Abstract
Background
The evolution of total hip arthroplasty (THA) generally has led to improved clinical results. However, THA in very young patients historically has been associated with lower survivorship, and it is unclear whether this, or results pertaining to pain and function, has improved with contemporary THA.
Questions/purposes
We performed a systematic review of the English literature on THA in patients 30 years of age and younger to assess changes in (1) indications; (2) implant selection; (3) clinical and radiographic outcomes; and (4) survivorship when comparing contemporary and historical reports.
Methods
Multiple databases were searched for articles published between 1965 and 2011 that reported clinical and radiographic outcomes of THA in patients 30 years and younger. Sixteen retrospective case series were identified. Surgical indications, implant selection, clinical and radiographic outcomes, and survivorship of patients undergoing THAs before 1988 were compared with those performed in 1988 and after.
Results
Reported THAs performed more recently were less likely to be performed for juvenile rheumatoid arthritis than earlier procedures. Cementless fixation became more prevalent in later years. Although clinical outcome scores remained constant, aseptic loosening and revision rates decreased substantially with more contemporary procedures.
Conclusions
This review of the literature demonstrates an improvement in radiographic outcomes and survivorship of THA, but no significant differences in pain and function scores, in very young patients treated over the past two decades when compared with historical controls.
Introduction
THA is a highly effective treatment for end-stage degenerative disease [16]. Various refinements in surgical technique and implant design such as cementless fixation and development of highly crosslinked polyethylene have contributed to improvement in pain, function, and overall survivorship of the implant [7, 8, 25]. Although THA was originally intended for elderly, low-demand patients, trends in contemporary practice indicate an increasing number of procedures are being performed in much younger patients [21, 29]. Historically, very young patients (defined as those 30 years of age and younger [4]) have not experienced the same survivorship as their older counterparts. This has been attributed to an antiquated surgical technique and the use of THA in patients with juvenile rheumatoid arthritis [5, 6, 14, 22, 23, 26]. However, it is unclear whether young patients have benefitted from improving outcomes afforded by contemporary THA. The purpose of this study was to perform a systematic review of the English literature on THA in patients 30 years of age and younger to assess changes in (1) indications; (2) implant selection; (3) clinical and radiographic outcomes; and (4) survivorship when comparing contemporary and historical reports.
Materials and Methods
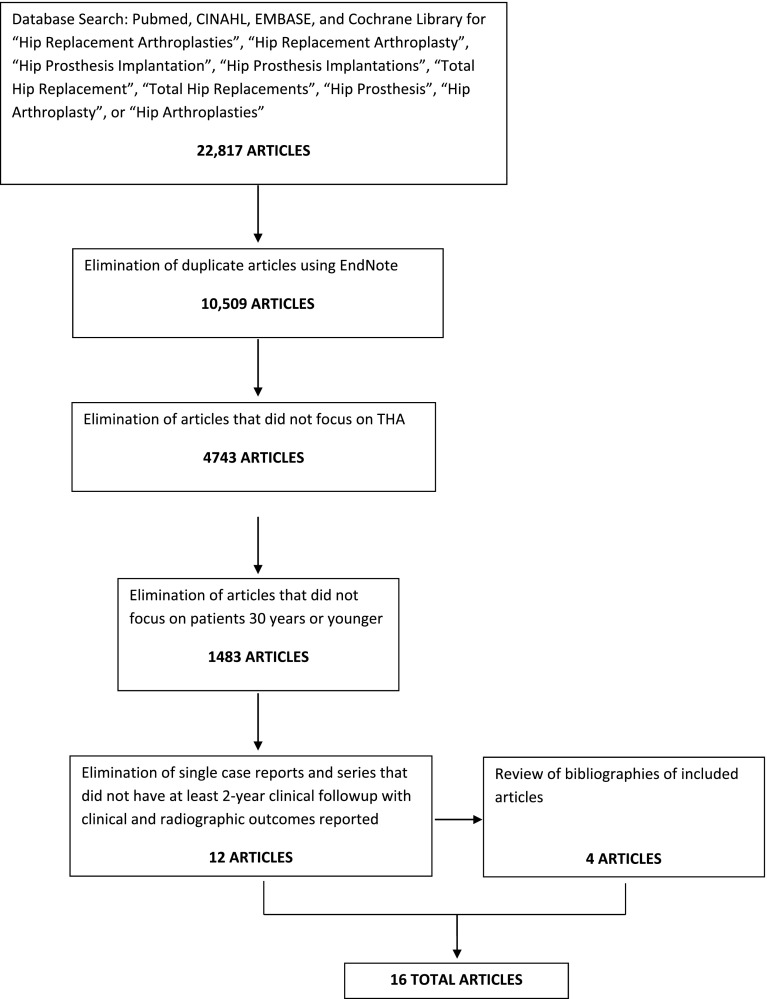
