Abstract
Background
Patellofemoral joint (PFJ) malalignment (lateral patella displacement and tilt) has been proposed as a cause of patellofemoral pain. Patella height and/or the morphologic features of the femoral trochlea may predispose one to patella malalignment.
Questions/purposes
The purposes of our study were to assess the associations among patella height, morphologic features of the trochlea, and measures of PFJ alignment and to determine which measures of patella height and morphologic features of the trochlea were the best predictors of PFJ alignment.
Methods
Measures of patella height (Insall-Salvati ratio and modified Insall-Salvati ratio), morphologic features of the trochlea (sulcus angle, trochlear angle, lateral trochlear inclination, medial trochlear inclination), and PFJ alignment (bisect offset and patella tilt angle) were assessed in 566 knees from the Multicenter Osteoarthritis Study.
Results
Bisect offset was correlated with the Insall-Salvati ratio (r = 0.25) and lateral trochlear inclination (r = −0.38). Patella tilt angle correlated with the trochlear angle (−0.27) and lateral trochlear inclination (−0.32). Linear regression models including the Insall-Salvati ratio and lateral trochlear inclination explained 20% and 11% of the variance in bisect offset and patella tilt angle, respectively.
Conclusions
Of the variables measured in the current study, the Insall-Salvati ratio and lateral trochlear inclination were the best predictors of lateral patella displacement and lateral tilt. This knowledge will aid clinicians in the identification of anatomic risk factors for PFJ malalignment and/or PFJ dysfunction.
Level of Evidence
Level III, diagnostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Patellofemoral joint (PFJ) malalignment (lateral patella displacement and tilt) has been proposed as a cause of patellofemoral dysfunction [8, 14, 21, 24, 38]. There are dynamic and structural factors that may predispose the PFJ to malalignment. Dynamic factors include an imbalance in quadriceps forces (ie, vastus medialis versus vastus lateralis) [27, 32], whereas structural features include a vertical position of the patella (patella alta) [15, 20, 25] and the morphologic features of the femoral trochlea [5, 10, 28].
Persons with patella alta are believed to have increased patella malalignment owing to the lack of osseous stability when the patella articulates superior to the femoral trochlea, especially when the knee is actively extended [15, 20, 25]. Several methods of measuring the vertical height of the patella have been proposed. The Insall-Salvati ratio, a ratio between the length of the patellar tendon and vertical height of the patella, is the most common reported in the literature and is easily measured from the lateral radiograph [16]. An Insall-Salvati ratio greater than 1.2 has been defined as patella alta. Additionally, the modified Insall-Salvati ratio was proposed by Grelsamer and Meadows [9] to account for different morphologic features of the sagittal plane of the patella. The modified Insall-Salvati ratio uses the length of the articular surface of the patella instead of the height of the entire patella. Grelsamer and Meadows suggested that a ratio greater than 2.0 is indicative of patella alta. Persons with patella alta have been shown to have a greater frequency of patella dislocation [15] and have shown 20% and 39% greater lateral displacement and tilt of the patella, respectively, when compared with persons without patella alta [37].
PFJ malalignment also may occur when the femoral trochlea is flattened or when the lateral trochlear facet does not project as far anterior as the medial facet. Abnormal trochlear geometry may allow the patella to migrate out of the trochlear groove as the quadriceps contracts and the knee extends from a flexed position [5, 10, 28]. The sulcus angle is a common measure of morphologic features of the trochlea and is defined as the angle between the medial and lateral trochlear facets [4, 28]. It has been reported that as the sulcus angle increased (ie, trochlea becomes more flattened), lateral patella displacement and lateral patella tilt also increased, especially during terminal knee extension [28]. However, alternative measures of trochlear shape have been reported, including the lateral trochlear inclination and trochlear angles [5, 19]. Low lateral trochlear inclination has been shown to be associated with patella dislocation [5] and patellofemoral maltracking [10], suggesting a flattened lateral trochlear facet decreases patella stability.
Previous studies with small numbers of subjects have shown that persons with patella alta and flattened trochleae have greater PFJ malalignment and instability [10, 15, 25, 28, 37]. Thus, there appears to be a relationship between morphologic features of the PFJ and PFJ alignment. However, the strength of this relationship in a large diverse sample is unknown. Furthermore, it is not known which measures of patella height or morphologic features of the trochlea are most strongly related to PFJ alignment. This knowledge will aid clinicians in identification of anatomic risk factors for PFJ malalignment and/or PFJ dysfunction. The purposes of this study were to determine (1) which measure of patella height (Insall-Salvati ratio or modified Insall-Salvati ratio) best predicted measurements of PFJ alignment (lateral patellar displacement and tilt), and (2) which measure of morphologic features of the trochlea (sulcus angle, trochlear angle, or trochlear inclination) best predicted PFJ alignment, in a large cohort study.
