Abstract
Conventionally, sarcopenia is defined by muscle mass and physical performance. We hypothesized that the disability caused by sarcopenia and sarcopenic obesity was related to the amount of adiposity or body weight bearing on a unit of muscle mass, or the adiposity to muscle ratio. We therefore examined whether this ratio could predict physical limitation by secondary analysis of the data in our previous study. We recruited 3,153 community-dwelling adults aged >65 years and their body composition was measured by dual-energy X-ray absorptiometry. Assessment of physical limitation was undertaken 4 years later. The relationship between baseline adiposity to muscle ratio and incident physical limitation was examined by logistic regression. In men, the adiposity to muscle ratios, namely total body fat to lower-limb muscle mass, total body fat to fat-free mass (FFM), and body weight to FFM, were predictive of physical limitation before and after adjustment for the covariates: age, Mini-mental Status Examination score, Geriatric Depression Scale score >8, and the diagnosis of chronic obstructive pulmonary disease, diabetes mellitus, hypertension, heart disease, and stroke (all p values < 0.001), when the total body fat to lower-limb muscle mass ratio was greater than or equal to 0.75. In women, throughout the entire range of that ratio, all three adiposity to muscle ratios were associated with physical limitation 4 years later both before and after adjustment for the same set of covariates (all p values < 0.05). Sarcopenia and sarcopenic obesity as measured by the body weight or adiposity bearing on a unit of muscle mass (the adiposity to muscle ratio) could predict incident or worsening physical limitation in older women across the entire range of the total body fat to lower-limb muscle mass ratio; and in older men when this ratio was equal to or greater than 0.75.
Keywords: Sarcopenia, Sarcopenic obesity, Elderly, Muscle mass, Fat mass, Physical limitations
Introduction
Sarcopenia is associated with physical disability in old age (Lee et al. 2007; Rolland et al. 2008; Cawthon et al. 2007; Laurentani et al. 2003; Topinkova 2008; Roubenoff 2003; Morley et al. 2001; Delmonico et al. 2007; Goodpaster et al. 2006; Janssen et al. 2002), although the definition of sarcopenia is still being debated in the literature. Conventionally, the definition of sarcopenia has adopted the method in osteoporosis, taking the two standard deviations below the mean of the young reference population as the cutoff for diagnosis (Baumgartner et al. 1998; Melton et al. 2000; Rolland et al. 2003). The European Working Group on Sarcopnia in Older People includes physical performance in the definition of sarcopenia rather than considering muscle mass alone (Cruz-Jentoft et al. 2010). An alternative method is to search for a cutoff value below which the risk of physical limitation is substantially increased, preferably in a prospective manner. We have attempted to examine sarcopenia in this latter approach in a cohort of older Chinese adults (Woo et al. 2009). A U-shaped relationship, however, was observed between physical limitation and muscle mass. Muscle mass was associated with physical limitation both below and paradoxically, above a certain value (Woo et al. 2009). It was postulated that the increase in physical limitation with increasing muscle mass is more likely a result of the increasing body mass index (BMI) or fat mass; or the associated fat infiltration into muscle (Kim et al. 2004; Goodpaster et al. 2001; Visser et al. 2002; Song et al. 2004; Visser et al. 2005; Beasley et al. 2009; Cesari et al. 2006). In the past, we (Auyeung et al. 2010) and others (Baumgartner et al. 1998; Forbes 1987; Iannuzzi-Sucich et al. 2002; Janssen et al. 2000) have demonstrated a consistent positive association between muscle mass and BMI. We carried out secondary analysis of this U-shaped relationship (Woo et al. 2009) and illustrated that the BMI values increased consistently along that U curve, confirming this speculation. In the ascending limb of the U curve, the increasing adiposity or body weight had exceeded the advantageous effect of increasing muscle mass, compatible with the phenomenon of sarcopenic obesity (SO). Studying muscle mass alone, without combining with the associated adverse effect of increasing fat mass or body weight may lead to erratic observation, particularly in the normal weight and overweight.
Sarcopenic obesity has been attributed as a major cause of disability in old age but the methods used to classify SO are variable (Baumgartner et al. 2004; Rolland et al. 2009; Bouchard et al. 2009; Lim et al. 2010; Kim et al. 2009; Broadwin et al. 2001). Baumgartner et al. (2004) first reported that SO as defined by both muscle mass and fat mass below and above a certain cutoff value, respectively, predicts disability. Broadwin et al. (2001) have illustrated that increased percentage of fat mass and decreased percentage of fat-free mass were associated with greater functional disability in older adults without categorizing muscle and fat mass into sarcopenia and obesity, respectively. The relative importance of sarcopenia and obesity in causing disability is intriguing. Rolland et al. (2009) observed that sarcopenia did not cause disability in the absence of obesity. Similarly, Bouchard et al. (2009) demonstrated that obesity contributed more to lower physical capacity than sarcopenia. Furthermore, fat mass has been shown to be a more important factor than appendicular muscle mass in determining walking speed in community-living older adults (Woo et al. 2007). Visser et al. (1998) have demonstrated that low skeletal muscle mass was not associated with self-reported physical disability and persons with high percent body fat had high level of disability; and that fat infiltration in muscle was a major determinant of disability (Visser et al. 2005, 2002). These studies suggest that when studying sarcopenia, fat mass should also be considered.
