Abstract
Background
Multiple radiographic parameters used for diagnosis and quantification of morphologic pincer features have emerged, but the degree to which pelvic tilt or rotation affects conventional radiography and EOS® is unknown.
Question/purposes
We asked: (1) What is the reliability of EOS® and conventional radiography at increasing sizes of morphologic pincer features with varying degrees of tilt and rotation? (2) What is the effect of tilt and rotation on acetabular overcoverage measurements?
Methods
Using a dry cadaveric pelvis, AP conventional radiographs and EOS® images were taken at intervals of increasing modeled pincer size with 0° to 15° varying tilt and rotation. Lateral center-edge angle, Sharp angle, Tönnis angle, crossover sign, and retroversion index were measured on all images. Statistical analysis was conducted.
Results
The intermodality intraclass correlation coefficients for conventional radiography and EOS® radiography across all pincer sizes, rotations, and tilts were excellent (0.93–0.98). Crossover sign was in perfect agreement in conventional radiography and EOS®. Rotation of the hip away from the beam source and/or increased anterior tilt falsely increased all overcoverage parameters except for Tönnis angle. Rotation away from the beam of 10°or greater or anterior tilt of 5° or greater produced a false-positive crossover sign.
Conclusions
EOS® radiography maintained excellent reliability in comparison to conventional radiography but both were equally vulnerable to the effects of tilt and rotation for quantification of hip parameters used in acetabular overcoverage assessment. A standardized pelvic radiograph ensuring that the pelvis is not excessively tilted or rotated should be used for assessing acetabular overcoverage parameters.
Introduction
Femoroacetabular impingement (FAI) is a well-defined disease entity, and the emerging understanding of symptomatic FAI and its associations with hip osteoarthritis have led to interest in its early diagnosis [9, 10]. Abnormal abutment motion in FAI either involves a bump on the femoral side, with resultant loss of head-neck offset (cam morphologic features), and/or overcoverage on the acetabular side (pincer morphologic features), leading to subsequent cartilage and labral degeneration [7, 9, 10, 13, 27]. Despite advances in three-dimensional (3-D) imaging (CT and MRI), quantification of pincer severity (acetabular overcoverage) continues to be based on biplanar radiographic imaging [16, 23, 29]. Limitations of biplanar radiography include subtle variations in patient positioning, which in turn can affect the reliability of radiographic parameters. The reliability of the crossover sign, a widely used parameter for diagnosis of acetabular retroversion and morphologic pincer features, is adversely affected with increased tilt and rotation of the pelvis, as noted in some studies [5, 26, 34]. In addition to the crossover sign, there are other radiographic parameters used for diagnosis and quantification of morphologic features of the pincer, but the reliability of these parameters in various tilts and rotations of the pelvis remains unknown [16, 22, 29]. We therefore sought to specifically explore the effect of pelvic tilt and rotation on these established radiographic parameters used for assessment of overcoverage.
Additionally, the EOS® imaging system (EOS Imaging Inc, Cambridge, MA, USA), is fast emerging as a low-radiation alternative to conventional radiography, and in certain circumstances, even CT for 3-D assessment [8, 12, 15, 20]. EOS® imaging uses a slot scanner that creates a horizontal fan beam and then physically moves vertically to capture the designated body part [6] as opposed to conventional radiography which uses a fixed cone beam [3]. Radiation doses of EOS® have been reported as eight to 10 times less than conventional radiography and 800 to 1000 times less than CT [15, 20, 31]. A couple studies have validated the use and reliability of EOS® in imaging of the hip and lower extremities [18, 31]. At this time, we are unaware of any studies showing the ability of EOS® to reliably measure established hip parameters in morphologic pincer features at varying degrees of tilt and rotation [27].
We therefore used a dry cadaveric pelvis with increasing interval sizes of modeled morphologic features of the pincer to answer the following study questions: (1) What is the reliability of EOS® and conventional radiography at increasing sizes of morphologic features of the pincer with varying degrees of tilt and rotation? (2) What is the effect of tilt and rotation on acetabular overcoverage measurements?
Materials and Methods
For this study, we used a dry cadaver pelvis with proximal femurs that did not show any evidence of proximal femoral deformity, acetabular dysplasia, severe degenerative sequelae, secondary osseous changes related to labral disorders (such as rim ossification or rim calcification which would create the appearance of a primary pincer), or previous surgical intervention. Institutional review board approval was not obtained, as our institution does not require approval for studies that do not involve living subjects.
