Abstract
Background
Although a large number of athletes’ returns to sports after hip arthroscopic surgery for femoroacetabular impingement (FAI), it is not clear if they do so to the preinjury level and whether professional athletes (PA) are more likely to return to the preinjury level compared with recreational athletes (RA).
Questions/purposes
We therefore compared (1) the time taken to return to the preinjury level of sport between professional and recreational athletes; (2) the degree of improvement in time spent in training and competitive activities after arthroscopic surgery for FAI; and (3) the difference in trend of improvement in hip scores.
Methods
We prospectively followed 80 athletes (PA = 40, RA = 40; mean age, 35.7 years; males = 50, females = 30; mean followup, 1.4 years; range, 1–1.8 years) who underwent hip arthroscopy for FAI. We measured the time to return to sports; training time and time in competition; and the modified Harris hip score and the nonarthritic hip score.
Results
There was a 2.6-fold improvement in the training time (from 7.8 to 20 hours per week) and a 3.2-fold increase in time in competition (from 2.5 to 7.9 hours per week) 1 year after surgery. The mean time to return to sporting activities was 5.4 months, which was lower for PA (4.2) as compared with RA (6.8). Eighty-two percent (66) (PA = 88% [35] versus RA = 73% [29]) returned to their preinjury level of sport within 1 year of surgery.
Conclusions
The data suggest PA may show quicker return to sports than RA but the hip scores and rate of return to sports are similar.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Hip arthroscopy is an established intervention for the treatment of hip disorders in the sporting and general population [1, 2, 6, 9, 15, 17, 21–23, 27]. Labral repair with osteochondroplasty for femoroacetabular impingement (FAI) in a professional sportsperson can lead to a high patient satisfaction rate and prompt return to sports [1, 10, 25, 26]. In the general population, arthroscopic management of FAI leads to pain and preoperative scores in 75% to 77% of patients at 1 year [14, 18, 20]. Botser et al. [4] in a review comparing arthroscopy with open surgical dislocation and a combined approach for FAI found consistent improvement in modified Harris hip score (mHHS) for all with a lower complication rate and higher return to sports for professional athletes with the arthroscopic approach. The arthroscopic approach has the benefit of less soft tissue damage leading to quicker rehabilitation and also is safer for the patients [4]. Even in patients with milder degrees of preoperative degenerative change on their radiographs, after osteochondroplasty for FAI, an improvement in pain and function has been demonstrated at followup from 12 to 60 months [19]. An acetabular labral tear is described as the most common pathology for which hip arthroscopy may be indicated and selective débridement of these tears leads to improvement in HHS at 10 years in 83% of patients without associated arthritis [8]. Although there is no evidence surgery prevents osteoarthritis, Ellis et al. in a review conclude that by resolving bony impingement, prevention of further labral and chondral damage is possible, and the progression of osteoarthritis may be delayed [13]. Most studies of the sporting population have been retrospective in nature or in a small series of patients ranging from 10 to 45 patients [21, 24–27, 29]. Furthermore, when it is reported that a patient has returned to sport after surgery, what does this mean? Does this imply a return to sport in general or a return to preinjury levels of activity? The latter is clearly important. Objective criteria like time spent in training and competition would directly indicate if the pain limits the duration of time these patients can spend in high-output activity and therefore will be one way to measure this. It is also unknown if there is a difference in the rate of return to the same level of sports, hip scores, and satisfaction scores between individuals engaged in competitive sports (professional athletes) as compared with recreational sports (recreational athletes).
We therefore determined (1) the time taken to return to the preinjury level of sport; (2) the degree of improvement in time spent in training and competitive activities after arthroscopic surgery for FAI; and (3) the difference in trend of improvement in hip scores between professional and recreational athletes.
