment of FAI.
Our purpose was to assess the true incidence of focal cranial retroversion using CT imaging in patients with the crossover sign on well-positioned, standardized radiographs. To understand the etiology of a crossover sign in the absence of cranial retroversion, we assessed the size, morphology, location, and contribution of the AIIS to the crossover sign.
Patients and Methods
From a consecutive series of 80 patients with symptomatic FAI, we identified 53 (31 male, 22 female) without substantial chondral degenerative changes (ie, Tönnis Grade 1 [16] or less) treated between 2008 and 2010. We excluded 27 patients with previous hip injury, fracture, or surgery. Of the 53 patients, 41 had supine AP pelvis radiographs with the following radiographic criteria: neutral tilt as determined by coccyx-symphyseal distance and neutral rotation as determined by symmetry of the obturator foramen. Patients were positioned supine with their frontal anatomic plane parallel to the film plate. The central beam was directed to the midpoint between the pubic symphysis and a horizontal line connecting both anterior superior iliac spines (ASISs). The distance between the sacrococcygeal joint and the superior border of the pubic symphysis measured between 3 and 4 cm [7]. This study was approved by our institutional review board.
Preoperative, high-resolution CT scans (GE LightSpeed® VCT 64 channel scanner; GE Medical Systems, Milwaukee, WI, USA) were obtained for all patients in a single imaging institution according to a similar protocol and setup with the patient in the supine position. The three-dimensional (3D) rendering was performed on the GE Advantage Workstation® (GE Centricity® PACS-IW workstation; GE Medical Systems; Version 4.3 software) creating 11 3D views of the hip, each view rotated in the axial plane 32.7° relative to the previous view, thus forming a 360° view of each hip (ie, 11 × 32.7 = 360). The scanning protocol involved scanning the pelvis and knee with 1.5-mm slices at the level of the ASIS and 1-mm slices across the acetabula to allow for definition of both acetabular and femoral version, as described by Dandachli et al. [3]. A modified CT protocol using a decreased radiation exposure of 1.6 rad (approximately ½ of the dose received from three views of the hip/pelvis) was utilized to maximize patient safety. Positioning of patients in the scanner was standardized, with the legs in neutral abduction/adduction and with the patellae pointing directly forward. Acetabular version was quantified at three transverse sections through the acetabulum: cranial (5 mm distal to the acetabular roof), central (through the longitudinal center of the acetabulum), and caudal (5 mm proximal from the most inferior edge of the acetabular cavity) correlating with 1-, 2-, and 3-o’clock positions, respectively.
Three of us (AB, IZ, BTK) independently determined presence and location of a crossover sign on the AP pelvis (superior, middle, or inferior 1/3 of the acetabulum). Disagreements occurred in two of 79 observations, and the final characterization was made by consensus in these cases.
We developed an AIIS classification system based on 3D CT reconstructions (Table 1). Among the 11 3D views of each hip, we identified two views that allowed for circumferential characterization of the shape of the AIIS and its relation to the anterior superior acetabular rim (Fig. 1): a one-internal rotation of 32.7° or head-on view (relative to the AP view) and a four-internal rotation of 32.7° or ischium view (relative to the AP view).
Table 1.
Classification of AIIS types
| Type | Description | CT definition | Suggested clinical applications |
|---|---|---|---|
| I | Up-sloping | Up-sloping on ischium view | AIIS does not contribute to impingement |
| II | Down-sloping | Down-sloping on ischium view but does not cross caudad to rim in any of the views | AIIS may contribute to impingement |
| III | Hooked | Down-sloping on ischium view and crosses caudad to rim in any of the views | AIIS may contribute to impingement |
AIIS = anterior inferior iliac spine.
Fig. 1A–D.
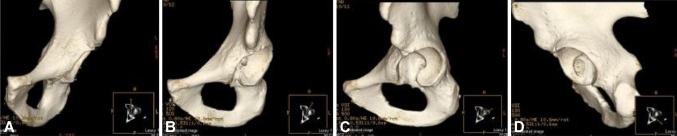
The four views that define the shape of the AIIS and its relation to the acetabular rim are shown: (A) AP view, (B) one-rotation or head-on view, (C) two-rotation view, and (D) four-rotation or ischium view. The yellow line in the box at the bottom right corner of each view shows the direction of the view.