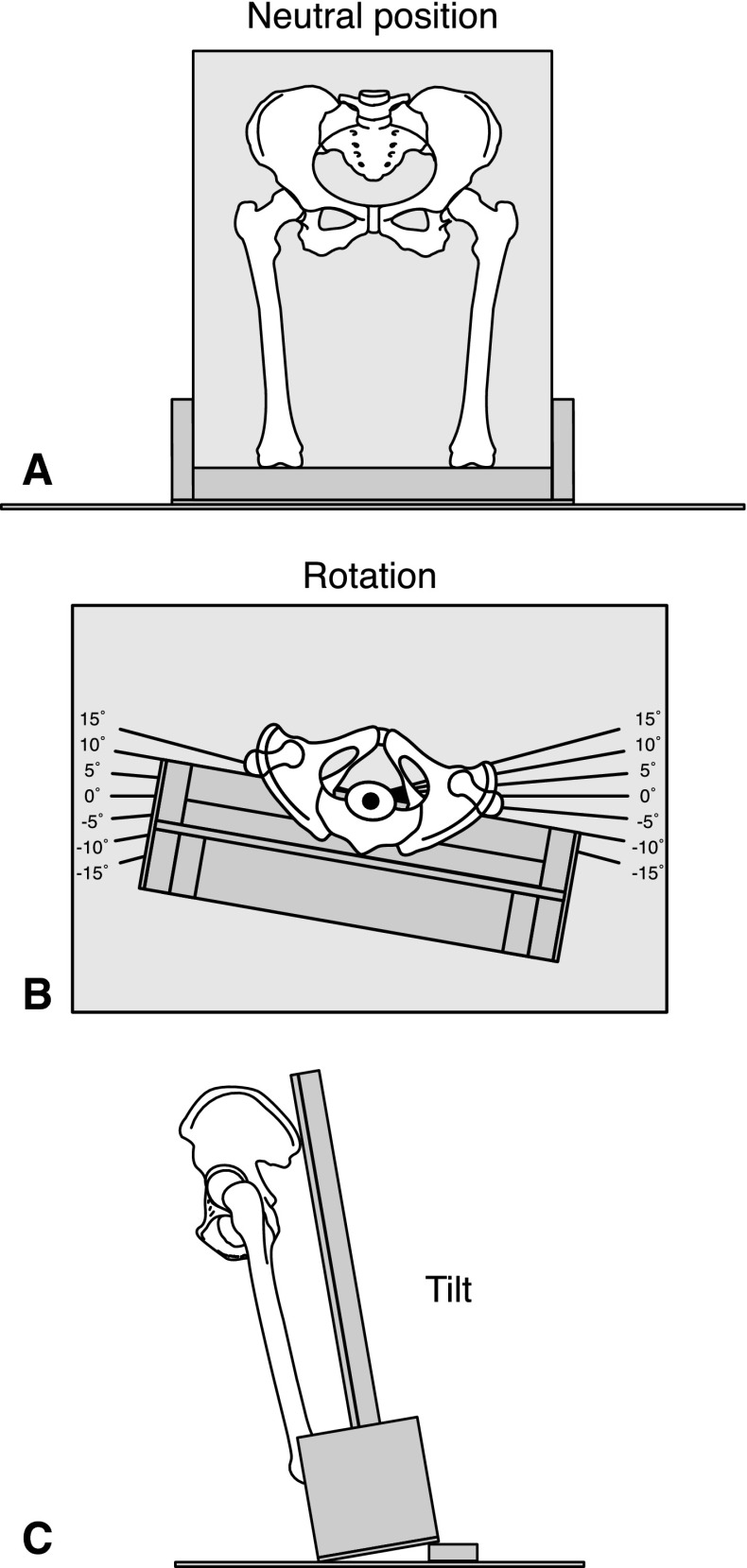
This pelvis and femur construct with neutral pelvic tilt, rotation, and inclination was securely fastened to a wood structure specifically designed for facilitation of upright imaging in EOS® and conventional radiography. Neutral position was achieved by using a carpenter zero level to align the left and right anterior superior iliac spines (ASISs) to ensure neutral rotation, align the left and right ASISs with the pubic symphysis to ensure neutral tilt, and align the left and right superior iliac spines to ensure neutral pelvic inclination. To facilitate accurate and reproducible rotations during imaging, lines were drawn from a central point on a separate square wood board delineating the neutral position (Fig. 1A) and rotations of 5°, 10°, and 15° to the left and right (Fig. 1B). The wood board then was placed under the wood structure during imaging by both modalities. Additionally, using a medical goniometer, three wooden blocks were calibrated to reproducibly create anterior and posterior tilts of 5°, 10°, and 15° when placed anteriorly or posteriorly under the wood structure (Fig. 1C).
Fig. 1A–C.
(A) The pelvis on the wood structure placed on top of the wood board is shown in the coronal plane. The pelvis is in neutral position. (B) An axial view of the pelvis on the wood structure on top of the wood board with rotation markings is shown. The pelvis is in 10° of left hip rotation and −10° of right hip rotation in this example. (C) A sagittal view of the wood structure on top of the wood board with the 10° calibrated wooden block is shown.