Patients and Methods
The Multicenter Osteoarthritis (MOST) Study is a prospective cohort study of 3026 individuals (ages, 50–79 years) who either had knee osteoarthritis or were at high risk (older than 50 years, overweight, or had a previous knee injury) for knee osteoarthritis. Participants were recruited from two communities in the United States surrounding Birmingham, AL, and Iowa City, IA. Details of the study population have been published elsewhere [7]. The institutional review boards at the University of Iowa, University of Alabama, Birmingham, University of California, San Francisco, and Boston University School of Medicine approved the study protocol.
The sample for the current study consisted of 907 knees (one knee per subject) that were used in a previous study investigating the relationship between patella height and PFJ structural damage [35]. These knees were randomly selected from participants who underwent MRI and whose MR images were read for structural abnormalities as part of other completed studies from the parent MOST study. Lateral fixed-flexion weightbearing radiographs [22] and MR images were acquired from all subjects. The radiograph protocol was standardized across the two study sites and yielded knee flexion angles of 20° to 50° (median, 39°). We used a 1.0-Tesla extremity MRI system (OrthOne™; ONI Medical Systems Wilmington, MA, USA) with a phased-array knee coil to acquire axial and sagittal MR images (fast spin echo fat-suppressed proton density-weighted and coronal short tau inversion recovery sequences). Knees were extended and the quadriceps muscle was relaxed during imaging.
Of the 907 knees selected for study, 33 were excluded as a result of the inability to identify all bony landmarks necessary to obtain the measurements described below. This occurred because of either poor image quality or severe osteoarthritis. Additionally we excluded knees with full thickness cartilage damage in any region of the PFJ (patella or trochlea). This left 566 knees (566 patients) eligible for the study.
We measured the Insall-Salvati ratio [16] and modified Insall-Salvati ratio [9] from the lateral fixed-flexion weightbearing radiographs (Fig. 1). The Insall-Salvati ratio [16] was calculated by dividing the distance from the tibial tuberosity to the inferior pole of the patella by the length of the patella measured by the distance from the apex of the patella to its most posterior superior point. We calculated the modified Insall-Salvati ratio [9] by dividing the distance from the tibial tuberosity to the inferior margin of the articular surface of the patella by the length of the articular surface of the patella. All measurements were made using OsiriX DICOM viewer software (Version 3.2.2; OsiriX Foundation, Geneva, Switzerland).
Fig. 1.
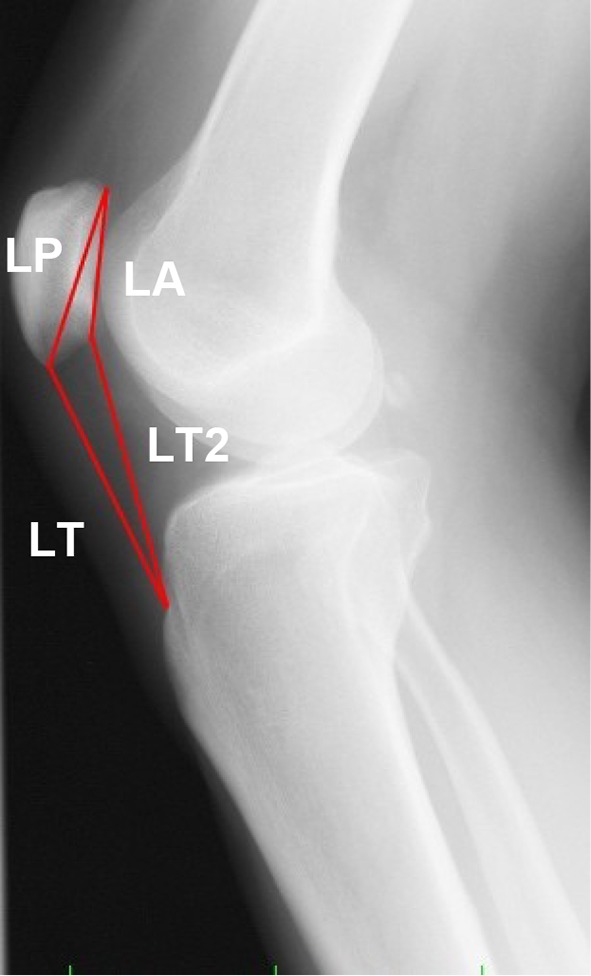
The Insall-Salvati ratio was calculated by dividing the length of the patella tendon (LT) by the length of the patella (LP) measured from the lateral radiograph. The modified Insall-Salvati ratio was calculated by dividing the distance from the tibial tuberosity to the inferior pole of the articular surface of the patella (LT2) by the length of the articular surface of the patella (LA). (Published with permission and adapted from from Stefanik JJ, Zhu Y, Zumwalt AC, Gross KD, Clancy M, Lynch JA, Frey Law LA, Lewis CE, Roemer FW, Powers CM, Guermazi A, Felson DT. Association between patella alta and the prevalence and worsening of structural features of patellofemoral joint osteoarthritis: the multicenter osteoarthritis study. Arthritis Care Res. 2010; 62: 1258–1265. Copyright (2010) Wiley.)