To categorize the AIIS morphology, a horizontal line was drawn on the ischium view, crossing at the most caudal level of the junction of the AIIS with the ilium wall. In Type I, the AIIS did not cross caudad to this horizontal line. In Type II, part of the AIIS crossed caudad to the horizontal line but not caudad to the anterior superior acetabular rim (Fig. 2). In this case, the AIIS prominence did not obscure the continuity of the acetabular rim seen on the head-on view and two-rotation view. In Type III, part of the AIIS crossed caudad to the horizontal line and also caudad to the anterior superior acetabular rim (Fig. 3). In this case, the AIIS prominence obscured part of the continuity of the acetabular rim seen on the head-on view, two-rotation view, or both. A reliability study of the classification system was performed in a cohort of patients in a blinded fashion with three independent observers (an orthopaedic surgeon [BTK], a musculoskeletal radiologist [GD], and a research assistant [IH]). The cohort comprised 58 patients (33 male, 25 female) treated by the senior author (BTK) between March 2008 and June 2010. The inclusion criteria were age of 15 to 30 years, insidious-onset hip pain or pain after low-energy sports trauma, positive hip impingement sign, Tönnis Grade 0 to 1, or CT scan confirming cam morphology, focal cranial acetabular retroversion (ie, pincer morphology), or combined cam morphology and focal cranial acetabular retroversion. The exclusion criteria were age younger than 15 years or older than 30 years, high-energy hip trauma (ie, fracture or dislocation), history of surgery involving the femur or pelvis, Tönnis Grade 2 or above, proliferative disease of the hip (ie, synovial chondromatosis, pigmented villonodular synovitis), neuromuscular disease (ie, cerebral palsy), Legg-Calvé-Perthes deformity, and developmental dysplasia of the hip. We calculated weighted kappa coefficients for AIIS morphology (Types I, II, III). Interobserver agreement was 0.9 for AIIS classification (Table 2). We performed statistical analyses using the SAS® System for Windows® Version 9.1 (SAS Institute Inc, Cary, NC, USA).
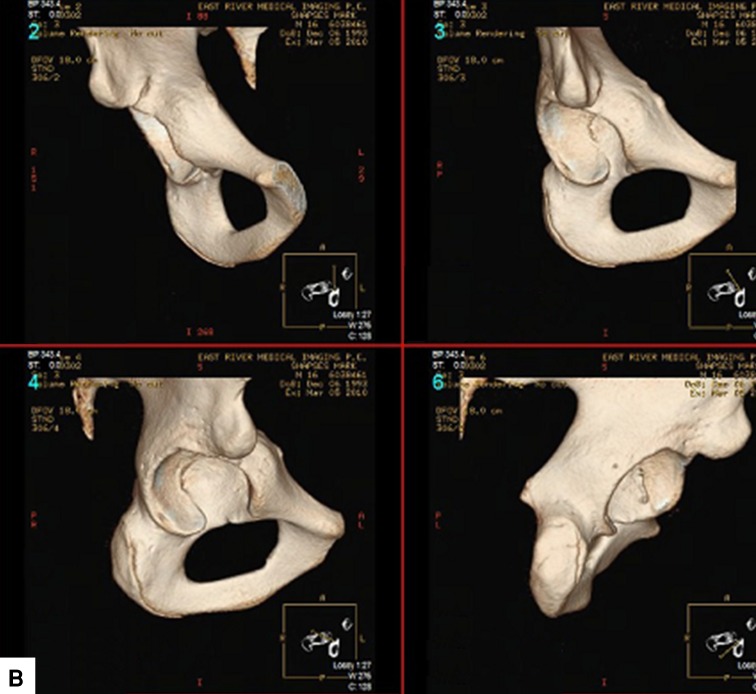
Fig. 2A–D.

Type II (flat or down-sloping) AIIS morphology is shown on (A) AP view, (B) one-rotation or head-on view, (C) two-rotation view, and (D) four-rotation or ischium view. Part of the AIIS crosses or is parallel to the caudal horizontal line on the ischium view, but it does not obscure the continuity of the acetabular rim on the head-on view and two-rotation view.
Fig. 3A–D.

Type III (hooked) AIIS morphology is shown on (A) AP view, (B) one-rotation or head-on view, (C) two-rotation view, and (D) four-rotation or ischium view. Part of the AIIS crosses caudad to the horizontal line on the ischium view and also obscures part of the continuity of the acetabular rim on the head-on view.
Table 2.