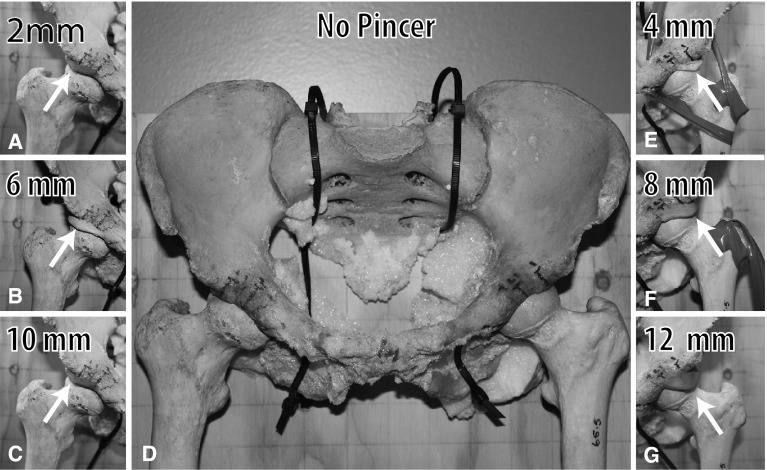
With the cadaveric pelvis in the neutral position, both acetabula were marked at the 11 o’clock, 12 o’clock, 1 o’clock, and 2 o’clock positions. EZ Shape® modeling clay (Polyform Products Co, Elk Grove Village, IL, USA), which is radiopaque, was used to create a crescent-shaped addition to the acetabular rim. This addition was built over the 11 o’clock to 2 o’clock positions with the maximal lateral extension at the 1 o’clock position to represent typically reported morphologic features of the pincer [27]. Interval sizes of morphologic features of the pincer were created by measuring the lateral extension at the 1 o’clock position on the cadaveric acetabulum (Fig. 2). Three sets of pincers 2 mm/4 mm, 6 mm/8 mm, and 10 mm/12 mm on the right and left acetabulum, respectively, were created (Fig. 3). The cadaveric proximal femurs were placed at 0° neutral and anatomic rotation by positioning the femoral neck parallel to the wood structure [4, 11, 33].
Fig. 2.

A caliper is used to measure the modeled pincer at the 1 o’clock position (in this case 12 mm). The pincer then is contoured into a crescent shape from the 11 to 2 o’clock position of the acetabulum with the most lateral edge or peak of the crescent at the 1 o’clock position.
Fig. 3A–G.
The left column shows (A) 2 mm, (B) 6 mm, and (C) 10 mm pincer sizes of the right hip. (D) The dry cadaveric pelvis without any modeled morphologic features of the pincer morphology is shown. The right column shows (E) 4 mm, (F) 8 mm, and (G) 12 mm pincer sizes of the left hip.
Certified radiology technicians (NM, DRA) obtained sequential AP images of the cadaveric pelvis and proximal femur model with 5° intervals of tilt and then 5° intervals of rotation with conventional radiography and EOS® imaging (a total of 13 with each modality). This was performed without any modeled morphologic pincer features and repeated for each interval of pincer size for a total of four sets of EOS® and conventional radiography images (104 total images). Degree of rotation or tilt that brought an individual hip or the whole pelvis (anterior tilt), respectively, toward the beam was labeled positive, and degree of rotation or tilt that brought an individual hip or the whole pelvis (posterior tilt), respectively, away from the beam was labeled negative.
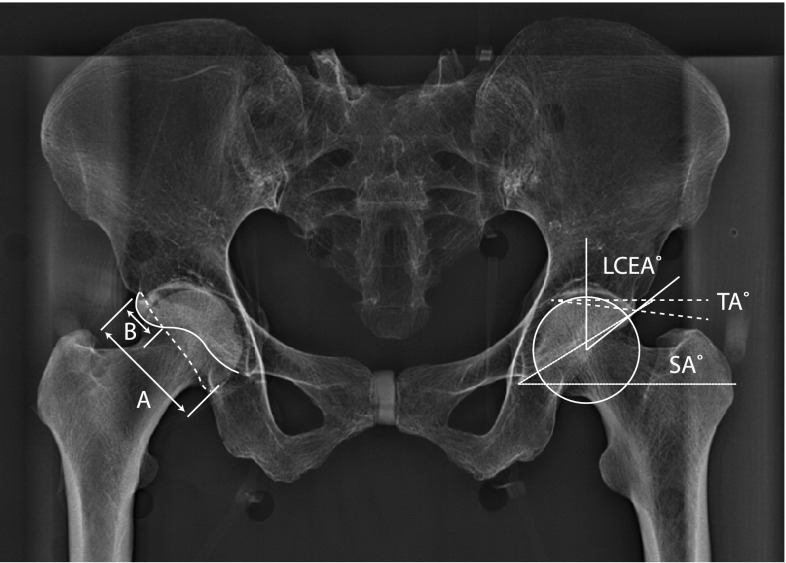
Using PACS imaging software (LightViewTM, AMICAS VisionTM Series PACS v. 5.0; AMICAS, Inc, Brighton, MA, USA), one physician observer (SM) performed measurements of multiple acetabular coverage parameters on EOS® and conventional radiographs, including lateral center-edge angle [35], Sharp’s angle [25], Tönnis angle [32], crossover sign [23], and retroversion index [26] (Fig. 4).
Fig. 4.