Patients and Methods
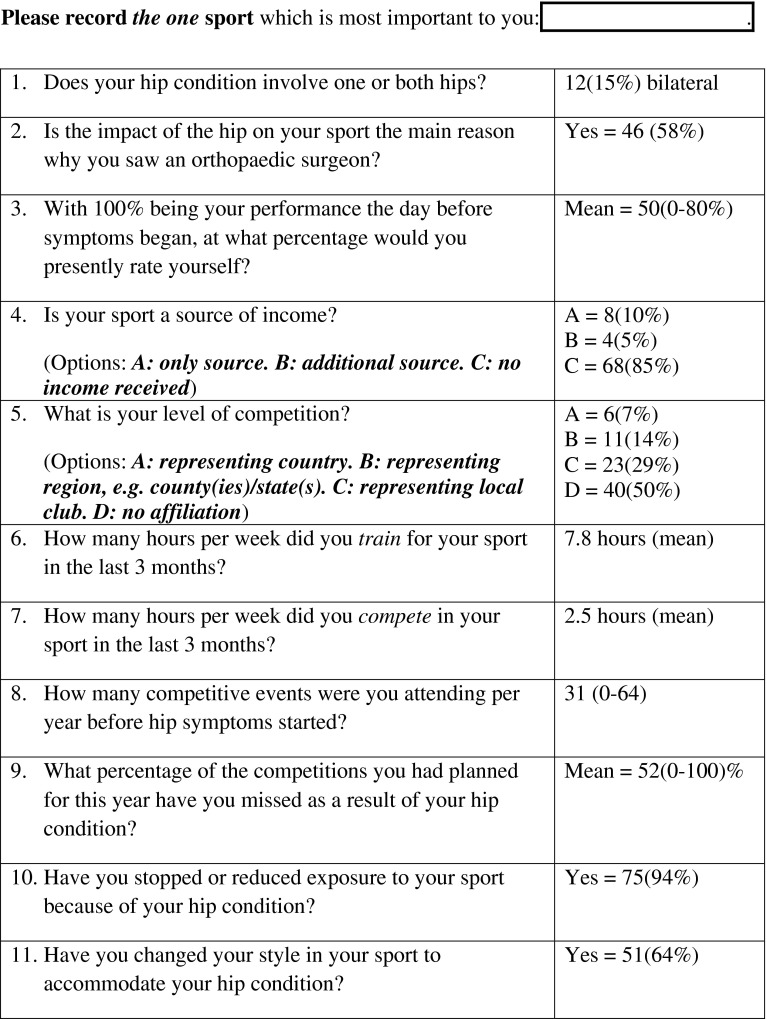
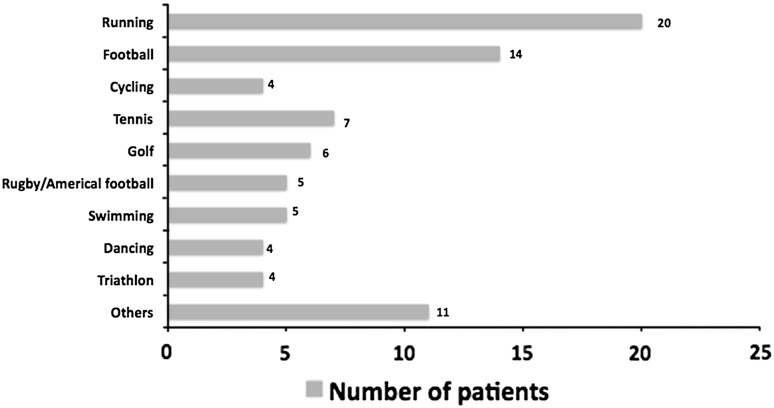
We prospectively followed all 80 athletes who underwent arthroscopy for FAI from November 2009 to August 2010. The indications for arthroscopy for the cohort of patients included in the study were (1) pain and limitation of activity; (2) positive impingement test; and (3) radiographically proven impingement lesion (cam, pincer, or both). We did not perform arthroscopy in patients with unrestricted activity. We excluded six patients with Tönnis 2 or 3 osteoarthritis treated during the study time. All patients were asked to complete a sports module questionnaire (Fig. 1), which required them to declare before surgery if they actively engaged in sporting activities or not and the level at which they participated. We defined the patients as professional athletes (PAs; n = 40), which included those who engage in competitive sports representing their country, region, or local club, and recreational athletes (RAs; n = 40) who were involved only in recreational sports. The mean age of the patients at the time of surgery was 35.7 years (range, 14–59 years). There were 50 (63% [N = 80]) males. Of the 40 PA patients, six (7%) represented their country, 11 (14%) their region, and 23 (29%) their club. The type of sporting activity varied widely (Fig. 2). Bilateral symptoms were present in 12 patients (15%). Forty-six patients (58%) had presented primarily because their hip pain was restricting their sporting activities. The responses to the sports questionnaire are included in Figure 1. Patients felt that their performance at the time of presentation was reduced to a mean of 50% (0%–80%) of their usual activity before the beginning of symptoms. The PA participated in a mean of 31 events/year (range, 0–64 events/year) before the onset of symptoms and had to miss a mean of 52% (0%–100%) of events because of their hip symptoms. There were 75 (94%) patients who had to reduce their exposure to sports before surgery and 51 (64%) who had modified their style in sport to accommodate their hip condition. For eight patients (10%), sport was their only source of income, whereas for four patients (5%), sport was an additional source of income. No patients were lost to followup. The minimum followup was 1 year (mean, 1.4 years; range, 1–1.8 years). No patients were recalled specifically for this study; all data were obtained from medical records.
Fig. 1.
Sports module questionnaire relating to the impact of the hip problem on the preferred sport. If someone played more than one sport, patients were requested to answer with respect to the activity that was most important to them.