Multiple databases, including PubMed, Cumulative Index to Nursing and Allied Health (CINAHL), EMBASE, and the Cochrane Library, were searched for articles published between 1965 and 2011 using the following search filter: “Hip Replacement Arthroplasties” OR “Hip Replacement Arthroplasty” OR “Hip Prosthesis Implantation” OR “Hip Prosthesis Implantations” OR “Total Hip Replacement” OR “Total Hip Replacements” OR “Hip Prosthesis” OR “Hip Arthroplasty” OR “Hip Arthroplasties”. A total of 22,817 articles were identified on the subject matter (Fig. 1). The articles were combined into EndNote and were reviewed manually, resulting in the exclusion of 12,308 duplicate articles. Of the remaining 10,509 articles, 5766 were excluded because THA was not the main focus and 3260 did not meet the age criteria of 30 years or younger. The remaining articles were reviewed independently by two authors (MA, AP) for inclusion based on the following criteria: minimum 2-year clinical followup, reported clinical outcome measures, and reported radiographic outcomes. Single case reports were excluded. Twelve studies met our criteria. The bibliographies of these articles were then reviewed, yielding an additional four studies. A total of 16 studies were included in this systematic review [1–4, 6, 10, 12, 13, 18–20, 27, 28, 30, 32, 33].
Fig. 1.
This flowchart depicts identification of articles included in the systematic review.
Each study was reviewed in detail by one author (MAA) for level of evidence, study type, demographic information, surgical indications, years in which arthroplasties were performed, surgical details, clinical outcome measures, and radiographic results. All studies were retrospective case series. The studies had an average of 46 hips (range, 10–102 hips) in 33 patients (range, six to 88 patients). A total of 736 THAs were performed in 542 patients. The average patient age was 21 years (range, 9–30 years). The minimum followup was 2 years (mean, 9.5 years; range, 2–30 years). These studies were then stratified according to the years when THA was performed. Two groups were created: studies in which all, or the majority of, procedures were performed before 1988 (Group I) and those in which surgeries were performed in 1988 or later (Group II). The year, 1988, was selected because it is the midpoint of the overall timespan during which arthroplasties in this review were performed (1969–2008).
The pooled patient populations in each group were described using descriptive statistics. Mean age, followup, and clinical outcome measures were calculated by weighted average. The frequency of each primary hip diagnosis, component fixation technique, and bearing surface was calculated. Acetabular and femoral component loosening rates were calculated. Overall revision rates as well as rates of acetabular and femoral component revision were calculated. Reported indications for THA, component fixation technique, bearing surface, clinical and radiographic outcomes, and survivorship were compared between the two groups. Student’s t-test was used to compare clinical outcome scores between the two groups. Differences in loosening and revision rates were assessed with the chi-square test.
Results
Overall, the most common primary hip diagnosis in these studies was juvenile rheumatoid arthritis (36.3%) followed by avascular necrosis (22.6%) and developmental dysplasia of the hip (12.8%). Before 1988 (Group I), THA was mostly performed for juvenile rheumatoid arthritis (49.5%). Avascular necrosis (34.8%) became the predominant hip diagnosis for patients undergoing THA in 1988 and later (Group II) (Table 1).
Table 1.