An AP EOS® image shows the dry cadaveric pelvis with 2- and 4-mm pincers. A crossover sign is considered positive when the anterior rim crosses the posterior rim. This is seen in the right hip by crossing of the dotted line (posterior rim) and solid line (anterior rim). The distance of the superior lateral edge of the weightbearing zone to the crossover of the anterior and posterior rim (B) divided by the entire length of lateral acetabular opening (A) constituted the retroversion index (A/B). The angle formed by a line from the inferior pelvic teardrop to the superior lateral edge of the acetabulum and a line horizontal from the inferior pelvic teardrop constituted the Sharp angle (SA). The lateral center-edge angle (LCEA) was formed by a line vertical from the center of the femoral head and a line from center of the femoral head to the superior lateral edge of the acetabulum. The Tönnis angle (TA) was formed by a horizontal line from the medial portion of the weightbearing zone (ie, sclerotic zone) and a line from the medial portion of the weightbearing zone to the superior lateral edge of the acetabulum. As the dry cadaveric pelvis had neutral inclination, no inclination compensatory methods were needed for lateral center-edge angle, Sharp angle, and Tönnis angle.
All statistical analyses were performed using SPSS® (Version 12; SPSS Inc, Chicago, IL, USA). Intermodality reliability for each measure was analyzed using intraclass correlation coefficients (ICCs). ICCs typically have a range of between 0.0 and 1.0, with values closer to 1.0 representing stronger agreement. The two-way mixed model in absolute agreement was used. Multiple linear regression analysis was performed to evaluate the effect of rotation and radiographic modality on lateral center-edge angle, Sharp angle, Tönnis angle, and retroversion index. The regression analysis was repeated to evaluate the effect of tilt, rotation, and modality on the same four measures.
Results
The overall reliability between conventional radiography and EOS® imaging across all pincer sizes, tilts, and rotations was excellent. With the numbers available, there was no difference between conventional radiography and EOS in these parameters. The overall intermodality ICCs for conventional radiography and EOS® across all pincer sizes, rotations, and tilts were 0.98 (95% CI, 0.97–0.99) (p < 0.001) for lateral center-edge angle, 0.93 (95% CI, 0.85–0.96) (p < 0.001) for Sharp angle, 0.96 (95% CI, 0.94–0.97) (p < 0.001) for Tönnis angle, and 0.96 (95% CI, 0.93–0.97) (p < 0.001) for retroversion index. The crossover sign was positive or negative in perfect agreement in all cases in conventional radiography and EOS®. Intermodality ICCs stratified by pincer size (Table 1), rotation (Table 2), and tilt (Table 3) remained excellent.
Table 1.
Intermodality conventional radiography versus EOS® ICCs by pincer size
| Pincer size (mm) | ICC (95% CI)* | |||
|---|---|---|---|---|
| Lateral center-edge angle | Sharp angle | Tönnis angle | Retroversion index | |
| 0 | 0.88 (0.72–0.95) | 0.71 (0.28–0.88) | 0.79 (0.58–0.90) | 0.87 (0.53–0.97) |
| 2 | 0.92 (0.54–0.98) | 0.76 (0.41–0.92) | 0.89 (0.66–0.96) | 0.92 (0.74–0.98) |
| 4 | 0.93 (0.79–0.98) | 0.86 (0.79–0.98) | 0.89 (0.68–0.97) | 0.98 (0.95–1.00) |
| 6 | 0.89 (0.65–0.97) | 0.90 (0.60–0.97) | 0.90 (0.72–0.97) | 0.97 (0.90–0.99) |
| 8 | 0.94 (0.81–0.98) | 0.77 (0.72–0.95) | 0.85 (0.29–0.96) | 0.95 (0.84–0.98) |
| 10 | 0.94 (0.83–0.98) | 0.71 (−0.05 to 0.92) | 0.77 (0.41–0.92) | 0.95 (0.84–0.98) |
| 12 | 0.97 (0.89–0.99) | 0.79 (0.02–0.95) | 0.90 (0.71–0.97) | 0.95 (0.85–0.98) |
* All ICCs have a p < 0.001; ICC = intraclass correlation coefficient.
Table 2.
Intermodality conventional radiography versus EOS® ICCs by rotation
| Rotation | ICC (95% CI) | |||
|---|---|---|---|---|
| Lateral center-edge angle | Sharp angle | Tönnis angle | Retroversion index | |
| Right 15° | 0.98 (0.93–1.00) | 0.98 (0.66–1.00) | 0.98 (0.90–1.00) | 0.91 (0.50–0.99) |
| Right 10° | 0.98 (0.89–1.00) | 0.96 (0.55–0.99) | 0.98 (0.91–1.00) | 0.88 (0.51–0.98)* |
| Right 5° | 0.99 (0.93–1.00) | 0.91 (0.56–0.98) | 0.99 (0.96–1.00) | 0.99 (0.95–1.00)† |
| Neutral | 0.99 (0.95–1.00) | 0.96 (0.80–0.99) | 0.95 (0.81–0.99) | 0.89 (0.37–0.98)‡ |
| Left 5° | 0.97 (0.86–0.99) | 0.98 (0.34–1.00) | 0.99 (0.89–1.00) | 0.82 (0.19–0.97)‡ |
| Left 10° | 0.99 (0.95–1.00) | 0.97 (0.64–0.99) | 0.96 (0.83–0.99) | 0.90 (0.54–0.98)* |
| Left 15° | 0.98 (0.93–1.00) | 0.93 (0.60–0.99) | 0.98 (0.90–1.00) | 0.93 (0.68–0.99) |
* p = 0.001; †p = 0.003; ‡p = 0.005; otherwise, all ICCs have a p < 0.001; ICC = intraclass correlation coefficient.