Fig. 2.
Bar chart depicting the type of sporting activity most important to the patients. Others included badminton, basketball, boxing, cricket, handball, hockey, martial arts, skiing, squash, table tennis, and volleyball.
Power analysis revealed that to detect a difference in the mean mHHS [7] or nonarthritic hip score (NAHS) [11] of five points with a SD of 5 for a 90% power with p value set at 0.05, 22 patients would be required in each group. A change 7 to 10 points has been suggested to show a minimum clinically important difference in hip scores [3, 12]. We chose a value of 5 to improve the robustness of the analyses.
The two groups were comparable by all preoperative measures (Table 1). There was no statistical difference between the two groups in terms of age, sex, or preoperative alpha angle.
Table 1.
Comparison of the two groups
| Parameters | Professional athletes | Recreational athletes | p value |
|---|---|---|---|
| Number | 40 | 40 | |
| Mean age (years) | 36 (range, 16–59) | 35 (range, 14–57) | 0.58 |
| Sex (male:female) | 26:14 | 24:16 | 0.57 |
| Alpha angle | 60° (range, 48°–66°) | 59° (range, 49°–65°) | 0.48 |
| Tönnis grade | |||
| 0 | 23 | 25 | 0.47 |
| 1 | 13 | 11 | 0.47 |
| 2 | 4 | 4 | 0.93 |
| 3 | 0 | 0 | |
| Surgical procedure | |||
| Cam lesion | 39 | 37 | 0.85 |
| Pincer lesion | 8 | 8 | 0.62 |
| Microfracture | 6 | 8 | 0.91 |
| Labral fixation | 11 | 9 | 0.67 |
The senior author (RNV) assessed all the patients and those who had a positive impingement sign and MRI-proven impingement lesion were counseled for surgery. Those who had progressively increasing pain affecting the quality of life despite a trial of nonoperative treatment underwent surgery. The senior author directly performed all the procedures. The surgery was performed in the lateral position with the patient under general anesthesia under image intensifier control and traction. The central compartment was accessed first followed by the peripheral compartment after releasing the traction. Details of the senior author’s surgical technique have been described elsewhere [16]. Surgery involved removal of the impingement lesion (femoral and/or acetabular) and, where appropriate, repair of chondral/labral/chondrolabral lesions. This was by microfracture, labral reattachment, or chondrolabral repair using either sutures or fibrin adhesive. The procedures were similar in both groups (Table 1). Labral preservation was the central philosophy in dealing with all the cases.