We measured four different aspects of morphologic features of the trochlea: lateral trochlear inclination, medial trochlear inclination, trochlear angle, and sulcus angle (Fig. 2). These measurements were made on the axial MR images on the slice in which the posterior femoral condyles were the largest (ie, the slice above and below showed a smaller amount of the posterior femoral condyle). First, the posterior condylar line was drawn along the most posterior surface of the femoral condyles. Lateral trochlear inclination was defined as the angle between the posterior condylar line and a line drawn along the surface of the lateral trochlear facet [5]. Medial trochlear inclination was defined as the angle between the posterior condylar line and a line drawn along the surface of the medial trochlear facet. Trochlear angle was defined as the angle between the posterior condylar line and a line passing along the most anterior margins of the medial and lateral trochlear facets [19]. Sulcus angle was defined as the angle between the medial and lateral trochlear facets [4]. The vertex of the angle was the deepest portion of the trochlea.
Fig. 2A–C.
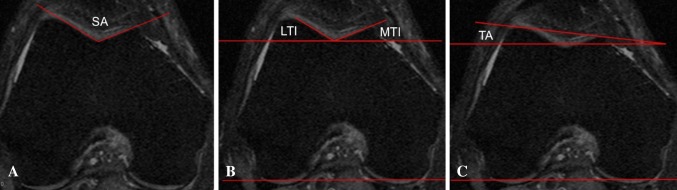
(A) The sulcus angle (SA) is the angle between the medial and lateral trochlear facets. (B) Lateral and medial trochlear inclination is the angle between the posterior condylar line and a line along the lateral and medial facets, respectively. (C) The trochlear angle is the angle between the posterior condylar line and a line passing along the most anterior margin of the medial and lateral trochlear facets. (Published with permission and adapted from Stefanik JJ, Roemer FW, Zumwalt AC, Zhu Y, Gross KD, Lynch JA, Frey-Law LA, Lewis CE, Guermazi A, Powers CM, Felson DT. Association between measures of trochlear morphology and structural features of patellofemoral joint osteoarthritis on MRI: the MOST study. J Orthop Res. 2012;30:1–8. Copyright 2012 Wiley.)
Lateral displacement (bisect offset) and patella tilt angle where measured on the same slice that morphologic features of the trochlea were measured (Fig. 3) [29, 36]. On this slice, a perpendicular line was drawn through the center of the trochlea intersecting with the posterior condylar line. Then, on the slice where the patella width was maximal, a line was drawn connecting medial and lateral margins of the patella. If the posterior condylar line was drawn on a different slice than the slice with maximal patellar width, the posterior condylar line was copied to the slice where patella width was maximal. Bisect offset was defined as the percentage of the patella lateral to the line through the center of the trochlea. Patella tilt angle was defined as the angle between the posterior condylar line and the line defining the maximal width of the patella.
Fig. 3A–C.
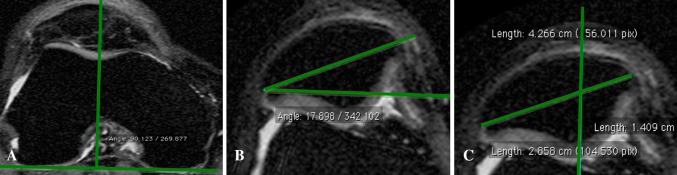
(A) On the slice where the posterior femoral condyles were largest, a line was drawn on their posterior surface (posterior condylar line). Then a line perpendicular to this line was projected anteriorly through the center of the femoral trochlea. (B) The patella tilt angle is the angle between the posterior condylar line and the maximal patella width line. (C) Bisect offset is equal to the length of the patella lateral to midline/maximal patella width × 100. (Published with permission and adapted from from Stefanik JJ, Zhu Y, Zumwalt AC, Gross KD, Clancy M, Lynch JA, Frey Law LA, Lewis CE, Roemer FW, Powers CM, Guermazi A, Felson DT. Association between patella alta and the prevalence and worsening of structural features of patellofemoral joint osteoarthritis: the multicenter osteoarthritis study. Arthritis Care Res. 2010; 62: 1258–1265. Copyright (2010) Wiley.)
Two readers (JJS and ACZ) took the measurements for patella height, morphologic features of the trochlea, and PFJ alignment measurements. To determine intrarater and interrater reliability, both readers repeated measurements in a random selection of 10% of all knees. Random selection of knees was performed blindly to the authors using a statistical program. The knees selected for reliability analysis were blindly distributed throughout a list of knees to be examined for patella height, morphologic features of the trochlea, and PFJ alignment after examining these features in at least 20 other knees. Interrater and intrarater intraclass correlation coefficients were good to excellent (Table 1).
Table 1.