We hypothesized that the disability caused by SO was related to the amount of adiposity that was bearing on a unit of muscle mass, or the adiposity to muscle ratio. We therefore, proposed an alternative method in examining sarcopenia and SO, using three ratios: (1) total body fat to lower-limb muscle mass, (2) total body fat to fat-free mass (FFM), and (3) body weight to FFM; and performed a secondary analysis of the data in a previous study (Woo et al. 2009) to examine their relationships with incident or worsening physical limitation.
Methods
Four thousand community-dwelling men and women aged 65 years or over were recruited in a project primarily examining the bone mineral density of older Chinese adults. Only ethnical Chinese subjects were recruited. The study was approved by the Clinical Research Ethics Committee of the Chinese University of Hong Kong. Written informed consent were obtained from all participants.
Body height and weight were measured to calculate BMI (body weight in kilograms divided by the square of stature in meters). We measured muscle and fat mass by dual-energy X-ray absorptiometry (DXA) using a Hologic QDR 2000 densitometer (Hologic, Waltham, WA). Appendicular skeletal mass (ASM) was calculated by the summation of muscle mass measured in the four limbs, with the operator adjusting the cut lines of the limbs according to specific anatomical landmarks as described by Heymsfield et al. (1990). The method has been described in detail in other reports of the same cohort of older adults (Woo et al. 2009; Auyeung et al. 2010, 2008).
At baseline, the physical performance was measured by 6-m walking speed. At baseline and 4 years afterwards, a questionnaire was administered by two trained research assistants containing information regarding demographics, Mini-mental Status Examination score (MMSE) (Folstein et al. 1975), Geriatric Depression Scale (GDS) (Yesavage et al. 1983), and medical history including chronic obstructive pulmonary disease (COPD), heart disease, diabetes mellitus, hypertension, and stroke. Assessment of physical limitation was undertaken by two questions:
“Does your current health now limit you on the following activities?
Moderate activities such as moving a table, pushing a vacuum cleaner?
Climbing several flights of stairs?
If so, how much? None, moderate or severe.”
These two questions were part of the questionnaire used for the Osteoporotic Fractures in Men Study, an observational multicenter study of the determinants of fracture in older men initiated in the USA (Orwoll et al. 2005). Our center became a satellite center after the main study was initiated and women were also recruited. If the participant responded any new or worsening physical functioning 4 years later, they were taken as the incident or worsening physical limitation group. Those that reported no change were taken as comparison group. This response was analyzed as dependent variable in a binary manner.
Statistical methods
All analyses were undertaken separately for women and men. The 6-m walking speed was plotted against the muscle mass per height square. The risk of incident or worsening physical limitation of individual group of participants having a certain total body fat to lower-limb muscle mass ratio was represented graphically. If a unidirectional trend was observed, a single logistic regression would be employed to examine whether this ratio at baseline was predictive of incident or worsening physical limitation 4 years later by univariate and then multivariate analysis, adjusting for the covariates: age, MMSE score, GDS >8, and the diagnosis of COPD, diabetes mellitus, hypertension, heart disease, and stroke. If a bidirectional relationship was present instead, the analysis would be undertaken separately by subdividing the participants into two groups according to the turning point of the relationship. This point would be determined by testing regression analysis on either side of the curve where it yielded the maximum sum of squares of the regression coefficients from both sides. Separate logistic regression was then carried out after subdividing the participants according to this turning point of the total body fat to lower-limb muscle mass ratio.
The analysis was repeated with two other adiposity to muscle ratio, namely body weight to FFM and body fat to FFM. All tests were two-sided and a p value less than 0.05 were taken as statistically significant. The tests were undertaken by the statistical package SAS, version 9.1 (SAS Institute, Inc., Cary, North Carolina).
Results
At baseline, we recruited 2,000 men and 2,000 women. One hundred sixty-nine participants died and 651 defaulted the fourth year assessment. Therefore 1,566 men and 1,587 women were included into the final analysis which was a secondary analysis of the data we published previously (Woo et al. 2009). The mean age of the cohort was 71.9 years and 49.7 % were men. The baseline characteristics of the participants were tabulated in Table 1. Men and women had different baseline and body composition characteristics (Table 1) and were analyzed separately.
Table 1.
