Abstract
This study aimed to explore the prognosis of very old people depending on their cardiovascular disease (CVD) history. This observational prospective cohort study included 570 participants aged 85 years from the general population with 5-year follow-up for morbidity, functional status, and mortality. At baseline, participants were assigned to three groups: no CVD history, “minor” CVD (angina pectoris, transient ischemic attack, intermittent claudication, and/or heart failure), or “major” CVD (myocardial infarction [MI], stroke, and/or arterial surgery). Follow-up data were collected on MI, stroke, functional status, and cause-specific mortality. The composite endpoint included cardiovascular events (MI or stroke) and cardiovascular mortality. At baseline, 270 (47.4 %) participants had no CVD history, 128 (22.4 %) had minor CVD, and 172 (30.2 %) had major CVD. Compared to the no CVD history group, the risk of the composite endpoint increased from 1.6 (95 % confidence interval [CI], 1.1–2.4) for the minor CVD group to 2.7 (95 % CI, 2.0–3.9) for the major CVD group. Similar trends were observed for cardiovascular and all-cause mortality risks. In a direct comparison, the major CVD group had a nearly doubled risk of the composite endpoint (hazard ratio, 1.8; 95 % CI, 1.2–2.7), compared to the minor CVD group. Both minor and major CVD were associated with an accelerated decline in cognitive function and accelerated increase of disability score (all p < 0.05), albeit most pronounced in participants with major CVD. CVD disease status in very old age is still of important prognostic value: a history of major CVD (mainly MI or stroke) leads to a nearly doubled risk of poor outcome, including cardiovascular events, functional decline, and mortality, compared with a history of minor CVD.
Keywords: Aged 80 and over, Cardiovascular disease, Prevention, Cardiovascular morbidity, Functional status, Mortality
Introduction
Cardiovascular disease (CVD) is characterized by a high prevalence and incidence up to the highest age groups. Moreover, cardiovascular morbidity is an important cause of disability and, from middle age onwards, CVD is the leading cause of death (Roger et al. 2011; McDermott 2007). Therefore, prevention of cardiovascular events has high priority and risk prediction models have been developed.
In daily practice, populations are usually dichotomized into people with known atherothrombotic CVD, such as coronary heart disease, stroke/transient ischemic attack (TIA), and peripheral arterial disease, and people without those manifest conditions, but possibly with risk factors for CVD, such as hypertension, hypercholesterolemia, diabetes, or smoking (Wilson et al. 1998; Wilson 2011; Graham et al. 2007; Dornbrook-Lavender et al. 2003). Persons without manifest CVD theoretically qualify for the so-called primary prevention, be it on a population scale or on a more personal level when their calculated CVD risk exceeds predefined thresholds (Graham et al. 2007; Wald et al. 2011). Persons with prior CVD are known to have a high risk of recurrent CVD (Kerr et al. 2009; Vaartjes et al. 2010; Steg et al. 2007; van Wijk et al. 2005) and should, therefore, receive optimal “secondary prevention,” including lifestyle advice and preventive medication.
Despite evidence of its value also in old age, elderly people do not receive optimal preventive treatment even after major events (Arnold et al. 2011; Kvan et al. 2006; Bhatt et al. 2006). At very old age, drug interactions, intoxications, and adverse effects can have serious impact on the quality of life (Banerjee et al. 2011) Therefore, further risk differentiation within those with prior CVD might help clinicians to select those at the highest risk of recurrent events. In younger age groups, it is already known that patients with prior CVD are at the highest risk of a recurrent cardiovascular event (Kerr et al. 2009). Within patients with prior CVD, a recent study showed that a history of ischemic events leads to a greater risk of future events than a history of stable coronary, cerebrovascular, or peripheral artery disease (Bhatt et al. 2010). At present, it is unknown whether these findings can also be applied to patients aged 85 and over.
We hypothesized that subgroups with different risks of recurrent CVD might also be observed within the population of the oldest old. A history of myocardial infarction (MI) or stroke might have a different prognosis than a history of relatively “minor” CVD such as stable angina or claudication, TIA, or milder cases of heart failure. This may have clinical consequences for the format and intensity of secondary prevention in these groups of older people.
We investigated whether differences in prognosis exist between very old people with various levels of prevalent CVD, compared to those with no manifest CVD. Since in older populations the outcomes “morbidity” and “functional status” become even more important than mortality, we studied the prognosis not only regarding (cause-specific) mortality, but also with respect to recurrent CVD morbidity and functional status.