Primary hip diagnoses in patients 30 years of age and younger undergoing THA
| Diagnosis | Group I | Percent | Group II | Percent | Total | Percent | p value |
|---|---|---|---|---|---|---|---|
| Juvenile rheumatoid arthritis | 164 | 49.5 | 103 | 25.4 | 267 | 36.2 | 1.30 × 10−11 |
| Developmental dysplasia of the hip | 35 | 10.6 | 59 | 14.6 | 94 | 12.8 | 0.10 |
| Posttraumatic osteoarthritis | 27 | 8.2 | 11 | 2.7 | 38 | 5.2 | 0.0009 |
| Avascular necrosis | 25 | 7.6 | 141 | 34.8 | 166 | 22.6 | 1.33 × 10−18 |
| Other | |||||||
| Ankylosing spondylitis | 24 | 7.3 | 6 | 1.5 | 30 | 4.1 | |
| Perthes’ disease | 11 | 3.3 | 22 | 5.4 | 33 | 4.5 | |
| Septic arthritis | 10 | 3.0 | 6 | 1.5 | 16 | 2.2 | |
| Slipped capital femoral epiphysis | 9 | 2.7 | 16 | 4.0 | 25 | 3.4 | |
| Acute fracture | 0 | 0 | 4 | 0.99 | 4 | 0.54 | |
| Other skeletal dysplasias | |||||||
| Multiple epiphyseal dysplasia | 2 | 0.60 | 5 | 1.2 | 7 | 0.95 | |
| Spondyloepiphyseal dysplasia | 0 | 0 | 3 | 0.74 | 3 | 0.41 | |
| Proximal focal femoral deficiency | 1 | 0.30 | 0 | 0 | 1 | 0.14 | |
| Other inflammatory arthropathies | |||||||
| Systemic lupus erythematosus | 5 | 1.5 | 0 | 0 | 5 | 0.68 | |
| Psoriatic arthritis | 0 | 0 | 1 | 0.25 | 1 | 0.14 | |
| Other connective tissue disorders | |||||||
| Dermatomyositis | 2 | 0.60 | 0 | 0 | 2 | 0.27 | |
| Ehlers-Danlos | 1 | 0.30 | 0 | 0 | 1 | 0.14 | |
| Unknown | 15 | 4.5 | 28 | 6.9 | 43 | 5.8 | |
| Total | 331 | 405 | 736 | ||||
Cemented fixation was used exclusively in four studies, cementless implants alone were used in four studies, and eight studies reported on both techniques. In Group I, 69% of THAs were cemented, whereas THA became mostly cementless in Group II (69%) (Table 2). A variety of bearing surfaces were used; however, reporting of bearing type is lacking in many of these series (45.4%). Specific reporting of bearing type was absent for 62.8% of THAs in Group I and 31.1% of THAs in Group II. Alternative bearing surfaces such as metal-on-highly crosslinked polyethylene or hard-on-hard bearings were reported more frequently in later years, accounting for 46.7% of bearing surfaces in Group II (Table 3).
Table 2.
Fixation in THA in patients 30 years of age and younger
| Type of THA | Group I | Percent | Group II | Percent | Total | Percent | p value |
|---|---|---|---|---|---|---|---|
| Cemented | 230 | 69.5 | 92 | 22.7 | 322 | 43.5 | 4.35 × 10−37 |
| Cementless | 99 | 29.9 | 279 | 68.9 | 378 | 51.3 | 6.61 × 10−26 |
| Hybrid | 2 | 0.60 | 20 | 4.9 | 22 | 3.0 | |
| Reverse hybrid | 0 | 0 | 14 | 3.5 | 14 | 1.9 | |
| Total | 331 | 405 | 736 |
Table 3.
Bearing surfaces in THA in patients 30 years of age and younger
| Bearing surface | Group I | Percent | Group II | Percent | Total | Percent |
|---|---|---|---|---|---|---|
| Metal on all-polyethylene acetabular component | 83 | 25.1 | 0 | 0 | 83 | 11.2 |
| Metal on CPE | 15 | 4.5 | 90 | 22.2 | 105 | 14.3 |
| Metal on HXLPE | 0 | 0 | 52 | 12.8 | 52 | 7.1 |
| Ceramic on Ceramic | 25 | 7.6 | 54 | 13.3 | 79 | 10.7 |
| Ceramic on HXLPE | 0 | 0 | 29 | 7.2 | 29 | 3.9 |
| Metal on metal | 0 | 0 | 54 | 13.3 | 54 | 7.3 |
| Not reported | 208 | 62.8 | 126 | 31.1 | 334 | 45.4 |
| Total | 331 | 405 | 736 |
CPE = conventional polyethylene; HXLPE = highly crosslinked polyethylene.