Reliability assessment for measures of patella alta, morphologic features of the trochlea, and PFJ alignment
| Variable | Interrater (ICC) | Intrarater (ICC) |
|---|---|---|
| Patella tendon length | 0.97 | 0.99 |
| Patella length | 0.98 | 0.99 |
| Insall-Salvati ratio | 0.97 | 0.99 |
| Length of articular surface of patella | 0.80 | 0.92 |
| Patella tendon length for modified Insall-Salvati ratio | 0.94 | 0.99 |
| Modified Insall-Salvati ratio | 0.71 | 0.93 |
| Lateral trochlear inclination | 0.80 | 0.90 |
| Trochlear angle | 0.80 | 0.92 |
| Sulcus angle | 0.86 | 0.94 |
| Bisect offset | 0.93 | 0.96 |
| Patella tilt angle | 0.89 | 0.93 |
PFJ = patellofemoral joint; ICC = intraclass correlation coefficient.
We first explored the relationship between measures of PFJ alignment (bisect offset and patella tilt angle) with the Insall-Salvati ratio, modified Insall-Salvati ratio, and measures of morphologic features of the trochlea using a Pearson’s correlation coefficient. Next, linear regression with manual forward selection was used to determine which variables contributed the most to the variance of bisect offset and patella tilt angle (dependent variables) with the Insall-Salvati ratio, modified Insall-Salvati ratio, and measures of morphologic features of the trochlea as independent variables. We added measures of patella height (Insall-Salvati ratio or modified Insall-Salvati ratio) separately to determine which explained the most variance of bisect offset and patella tilt angle. Next, measures of morphologic features of the trochlea were added individually to determine which explained the most variance of bisect offset and patella tilt angle. We used standardized beta coefficients (relative predictive values of the individual independent variables) and partial r2 values for each variable to select the variables that were the best predictors of bisect offset and patella tilt angle. Statistical analyses were performed using SAS software (Version 9.1; SAS Institute Inc, Cary, NC, USA).
The mean age of the 566 patients was 62 years and 59% of the 566 knees studied were from female subjects (Table 2). The mean Insall-Salvati ratio, modified Insall-Salvati ratio, trochlear angle, sulcus angle, lateral trochlear inclination, medial trochlear inclination, bisect offset, and patella tilt angle were 1.09, 1.7, 3.1, 130.4, 25.5, 24.4, 58.7, and 10.0, respectively (Table 2).
Table 2.
Descriptive statistics (n = 566 patients and knees)*
| Variable | Value |
|---|---|
| Female (%) | 59 |
| Age (years) | 61.5 (7.9) |
| Insall-Salvati ratio | 1.09 (0.16) |
| Modified Insall-Salvati ratio | 1.7 (0.2) |
| Trochlear angle mean (degrees) | 3.1 (3.1) |
| Sulcus angle mean (degrees) | 130.4 (8.7) |
| Lateral trochlear inclination (degrees) | 25.5 (4.9) |
| Medial trochlear inclination (degrees) | 24.4 (6.0) |
| Bisect offset (%) | 58.7 (9.4) |
| Patella tilt angle (degrees) | 10.0 (6.3) |
* Values are mean (SD) unless otherwise indicated.
Results
The Insall-Salvati ratio correlated better with PFJ alignment than did the modified Insall-Salvati ratio (Table 3). The Insall-Salvati ratio was correlated with bisect offset (r = 0.25; p < 0.0001). Weak correlations were observed between the Insall-Salvati ratio and patella tilt angle and between the modified Insall-Salvati ratio and both measures of patellofemoral alignment. In the linear regression model with bisect offset as the dependent variable, the Insall-Salvati ratio was kept in the final model rather than the modified Insall-Salvati ratio because the standardized beta and individual r2 were greater than for the modified Insall-Salvati ratio (0.25 versus 0.15 and 0.06 versus 0.02, respectively) (Table 4). Similarly, in the linear regression model with patella tilt angle as the dependent variable, the Insall-Salvati ratio was chosen over the modified Insall-Salvati ratio to remain in the model because the standardized beta and individual r2 were greater than for the modified Insall-Salvati ratio, 0.08 versus 0.06 and 0.007 versus 0.003, respectively (Table 4).
Table 3.
Correlation coefficients (r) between bisect offset, patella tilt angle, and measures of patella alta and morphologic features of the trochlea
| Variable | ISR | MISR | SA | TA | LTI | MTI |
|---|---|---|---|---|---|---|
| Bisect offset | 0.25* | 0.15** | 0.19* | −0.03 | −0.38* | 0.04 |
| Patella tilt angle | 0.08** | 0.06 | 0.15** | −0.27* | −0.32* | 0.05 |
* p < 0.0001, ** p ≤ 0.05; ISR = Insall-Salvati ratio; MISR = modified Insall-Salvati ratio; SA = sulcus angle; TA = trochlear angle; LTI = lateral trochlear inclination; MTI = medial trochlear inclination.