All patients received an identical, standardized physiotherapy regimen in the postoperative period. The patients were asked to partially weightbear for the first 4 weeks with the help of crutches. Formal physiotherapy was started 1 week after surgery and continued for a period of 4 months after surgery using a documented rehabilitation plan.
The patients were followed up at 6 weeks, 3 months, 1 year, and annually thereafter. We prospectively collected the mHHS and the NAHS. The scores were collected immediately preoperatively on the day of surgery and at each followup visit. The sports module questionnaire included information on the training time (in hours per week) and also competitive activity (hours per week).
To determine whether the data normally distributed, we used a Kolmogorov-Smirnov test. If p < 0.05, the data were treated as nonparametric. To compare the training time, time in competition, mHHS, and NAHS, we used two-sample t-tests for parametric data and the Mann-Whitney U test for nonparametric data. All the tests were two-tailed. A chi-square test was used to compare the number of patients returning to sporting activities in the two groups. The statistical analysis was performed using the SPSS Version 15 statistical program (SPSS Inc, Chicago, IL, USA).
Results
The mean time to return to sporting activities was 5.4 months (range, 3–10 months) for the entire group. This was lower (p = 0.03) for PA (4.2 months) compared with RA (6.8 months). At 6 months followup, 57 (72%) had returned to their preferred sporting activity. This tended to be higher (p = 0.21) in PA (31 of 40 [78%]) as compared with RA (26 of 40 [65%]). At 1-year followup, 66 (82% [N = 80]) had returned to their preferred sporting activity. This again tended to be higher (p = 0.09) in PA (35 of 40 [88%]) as compared with RA (29 of 40 [73%]).
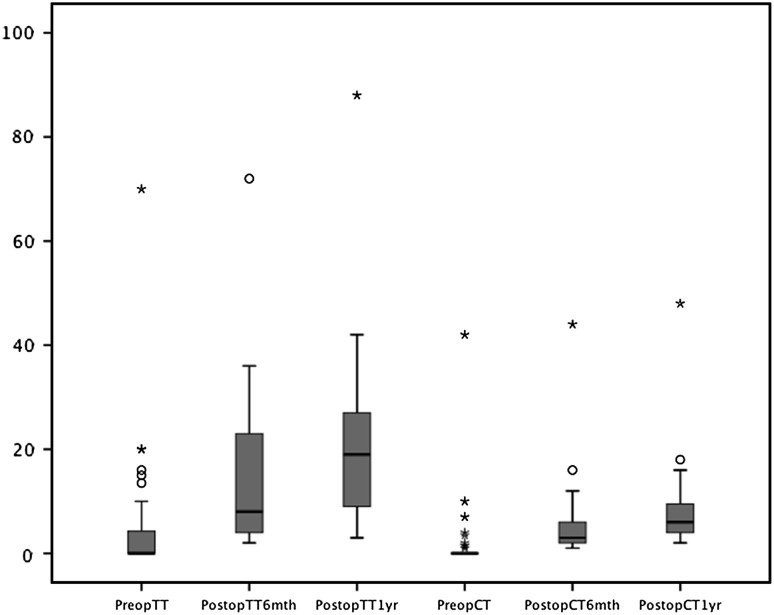
There was a 2.6-fold improvement in the training time after surgery and a 3.2-fold increase in the time in competition 1 year after surgery. For the entire study group, there was an improvement in the training time (hours per week) from a mean of 7.8 hours before surgery to 16 hours 6 months after surgery (p < 0.001) and 20 hours 1 year after surgery (p < 0.001) (Fig. 3). An improvement in the time in competition was also noted from a mean of 2.5 hours before surgery to 5.2 hours 6 months after surgery (p = 0.02) and 7.9 hours 1 year after surgery (p < 0.001). We did not find any sex difference in the training time and time in competition both before and after surgery.