Interobserver reliability for AIIS types
| Comparison | Weighted kappa (95% CI) |
|---|---|
| Observer 1-Observer 2 | 0.987 (0.961, 0.999) |
| Observer 1-Observer 3 | 0.960 (0.922, 0.999) |
| Observer 2-Observer 3 | 0.973 (0.940, 0.999) |
AIIS = anterior inferior iliac spine.
Results
Thirty-eight of 41 patients (92.7%) had a crossover sign on AP pelvis radiographs (Fig. 4). Twenty-four (63%) were in the superior, 10 (26%) were in the middle, and four (11%) were in the inferior 1/3 of the acetabulum. Only 19 of these 38 radiographs with a crossover sign demonstrated focal or true acetabular retroversion on 3D CT analysis (PPV and NPV = 50%). In contrast, the AIIS extended to the level of the anterior superior acetabular rim and was partially or completely responsible for the appearance of a radiographic crossover sign in all hips with an anteverted acetabulum (Fig. 5). Type I morphology was the most common type in both males and females, while Type III morphology was almost exclusively observed in males (seven of eight) (Table 3).
Fig. 4A–B.
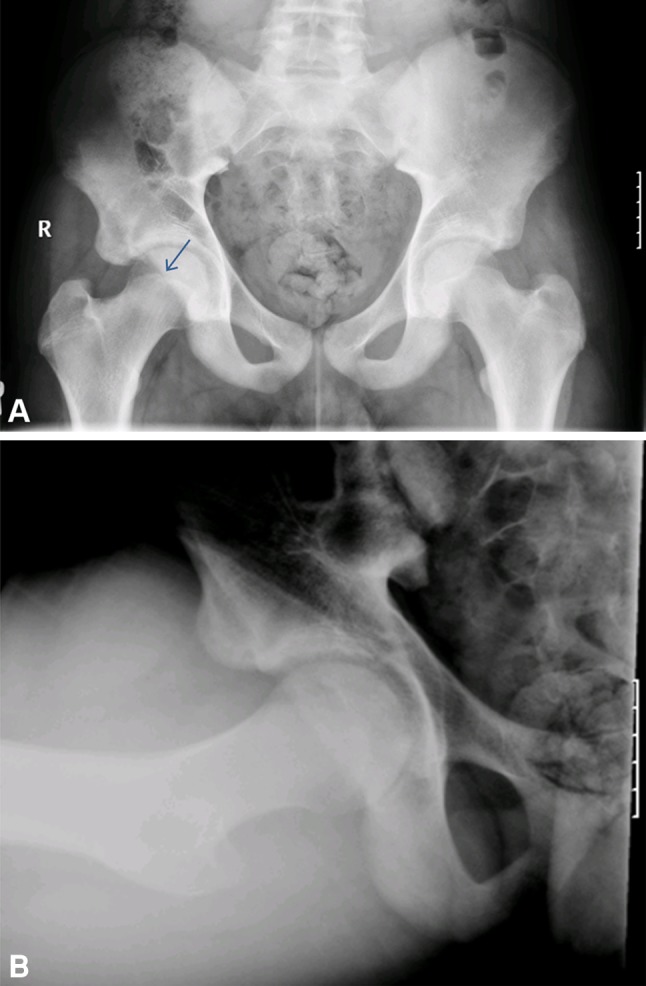
(A) AP pelvis and (B) Dunn (extended-neck) lateral radiographs from a patient with right groin pain demonstrate evidence of the crossover sign (arrow). Note the AP pelvis radiograph is appropriate, with no substantial tilt or obliquity and appropriate distance between the coccyx and symphysis pubis. The lateral radiograph demonstrates appropriate femoral head-neck offset.