Methods
Study population
The Leiden 85-plus Study is a prospective population-based study in 85-year-old inhabitants of the city of Leiden, The Netherlands. The study design and characteristics of the cohort have previously been described in detail (der Wiel et al. 2002; van Exel et al. 2002). In brief, between September 1997 and September 1999, 705 people from the 1912–1914 birth cohorts living in the city of Leiden who reached the age of 85 years were eligible to participate. No exclusion criteria were used. From the 705 people who were eligible at age 85, 92 refused participation and 14 died before enrolment. A total of 599 (87 %) people gave informed consent and were enrolled. At baseline and yearly up to the age of 90 years, participants were visited at their place of residence to obtain extensive data on health, functioning, and well-being. In addition, a medical history was obtained from the participant’s primary care physician. For all participants, classic cardiovascular risk factors were determined. The Medical Ethics Committee of the Leiden University Medical Centre approved the study.
Prevalence of CVD at age 85 years
For each participant, the primary care physician was interviewed about the history of CVD using a standardized questionnaire, which included questions on present and past cardiovascular pathologies, including MI, stroke, surgery for arterial disease (aorta, carotid, coronary, or peripheral arteries), angina pectoris, TIA, intermittent claudication, and heart failure. An ECG was recorded. The presence of MI on the ECG was defined as the presence of Minnesota Code 1-1 or 1-2 (excluding 1-2-8). Participants were assigned to three different groups according to their CVD status: a group with no known history of CVD (reference group), a group with a history of “minor” CVD, and a group with a history of “major” CVD. Minor CVD was considered present if the primary care physician had recorded a history of angina pectoris, TIA, intermittent claudication, and/or heart failure. Major CVD was defined as a history of MI (including MI on baseline ECG), stroke, or surgery for arterial disease (aorta, carotid, coronary, or peripheral arteries). These criteria for minor and major CVD were based on literature in younger age groups (Bhatt et al. 2006; Rosengren et al. 1998).
Clinical endpoints
(Non)fatal myocardial infarction
Up to 90 years of age, all incident fatal and nonfatal MIs were annually registered using data from the primary care physician, ECGs, and death registration forms. Incident MI on the ECG was defined as the appearance of Minnesota Code 1-1 or 1-2 or Minnesota Code 1-3 in combination with the first appearance of Minnesota Code 5-x in the same myocardial area (Macfarlane and Latif 1996). A fatal incident MI was categorized by cause of death codes I21–I23 (International Classification of Diseases [ICD]-10).
(Non)fatal stroke
Information on incident stroke was collected annually from the primary care physician up to 90 years of age. A fatal incident stroke was categorized by cause of death codes I61–I69 (ICD-10).
Incident cardiovascular events or cardiovascular mortality
The composite endpoint “incident cardiovascular events or cardiovascular mortality” was defined as fatal and nonfatal MI, fatal and nonfatal stroke, or other cardiovascular mortality.
Mortality
All participants were followed up for mortality until the age of 95 years. Dates and causes of death were obtained from civic and national registries. Causes of death were divided into cardiovascular causes (ICD-10 codes I00–I99) and noncardiovascular causes (all other ICD-10 codes). Assignment of cause of death was done blinded for baseline and follow-up study data.
Functional status
Up to 90 years of age, participants were annually visited by a research nurse at their place of residence. Cognitive function was assessed by the Mini-Mental State Examination (MMSE) with scores ranging from 0 to 30 points (optimal) (Tombaugh and McIntyre 1992). Disability was assessed using the Activities of Daily Living (ADL) items from the Groningen Activity Restriction Scale with scores ranging from 9 (optimal) to 36 points (Kempen et al. 1996). In those with MMSE scores above 18, Cantril’s Ladder of Life with a score from 1 to 10 (optimal) points was used as a measure of general well-being (Cantril 1965) and the 15-item Geriatric Depression Scale (GDS) with scores ranging from 0 (optimal) to 15 points was used to screen for depressive symptoms (de Craen et al. 2003).