Baseline characteristics and incident or worsening of physical limitation
| Mean (SD) or frequency (%) | p value | ||
|---|---|---|---|
| Men (n = 1,566) | Women (n = 1,587) | ||
| Age (year) | 71.76 (4.67) | 72.03 (5.07) | 0.1255 |
| Total body fat (kg) | 15.32 (4.61) | 19.19 (5.12) | <0.0001 |
| Total body fat (%) | 24.32 (4.87) | 34.62 (5.09) | <0.0001 |
| FFM (kg) | 46.57 (5.52) | 35.42 (4.20) | <0.0001 |
| Weight (kg) | 61.90 (9.02) | 54.60 (8.39) | <0.0001 |
| LLMM (kg) | 14.31 (1.92) | 10.43 (1.45) | <0.0001 |
| Body fat/LLMM (kg/kg) | 1.07 (0.28) | 1.84 (0.41) | <0.0001 |
| Body fat/FFM (kg/kg) | 0.33 (0.08) | 0.54 (0.12) | <0.0001 |
| Weight/FFM (kg/kg) | 1.33 (0.08) | 1.54 (0.12) | <0.0001 |
| Body mass index | 23.52 (3.06) | 23.96 (3.36) | <0.0001 |
| MMSE score | 27.24 (2.47) | 24.62 (3.76) | <0.0001 |
| GDS > 8 | 112 (7.15) | 153 (9.65) | 0.0116 |
| COPD | 157 (10.03) | 75 (4.73) | <.0001 |
| Diabetes mellitus | 222 (14.18) | 220 (13.86) | 0.7998 |
| Hypertension | 647 (41.32) | 694 (43.73) | 0.1702 |
| Heart disease | 275 (17.56) | 257 (16.19) | 0.3056 |
| Stroke | 71 (4.53) | 54 (3.40) | 0.1036 |
| New or worsening physical limitation in 4 years | 366 (23.37) | 592 (37.30) | <.0001 |
LLMM lower-limb muscle mass, FFM fat-free mass, MMSE mini-mental status examination, GDS geriatric depression scale, COPD chronic obstructive pulmonary disease
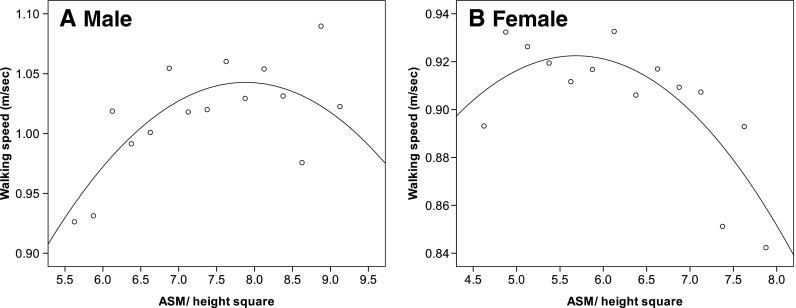
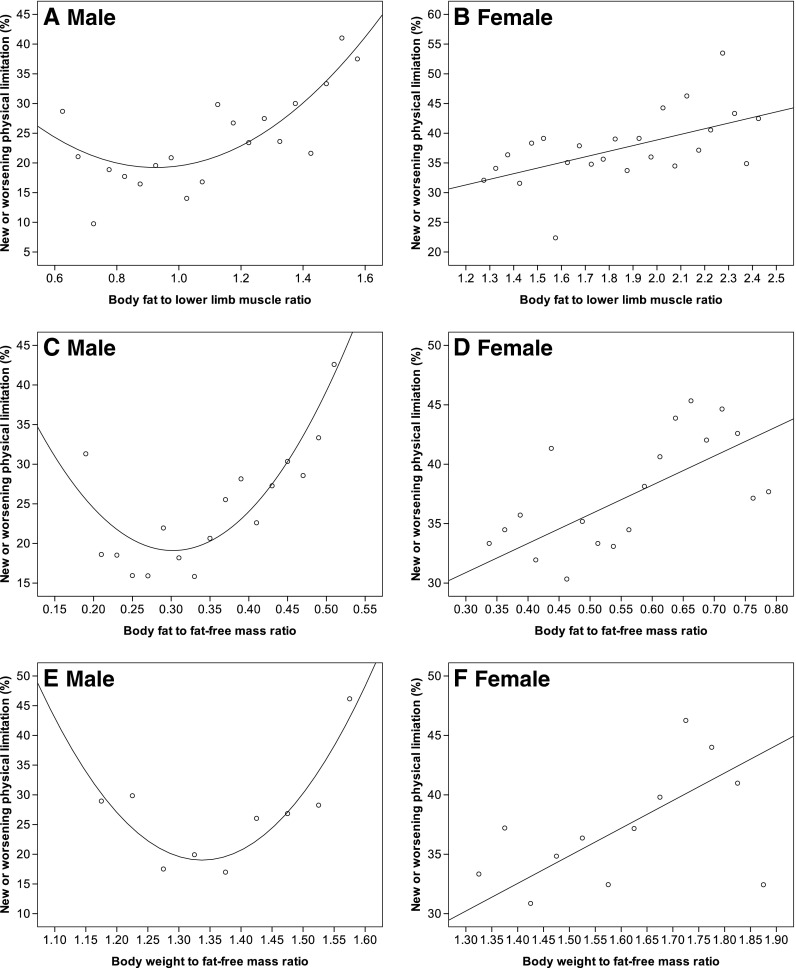
The 6-m walking speed followed an inverted U-shaped curve with increasing muscle mass in both men and women (Fig. 1). The relationship between physical limitation and total body fat to lower-limb muscle mass ratio, in men, was U-shaped (quadratic regression, R2 = 0.568, p < 0.0001; Fig. 2). As such the analysis in men was divided into two groups according to the turning point of the curve which was determined to be a ratio value of 0.75, according to the method described in the method section. All three adiposity to muscle ratios, namely body fat to lower-limb muscle mass, body fat to FFM, and body weight to FFM, were predictive of incident or worsening physical limitation before and after adjustment both when the value was above or below 0.75 though the associations were in the opposite direction (Table 2). When the ratio was less than 0.75, the models explained from 17.1 to 19 % variation in the risk of any new or worsening physical limitation; and 4.8 to 4.9 % when it was greater than or equal to 0.75 (McFadden R2, Table 2).
Fig. 1.
Relationship between walking speed and muscle mass
Fig. 2.
Relationship between physical limitation and adiposity to muscle ratios
Table 2.