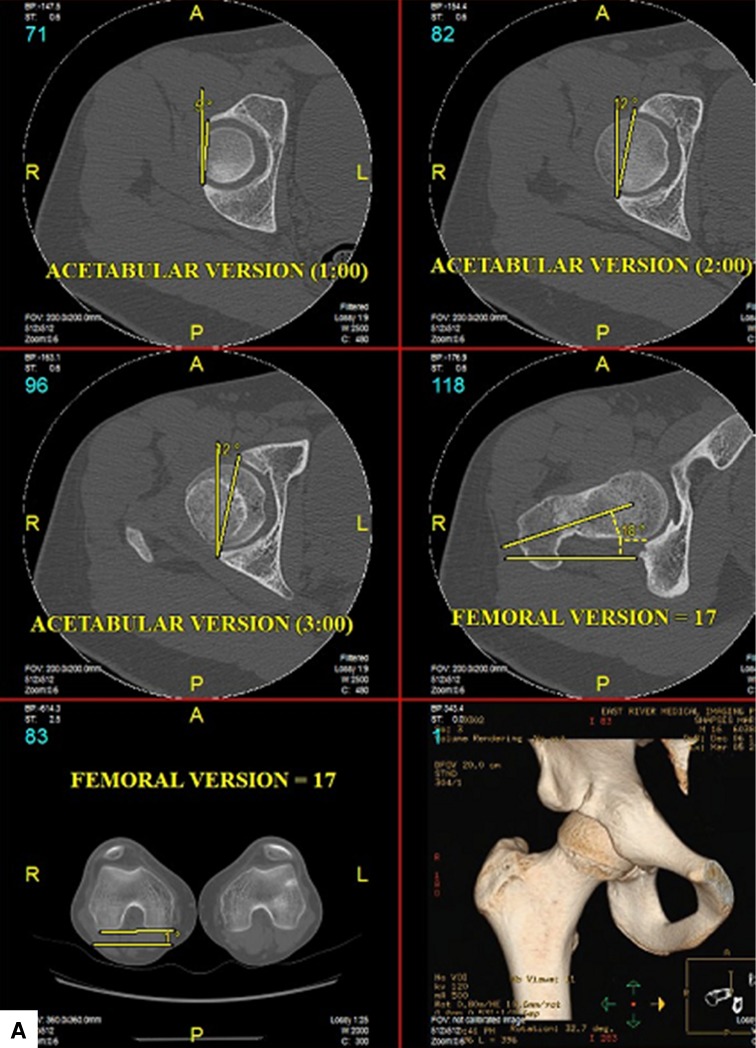
Fig. 5A–B.
(A) Axial CT images of the right hip demonstrate anteversion of the acetabulum at the 12-, 1-, and 2-o’clock locations despite the radiographic appearance of a crossover sign. Femoral version is also assessed at 17° as referenced from the posterior condylar axis of the distal femur. (B) Type III AIIS morphology is shown in AP view (upper left), one-rotation or head-on view (upper right), two-rotation view (lower left), and four-rotation or ischium view (lower right). Part of the AIIS crosses caudad to the horizontal line and also caudad to the anterior superior acetabular rim.
Table 3.
Prevalence of AIIS type in males and females
| AIIS type | Number of hips | |
|---|---|---|
| Males (n = 33) |
Females (n = 25) |
|
| I | 23 | 23 |
| II | 3 | 1 |
| III | 7 | 1 |
AIIS = anterior inferior iliac spine.
Discussion
The diagnosis of acetabular retroversion in patients with symptomatic hip impingement is challenging and depends on a reliable and reproducible method to quantify the relationship between the anterior and posterior acetabular walls. This assessment is further complicated by the changing relationship between the walls from a cephalad to caudal position in the normal acetabulum. While radiographic findings such as the crossover or ischial spine sign facilitate the recognition of acetabular retroversion, the incidence of false-positives is not insignificant and may result in an overestimation of the incidence of rim impingement (pincer-type FAI) and an errant surgical treatment in symptomatic patients. We therefore determined the true incidence of acetabular retroversion in patients with a positive crossover sign on appropriately positioned pelvis radiographs and evaluated the contribution of AIIS size and morphology to the appearance of the crossover sign.
This study is not without limitations. First, the relevance of a caudal AIIS morphology and its contribution to symptoms in patients with crossover sign is unclear. Future cadaveric and clinical studies are necessary to characterize the anatomic variability in AIIS morphology and its potential contribution to mechanical impingement in the symptomatic hip. Second, we included only symptomatic patients in the study and a control population of asymptomatic subjects with appropriate imaging studies would be invaluable for comparison. Previous work by Jamali et al. [8] reported a 96% sensitivity of the crossover sign to detect a cranial acetabular anteversion of less than 4° but not necessarily absolute retroversion due to divergence of the x-ray beam. It is possible a crossover sign in some of the cases in this series were not necessarily attributable to the AIIS morphology. In this regard, there may be slight overestimation of the number of false-positive crossover signs by the criteria of Jamali et al. [8]. However, it should also be noted, while the study of Jamali et al. [8] has been considered the standard, that work was in cadaveric specimens and it has never been independently repeated and verified. In this regard, this study helps to establish, along with the results of Jamali et al. [8], the concern that the crossover sign is not pathognomonic of pathologic cranial retroversion requiring surgical correction in the setting of symptomatic FAI.