Statistical analysis
Differences in baseline characteristics between the groups according to CVD status were analyzed with the chi-square test for categorical variables and the Jonckheere–Terpstra test for continuous variables. Time-to-event curves were constructed with the Kaplan–Meier method and compared using a log-rank test. If no exact time to event was available, the time to event was calculated as halfway that particular year. Mortality and morbidity hazard ratios (HR) and corresponding 95 % confidence intervals (CIs) were calculated in a Cox proportional hazards model adjusted for sex. The same HRs were calculated in a model with additional adjustments for the use of antihypertensive medication, income, and level of education. Incidence rate was calculated using the timetable method as number of incidents per 1,000 person-years at risk with corresponding 95 % CIs. Differences in cognitive function (MMSE), changes in disability (ADL), general well-being (Cantril), and depressive symptoms (GDS) were estimated using linear mixed models adjusted for sex and are presented as (predicted) means with standard errors. As a first sensitivity analysis, the stratification in groups according to CVD status was repeated at the age of 90 years, with updated information about incidence of cardiovascular events from 85 to 90 years of age. A second sensitivity analysis was done with risk groups according to site of CVD: a group with a history of cardiac CVD (angina pectoris and/or MI), a group with a history of cerebrovascular CVD (TIA and/or stroke), a group with a history of peripheral CVD (intermittent claudication and/or surgery for noncoronary arterial disease), and a group with a history of CVD at multiple sites. Data analysis was performed using SPSS 17.0 for Windows (SPSS Inc., Chicago, IL, USA).
Results
Baseline characteristics
For 570 of the 599 participants, all baseline measurements were available. At 85 years of age, 270 (47.4 %) participants had no history of CVD, 128 (22.4 %) participants had minor CVD, and 172 (30.2 %) participants had major CVD (Table 1). Participants with major CVD were more often men (47 versus 27 % for minor CVD and 28 % for no CVD, p trend < 0.001) and more often institutionalized (23 versus 18 % for minor CVD and 15 % for no CVD, p trend = 0.048). They had higher scores of disability (p trend = 0.009) and their MMSE scores were the lowest (p trend < 0.001). Only 36 % of the participants with minor CVD and 51 % of the participants with major CVD used aspirin or oral anticoagulants. Median systolic blood pressure was 154 mmHg (interquartile range [IQR], 143–166), median total cholesterol was 5.7 mmol/L (IQR, 4.9–6.4). Participants with major CVD had lower HDL cholesterol levels (p trend < 0.001). Use of statins was minimal: no more than 1 % of all participants used lipid-lowering drugs. From all participants with heart failure (n = 74), more than half (n = 38 [51 %]) also had a history of major CVD.
Table 1.
Baseline characteristics of participants from the Leiden 85-plus Study (n = 570), depending on cardiovascular history
| Total | CVD history | p for trenda | |||
|---|---|---|---|---|---|
| 570 (100) | None 270 (47.4) | Minor 128 (22.4) | Major 172 (30.2) | ||
| Sociodemographic characteristics | |||||
| Women | 379 (67) | 195 (72) | 93 (73) | 91 (53) | <0.001 |
| Net monthly income >750€ | 276 (49) | 147 (55) | 52 (41) | 77 (45) | 0.058 |
| Post primary school education | 197 (35) | 104 (39) | 41 (32) | 52 (31) | 0.091 |
| Noninstitutionalized living | 467 (82) | 229 (85) | 105 (82) | 133 (77) | 0.048 |
| Functional status | |||||
| Cognitive function (MMSE) | 26 (22–28) | 27 (24–29) | 26 (23–28) | 25 (19–28) | <0.001 |
| ADL disability | 10 (9–15) | 10 (9–13) | 10 (9–15) | 10 (9–16) | 0.009 |
| Subjective well-being (Cantril) b | 8 (7–9) | 8 (6–9) | 8 (7–8) | 8 (7–9) | 0.177 |
| Depressive symptoms (GDS) b | 2 (1–3) | 2 (1–3) | 2 (1–4) | 2 (1–3) | 0.636 |
| Cardiovascular characteristics | |||||
| Classic risk factors | |||||