Table 3.
Intermodality conventional radiography versus EOS® ICCs by tilt
| Tilt | ICC (95% CI) | |||
|---|---|---|---|---|
| Lateral center-edge angle | Sharp angle | Tönnis angle | Retroversion index | |
| Posterior 15° | 0.96 (0.83–0.99) | 0.93 (0.69–0.98) | 0.96 (0.84–0.99) | 0.94 (0.64–0.99) |
| Posterior 10° | 0.98 (0.89–1.00) | 0.97 (0.86–0.99) | 0.94 (0.75–0.99) | 0.82 (0.12–0.97)* |
| Posterior 5° | 0.99 (0.94–1.00) | 0.90 (0.57–0.98) | 0.97 (0.87–0.99) | 0.90 (0.14–0.99)† |
| Neutral | 0.99 (0.95–1.00) | 0.96 (0.80–0.99) | 0.95 (0.81–0.99) | 0.89 (0.37–0.98) |
| Anterior 5° | 0.99 (0.94–1.00) | 0.90 (0.60–0.98) | 0.94 (0.39–0.99) | 0.93 (0.66–0.99)† |
| Anterior 10° | 0.97 (0.71–1.00) | 0.87 (0.29–0.98) | 0.92 (0.66–0.98) | 0.92 (0.68–0.98) |
| Anterior 15° | 0.97 (0.79–1.00) | 0.83 (−0.04 to 0.97) | 0.91 (0.27–0.99) | 0.85 (0.46–0.97)† |
* p = 0.004; †p = 0.001; otherwise, all ICCs have a p < 0.001; ICC = intraclass correlation coefficient.
We found rotation affected all measurements and tilt affected all measurements except for Tönnis angle. The multiple linear regression analysis also corroborated our ICC findings in that modality of imaging did not affect lateral center-edge angle, Sharp angle, Tönnis angle, and retroversion index. For each additional degree of increase in rotation (rotation toward the beam), the lateral center-edge angle decreased by 0.3° (p < 0.001), Sharp angle increased by 0.1° (p < 0.001), Tönnis angle increased by 0.3° (p < 0.001), and retroversion index decreased by 0.01 (p < 0.001) (Table 4). For each additional degree of increase in tilt (tilt toward the beam), the lateral center-edge angle increased by 0.4° (p < 0.001), Sharp angle decreased by 0.2° (p < 0.001), and retroversion index increased by 0.02 (p < 0.001) (Table 5). Additionally, pincer sizes of 2 to 12 mm in EOS® and conventional radiography in all rotations and tilt showed a crossover sign except for a pincer size of 2 mm at rotation of positive 15°. At a pincer size of 0 mm in the neutral position, neither hip had a positive crossover sign in EOS® or conventional radiography. At a negative rotation of 10° and 15°, both hips had a positive crossover sign in EOS® and conventional radiography, falsely indicating acetabular retroversion. At a positive tilt of 5° or more for the right hip and 10° or more for the left hip, there was a positive crossover sign in EOS® and conventional radiography, falsely indicating acetabular retroversion.
Table 4.
Linear regression of the effect of rotation and change in modality on hip parameters
| Hip parameter | R2 | Change in measurement with every 1° rotation toward the beam | Was change in modality significant? |
|---|---|---|---|
| Lateral center-edge angle | 0.135 | −0.332° (p < 0.001) | No (p = 0.912) |
| Sharp angle | 0.113 | 0.125° (p < 0.001) | No (p = 0.227) |
| Tönnis angle | 0.265 | 0.276° (p < 0.001) | No (p = 0.227) |
| Retroversion index | 0.298 | −0.009° (p < 0.001) | No (p = 0.227) |
Table 5.
Linear regression of the potential effect of tilt and change in modality on hip parameters
| Hip parameter | R2 | Change in measurement with every 1° increase in anterior tilt | Was change in modality significant? |
|---|---|---|---|
| Lateral center-edge angle | 0.190 | 0.420 (p < 0.001) | No (p = 0.814) |
| Sharp angle | 0.205 | −0.204° (p < 0.001) | No (p = 0.373) |
| Tönnis angle | 0.030 | −0.079° (p = 0.083) | No (p = 0.597) |
| Retroversion index | 0.782 | 0.018° (p < 0.001) | No (p = 0.979) |
Discussion
We have continued to increase our understanding of the clinical features, natural history, and radiographic assessment of FAI since its original description in 2001 [13]. FAI is increasingly being considered a major differential diagnosis in young patients presenting with nonspecific groin and hip pain with activity, leading to additional need for reliable diagnostic tools and criteria [21]. Standard imaging workup for these patients begins with AP biplanar radiography of the pelvis (using either conventional radiography or EOS® imaging). However, biplanar radiography with either technique may be limited by some variation in pelvic tilt, magnification, and femoral rotation [2, 19, 26, 28, 30, 34], which must be identified and accounted for when interpreting these biplanar radiographs. We therefore used a dry cadaveric pelvis with increasing interval sizes of modeled morphologic features of the pincer to answer the following study questions: (1) What is the reliability of EOS® and conventional radiography at increasing sizes of morphologic features of the pincer with varying degrees of tilt and rotation? (2) What is the effect of tilt and rotation on acetabular overcoverage measurements?