Reported clinical outcomes at final followup in each study included either the Harris hip score or Merle d’Aubigne score in all but one study, which only used the scoring system of the Hospital for Special Surgery [33]. The Harris hip score was reported in 12 studies with a mean postoperative score of 84.5 (range, 17–100) at an average followup of 7.5 years. The Merle d’Aubigne score was used in three studies with an average of 16.5 (range, 8–18) at mean followup of 15 years. Clinical outcomes were similar between Group I and Group II (average Harris hip score was 84.4 at mean followup of 7.7 years and 84.6 at mean followup of 7.4 years, respectively; p = 0.5). Comparison of Merle d’Aubigne scores in the two groups was not feasible as a result of the paucity of studies using this scoring system. Radiographic evaluation revealed acetabular component loosening in 10.7% of all cases. Femoral component loosening was present in 3.4%. Rates of both acetabular and femoral component loosening were significantly lower in Group II than in Group I (1.5% versus 22%, p = 2.9 × 10−19 and 0% versus 7.6%, respectively, p = 1.8 × 10−8).
Revision of any type (head/liner exchange, revision of the acetabular component, femoral component, or both) occurred in 15.6% of patients. Overall revision rates were lower in Group II than Group I (12.3% versus 19.6%, p = 0.007). The most common reason for revision was aseptic loosening (60.9% of all revisions) followed by polyethylene wear (12.2%) and infection (10.4%). In Group I, aseptic loosening was the predominant mode of failure (70.7%). Loosening remained the major reason for revision in Group II (48%), but it represented a smaller proportion. Wear emerged as the second most common cause (24%) (Table 4).
Table 4.
Revision after THA in patients 30 years of age and younger
| Reason for revision | Group I | Percent | Group II | Percent | Total | Percent | p value |
|---|---|---|---|---|---|---|---|
| Loosening | 46 | 70.7 | 24 | 48.0 | 70 | 60.9 | |
| Infection | 8 | 12.3 | 4 | 8.0 | 12 | 10.4 | |
| Instability | 0 | 0 | 6 | 12.0 | 6 | 5.2 | |
| Lysis | 1 | 1.5 | 1 | 2.0 | 2 | 1.7 | |
| Wear | 2 | 3.1 | 12 | 24.0 | 14 | 12.2 | |
| Periprosthetic fracture | 2 | 3.1 | 0 | 0 | 2 | 1.7 | |
| Acetabular component fracture | 2 | 3.1 | 0 | 0 | 2 | 1.7 | |
| Femoral component fracture | 4 | 6.2 | 0 | 0 | 4 | 3.5 | |
| Liner fracture | 0 | 0 | 1 | 2.0 | 1 | 0.86 | |
| Acetabular component protrusio | 0 | 0 | 1 | 2.0 | 1 | 0.86 | |
| Impingement | 0 | 0 | 1 | 2.0 | 1 | 0.86 | |
| Total | 65 | 50 | 115 | ||||
| Overall revision rate | 19.6 | 12.3 | 15.6 | 0.007 |
Discussion
This systematic review compares changes in surgical indications, implant selection, clinical and radiographic outcomes, and survivorship of THAs in patients 30 years and younger over time. After 1988 (the midpoint in our analysis), there has been a relative decrease in THA for rheumatoid arthritis compared with other indications. In addition, there has been an increase in use of cementless fixation along with decreases in aseptic loosening and revision rates. Despite improved survivorship, clinical outcomes, including the Harris hip score and the Merle d’Aubigne score, have not improved when we compared THAs done since 1988 THAs with those done earlier.