| Hypertension c | 325 (58) | 134 (50) | 87 (68) | 104 (64) | 0.003 |
| RR systolic, mmHg | 154 (143–166) | 155 (144–166) | 154 (142–168) | 153 (141–166) | 0.332 |
| Hypercholesterolemia d | 123 (22) | 59 (22) | 30 (24) | 34 (22) | 0.928 |
| Total cholesterol, mmol/L | 5.7 (4.9–6.4) | 5.7 (5.0–6.4) | 5.8 (4.9–6.4) | 5.6 (4.8–6.3) | 0.320 |
| HDL cholesterol, mmol/L | 1.3 (1.0–1.6) | 1.3 (1.1–1.6) | 1.3 (1.0–1.5) | 1.1 (0.9–1.4) | <0.001 |
| BMI, kg/m² | 27 (24–30) | 27 (25–30) | 27 (24–31) | 26 (24–29) | 0.096 |
| Diabetes e | 89 (16) | 38 (14) | 19 (15) | 32 (20) | 0.151 |
| Smoking f | 267 (49) | 122 (46) | 54 (42) | 91 (58) | 0.029 |
| Medication use | |||||
| Blood pressure lowering drugs g | 316 (57) | 111 (42) | 92 (72) | 113 (71) | <0.001 |
| Anticoagulants/aspirin | 162 (28) | 28 (10) | 46 (36) | 88 (51) | <0.001 |
| Lipid-lowering drugs | 6 (1) | 1 (0.4) | 2 (1.6) | 3 (1.7) | 0.15 |
| Cardiovascular history | |||||
| Angina | 109 (19) | 0 | 60 (48) | 49 (29) | |
| Transient ischemic attack | 75 (13) | 0 | 40 (31) | 35 (21) | |
| Intermittent claudication | 37 (7) | 0 | 12 (10) | 25 (15) | |
| Heart failure | 74 (13) | 0 | 36 (28) | 38 (22) | |
| Myocardial infarction | 99 (17) | 0 | 0 | 99 (58) | |
| Stroke | 61 (11) | 0 | 0 | 61 (36) | |
| Surgery for arterial disease h | 42 (7) | 0 | 0 | 42 (25) | |
Data presented as n (%) for categorical variables, and median (IQR) for continuous variables
CVD = cardiovascular disease; No CVD = participants with no history of CVD; Minor CVD = participants with a history of angina, transient ischemic attack, intermittent claudication or heart failure; Major CVD = participants with a history of myocardial infarction, stroke or surgery for arterial disease ; MMSE = Mini-Mental State Examination (range 0-30); ADL = basic activities of daily living (range 9-36); Cantril = Cantril’s ladder of life (range 0–10); GDS = Geriatric Depression Scale (range 0–15)
aChi-square test for categorical variables and Jonckheere-Terpstra for continuous variables;
bassessed only in participants with MMSE >18; c RR ≥160 systolic at baseline or a history of hypertension; d total cholesterol ≥6.5 at baseline or statin use; e history of diabetes, antidiabetic medication use or non-fasting glucose ≥11 mmol/L; f current or past smoker; g use of β-blockers, ACE inhibitors, diuretics or calciumchannel blockers as reported by the participants pharmacists
haorta, carotid, coronary or peripheral arteries
At 90 years of age, 303 (53 %) participants were still alive. Follow-up for mortality was complete, and for 296 participants, we completed all clinical measurements at 90 years.
Morbidity and mortality
During 5 years of follow-up, 181 (32 %) participants reached the composite endpoint, including 76 (42 %) fatal and nonfatal MI, 76 (42 %) fatal and nonfatal strokes, and 29 (16 %) additional cardiovascular deaths. Figure 1 shows the Kaplan–Meier curves for the three groups for the composite endpoint “incident cardiovascular events or cardiovascular mortality” (left panel) and all-cause mortality (right panel). Overall, during these 5 years, 267 (47 %) participants died; of which, 106 (40 %) died from cardiovascular causes. The incidence rate for “incident cardiovascular events or cardiovascular mortality” increased from 56 (95 % CI, 44–72) per 1,000 person-years at risk in the group with no CVD to 88 (95 % CI, 65–118) in the group with minor CVD and to 164 (95 % CI, 144–199) in the group with major CVD (Table 2). The risks for a fatal or nonfatal MI, a fatal or nonfatal stroke, and the composite endpoint increased from 1.7 (95 % CI, 0.9–3.1), 1.7 (95 % CI, 0.9–3.2), and 1.6 (95 % CI, 1.1–2.4), respectively, in participants with minor CVD to 2.6 (95 % CI, 1.6–4.5), 3.4 (95 % CI, 2.0–5.8), and 2.7 (95 % CI, 2.0–3.9), respectively, in those with major CVD. In a direct comparison of the group with major CVD with the group with minor CVD, the risk of the composite endpoint was nearly doubled in the major CVD group (HR, 1.8; 95 % CI, 1.2–2.7).