Fig. 3.
Box plot (data within 95% CI) showing the change in training time (hours per week) and the time spent in competition (hours per week). PreopTT = preoperative training time; PostopTT6mth = postoperative training time (6 months); PostopTT1yr = postoperative training time (1 year); PreopCT = preoperative competition time; PostopCT6mth = postoperative competition time (6 months); PostopCT1yr = postoperative competition time (1 year). The central line is a measure of median; a minor outlier (denoted by a “o”) is an observation 1.5 × interquartile range (IQR) outside the central box; a major outlier (denoted by an asterisk) is an observation 3.0 × IQR outside the central box.
The mHHS increased from a mean of 61 before surgery to a mean of 73 at 6 months (p < 0.001) and 84 at 1 year (p < 0.001) after surgery. Similarly, the NAHS increased from a mean of 68 before surgery to 79 at 6 months (p < 0.001) and 88 (p < 0.001) at 1 year after surgery. We found no difference between the two groups in terms of the change of mHHS at 6 months (PA = 12.8, RA = 11.7; p = 0.38) and 1 year (PA = 22.6, RA = 23.4; p = 0.23) and also the NAHS at 6 months (PA = 11.3, RA = 10.7; p = 0.42) and 1 year (PA = 20.2, RA = 19.8; p = 0.46).
Discussion
Hip arthroscopic treatment of FAI leads to a high patient satisfaction rate and return to sports [1, 2, 6, 9, 15, 17, 21–23, 25–27] with improvement in pain and preoperative scores in up to 75% of patients at 1 year [14, 18, 20]. Most studies of the sporting population have been retrospective in nature or in a small series of patients and do not report objective criteria to assess their level of activity. It is not clear to what extent these patients improve and whether they are able to return to their preinjury level of sports. The motivation to return to sports is multifactorial and the evidence is limited to show if this is expected to be different for athletes in competitive sports as compared with those who do it just as a hobby. In our cohort of athletes undergoing hip arthroscopic intervention for FAI, we questioned if training time and time in competition improve after surgery and whether the hip scores and time to return to preinjury level of sports were different for PA as compared with RA.
We acknowledge limitations to our study. First, the patient population may be biased by the tertiary referral pattern of the service. We cannot ensure these findings would apply to all athletes, although it is a relatively large cohort. Second, we have a relatively short-term followup, but it is expected that the majority of improvement in pain and hip scores would occur during the first year of surgery. Third, we had no control group in which patients received no treatment or where patients were treated using an open surgical dislocation; however, Botser et al. [4], in a review of the literature on patients having treatment for FAI, suggested those with hip arthroscopy alone had similar or better improvement than those having open approaches. Fourth, the measurement of training time and time in competition has not been described or validated, but we believe this is the only objective way to measure a change in the extent to which these patients can be involved in sporting activities. We have also deliberately not elected to contrast the two groups in terms of training time and time in competition because it would have been an unfair comparison because of the different level of sports between the two groups. Fifth, the patients in this study group engaged in a wide variety of sports with their different intensities, but we believe that using the total time for these in terms of training time and time in competition would control for this limitation.