This study is limited both by our own exclusion criteria and by the design and quality of included studies. Our review was restricted to articles written in, or translated into, the English language. This may exclude some studies that might substantially contribute to our understanding of the clinical performance of THA in this patient population. However, this was necessary for the completion of the study, because none of the authors were able to critically review any articles that were not in English. The exclusion of studies that did not report validated patient outcome measures and/or radiographic results may also eliminate studies that might still provide important information on survivorship. Nevertheless, we wanted to include only studies that provide common end points that could be summarized relative to other reports on this clinical issue. In addition, lack of consistency in outcomes of interest reported by some included studies also limits our results. There was a great deal of variability in the reporting of patient outcome measures and bearing surfaces, particularly before 1988, which make results difficult to synthesize. However, at the time of those reports, alternative bearings were uncommon, so it is reasonable to assume that most of those unreported bearings were metal on conventional polyethylene. Overall, the quality of the articles included in this review may be a limitation. All articles were retrospective case series, so the level of evidence is not as strong as some other study designs. Nevertheless, our aim was to summarize and compare existing historical and contemporary reports, and the literature on this topic is only presented in a retrospective manner. The existing literature may also limit the generalizability of the findings. For example, relatively rare indications for arthroplasty are included in this review, which may not be the experience of the average arthroplasty surgeon. However, as stated previously, our aims were to summarize what the literature states about arthroplasty in young patients; these findings are part of what the literature states. This study does identify some interesting trends. Aseptic loosening, traditionally a major limitation in survivorship of THA, was substantially lower in Group II than Group I. The changing patient population demonstrated in this study may explain this, at least in part. Historically, the success of THA has been limited in patients with rheumatoid arthritis as a result of excessive loosening [5, 28, 33]. The decrease in patients with rheumatoid arthritis over time, which has been associated with the introduction of modern disease-modifying antirheumatic drugs, has been demonstrated in other studies [9, 17]. Hekmat et al. reported a nearly 50% decrease in incidence of THA in patients with rheumatoid arthritis once tumor necrosis factor-alpha inhibitors were introduced and became the established treatment for this disease [17]. It is possible that the decreasing incidence of THA for patients with rheumatoid arthritis has decreased a population particularly at risk for aseptic loosening, leading to a decrease in loosening rates over time. The decrease in loosening may also be attributed to improvement in implant fixation techniques, because Group II is predominated by cementless implants. Cementless fixation has been associated with decreased rates of failure as a result of aseptic loosening in multiple studies [7, 8, 11, 31, 34], including a randomized controlled trial [7, 8]; however, this has not necessarily been corroborated with registry data [15]. It is unclear whether the introduction of alternative bearing surfaces has contributed to this reduction in aseptic loosening, because most studies failed to report the type of bearing surface used. The reduction in revision over time is most likely reflective of this decrease in aseptic loosening. This improvement in survival is more evident in femoral component survivorship with a 0% stem revision rate in Group II. This is consistent with improvements in femoral component survivorship associated with cementless fixation that has been demonstrated across the literature [11, 15, 24, 31].
It is interesting that despite the major improvements in radiographic loosening and revision, clinical outcomes have not improved over time. Perhaps systemic diseases, which contribute to the majority of the primary hip diagnoses in this review, play a role in limiting maximal improvement in clinical outcomes. Most patients in this series have either inflammatory arthropathy or avascular necrosis (combined 59.6%), likely related to the pathophysiology or treatment of other illnesses such as sickle cell anemia, cancer, and HIV/AIDS. Improvement in pain and function after THA in these patients may thus be limited by their overall health status. It was not possible to assess this theory in this review, because these studies did not routinely stratify results based on the primary hip diagnosis.