Fig. 1.
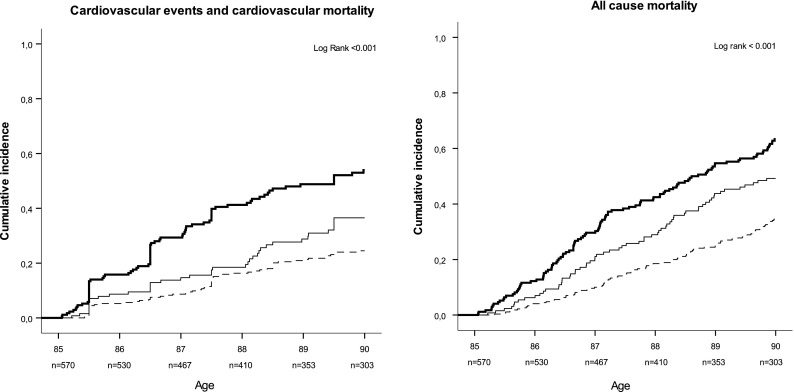
History of CVD and 5-year incidence of the composite endpoint “MI, stroke, and cardiovascular mortality” (left panel), as well as incidence of all-cause mortality (right panel) for three groups with no history of CVD, a history of minor CVD, and a history of major CVD, respectively. Thick solid line major CVD, thin solid line minor CVD, dashed line no CVD
Table 2.
Five-year hazard ratios and absolute risks of cardiovascular morbidity and mortality, depending on cardiovascular history adjusted for sex (n = 570)
| CVD history | p for trend | HR major versus minor | |||||
|---|---|---|---|---|---|---|---|
| None (n = 270) | Minor (n = 128) | Major (n = 172) | |||||
| Morbidity and mortality | Fatal and nonfatal MI | HR | 1 | 1.7 (0.9–3.1) | 2.6 (1.6–4.5) | 0.001 | 1.8 (0.97–3.2) |
| No. of events | 25 (9.3) | 17 (13.3) | 34 (19.8) | ||||
| Incidence rate | 23 (15–33) | 37 (23–58) | 65 (47–90) | ||||
| Fatal and nonfatal stroke | HR | 1 | 1.7 (0.9–3.2) | 3.4 (2.0–5.8) | <0.001 | 2.0 (1.1–3.6) | |
| No. of events | 23 (8.5) | 16 (12.5) | 37 (21.5) | ||||
| Incidence rate | 20 (14–30) | 35 (21–56) | 69 (51–94) | ||||
| CV events or CV mortalitya | HR | 1 | 1.6 (1.1–2.4) | 2.7 (2.0–3.9) | <0.001 | 1.8 (1.2–2.7) | |
| No. of events | 61 (22.6) | 39 (30.5) | 81 (47.1) | ||||
| Incident rate | 56 (44–72) | 88 (65–118) | 164 (144–199) | ||||
| Mortality | Cardiovascular | HR | 1 | 2.0 (1.1–3.4) | 3.7 (2.3–5.8) | <0.001 | 1.9 (1.2–3.1) |
| No. of events | 29 (10.7) | 23 (18.0) | 54 (31.4) | ||||
| Incidence rate | 25 (18–36) | 48 (32–71) | 95 (74–122) | ||||
| Noncardiovascular | HR | 1 | 1.5 (1.03–2.3) | 1.7 (1.2–2.5) | 0.001 | 1.1 (0.7–1.7) | |
| No. of events | 66 (24.4) | 40 (31.3) | 55 (32.0) | ||||
| Incidence rate | 57 (54–72) | 83 (62–111) | 97 (75–124) | ||||
| All-cause | HR | 1 | 1.7 (1.2–2.3) | 2.3 (1.7–3.1) | <0.001 | 1.4 (1.02–1.9) | |
| No. of events | 95 (35.2) | 63 (49.2) | 109 (63.4) | ||||
| Incidence rate | 82 (68–100) | 131 (104–164) | 193 (162–227) | ||||
Data are presented as HR with corresponding 95 % CIs, absolute numbers of events (%), and incidence rates as number of incidents per 1,000 person-years at risk with corresponding 95 % CIs
CVD cardiovascular disease, No CVD participants with no history of CVD, Minor CVD participants with a history of angina, TIA, intermittent claudication, or heart failure, Major CVD participants with a history of MI, stroke, or surgery for arterial disease (aorta, carotid, coronary, or peripheral arteries)
aComposite endpoint: fatal and nonfatal MI, fatal and nonfatal stroke, and cardiovascular mortality
For cardiovascular mortality, the risks increased from 2.0 (95 % CI, 1.1–3.4) in the minor CVD group to 3.7 (95 % CI, 2.3–5.8) in the major CVD group (p trend < 0.001). For all-cause mortality, the risks rose from 1.7 (95 % CI, 1.2–2.3) in the minor group to 2.3 (95 % CI, 1.7–3.1) in the major group (p trend < 0.001). After adjustment for the use of antihypertensive medication, income, and level of education, all these estimates remained roughly similar (data not shown).