There are some limitations to our study. One limitation was in using a dry cadaveric pelvis and proximal femur with no capsule, soft tissues, or cartilage. This resulted in little to no joint space and manifested as abnormally high lateral center-edge angle measurements owing to the medialization of the center of the femoral head. However, our study questions were not related to the absolute lateral center-edge angle measurements but rather its agreement between modalities and the relative effect of rotation and tilt. A second limitation was the use of molding clay to model morphologic features of the pincer. In addressing this limitation, we used a substance that had similar opacity to bone. Additionally, the pincer was designed to match previous literature descriptions of the morphologic features, and at each interval size, it was validated by the senior author (HSH) who has extensive surgical experience with open treatment of FAI. A third limitation was the use of only one cadaver with morphologic features of the hip that obviously were individual to it. To address this limitation, we used a normal cadaver with no evidence of gross deformities, previous surgery, or severe arthritis that may have affected the results. A fourth limitation was the method used in tilting the pelvis, which was done by tilting the bottom of the wood structure. This resulted in increasing (posterior tilt) and decreasing (anterior tilt) distances of the beam to the pelvis in EOS® and conventional radiography. In normal clinical situations, this is often a variable not fully controlled that largely depends on patient positioning, radiography technician, and the level of compliance of the patient. Additionally, the effect, if any, of this variability likely decreased the resulting reliability between EOS® and conventional radiography in tilt and provided an important insight into the differing effect of position in EOS® and conventional radiography, as discussed below.
The overall reliability between EOS® and conventional radiography was excellent, as seen by intermodality ICCs greater than 0.90 in all measurements between EOS® and conventional radiography. Stratified by pincer size, rotation, and tilt, the intermodality ICCs showed excellent reliability between EOS® and conventional radiography in morphologic features of the pincer. Our study also is consistent with previous EOS® imaging studies, which all showed an image quality of EOS® comparable to improved compared with that of conventional radiography [1, 6, 17, 18, 20, 24, 31]. However, we did see relative horizontal widening of the image in EOS® with extreme anterior tilt (≥ 10°) and horizontal narrowing in extreme posterior tilt (≥ 10°) owing to the decrease or increase in distance between the x-ray beam and the pelvis (Fig. 5). This did not decrease the reliability of the hip measurements, likely owing to the symmetric widening or narrowing, but did show a slightly different overall image from conventional radiography. EOS® imaging uses a slot scanner that creates a horizontal fan beam and then physically moves vertically to capture the designated body part [6], in contrast to conventional radiography which uses a fixed cone beam [3]. We postulate, in extreme tilts, the minor distortion of the image is attributable to the relative magnification in the horizontal plane caused by the divergent horizontal beam, which becomes contrasted to the lack of magnification effect in the vertical plane. Continued education, guidance, and awareness of the effect of patient positioning are recommended as EOS® imaging becomes more widely used.
Fig. 5A–C.

AP EOS® images show the dry cadaveric pelvis with 6- and 8-mm pincers at (A) neutral position, (B) anterior tilt of 15°, and (C) posterior tilt of 15°. Horizontal widening and narrowing can be seen in the anterior tilt of 15° and posterior tilt of 15°, respectively.
Multiple linear regression analysis showed pelvic rotation affected all measurements and pelvic tilt affected all measurements except Tönnis angle. Additionally, change in modality did not affect measurements, indicating this effect was shared by EOS® and conventional radiography. Generally, we found, as the hip rotated away from the beam, the anterior rim and/or pincer became more prominent, resulting in the measured parameters showing increased acetabular coverage (increase in lateral center-edge angle and retroversion index, decrease in Sharp angle and Tönnis angle). As the hip rotated away from the beam, the anterior rim and/or pincer became less prominent, resulting in the measured parameters showing decreased acetabular coverage (decrease in lateral center-edge angle and retroversion index, increase in Sharp angle and Tönnis angle). Except for Tönnis angle, as the pelvis tilted anteriorly toward or posteriorly away from the beam, the acetabular parameters showed increased or decreased acetabular coverage, respectively. Consistent with our findings from a cadaver with varying abnormal morphologic features of the pincer, Jacobsen et al. [14] found rotation and tilt affected lateral center-edge angle and Sharp angle in two cadavers with normal morphologic features of the hip. Siebenrock et al. [26] found an anterior tilt of 9° and rotation of 6° away from the x-ray beam produced a crossover sign in every pelvis. Similarly, in our study, we found a tilt of 10° or more anteriorly or rotation toward the beam of 10° or more produced a crossover sign in both hips falsely indicating acetabular retroversion when none was apparent at the neutral position. Interestingly, if a crossover was apparent at the neutral position, except for the 2-mm position at 15° rotation, no amount of rotation or tilt resulted in the loss of crossover sign, showing this sign is sensitive but may not be specific to retroversion when tilt and rotation are not corrected.