Table 4.
Linear regression results for predictors of PFJ alignment
| Dependent variable (outcome) | Independent variable (predictor) | Standardized beta | Partial r2 | p value | Model adjusted r2 | Model p value |
|---|---|---|---|---|---|---|
| Bisect offset | ||||||
| Insall-Salvati ratio | 0.24 | 0.07 | < 0.0001 | |||
| Lateral trochlear inclination | −0.37 | 0.15 | < 0.0001 | 0.20 | < 0.0001 | |
| Patellar tilt angle | ||||||
| Insall-Salvati ratio | 0.07 | 0.006 | 0.07 | |||
| Lateral trochlear inclination | −0.32 | 0.10 | < 0.0001 | 0.11 | < 0.0001 | |
PFJ = patellofemoral joint.
Among the variables evaluated for morphologic features of the trochlea, the lateral trochlear inclination angle was the best predictor of PFJ alignment (Table 3). Lateral trochlear inclination was moderately (inversely) correlated with bisect offset (r = −0.38; p < 0.0001) and patella tilt angle (r = −0.32; p < 0.0001). Trochlear angle was moderately (inversely) correlated with patella tilt angle (r = −0.27; p < 0.0001). Sulcus angle and medial trochlear inclination were weakly correlated with both measures of patellofemoral alignment. In the linear regression model with bisect offset as the dependent variable, each measure of morphologic features of the trochlea then was added individually to the model including the Insall-Salvati ratio. Lateral trochlear inclination yielded the greatest standardized beta and partial r2 (beta = −0.37, partial r2 = 0.15) compared with sulcus angle (0.17, 0.03) and trochlear angle (−0.07, 0.05). The final model with Insall-Salvati ratio and lateral trochlear inclination had an overall model adjusted r2 of 0.20 (p < 0.0001) (Table 4). In the linear regression model with patella tilt angle as the dependent variable, each measure of morphologic features of the trochlea was individually compared in the model including the Insall-Salvati ratio. The model with the Insall-Salvati ratio and lateral trochlear inclination yielded the greatest standardized beta coefficient and partial r2 (−0.32, 0.10) compared with trochlear angle (−0.29, 0.08), sulcus angle (0.11, 0.01), and medial trochlear inclination (0.09, 0.008). The final model with patella tilt angle as the dependent variable including the Insall-Salvati ratio and lateral trochlear inclination had an overall model adjusted r2 of 0.11 (p < 0.0001) (Table 4).
Discussion
In this study, we evaluated multiple measures of patella height and morphologic features of the trochlea to determine which predicted PFJ alignment best. The Insall-Salvati ratio was a better predictor of bisect offset and patella tilt angle than was the modified Insall-Salvati ratio. In addition, lateral trochlear inclination was the best predictor of PFJ alignment among the variables for morphologic features of the trochlea. Conversely, we found the sulcus angle, a commonly reported measure of morphologic features of the trochlea [4, 28], only showed weak relationships with bisect offset and patella tilt angle.
There are certain limitations to our study. First, the slice at which morphologic features of the trochlea was measured could have affected our results. We selected the slice in which the medial and lateral trochlear facets were observed. Measurement of lateral trochlear inclination on a more proximal slice, as done by Carrillon et al. [5], may have produced different results. Second, we recognize that we likely underestimated the amount of lateral displacement and tilt when measuring these variables from images obtained with the quadriceps relaxed. However, this type of imaging is typical of most routine clinical MRI scans, and thus, it could be argued that our results would be generalizable to clinicians who can measure these parameters from their patients’ images. Finally, there are other measures of patella height that were not incorporated into our study such as the Caton-Deschamps [6], Blackburne-Peel [3], and patellotrochlear [2] indices. We chose to use the Insall-Salvati ratio as it is commonly used and easily measured from the lateral radiograph.
Ward et al. [37] reported a significant positive correlation between the Insall-Salvati ratio and lateral displacement (r2 = 0.37) and patella tilt (r2 = 0.28) with the knee extended and quadriceps contracted. We found a more moderate correlation between the Insall-Salvati ratio and bisect offset (r = 0.25), weak correlations between the Insall-Salvati ratio and patella tilt angle (r = 0.08), and weak correlations between the modified Insall-Salvati ratio and bisect offset and patella tilt angle (r = 0.15 and 0.06, respectively). As noted above, lateral displacement and tilt were measured on MR images obtained with the knee extended and quadriceps relaxed, typical of a routine MR image obtained in clinical practice. When the quadriceps contract, lateral displacement and tilt become greater as a result of the increase in the laterally directed force acting on the patella caused by the quadriceps angle [12, 31]. It is likely the differences in the strength of the observed relationships between our study and that of Ward et al. [37] may be related to the state of quadriceps contraction at the time of imaging. Our correlations likely would have been stronger if we had obtained measures of patella displacement and tilt with the quadriceps contracted.