Relationship between baseline adiposity to muscle ratio and physical limitation after 4 years
| New or worsening physical limitation in 4 years | ||||||||
|---|---|---|---|---|---|---|---|---|
| Crude OR (95 % CI) | Wald | p value | McFadden's R2 of model | Adjusted OR (95 % CI) | Wald | p value | McFadden's R2 of model | |
| Men | ||||||||
| Body fat/LLMM <0.75 | ||||||||
| Body fat/LLMM | 0.431 (0.190, 0.978) | 4.056 | 0.044 | 0.019 | 0.373 (0.145, 0.956) | 4.213 | 0.040 | 0.171 |
| Body fat/FFM | 0.371 (0.170, 0.810) | 6.197 | 0.013 | 0.029 | 0.324 (0.130, 0.804) | 5.902 | 0.015 | 0.180 |
| Body weight/FFM | 0.371 (0.170, 0.810) | 6.197 | 0.013 | 0.029 | 0.324 (0.130, 0.804) | 5.902 | 0.015 | 0.180 |
| ASM/height square | 0.478 (0.318, 0.719) | 12.595 | 0.0004 | 0.065 | 0.479 (0.293, 0.783) | 8.615 | 0.003 | 0.195 |
| FFM/height square | 0.536 (0.362, 0.796) | 9.595 | 0.002 | 0.048 | 0.531 (0.329, 0.858) | 6.689 | 0.010 | 0.184 |
| Body fat/LLMM ≥0.75 | ||||||||
| Body fat/LLMM | 1.454 (1.246, 1.697) | 22.497 | <.0001 | 0.015 | 1.355 (1.155, 1.590) | 13.895 | 0.0002 | 0.049 |
| Body fat/FFM | 1.419 (1.214, 1.660) | 19.303 | <.0001 | 0.013 | 1.340 (1.141, 1.574) | 12.691 | 0.0004 | 0.048 |
| Body weight/FFM | 1.419 (1.214, 1.660) | 19.303 | <.0001 | 0.013 | 1.340 (1.141, 1.574) | 12.691 | 0.0004 | 0.048 |
| Women | ||||||||
| All body fat/LLMM | ||||||||
| Body fat/LLMM | 1.143 (1.029, 1.271) | 6.166 | 0.013 | 0.003 | 1.136 (1.018, 1.266) | 5.245 | 0.022 | 0.017 |
| Body fat/FFM | 1.127 (1.015, 1.252) | 4.996 | 0.025 | 0.002 | 1.125 (1.009, 1.254) | 4.530 | 0.033 | 0.017 |
| Body weight/FFM | 1.127 (1.015, 1.252) | 4.996 | 0.025 | 0.002 | 1.125 (1.009, 1.254) | 4.530 | 0.033 | 0.017 |
Numbers are OR increase per one SD increase in the adiposity to muscle ratio
Adjusted for age, Mini-mental status examination score, Geriatric depression scale score > 8, chronic obstructive pulmonary disease, diabetes mellitus, hypertension, heart disease, stroke
LLMM lower limb muscle mass, FFM fat-free mass, CI confidence interval, OR odds ratio
In women, the incidence of any new or worsening physical limitation increased consistently from the lowest to the highest body fat to lower-limb muscle mass ratio (linear regression, R2 = 0.358, p < 0.0001; Fig. 2). Therefore the analysis was undertaken without subdivision. A higher ratio in any one of the three adiposity to muscle ratios was associated with a higher probability of incident or worsening physical limitation 4 years later both before and after adjustment (Table 2). The models explained 1.7 % variation in the risk of any new or worsening physical limitation (McFadden R2, Table 2).