In summary, radiographic loosening and revision rates have decreased substantially over time in very young patients undergoing THA with the advent of contemporary surgical techniques and implants. However, clinical outcome scores have remained constant despite these apparent improvements in durability.
Footnotes
One of the authors certifies that he (JJC) has or may receive payments or benefits, during the study period, of less than USD 10,000 from Biomet (Warsaw, IN, USA), less than USD 10,000 from Pivot Medical (Sunnyvale, CA, USA), and USD 10,000–USD 100,000 from Zimmer (Warsaw, IN, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
References
- 1.Bessette BJ, Fassier F, Tanzer M. Total hip arthroplasty in patients younger than 21 years: a minimum 10-year follow-up. Can J Surg. 2003;46:257–262. [PMC free article] [PubMed] [Google Scholar]
- 2.Bilsel N, Gokce A, Kesmezacar H, Mumcuoglu E, Ozdogan H. Long-term results of total hip arthroplasty in patients with juvenile rheumatoid arthritis. Acta Orthop Traumatol Turc. 2008;42:119–124. doi: 10.3944/aott.2008.42.2.119. [DOI] [PubMed] [Google Scholar]
- 3.Busch V, Klarenbeek R, Sloof T, Schreurs W, Gardeniers J. Cemented hip designs are a reasonable option in young patients. Clin Orthop Relat Res. 2010;468:3214–3320. doi: 10.1007/s11999-010-1355-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chandler HP, Reineck FT, Wixson RL, McCarthy JC. Total hip replacement in patients younger than thirty years old: a five-year follow-up study. J Bone Joint Surg Am. 1981;63:1426–1434. [PubMed] [Google Scholar]
- 5.Chmell MJ, Scott RD, Thomas WH, Sledge CB. Total hip arthroplasty with cement for juvenile rheumatoid arthritis. Results at a minimum of ten years in patients less than thirty years old. J Bone Joint Surg Am. 1997;79:44–52. doi: 10.2106/00004623-199701000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Clohisy JC, Oryhon JM, Seyler TM, Wells CW, Liu SS, Callaghan JJ, Mont MA. Function and fixation of total hip arthroplasty in patients 25 years of age or younger. Clin Orthop Relat Res. 2010;468:3207–3213. doi: 10.1007/s11999-010-1468-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Corten K, Bourne RB, Charron KD, Au K, Rorabeck CH. What works best, a cemented or cementless primary total hip arthroplasty? A minimum 17 year follow-up of a randomized control trial. Clin Orthop Relat Res. 2011;469:209–217. doi: 10.1007/s11999-010-1459-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Corten K, Bourne RB, Charron KD, Au K, Rorabeck CH. Comparison of total hip arthroplasty performed with and without cement: a randomized trial. A concise follow-up, at twenty years, of previous reports. J Bone Joint Surg Am. 2011;93:1335–1338. doi: 10.2106/JBJS.J.00448. [DOI] [PubMed] [Google Scholar]
- 9.Da Silva E, Doran MF, Crowson CS, O’Fallon WM, Matteson EL. Declining use of orthopedic surgery in patients with rheumatoid arthritis? Results of a long-term, population-based assessment. Arthritis Rheum. 2003;49:216–220. doi: 10.1002/art.10998. [DOI] [PubMed] [Google Scholar]
- 10.Dudkiewicz I, Salai M, Israeli A, Amit Y, Chechick A. Total hip arthroplasty in patients younger than 30 years of age. IMAJ. 2003;5:709–712. [PubMed] [Google Scholar]
- 11.Emerson RH, Head WC, Emerson CB, Rosenfeldt W, Higgins LL. A comparison of cemented and cementless titanium femoral components used for primary total hip arthroplasty: a radiographic and survivorship study. J Arthroplasty. 2002;17:584–591. doi: 10.1054/arth.2002.32696. [DOI] [PubMed] [Google Scholar]
- 12.Finkbone PR, Severson EP, Cabanela ME, Trousdale RT. Ceramic-on-ceramic total hip arthroplasty in patients younger than 20 years. J Arthroplasty. 2012;27:213–219. doi: 10.1016/j.arth.2011.05.022. [DOI] [PubMed] [Google Scholar]
- 13.Girard J, Bocquet D, Autissier G, Fouilleron N, Fron D, Migaud H. Metal-on-metal hip arthroplasty in patients thirty years of age or younger. J Bone Joint Surg Am. 2010;92:2419–2426. doi: 10.2106/JBJS.I.01644. [DOI] [PubMed] [Google Scholar]
- 14.Haber D, Goodman SB. Total hip arthroplasty in juvenile chronic arthritis: a consecutive series. J Arthroplasty. 1998;12:259–265. doi: 10.1016/S0883-5403(98)90170-X. [DOI] [PubMed] [Google Scholar]