Conventional radiography and recently established EOS® imaging continue to be vital diagnostic tools, especially in conditions such as FAI. Additionally, the global availability and low cost of conventional radiography and the decreased radiation associated with EOS® remain strong factors related to their continued use. Unfortunately, there remains variability in patient position, especially in new modalities. Our study clearly showed tilt and rotation affect the appearance and quantification of a multitude of hip parameters used in acetabular overcoverage assessment. A standardized pelvic radiograph ensuring that the pelvis is not excessively tilted or rotated should be used for assessing acetabular overcoverage parameters.
Acknowledgments
We thank Natalie McNeil RT, for assistance with conventional radiography acquisition and Dave R. Andrews RT, for assistance with EOS® acquisition.
Footnotes
The institution of the authors has received, during the study period, funding from EOS Imaging Inc (Cambridge, MA, USA).
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This study was performed at Rady Children’s Hospital, San Diego, CA, USA.
References
- 1.Azmy C, Guerard S, Bonnet X, Gabrielli F, Skalli W. EOS orthopaedic imaging system to study patellofemoral kinematics: assessment of uncertainty. Orthop Traumatol Surg Res. 2010;96:28–36. doi: 10.1016/j.otsr.2009.10.013. [DOI] [PubMed] [Google Scholar]
- 2.Bell AL, Brand RA. Roentgenographic changes in proximal femoral dimensions due to hip rotation. Clin Orthop Relat Res. 1989;240:194–199. [PubMed] [Google Scholar]
- 3.Bushberg JT. The Essential Physics of Medical Imaging. Philadelphia, PA: Lippincott Williams & Wilkins; 2002. [Google Scholar]
- 4.Clohisy JC, Carlisle JC, Beaule PE, Kim YJ, Trousdale RT, Sierra RJ, Leunig M, Schoenecker PL, Millis MB. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90(suppl 4):47–66. doi: 10.2106/JBJS.H.00756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dandachli W, Najefi A, Iranpour F, Lenihan J, Hart A, Cobb J. Quantifying the contribution of pincer deformity to femoro-acetabular impingement using 3D computerised tomography. Skeletal Radiol. 2012;41:1295–1300. doi: 10.1007/s00256-012-1389-2. [DOI] [PubMed] [Google Scholar]
- 6.Deschenes S, Charron G, Beaudoin G, Labelle H, Dubois J, Miron MC, Parent S. Diagnostic imaging of spinal deformities: reducing patients radiation dose with a new slot-scanning X-ray imager. Spine (Phila Pa 1976). 2010;35:989–994. [DOI] [PubMed]
- 7.Dolan MM, Heyworth BE, Bedi A, Duke G, Kelly BT. CT reveals a high incidence of osseous abnormalities in hips with labral tears. Clin Orthop Relat Res. 2011;469:831–838. doi: 10.1007/s11999-010-1539-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dubousset J, Charpak G, Dorion I, Skalli W, Lavaste F, Deguise J, Kalifa G, Ferey S. [A new 2D and 3D imaging approach to musculoskeletal physiology and pathology with low-dose radiation and the standing position: the EOS system][in French] Bull Acad Natl Med. 2005;189:287–297. [PubMed] [Google Scholar]
- 9.Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466:264–272. doi: 10.1007/s11999-007-0060-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 11.Hananouchi T, Sugano N, Nakamura N, Nishii T, Miki H, Yamamura M, Yoshikawa H. Preoperative templating of femoral components on plain X-rays: rotational evaluation with synthetic X-rays on ORTHODOC. Arch Orthop Trauma Surg. 2007;127:381–385. doi: 10.1007/s00402-007-0349-0. [DOI] [PubMed] [Google Scholar]
- 12.Hoan NN, Majewski S, Charpak G, Policarpo AJ. An efficient, gaseous detector with good low-energy resolution for (less than or equal to 50 keV) imaging. J Nucl Med. 1979;20:335–340. [PubMed] [Google Scholar]
- 13.Ito K, Minka MA, 2nd, Leunig M, Werlen S, Ganz R. Femoroacetabular impingement and the cam-effect: a MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br. 2001;83:171–176. doi: 10.1302/0301-620X.83B2.11092. [DOI] [PubMed] [Google Scholar]
- 14.Jacobsen S, Sonne-Holm S, Lund B, Soballe K, Kiaer T, Rovsing H, Monrad H. Pelvic orientation and assessment of hip dysplasia in adults. Acta Orthop Scand. 2004;75:721–729. doi: 10.1080/00016470410004094. [DOI] [PubMed] [Google Scholar]
- 15.Kalifa G, Charpak Y, Maccia C, Fery-Lemonnier E, Bloch J, Boussard JM, Attal M, Dubousset J, Adamsbaum C. Evaluation of a new low-dose digital x-ray device: first dosimetric and clinical results in children. Pediatr Radiol. 1998;28:557–561. doi: 10.1007/s002470050413. [DOI] [PubMed] [Google Scholar]