Discussion
In the secondary analysis of our previous study (Woo et al. 2009), we have observed that in the ascending limb of the physical limitation and muscle mass relationship curve, it was the increasing BMI that caused disability, revealing the adverse effect of SO. This observation is further supported by the present study, in which we have demonstrated again an inverted U-shaped relationship between objective physical performance test and muscle mass, signifying the paradoxical deterioration in physical performance with increasing muscle mass in the descending limb of the curves (Fig. 1).
We attempted to assess SO quantitatively by measuring the amount of weight or adiposity bearing on one unit of muscle mass as represented by the adiposity (body weight or total body fat mass) to muscle ratio. By employing this ratio, the paradoxical U-shaped relationship of our previous study (Woo et al. 2009) was transformed into a unidirectional one in women (Fig. 2b, d, f), though not in men (Fig. 2a, c, e).
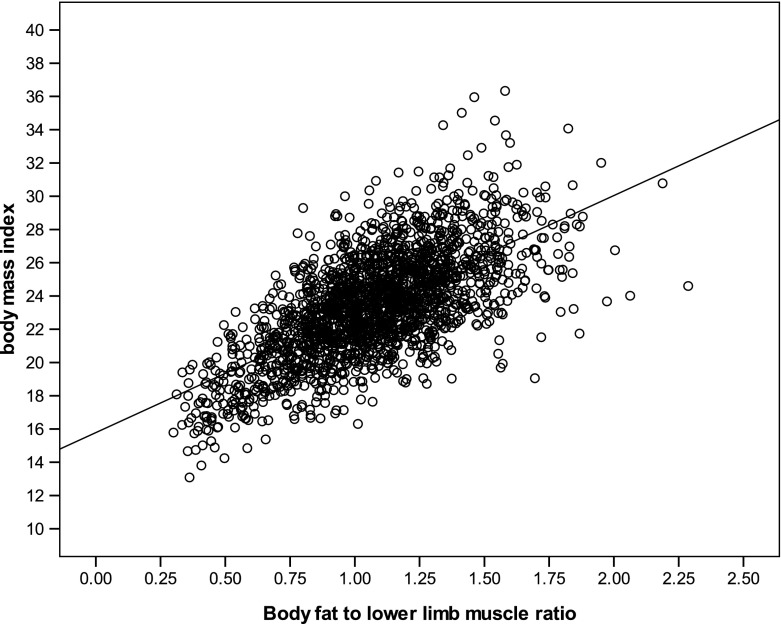
We have demonstrated the risk of physical limitation increased across the entire range of adiposity to muscle ratio in women and in men when the ratio was above 0.75. Our hypothesis that disability was associated with the amount of adiposity or body weight bearing on one unit of muscle, however, became invalid in men when the ratio was below 0.75. This ratio appeared to be protective rather than hazardous or the risk decreased with increasing adiposity to muscle ratio. We postulated that they belonged to the underweight group in whom increasing adiposity may be advantageous instead. As such, we have examined the relationship between BMI and adiposity to muscle ratio and revealed a significant correlation by linear regression (Fig. 3), in which a ratio of 0.75 corresponded to a BMI value of 21. We tested further whether in this lower range of the ratio or BMI (ratio < 0.75 or BMI < 21), muscle mass alone could yield a non-paradoxical protective relationship instead. The risk of physical limitation decreased with increasing muscle mass in this range (Table 2). In men, therefore, there appeared a dividing point, below which muscle mass is the determinant of disability alone and above which, muscle and fat have to be considered collectively. In women, in contrary, the adiposity to muscle ratio is a valid predictor across the entire range of body composition. This may indicate that even in the underweight range, body weight exceeding the supporting capacity of muscle could determine disability in women but not in men. This observation is compatible with the survey undertaken by Visser et al., which failed to observe any association between muscle mass and physical function (Visser et al. 1998), and other studies demonstrating the combined effect of adiposity and muscle, instead of muscle alone (Cesari et al. 2006; Auyeung et al. 2010; Janssen et al. 2000; Rolland et al. 2009; Bouchard et al. 2009; Lim et al. 2010). Perhaps, the disability in women is more body weight or adiposity dependent and in men it is more muscle dependent particularly in the underweight range. However, the underlying mechanism of this gender variation is still unknown at present.
Fig. 3.