The morphologic features of the femoral trochlea have been studied in various investigations aimed at identifying risk factors for PFJ cartilage damage [1, 17, 34], bone marrow lesions [17, 34], radiographic features of patellofemoral osteoarthritis [13, 18], pain and function [19, 20], and patella kinematics [10, 28]. In the majority of these investigations, the sulcus angle was the primary measure used to assess morphologic features of the trochlea. Lateral trochlear inclination [1, 5, 10, 19] and the trochlear angle [19] have been used as alternative measures of morphologic features of the trochlea. Carrillon et al. were the first to describe the use of the lateral trochlear inclination on MRI [5]. They reported mean values of 6.2° in subjects with a history of patella dislocation and 16.9° in control subjects (p < 0.001). Their results are consistent with our findings in that a lower lateral trochlear inclination angle (ie, flattened lateral trochlea) was associated with increased bisect offset and patella tilt angle. Conversely, Harbaugh et al. reported no difference in lateral trochlear inclination between a control group and a group with patellofemoral pain with lateral PFJ maltracking [10]. These differences may be the result of the inclusion criteria in each study. Subjects in the former study had a history of patellar dislocation, whereas those in the later study mostly had patellofemoral pain.
We found the Insall-Salvati ratio and lateral trochlear inclination explained 20% and 11% of the variance in bisect offset and patella tilt angle, respectively. This suggests there are variables contributing to the variance in patella alignment other than those measured in the current investigation. Internal rotation of the femur has been shown to be associated with PFJ alignment [30, 33]. Additionally, soft tissue structures such as the patellofemoral ligaments and retinaculum [11, 23, 26] may have had an influence on PFJ alignment. To our knowledge, there is no study that has taken all of these factors into account.
In our study, the Insall-Salvati ratio, lateral trochlear inclination, and trochlear angle were the best predictors of PFJ alignment. A combination of a high patella and flattened lateral femoral trochlea appears to be particularly important with respect to PFJ alignment. Morphologic features of the trochlea may be more important than the Insall-Salvati ratio, explaining 14% of the variance in lateral displacement compared with 11%. Measures of morphologic features of the trochlea also had greater standardized beta coefficients compared with the Insall-Salvati ratio suggesting morphologic features of the trochlea may have a stronger influence on PFJ alignment. We also reported that the Insall-Salvati ratio [35] and lateral trochlear inclination [34] showed the strongest associations with lateral PFJ structural damage compared with other measures of patella height and morphologic features of the trochlea. The results of the previous studies and the current investigation suggest these measurements may be the most important measures of patella height and morphologic features of the trochlea as they relate to disease and PFJ dysfunction.
Using multiple measures of patella height and morphologic features of the trochlea, we found the Insall-Salvati ratio and lateral trochlear inclination were the best predictors of lateral patella displacement and lateral tilt. This knowledge will aid clinicians in the identification of anatomic risk factors for PFJ malalignment and/or PFJ dysfunction. Future studies should be conducted to identify thresholds of measures of patellar height and morphologic features of the trochlea that may put an individual at risk for PFJ dysfunction. Additionally, studies that include structural, passive, and dynamic structures are needed to develop treatments that can reduce patellofemoral malalignment and PFJ dysfunction.
Acknowledgments
We thank the MOST study participants.
Footnotes
The Multicenter Osteoarthritis Study was supported by the National Institutes of Health (NIH) (grants U01-AG18820, U01-AG18832, U01-AG18947, U01-AG19069, and AR-47785). One of the author’s (JJS) work was supported by a doctoral dissertation award from the Arthritis Foundation and NIH grant T32AR007598. He is currently supported by a Postdoctoral Fellowship from the Arthritis Foundation and the Research Scientist Development Award from the American College of Rheumatology.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained. One author (CMP) confirms that no institutional review board approval was required from his institution.
Each author certifies that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained from the institutions that supplied data.