The mean time to return to the preinjury level of sporting activities in this study was 5.4 months with 82% having returned to sports by 1 year. In a recent systematic review of patients with FAI in athletes considering open surgical dislocation apart from hip arthroscopic intervention, rate of return to sports was 92% with 88% returning to the preinjury level of sports [1]. Philippon et al. [26] reported a high patient satisfaction rate with a return to sports at a mean of 3.4 months (Table 2). In a separate report on 45 professional athletes, Philippon et al. [25] also found that 78% remained in active professional sport at a mean of 1.6 years after surgery. In contrast, Nho et al. [24] reported a mean time to return to sports of 9.4 months. Singh and O’Donnell, in a series of 24 Australian Football League players who underwent arthroscopic treatment for various hip abnormalities, reported that the improved function was maintained for up to 4 years followup [27]. In a 10-year followup of 15 athletes, Byrd and Jones reported that 87% returned to sports, but five of these patients required hip arthroplasty at a mean of 6 years [9].
Table 2.
Review of literature on return to sports
| Author | Number | Followup | Return to sports | Time to return to sports (months) |
|---|---|---|---|---|
| Byrd and Jones, 2011 [10] | 200 | 19 (12–60) months | 95% of professional athletes and 85% of intercollegiate athletes | |
| Nho et al., 2011 [24] | 33 | 27 months | 79% | 9.4 |
| Philippon et al., 2010 [26] | 28 | 24 (12–42) months | 100% | 3.8 |
| Singh and O’Donnell, 2010 [27] | 24 | 22 (6–60) months | 96% | |
| Brunner et al., 2009 [5] | 53 | 2.4 (2–3.2) years | 69% | |
| Byrd and Jones, 2009 [9] | 15 | 10 years | 87% | |
| Philippon et al., 2007 [25] | 45 | 1.6 years (6 month to 5.5 years) | 78% | |
| Current study | 80 | 1.4 (1–1.8) years | 83% | 5.4 |
Ranges shown in parentheses.
At 1 year after surgery, we found a 2.6-fold improvement in the training time after surgery and a 3.2-fold increase in the time in competition. We could not find comparative data in the literature looking into these parameters. Using a sports frequency score (SFS) to look at the rate and level of sporting activities after hip arthroscopic intervention for FAI, Brunner et al. [28] reported an increase of the SFS from 0.78 to 1.84 at a mean of 2.4 years after surgery in a series of 53 patients [5]. The SFS graded patients as per their level of sporting activities from Grade 0 (no sports) to Grade 4 (professional level of activity, elite athlete). Philippon et al. [26] attempted to quantify activities using the number of games played after surgery.
We found the mHHS and NAHS continued to improve 1 year after surgery but found no difference in these outcome measures between the PA and RA. The proportion of athletes that returned to preinjury level of sports was also similar in the two groups, although we did notice that a higher proportion of PA returned to sporting activities as compared with RA (78% versus 65% at 6 months and 88% versus 73% at 1 year). This finding is similar to that of Byrd and Jones [10] who reported 95% of PA return to their previous level of competition as compared with 85% of intercollegiate athletes. Alradwan et al. [1] in a systematic review found a return to preinjury level of sports of 92% for PA as compared with 84% for RA. The return to sports was quicker for PA (4.2 months) as compared with RA (6.8 months). This may be secondary to motivational or fitness issues because all our patients received an identical postoperative rehabilitation protocol. This information can be useful in an informed consenting process to explain the prognosis and expected recovery.
In a prospective series of 80 athletes, we demonstrated the majority of the athletes (72%) return to sports within 6 months of arthroscopic surgery for FAI, increasing to 82% at 1 year. The duration of time that athletes are able to engage in training and competitive sports shows a threefold improvement after arthroscopic surgery for FAI. There is a trend that suggests PA and RA have similar improvement in mHHS and NAHS and ability to return to their preinjury level of sports, although the PA may return to sports sooner than RA.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed in The Richard Villar Practice, Spire Cambridge Lea Hospital, Cambridge, UK.