Relationship between BMI and total body fat to lower limb muscle mass ratio BMI = 21.1 when the total body fat to lower limb muscle mass ratio = 0.75 R2 = 0.434, p < 0.001
In our previous study (Woo et al. 2009), one of our analyses was examining the relationship between the risk of physical limitation and the muscle mass to body weight ratio, which mathematically was similar to the inverse of body weight to FFM ratio, one of the three ratios used in the present study. The two ratios, however, represented different meanings. The muscle mass to body weight ratio (Woo et al. 2009) was employed to achieve a better correction of body build as proposed by another study (Estrada et al. 2007) while the body weight to FFM ratio in the present study represented the amount of body weight bearing on one unit of muscle mass.
Older women were more likely to report new or worsening limitation after 4 years in general (Table 1). In men, however, the risk of physical limitation rose more steeply with every unit change of adiposity to muscle ratio (Fig. 2 and Table 2).
We did not observe a threshold value of either muscle mass or adiposity to muscle ratio at which the incident of physical limitation starting to rise substantially. Instead, physical limitation incidence rose uniformly with increasing adiposity to muscle ratio (Fig. 2b). Adopting a certain cutoff value to categorize muscle mass or adiposity to muscle ratio may not be an appropriate approach in the definition of sarcopenia or SO.
Our survey has several limitations. Our sample was not generated from population random sampling but rather by voluntary participation. We have a considerable defaulter rate (16.3 %) and some subjects died (4.9 %) in between these 4 years. As such, the sample was biased towards those who were healthier and physically more active. Physical limitation was defined by self-report and therefore it would be subjected to reporting error. The use of DXA to measure regional muscle mass (lower-limb muscle mass) is not readily available. We have deliberately included body weight to FFM and total body fat to FFM ratio into our analyses because these parameters can be measured by bio-impedance method. The data we had were derived from DXA and though they were predictive of physical limitation, it is uncertain whether bio-impedance measurement can predict disability similarly. This warrants future studies. If body weight to FFM ratio by bio-impedance method can be shown to be equally predictive, this adiposity to muscle ratio taken as a measurement SO can then be widely employed in clinical practice to predict future disability risk. Body composition is ethnic dependent and the body composition values or ratio derived in this survey may not be applicable to other ethnic groups. Whether adiposity to muscle ratio can be applied as a measurement of SO in other ethnicities remains uncertain.
We have followed a relatively large cohort of older adults for an optimal period of 4 years to observe the new emergence or worsening of the existing physical limitation. Being prospective rather than cross-sectional, the SO assessment method, namely the adiposity to muscle ratio, perhaps can be considered an alternative method.
Conclusion
Sarcopenia and sarcopenic obesity as measured by the body weight or adiposity bearing on a unit of muscle mass (the adiposity to muscle ratio) could predict incident or worsening physical limitation in older women across the entire range of the total body fat to lower-limb muscle mass ratio; and in older men when this ratio was equal to or greater than 0.75.
Footnotes
This work was done at: The S. H. Ho Centre for Gerontology and Geriatrics, The Chinese University of Hong Kong
References
- Auyeung TW, Kwok T, Lee J, Leung J, Leung PC, Woo J. Functional decline in cognitive impairment—the relationship between physical and cognitive function. Neuroepidemiol. 2008;31:167–173. doi: 10.1159/000154929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auyeung TW, Lee JSW, Leung J, Kwok T, Leung PC, Woo J. Survival in older men may benefit from being slightly overweight and centrally obese—a five-year follow up study in 4000 older adults using DXA. J Gerontol Med Sci. 2010;65:M99–M104. doi: 10.1093/gerona/glp099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumgartner RN, Koehler KM, Gallagher D, et al. Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol. 1998;147:755–763. doi: 10.1093/oxfordjournals.aje.a009520. [DOI] [PubMed] [Google Scholar]