- 15.Hailer NP, Garellick G, Karrholm J. Uncemented and cemented primary total hip arthroplasty in the Swedish Hip Arthroplasty Register. Acta Orthop. 2010;81:34–41. doi: 10.3109/17453671003685400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harris WH, Sledge CB. Total hip and total knee replacement (1) N Engl J Med. 1990;323:725–731. doi: 10.1056/NEJM199009133231106. [DOI] [PubMed] [Google Scholar]
- 17.Hekmat K, Jacobsson L, Nilsson JA, Petersson IF, Robertsson O, Garellick G, Turesson C. Decrease in the incidence of total hip arthroplasties in patients with rheumatoid arthritis—results from a well-defined population in south Sweden. Arthritis Res Ther. 2011;1:R67. doi: 10.1186/ar3328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hyder N, Nevelos AB, Barabas TG. Cementless ceramic hip arthroplasties in patients less than 30 years old. J Arthroplasty. 1996;11:679–686. doi: 10.1016/S0883-5403(96)80006-4. [DOI] [PubMed] [Google Scholar]
- 19.Kamath AF, Sheth NP, Hosalkar HH, Babatunde OM, Lee GC, Nelson CL. Modern total hip arthroplasty in patients younger than 21 years. J Arthroplasty. 2012;27:402–408. doi: 10.1016/j.arth.2011.04.042. [DOI] [PubMed] [Google Scholar]
- 20.Kitsoulis PB, Stafilas KS, Siamopoulou A, Soucacaos PN, Xenakis TA. Total hip arthroplasty in children with juvenile chronic arthritis: long-term results. J Pediatr Orthop. 2006;26:8–12. doi: 10.1097/01.bpo.0000187997.84213.d9. [DOI] [PubMed] [Google Scholar]
- 21.Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467:2606–2612. doi: 10.1007/s11999-009-0834-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lachiewicz PF, McCaskill B, Inglis A, Ranawat CS, Rosenstein BD. Total hip arthroplasty in juvenile rheumatoid arthritis. Two to eleven-year results. J Bone Joint Surg Am. 1986;68:502–508. [PubMed] [Google Scholar]
- 23.Learmonth ID, Heywood AW, Kaye J, Dall D. Radiological loosening after cemented hip replacement for juvenile chronic arthritis. J Bone Joint Surg Br. 1989;71:209–212. doi: 10.1302/0301-620X.71B2.2925736. [DOI] [PubMed] [Google Scholar]
- 24.Makela KT, Eskelinen A, Pulkkinen P, Virolainen P, Paavolainen P, Remes V. Cemented versus cementless total hip arthroplasty in patients fifty-five years or older with rheumatoid arthritis. J Bone Joint Surg Am. 2011;93:178–186. doi: 10.2106/JBJS.I.01283. [DOI] [PubMed] [Google Scholar]
- 25.Mall NA, Nunley RM, Zhu JJ, Maloney WJ, Barrack RL, Clohisy JC. The incidence of acetabular osteolysis in young patients with conventional versus highly crosslinked polyethylene. Clin Orthop Relat Res. 2011;469:372–381. doi: 10.1007/s11999-010-1518-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maric Z, Haynes RJ. Total hip arthroplasty in juvenile rheumatoid arthritis. Clin Orthop Relat Res. 1993;290:197–199. [PubMed] [Google Scholar]
- 27.Restrepo C, Lettich T, Roberts N, Parvizi J, Hozack WJ. Uncemented total hip arthroplasty in patients less than twenty-years. Acta Orthop Belg. 2008;74:615–622. [PubMed] [Google Scholar]
- 28.Roach JW, Paradies LH. Total hip arthroplasty performed during adolescence. J Pediatr Orthop. 1984;4:418–421. doi: 10.1097/01241398-198408000-00005. [DOI] [PubMed] [Google Scholar]
- 29.Skyttä ET, Jarkko L, Antti E, Huhtala H, Ville R. Increasing incidence of hip arthroplasty for primary osteoarthritis in 30- to 59-year-old patients. Acta Orthop. 2011;82:1–5. doi: 10.3109/17453674.2010.548029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sochart DH, Porter ML. Long-term results of cemented Charnley low-friction artrhoplasty in patients aged less than 30 years. J Arthroplasty. 1998;13:123–131. doi: 10.1016/S0883-5403(98)90089-4. [DOI] [PubMed] [Google Scholar]
- 31.Springer BD, Connelly SE, Odum SM, Fehring TK, Griffin WL, Mason JB, Masonis JL. Cementless femoral components in young patients: review and meta-analysis of total hip arthroplasty and hip resurfacing. J Arthroplasty. 2009;24(Suppl):2–8. doi: 10.1016/j.arth.2009.04.032. [DOI] [PubMed] [Google Scholar]
- 32.Wangen H, Lereim P, Holm I, Gunderson R, Reikeras O. Hip arthroplasty in patients younger than 30 years: excellent ten to 16-year follow-up results with a HA-coated stem. Int Orthop. 2008;32:203–208. doi: 10.1007/s00264-006-0309-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Witt JD, Swann M, Ansell BM. Total hip replacement for juvenile chronic arthritis. J Bone Joint Surg Br. 1991;73:770–773. doi: 10.1302/0301-620X.73B5.1894663. [DOI] [PubMed] [Google Scholar]
- 34.Zwartele RE, Witjes S, Doets HC, Stijnen T, Poll RG. Cementless total hip arthroplasty in rheumatoid arthritis: a systematic review of the literature. Arch Orthop Trauma Surg. 2012;132:535–546. doi: 10.1007/s00402-011-1432-0. [DOI] [PMC free article] [PubMed] [Google Scholar]