- 16.Kutty S, Schneider P, Faris P, Kiefer G, Frizzell B, Park R, Powell JN. Reliability and predictability of the centre-edge angle in the assessment of pincer femoroacetabular impingement. Int Orthop. 2012;36:505–510. doi: 10.1007/s00264-011-1302-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lazennec JY, Rangel A, Baudoin A, Skalli W, Catonne Y, Rousseau MA. The EOS imaging system for understanding a patellofemoral disorder following THR. Orthop Traumatol Surg Res. 2011;97:98–101. doi: 10.1016/j.otsr.2010.07.010. [DOI] [PubMed] [Google Scholar]
- 18.Lazennec JY, Rousseau MA, Rangel A, Gorin M, Belicourt C, Brusson A, Catonne Y. Pelvis and total hip arthroplasty acetabular component orientations in sitting and standing positions: measurements reproductibility with EOS imaging system versus conventional radiographies. Orthop Traumatol Surg Res. 2011;97:373–380. doi: 10.1016/j.otsr.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 19.Linclau L, Dokter G, Peene P. Radiological aspects in preoperative planning and postoperative assessment of cementless total hip arthroplasty. Acta Orthop Belg. 1993;59:163–167. [PubMed] [Google Scholar]
- 20.McKenna C, Wade R, Faria R, Yang H, Stirk L, Gummerson N, Sculpher M, Woolacott N. EOS 2D/3D X-ray imaging system: a systematic review and economic evaluation. Health Technol Assess. 2012;16:1–188. doi: 10.3310/hta16140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ochoa LM, Dawson L, Patzkowski JC, Hsu JR. Radiographic prevalence of femoroacetabular impingement in a young population with hip complaints is high. Clin Orthop Relat Res. 2010;468:2710–2714. doi: 10.1007/s11999-010-1233-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Philippon MJ, Wolff AB, Briggs KK, Zehms CT, Kuppersmith DA. Acetabular rim reduction for the treatment of femoroacetabular impingement correlates with preoperative and postoperative center-edge angle. Arthroscopy. 2010;26:757–761. doi: 10.1016/j.arthro.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 23.Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum: a cause of hip pain. J Bone Joint Surg Br. 1999;81:281–288. doi: 10.1302/0301-620X.81B2.8291. [DOI] [PubMed] [Google Scholar]
- 24.Schlatterer B, Suedhoff I, Bonnet X, Catonne Y, Maestro M, Skalli W. Skeletal landmarks for TKR implantations: evaluation of their accuracy using EOS imaging acquisition system. Orthop Traumatol Surg Res. 2009;95:2–11. doi: 10.1016/j.otsr.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 25.Sharp IK. Acetabular dysplasia: the acetabular angle. J Bone Joint Surg Br. 1961;43:268–272. [Google Scholar]
- 26.Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res. 2003;407:241–248. doi: 10.1097/00003086-200302000-00033. [DOI] [PubMed] [Google Scholar]
- 27.Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion: treatment with periacetabular osteotomy. J Bone Joint Surg Am. 2003;85:278–286. doi: 10.2106/00004623-200302000-00015. [DOI] [PubMed] [Google Scholar]
- 28.Tannast M, Mistry S, Steppacher SD, Reichenbach S, Langlotz F, Siebenrock KA, Zheng G. Radiographic analysis of femoroacetabular impingement with Hip2Norm-reliable and validated. J Orthop Res. 2008;26:1199–1205. doi: 10.1002/jor.20653. [DOI] [PubMed] [Google Scholar]
- 29.Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis—what the radiologist should know. AJR Am J Roentgenol. 2007;188:1540–1552. doi: 10.2214/AJR.06.0921. [DOI] [PubMed] [Google Scholar]
- 30.Tannast M, Zheng G, Anderegg C, Burckhardt K, Langlotz F, Ganz R, Siebenrock KA. Tilt and rotation correction of acetabular version on pelvic radiographs. Clin Orthop Relat Res. 2005;438:182–190. doi: 10.1097/01.blo.0000167669.26068.c5. [DOI] [PubMed] [Google Scholar]
- 31.Than P, Szuper K, Somoskeoy S, Warta V, Illes T. Geometrical values of the normal and arthritic hip and knee detected with the EOS imaging system. Int Orthop. 2012;36:1291–1297. doi: 10.1007/s00264-011-1403-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tönnis D. Congenital Dysplasia and Dislocation of the Hip in Children and Adults. Berlin, Germany: Springer-Verlag; 1987. [Google Scholar]
- 33.Toogood PA, Skalak A, Cooperman DR. Proximal femoral anatomy in the normal human population. Clin Orthop Relat Res. 2009;467:876–885. doi: 10.1007/s11999-008-0473-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wassilew GI, Heller MO, Diederichs G, Janz V, Wenzl M, Perka C. Standardized AP radiographs do not provide reliable diagnostic measures for the assessment of acetabular retroversion. J Orthop Res. 2012;30:1369–1376. doi: 10.1002/jor.22086. [DOI] [PubMed] [Google Scholar]
- 35.Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint: with special referance to the complication of osteoarthritis. Acta Chir Scand Suppl. 1939;83(suppl 58):1–135. [Google Scholar]