References
- 1.Ali SA, Helmer R, Terk MR. Analysis of the patellofemoral region on MRI: association of abnormal trochlear morphology with severe cartilage defects. AJR Am J Roentgenol. 2010;194:721–727. doi: 10.2214/AJR.09.3008. [DOI] [PubMed] [Google Scholar]
- 2.Biedert RM, Albrecht S. The patellotrochlear index: a new index for assessing patellar height. Knee Surg Sports Traumatol Arthrosc. 2006;14:707–712. doi: 10.1007/s00167-005-0015-4. [DOI] [PubMed] [Google Scholar]
- 3.Blackburne JS, Peel TE. A new method of measuring patellar height. J Bone Joint Surg Br. 1977;59:241–242. doi: 10.1302/0301-620X.59B2.873986. [DOI] [PubMed] [Google Scholar]
- 4.Brattstroem H. Shape of the intercondylar groove normally and in recurrent dislocation of the patella: a clinical and x-ray–anatomical investigation. Acta Orthop Scand Suppl. 1964;68:1–148. [PubMed] [Google Scholar]
- 5.Carrillon Y, Abidi H, Dejour D, Fantino O, Moyen B, Tran-Minh VA. Patellar instability: assessment on MR images by measuring the lateral trochlear inclination-initial experience. Radiology. 2000;216:582–585. doi: 10.1148/radiology.216.2.r00au07582. [DOI] [PubMed] [Google Scholar]
- 6.Caton J. [Method of measuring the height of the patella][in French] Acta Orthop Belg. 1989;55:385–386. [PubMed] [Google Scholar]
- 7.Felson DT, Niu J, Guermazi A, Roemer F, Aliabadi P, Clancy M, Torner J, Lewis CE, Nevitt MC. Correlation of the development of knee pain with enlarging bone marrow lesions on magnetic resonance imaging. Arthritis Rheum. 2007;56:2986–2992. doi: 10.1002/art.22851. [DOI] [PubMed] [Google Scholar]
- 8.Fulkerson JP, Shea KP. Disorders of patellofemoral alignment. J Bone Joint Surg Am. 1990;72:1424–1429. [PubMed] [Google Scholar]
- 9.Grelsamer RP, Meadows S. The modified Insall-Salvati ratio for assessment of patellar height. Clin Orthop Relat Res. 1992;282:170–176. [PubMed] [Google Scholar]
- 10.Harbaugh CM, Wilson NA, Sheehan FT. Correlating femoral shape with patellar kinematics in patients with patellofemoral pain. J Orthop Res. 2010;28:865–872. doi: 10.1002/jor.21101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hautamaa PV, Fithian DC, Kaufman KR, Daniel DM, Pohlmeyer AM. Medial soft tissue restraints in lateral patellar instability and repair. Clin Orthop Relat Res. 1998;349:174–182. doi: 10.1097/00003086-199804000-00021. [DOI] [PubMed] [Google Scholar]
- 12.Huberti HH, Hayes WC. Patellofemoral contact pressures: the influence of q-angle and tendofemoral contact. J Bone Joint Surg Am. 1984;66:715–724. [PubMed] [Google Scholar]
- 13.Hunter DJ, Zhang YQ, Niu JB, Felson DT, Kwoh K, Newman A, Kritchevsky S, Harris T, Carbone L, Nevitt M. Patella malalignment, pain and patellofemoral progression: the Health ABC Study. Osteoarthritis Cartilage. 2007;15:1120–1127. doi: 10.1016/j.joca.2007.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Insall J. Current concepts review: patellar pain. J Bone Joint Surg Am. 1982;64:147–152. [PubMed] [Google Scholar]
- 15.Insall J, Goldberg V, Salvati E. Recurrent dislocation and the high-riding patella. Clin Orthop Relat Res. 1972;88:67–69. doi: 10.1097/00003086-197210000-00012. [DOI] [PubMed] [Google Scholar]
- 16.Insall J, Salvati E. Patella position in the normal knee joint. Radiology. 1971;101:101–104. doi: 10.1148/101.1.101. [DOI] [PubMed] [Google Scholar]
- 17.Kalichman L, Zhang Y, Niu J, Goggins J, Gale D, Felson DT, Hunter D. The association between patellar alignment and patellofemoral joint osteoarthritis features: an MRI study. Rheumatology (Oxford). 2007;46:1303–1308. doi: 10.1093/rheumatology/kem095. [DOI] [PubMed] [Google Scholar]
- 18.Kalichman L, Zhang Y, Niu J, Goggins J, Gale D, Zhu Y, Felson DT, Hunter DJ. The association between patellar alignment on magnetic resonance imaging and radiographic manifestations of knee osteoarthritis. Arthritis Res Ther. 2007;9:R26. doi: 10.1186/ar2138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kalichman L, Zhu Y, Zhang Y, Niu J, Gale D, Felson DT, Hunter D. The association between patella alignment and knee pain and function: an MRI study in persons with symptomatic knee osteoarthritis. Osteoarthritis Cartilage. 2007;15:1235–1240. doi: 10.1016/j.joca.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 20.Kannus PA. Long patellar tendon: radiographic sign of patellofemoral pain syndrome: a prospective study. Radiology. 1992;185:859–863. doi: 10.1148/radiology.185.3.1438776. [DOI] [PubMed] [Google Scholar]