References
- 1.Alradwan H, Philippon MJ, Farrokhyar F, Chu R, Whelan D, Bhandari M, Ayeni OR. Return to preinjury activity levels after surgical management of femoroacetabular impingement in athletes. Arthroscopy. 2012;28:1567–1576. doi: 10.1016/j.arthro.2012.03.016. [DOI] [PubMed] [Google Scholar]
- 2.Bardakos NV, Vasconcelos JC, Villar RN. Early outcome of hip arthroscopy for femoroacetabular impingement: the role of femoral osteoplasty in symptomatic improvement. J Bone Joint Surg Br. 2008;90:1570–1575. doi: 10.2106/JBJS.G.01673. [DOI] [PubMed] [Google Scholar]
- 3.Beaton DE. Simple as possible? Or too simple? Possible limits to the universality of the one half standard deviation. Med Care. 2003;41:593–596. doi: 10.1097/01.MLR.0000064706.35861.B4. [DOI] [PubMed] [Google Scholar]
- 4.Botser IB, Smith TW, Jr, Nasser R, Domb BG. Open surgical dislocation versus arthroscopy for femoroacetabular impingement: a comparison of clinical outcomes. Arthroscopy. 2011;27:270–278. doi: 10.1016/j.arthro.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 5.Brunner A, Horisberger M, Herzog RF. Sports and recreation activity of patients with femoroacetabular impingement before and after arthroscopic osteoplasty. Am J Sports Med. 2009;37:917–922. doi: 10.1177/0363546508330144. [DOI] [PubMed] [Google Scholar]
- 6.Byrd JW, Jones KS. Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy. 2000;16:578–587. doi: 10.1053/jars.2000.7683. [DOI] [PubMed] [Google Scholar]
- 7.Byrd JW, Jones KS. Hip arthroscopy in the presence of dysplasia. Arthroscopy. 2003;19:1055–1060. doi: 10.1016/j.arthro.2003.10.010. [DOI] [PubMed] [Google Scholar]
- 8.Byrd JW, Jones KS. Hip arthroscopy for labral pathology: prospective analysis with 10-year follow-up. Arthroscopy. 2009;25:365–368. doi: 10.1016/j.arthro.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 9.Byrd JW, Jones KS. Hip arthroscopy in athletes: 10-year follow-up. Am J Sports Med. 2009;37:2140–2143. doi: 10.1177/0363546509337705. [DOI] [PubMed] [Google Scholar]
- 10.Byrd JW, Jones KS. Arthroscopic management of femoroacetabular impingement in athletes. Am J Sports Med. 2011;39(Suppl):7S–13S. doi: 10.1177/0363546511404144. [DOI] [PubMed] [Google Scholar]
- 11.Christensen CP, Althausen PL, Mittleman MA, Lee JA, McCarthy JC. The nonarthritic hip score: reliable and validated. Clin Orthop Relat Res. 2003;406:75–83. doi: 10.1097/00003086-200301000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Costa ML, Achten J, Parsons NR, Edlin RP, Foguet P, Prakash U, Griffin DR. Total hip arthroplasty versus resurfacing arthroplasty in the treatment of patients with arthritis of the hip joint: single centre, parallel group, assessor blinded, randomised controlled trial. BMJ. 2012;344:e2147. doi: 10.1136/bmj.e2147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ellis HB, Briggs KK, Philippon MJ. Innovation in hip arthroscopy: is hip arthritis preventable in the athlete? Br J Sports Med. 2011;45:253–258. doi: 10.1136/bjsm.2010.082529. [DOI] [PubMed] [Google Scholar]
- 14.Gedouin JE, May O, Bonin N, Nogier A, Boyer T, Sadri H, Villar RN, Laude F. Assessment of arthroscopic management of femoroacetabular impingement. A prospective multicenter study. Orthop Traumatol Surg Res. 2010;96(Suppl):S59–67. [DOI] [PubMed]