- Baumgartner RN, Wayne SJ, Waters DL, Janssen I, Gallagher D, Morley JE. Sarcopenic obesity predicts instrumental activities of daily living disability in the elderly. Obes Res. 2004;12:1995–2004. doi: 10.1038/oby.2004.250. [DOI] [PubMed] [Google Scholar]
- Beasley LE, Koster A, Newman AB, et al. The Health ABC Study. Inflammation and race and gender differences in computerized tomography-measured adipose depots. Obesity. 2009;17:1062–1069. doi: 10.1038/oby.2008.627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouchard DR, Dionne IJ, Brochu M. Sarcopenic/obesity and physical capacity in older men and women: data from the nutrition as a determinant of successful aging (NuAge)—the Quebec Longitudinal Study. Obesity. 2009;17:2082–2088. doi: 10.1038/oby.2009.109. [DOI] [PubMed] [Google Scholar]
- Broadwin J, Goodman-Gruen D, Slymen D. Ability of fat and fat-free mass percentages to predict functional disability in older men and women. J Am Geriatr Soc. 2001;49:1641–1645. doi: 10.1111/j.1532-5415.2001.49273.x. [DOI] [PubMed] [Google Scholar]
- Cawthon PM, Marshall LM, Michael Y, et al. Frailty in older men: prevalence, progression, and relationship with mortality. J Am Geriatr Soc. 2007;55:1216–23. doi: 10.1111/j.1532-5415.2007.01259.x. [DOI] [PubMed] [Google Scholar]
- Cesari M, Leeuwenburgh C, Lauretani F, et al. Frailty syndrome and skeletal muscle: results from the Invecchiare in Chianti study. Am J Clin Nutr. 2006;83:1142–1148. doi: 10.1093/ajcn/83.5.1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Report of the European working group on sarcopenia in older people Sarcopenia: European consensus on definition and diagnosis. Age Ageing. 2010;39:412–423. doi: 10.1093/ageing/afq034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delmonico MJ, Harris TB, Lee JS, et al. Alternative definitions of sarcopenia, lower extremity performance, and functional impairment with aging in older men and women. J Am Geriatr Soc. 2007;55:769–74. doi: 10.1111/j.1532-5415.2007.01140.x. [DOI] [PubMed] [Google Scholar]
- Estrada M, Kleppinger A, Judge JO, et al. Functional impact of relative versus absolute sarcopenia in healthy older women. J Am Geriatr Soc. 2007;55:1712–1719. doi: 10.1111/j.1532-5415.2007.01436.x. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. ‘Mini-mental state’. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Forbes GB. Lean body mass-body fat interrelationships in humans. Nutr Rev. 1987;5:225–231. doi: 10.1111/j.1753-4887.1987.tb02684.x. [DOI] [PubMed] [Google Scholar]
- Goodpaster BH, Carlson CL, Visser M, et al. Attenuation of skeletal muscle and strength in the elderly: the Health ABC Study. J Appl Physiol. 2001;90:2157–2165. doi: 10.1152/jappl.2001.90.6.2157. [DOI] [PubMed] [Google Scholar]
- Goodpaster BH, Park SW, Harris TB, et al. The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. J Gerontol A Biol Sci Med Sci. 2006;61:1059–64. doi: 10.1093/gerona/61.10.1059. [DOI] [PubMed] [Google Scholar]
- Heymsfield SB, Smith R, Aulet M, et al. Appendicular skeletal muscle mass: measurement by dual-energy X-ray absorptiometry. Am J Clin Nutr. 1990;52:214–218. doi: 10.1093/ajcn/52.2.214. [DOI] [PubMed] [Google Scholar]
- Iannuzzi-Sucich M, Prestwood KM, Kenny AM. Prevalence of sarcopenia and predictors of skeletal muscle mass in healthy, older men and women. J Gerontol Med Sci. 2002;57A:M772–M777. doi: 10.1093/gerona/57.12.M772. [DOI] [PubMed] [Google Scholar]
- Janssen I, Heymsfield SB, Wang Z, Ross R. Skeletal muscle mass and distribution in 468 men and women age 18–99 yr. J Appl Physiol. 2000;89:81–88. doi: 10.1152/jappl.2000.89.1.81. [DOI] [PubMed] [Google Scholar]
- Janssen I, Heymsfield SB, Ross R. Low relative skeletal muscle mass (Sarcopenia) in older persons is associated with functional impairment and physical disability. J Am Geriatr Soc. 2002;50:889–896. doi: 10.1046/j.1532-5415.2002.50216.x. [DOI] [PubMed] [Google Scholar]
- Kim J, Heshka S, Gallagher D, et al. Intermuscular adipose tissue-free skeletal muscle mass: estimation by dual-energy X-ray absorptiometry in adults. J Appl Physiol. 2004;97:655–660. doi: 10.1152/japplphysiol.00260.2004. [DOI] [PubMed] [Google Scholar]
- Kim TN, Yang SJ, Yoo HJ, Lim KI, Kang HJ, Song W, Seo JA, Kim SG, Kim NH, Baik SH, Choi DS, Choi KM. Prevalence of sarcopenia and sarcopenic obesity in Korean adults: the Korean sarcopenic obesity study. Int J Obes. 2009;33:885–892. doi: 10.1038/ijo.2009.130. [DOI] [PubMed] [Google Scholar]