- 21.LaBella C. Patellofemoral pain syndrome: evaluation and treatment. Prim Care. 2004;31:977–1003. doi: 10.1016/j.pop.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 22.LaValley MP, McLaughlin S, Goggins J, Gale D, Nevitt MC, Felson DT. The lateral view radiograph for assessment of the tibiofemoral joint space in knee osteoarthritis: its reliability, sensitivity to change, and longitudinal validity. Arthritis Rheum. 2005;52:3542–3547. doi: 10.1002/art.21374. [DOI] [PubMed] [Google Scholar]
- 23.Merican AM, Amis AA. Iliotibial band tension affects patellofemoral and tibiofemoral kinematics. J Biomech. 2009;42:1539–1546. doi: 10.1016/j.jbiomech.2009.03.041. [DOI] [PubMed] [Google Scholar]
- 24.Moller BN, Moller-Larsen F, Frich LH. Chondromalacia induced by patellar subluxation in the rabbit. Acta Orthop Scand. 1989;60:188–191. doi: 10.3109/17453678909149251. [DOI] [PubMed] [Google Scholar]
- 25.Neyret P, Robinson AH, Le Coultre B, Lapra C, Chambat P. Patellar tendon length: the factor in patellar instability? Knee. 2002;9:3–6. doi: 10.1016/S0968-0160(01)00136-3. [DOI] [PubMed] [Google Scholar]
- 26.Nomura E, Horiuchi Y, Kihara M. Medial patellofemoral ligament restraint in lateral patellar translation and reconstruction. Knee. 2000;7:121–127. doi: 10.1016/S0968-0160(00)00038-7. [DOI] [PubMed] [Google Scholar]
- 27.Powers CM. Patellar kinematics, part I: the influence of vastus muscle activity in subjects with and without patellofemoral pain. Phys Ther. 2000;80:956–964. [PubMed] [Google Scholar]
- 28.Powers CM. Patellar kinematics, part II: the influence of the depth of the trochlear groove in subjects with and without patellofemoral pain. Phys Ther. 2000;80:965–978. [PubMed] [Google Scholar]
- 29.Powers CM, Shellock FG, Pfaff M. Quantification of patellar tracking using kinematic MRI. J Magn Reson Imaging. 1998;8:724–732. doi: 10.1002/jmri.1880080332. [DOI] [PubMed] [Google Scholar]
- 30.Powers CM, Ward SR, Fredericson M, Guillet M, Shellock FG. Patellofemoral kinematics during weight-bearing and non-weight-bearing knee extension in persons with lateral subluxation of the patella: a preliminary study. J Orthop Sports Phys Ther. 2003;33:677–685. doi: 10.2519/jospt.2003.33.11.677. [DOI] [PubMed] [Google Scholar]
- 31.Schulthies SS, Francis RS, Fisher AG, Van de Graaff KM. Does the Q angle reflect the force on the patella in the frontal plane? Phys Ther. 1995;75:24–30. doi: 10.1093/ptj/75.1.24. [DOI] [PubMed] [Google Scholar]
- 32.Souza DR, Gross MT. Comparison of vastus medialis obliquus: vastus lateralis muscle integrated electromyographic ratios between healthy subjects and patients with patellofemoral pain. Phys Ther. 1991;71:310–316. doi: 10.1093/ptj/71.4.310. [DOI] [PubMed] [Google Scholar]
- 33.Souza RB, Draper CE, Fredericson M, Powers CM. Femur rotation and patellofemoral joint kinematics: a weight-bearing magnetic resonance imaging analysis. J Orthop Sports Phys Ther. 2010;40:277–285. doi: 10.2519/jospt.2010.3215. [DOI] [PubMed] [Google Scholar]
- 34.Stefanik JJ, Roemer FW, Zumwalt AC, Zhu Y, Gross KD, Lynch JA, Frey-Law LA, Lewis CE, Guermazi A, Powers CM, Felson DT. Association between measures of trochlear morphology and structural features of patellofemoral joint osteoarthritis on MRI: the MOST study. J Orthop Res. 2012;30:1–8. doi: 10.1002/jor.21486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stefanik JJ, Zhu Y, Zumwalt AC, Gross KD, Clancy M, Lynch JA, Frey Law LA, Lewis CE, Roemer FW, Powers CM, Guermazi A, Felson DT. Association between patella alta and the prevalence and worsening of structural features of patellofemoral joint osteoarthritis: the multicenter osteoarthritis study. Arthritis Care Res (Hoboken). 2010;62:1258–1265. doi: 10.1002/acr.20214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ward SR, Shellock FG, Terk MR, Salsich GB, Powers CM. Assessment of patellofemoral relationships using kinematic MRI: comparison between qualitative and quantitative methods. J Magn Reson Imaging. 2002;16:69–74. doi: 10.1002/jmri.10124. [DOI] [PubMed] [Google Scholar]
- 37.Ward SR, Terk MR, Powers CM. Patella alta: association with patellofemoral alignment and changes in contact area during weight-bearing. J Bone Joint Surg Am. 2007;89:1749–1755. doi: 10.2106/JBJS.F.00508. [DOI] [PubMed] [Google Scholar]
- 38.Wilson T. The measurement of patellar alignment in patellofemoral pain syndrome: are we confusing assumptions with evidence? J Orthop Sports Phys Ther. 2007;37:330–341. doi: 10.2519/jospt.2007.2281. [DOI] [PubMed] [Google Scholar]