Based on our results in symptomatic individuals, a crossover sign may be present on 50% of appropriately obtained AP pelvis radiographs in the absence of cranial acetabular retroversion. The crossover sign and ischial spine sign have been variably reported as reliable radiographic indicators of acetabular retroversion [8, 10, 14, 15]. Jamali et al. [8] found the crossover sign had a PPV of 90% and a specificity of 95%. They correlated radiographs of skeletal specimens with anatomic measurements made with the position of the pelvis standardized to the anterior pelvic plane [8]. While this position may be more closely controlled in cadaveric models, the crossover sign is greatly influenced by the quality of the radiograph and the degree of pelvic tilt in vivo. Furthermore, supine versus standing position and the impact of lumbar lordosis on pelvic tilt may further confound the standardization of pelvic orientation. The frequency with which pelvic tilt affects interpretation of radiographs was demonstrated by Kalberer et al. [10], who reviewed 1010 pelvic radiographs in patients assessed for a painful hip to note the presence of an ischial spine sign. Only radiographs denoting neutral rotation of the pelvis were included. Further exclusion of radiographs with inadequate exposures left only 149 of the original 1010 (14.7%) for analysis [10]. Siebenrock et al. [13] reported on the considerable variability in pelvic tilt based on 86 pelvic radiographs compared with a cadaver model. Dandachli et al. [2] has reported on the limited reliability of the crossover sign and attributed this finding to variability in pelvic tilt. Using a CT technique that allowed standardized 3D analysis of acetabular inclination and calculation of femoral head cover in relation to a specific anterior reference plane, the sensitivity, specificity, PPV, and NPV for the crossover sign were 92%, 55%, 59%, and 91%, respectively [2]. We found a 50% false-positive rate for the crossover sign. Unlike previous studies, however, the false-positive crossover sign was not attributable to variable pelvic tilt or inappropriately positioned pelvic radiographs. Rather, we identified a variable caudally projecting AIIS morphology caused the appearance of a crossover sign in 95% of hips, independent of the presence or absence of true acetabular retroversion. These findings suggest the assessment of acetabular retroversion based on the presence of a crossover sign alone is inadequate and further identification and characterization of AIIS morphology in the presence of a crossover sign on pelvic radiographs are of paramount importance.
Variable AIIS morphology may be responsible for the radiographic appearance of the crossover sign. Furthermore, the AIIS may represent a novel mechanism of mechanical impingement in the hip. Even in the presence of focal acetabular retroversion, the AIIS may contribute to the crossover sign. A prominent AIIS at the anterior superior acetabular rim level has been reported as another contributing factor for hip impingement [11]. In these cases, the caudad prominence of the AIIS impinged against the femoral head-neck junction during hip flexion and the impingement was relieved after partial resection of the pathologic portion of the AIIS [11, 12]. Our proposed classification and validation suggest high interobserver agreement in defining AIIS morphology on 3D CT imaging. Some preliminary studies indicate a morphology that may be contributory to subspinal, extraarticular impingement and result in a symptomatic restriction in hip flexion and internal rotation [11, 12]. Inappropriate correction of acetabular retroversion based on a false-positive crossover sign may contribute in some cases to failure or modestly improved clinical outcomes observed after open or arthroscopic hip preservation surgery. Overlooking and undertreating extraarticular impingement associated with prominent AIIS morphology may be a contributing factor to failed FAI surgery. As such, recognition of the specific morphology of the AIIS should be carefully considered in planning for surgical intervention for symptomatic hip impingement.
In summary, acetabular retroversion remains difficult to identify and cannot be definitively diagnosed based on the presence of a crossover or ischial spine sign alone, even on well-aligned pelvic radiographs with acceptable tilt and obliquity. Inferring the potential for pathologic rim impingement based on the presence of these findings should not prompt a rim recession and labral refixation in patients with symptomatic hip or groin pain. This may result in unnecessary resection of acetabular hyaline cartilage, increased risk of iatrogenic hip instability, and production of iatrogenic acetabular dysplasia. Rather, these findings warrant further evaluation for a quantitative assessment of acetabular version and characterization of the AIIS morphology.
Acknowledgments
The authors thank Gavin Duke, MD, musculoskeletal radiologist, East River Medical Imaging, New York, NY, USA, for his help in performing the agreement study to validate AIIS type classification.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the Hospital for Special Surgery, New York, NY, USA.