- Laurentani F, Russo C, Bandinelli S, et al. Age-associated changes in skeletal muscles and their effect on mobility: an operational diagnosis of sarcopenia. J Appl Physiol. 2003;95:1851–60. doi: 10.1152/japplphysiol.00246.2003. [DOI] [PubMed] [Google Scholar]
- Lee JSW, Auyeung TW, Kwok T, Leung PC, Lau E, Woo J. Associated factors and health impact of sarcopenia in older Chinese men and women: a cross-sectional study. Gerontology. 2007;53:166–172. doi: 10.1159/000107355. [DOI] [PubMed] [Google Scholar]
- Lim S, Kim JH, Yoon JW, Kang SM, Choi SH, Park YJ, Kim KW, Lim JY, Park KS, Jang HC. Sarcopenic obesity: prevalence and association with metabolic syndrome in the Korean Longitudinal Study on Health and Aging (KLoSHA) Diabetes Care. 2010;33:1652–1654. doi: 10.2337/dc10-0107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melton LJ, III, Khosla S, Crowson CS, et al. Epidemiology of sarcopenia. J Am Geriatr Soc. 2000;48:625–630. [PubMed] [Google Scholar]
- Morley JE, Baumgartner RN, Roubenoff R, et al. Sarcopenia. J Lab Clin Med. 2001;137:231–243. doi: 10.1067/mlc.2001.113504. [DOI] [PubMed] [Google Scholar]
- Orwoll E, Blank JB, Barrett-Connor E, et al. Design and baseline characteristics of the Osteoporotic Fractures in Men (MrOS) Study—a large observational study of the determinants of fracture in older men. Contemp Clin Trials. 2005;26:569–585. doi: 10.1016/j.cct.2005.05.006. [DOI] [PubMed] [Google Scholar]
- Rolland Y, Lauwers-Cances V, Cournot M, et al. Sarcopenia, calf circumference, and physical function of elderly women: a cross-sectional study. J Am Geriatr Soc. 2003;51:1120–1124. doi: 10.1046/j.1532-5415.2003.51362.x. [DOI] [PubMed] [Google Scholar]
- Rolland Y, Czerwinski S, Van Kan Abellan G, et al. Sarcopenia: its assessment, etiology, pathogenesis, consequences and future perspectives. J Nutr Health Aging. 2008;12:433–50. doi: 10.1007/BF02982704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rolland Y, Lauwers-Cances V, Cristini C, van Kan Abellan G, Janssen I, Morley JE, Vellas B. Difficulties with physical function associated with obesity, sarcopenia, and sarcopenic-obesity in community-dwelling elderly women: the EPIDOS (EPIDemiologie de l'OSteoporose) Study. Am J Clin Nutr. 2009;89:1895–900. doi: 10.3945/ajcn.2008.26950. [DOI] [PubMed] [Google Scholar]
- Roubenoff R. Sarcopenia: effects on body composition and function. J Gerontol A Biol Sci Med Sci. 2003;58A:1012–1017. doi: 10.1093/gerona/58.11.M1012. [DOI] [PubMed] [Google Scholar]
- Song MY, Ruts E, Kim J, Janumala I, Heymsfield S, Gallagher D. Sarcopenia and increased adipose tissue infiltration of muscle in elderly African American women. Am J Clin Nutr. 2004;79:874–880. doi: 10.1093/ajcn/79.5.874. [DOI] [PubMed] [Google Scholar]
- Topinkova E. Aging, disability and frailty. Ann Nutr Metab. 2008;52(1):6–11. doi: 10.1159/000115340. [DOI] [PubMed] [Google Scholar]
- Visser M, Harris TB, Langlois J, Hannan MT, et al. Body fat and skeletal muscle mass in relation to physical disability in very old men and women of the Framingham Heart Study. J Gerontol Med Sci. 1998;53A:M214–M221. doi: 10.1093/gerona/53A.3.M214. [DOI] [PubMed] [Google Scholar]
- Visser M, Kritchevsky SB, Goodpaster BH, Newman AB, Nevitt M, Stamm E, Harris TB (2002) Leg muscle mass and composition in relation to lower extremity performance in men and women aged 70 to 79: the health, aging and body composition study. J Am Geriatr Soc 50(5):897–904 [DOI] [PubMed]
- Visser M, Goodpaster BH, Kritchevsky SB, Newman AB, Nevitt M, Rubin SM, Simonsick EM, Harris TB (2005) Muscle mass, muscle strength, and muscle fat infiltration as predictors of incident mobility limitations in well-functioning older persons. J Gerontol A Biol Sci Med Sci 60(3):324–33 [DOI] [PubMed]
- Woo J, Leung J, Kwok T. BMI, body composition, and physical functioning in older adults. Obesity. 2007;15:1886–1894. doi: 10.1038/oby.2007.223. [DOI] [PubMed] [Google Scholar]
- Woo J, Leung J, Sham A, Kwok T. Defining sarcopenia in terms of risk of physical limitations: a 5-year follow-up study of 3,153 Chinese men and women. J Am Geriatr Soc. 2009;57:2224–2231. doi: 10.1111/j.1532-5415.2009.02566.x. [DOI] [PubMed] [Google Scholar]
- Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, et al. Development and validation of a geriatric depression screening scale. J Psychiatr Res. 1983;17:37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]