- 15.Keogh MJ, Batt ME. A review of femoroacetabular impingement in athletes. Sports Med. 2008;38:863–878. doi: 10.2165/00007256-200838100-00005. [DOI] [PubMed] [Google Scholar]
- 16.Khanduja V, Villar RN. Arthroscopic surgery of the hip: current concepts and recent advances. J Bone Joint Surg Br. 2006;88:1557–1566. doi: 10.1302/0301-620X.88B12.18584. [DOI] [PubMed] [Google Scholar]
- 17.Larson CM. Arthroscopic management of pincer-type impingement. Sports Med Arthrosc. 2010;18:100–107. doi: 10.1097/JSA.0b013e3181dc652e. [DOI] [PubMed] [Google Scholar]
- 18.Larson CM, Giveans MR. Arthroscopic management of femoroacetabular impingement: early outcomes measures. Arthroscopy. 2008;24:540–546. doi: 10.1016/j.arthro.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 19.Larson CM, Giveans MR, Taylor M. Does arthroscopic FAI correction improve function with radiographic arthritis? Clin Orthop Relat Res. 2011;469:1667–1676. doi: 10.1007/s11999-010-1741-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Malviya A, Stafford GH, Villar RN. Impact of arthroscopy of the hip for femoroacetabular impingement on quality of life at a mean follow-up of 3.2 years. J Bone Joint Surg Br. 2012;94:466–470. doi: 10.1302/0301-620X.94B4.28023. [DOI] [PubMed] [Google Scholar]
- 21.McCarthy J, Barsoum W, Puri L, Lee JA, Murphy S, Cooke P. The role of hip arthroscopy in the elite athlete. Clin Orthop Relat Res. 2003;406:71–74. doi: 10.1097/00003086-200301000-00012. [DOI] [PubMed] [Google Scholar]
- 22.McCarthy JC, Busconi B. The role of hip arthroscopy in the diagnosis and treatment of hip disease. Orthopedics. 1995;18:753–756. doi: 10.3928/0147-7447-19950801-12. [DOI] [PubMed] [Google Scholar]
- 23.McCarthy JC, Lee JA. Arthroscopic intervention in early hip disease. Clin Orthop Relat Res. 2004;429:157–162. doi: 10.1097/01.blo.0000150118.42360.1d. [DOI] [PubMed] [Google Scholar]
- 24.Nho SJ, Magennis EM, Singh CK, Kelly BT. Outcomes after the arthroscopic treatment of femoroacetabular impingement in a mixed group of high-level athletes. Am J Sports Med. 2011;39(Suppl):14S–19S. doi: 10.1177/0363546511401900. [DOI] [PubMed] [Google Scholar]
- 25.Philippon M, Schenker M, Briggs K, Kuppersmith D. Femoroacetabular impingement in 45 professional athletes: associated pathologies and return to sport following arthroscopic decompression. Knee Surg Sports Traumatol Arthrosc. 2007;15:908–914. doi: 10.1007/s00167-007-0332-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Philippon MJ, Weiss DR, Kuppersmith DA, Briggs KK, Hay CJ. Arthroscopic labral repair and treatment of femoroacetabular impingement in professional hockey players. Am J Sports Med. 2010;38:99–104. doi: 10.1177/0363546509346393. [DOI] [PubMed] [Google Scholar]
- 27.Singh PJ, O’Donnell JM. The outcome of hip arthroscopy in Australian football league players: a review of 27 hips. Arthroscopy. 2010;26:743–749. doi: 10.1016/j.arthro.2009.10.010. [DOI] [PubMed] [Google Scholar]
- 28.Valderrabano V, Pagenstert G, Horisberger M, Knupp M, Hintermann B. Sports and recreation activity of ankle arthritis patients before and after total ankle replacement. Am J Sports Med. 2006;34:993–999. doi: 10.1177/0363546505284189. [DOI] [PubMed] [Google Scholar]
- 29.Vaughn ZD, Safran MR. Arthroscopic femoral osteoplasty/chielectomy for cam-type femoroacetabular impingement in the athlete. Sports Med Arthrosc. 2010;18:90–99. doi: 10.1097/JSA.0b013e3181dfce63. [DOI] [PubMed] [Google Scholar]