References
- 1.Beaule PE, Allen DJ, Clohisy JC, Schoenecker PL, Leunig M. The young adult with hip impingement: deciding on the optimal intervention. Instr Course Lect. 2009;58:213–222. [PubMed] [Google Scholar]
- 2.Dandachli W, Islam SU, Liu M, Richards R, Hall-Craggs M, Witt J. Three-dimensional CT analysis to determine acetabular retroversion and the implications for the management of femoro-acetabular impingement. J Bone Joint Surg Br. 2009;91:1031–1036. doi: 10.1302/0301-620X.91B8.22389. [DOI] [PubMed] [Google Scholar]
- 3.Dandachli W, Ul Islam S, Tippett R, Hall-Craggs MA, Witt JD. Analysis of acetabular version in the native hip: comparison between 2D axial CT and 3D CT measurements. Skeletal Radiol. 2011;40:877–883. doi: 10.1007/s00256-010-1065-3. [DOI] [PubMed] [Google Scholar]
- 4.Dora C, Leunig M, Beck M, Simovitch R, Ganz R. Acetabular dome retroversion: radiological appearance, incidence and relevance. Hip Int. 2006;16:215–222. doi: 10.1177/112070000601600307. [DOI] [PubMed] [Google Scholar]
- 5.Eckman K, Hafez MA, Ed F, Jaramaz B, Levison TJ, Digioia AM., 3rd Accuracy of pelvic flexion measurements from lateral radiographs. Clin Orthop Relat Res. 2006;451:154–160. doi: 10.1097/01.blo.0000238809.72164.54. [DOI] [PubMed] [Google Scholar]
- 6.Ferguson SJ, Bryant JT, Ganz R, Ito K. An in vitro investigation of the acetabular labral seal in hip joint mechanics. J Biomech. 2003;36:171–178. doi: 10.1016/S0021-9290(02)00365-2. [DOI] [PubMed] [Google Scholar]
- 7.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 8.Jamali AA, Mladenov K, Meyer DC, Martinez A, Beck M, Ganz R, Leunig M. Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the “cross-over-sign”. J Orthop Res. 2007;25:758–765. doi: 10.1002/jor.20380. [DOI] [PubMed] [Google Scholar]
- 9.Kakaty DK, Fischer AF, Hosalkar HS, Siebenrock KA, Tannast M. The ischial spine sign: does pelvic tilt and rotation matter? Clin Orthop Relat Res. 2010;468:769–774. doi: 10.1007/s11999-009-1021-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kalberer F, Sierra RJ, Madan SS, Ganz R, Leunig M. Ischial spine projection into the pelvis: a new sign for acetabular retroversion. Clin Orthop Relat Res. 2008;466:677–683. doi: 10.1007/s11999-007-0058-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Larson CM, Kelly BT, Stone RM. Making a case for anterior inferior iliac spine/subspine hip impingement: three representative case reports and proposed concept. Arthroscopy. 2011;27:1732–1737. doi: 10.1016/j.arthro.2011.10.004. [DOI] [PubMed] [Google Scholar]
- 12.Pan HL, Kawanabe K, Akiyama H, Goto K, Onishi E, Nakamura T. Operative treatment of hip impingement caused by hypertrophy of the anterior inferior iliac spine. J Bone Joint Surg Br. 2008;90:677–679. doi: 10.2106/JBJS.G.01544. [DOI] [PubMed] [Google Scholar]
- 13.Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res. 2003;407:241–248. doi: 10.1097/00003086-200302000-00033. [DOI] [PubMed] [Google Scholar]
- 14.Tannast M, Kubiak-Langer M, Langlotz F, Puls M, Murphy SB, Siebenrock KA. Noninvasive three-dimensional assessment of femoroacetabular impingement. J Orthop Res. 2007;25:122–131. doi: 10.1002/jor.20309. [DOI] [PubMed] [Google Scholar]
- 15.Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis—what the radiologist should know. AJR Am J Roentgenol. 2007;188:1540–1552. doi: 10.2214/AJR.06.0921. [DOI] [PubMed] [Google Scholar]
- 16.Tönnis D. [Letter: Congenital hip dysplasia: clinical and radiological diagnosis (author’s transl)] [in German] Z Orthop Ihre Grenzgeb. 1976;114:98–99. [PubMed] [Google Scholar]