When we analyzed the HRs with 10-year follow-up, we found similar risks for cardiovascular and all-cause mortality: HR, 1.5 (95 % CI, 0.99–2.2) and 1.4 (95 % CI, 1.1–1.8), respectively, for minor CVD and HR, 2.6 (95 % CI, 1.9–3.7) and 2.0 (95 % CI, 1.6–2.5), respectively, for major CVD.
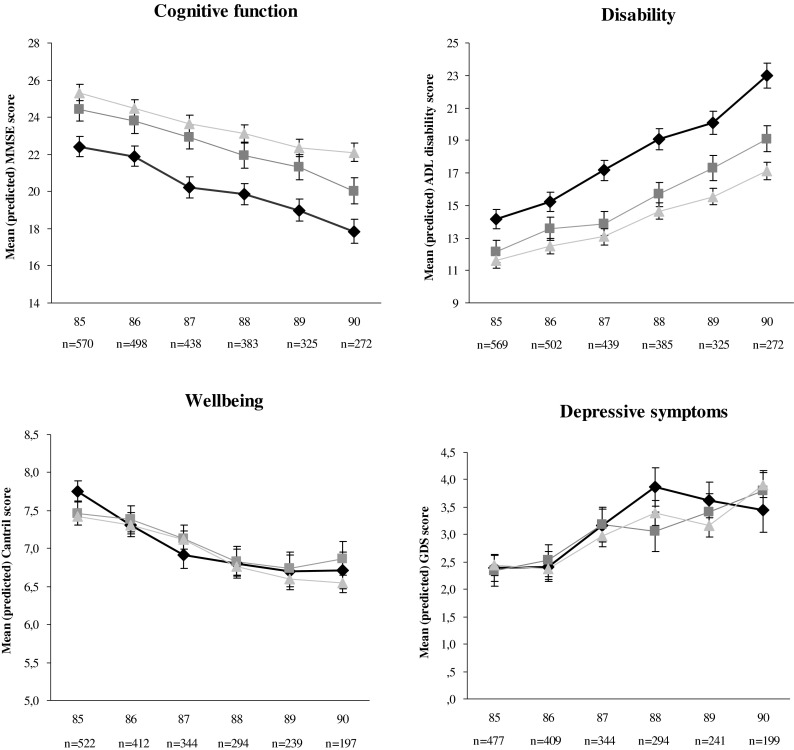
Functional status
At baseline, there were no differences in functional status between participants with minor CVD and those with no CVD (Table 3; Fig. 2). But the MMSE score was lower (−2.8 points, p < 0.001) and ADL disability score was higher (2.6 points, p = 0.003) in participants with major CVD. Compared to participants with no CVD, participants with minor CVD had an additional annual decrease in MMSE score of −0.19 points (p = 0.023) and increase in ADL disability score of 0.25 points (p = 0.042) over time. Participants with major CVD had an additional annual decrease in MMSE score (−0.24 points, p = 0.005) and increase in ADL disability score (0.61 points, p < 0.001). Compared to participants with minor CVD, participants with major CVD had an additional annual increase in ADL disability score of 0.36 points (p = 0.023). All other changes in functional status over time were not significant.
Table 3.
Association between history of cardiovascular disease at 85 years of age and (changes in) functional status from 85 through 90 years of age (n = 570)
| Cross-sectional effecta | Annual effect reference group | Additional annual effecta | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Minor CVD | Major CVD | Minor CVD | Major CVD | |||||||
| B (SE) | p value | B (SE) | p value | B (SE) | p value | B (SE) | p value | B (SE) | p value | |
| MMSE | −0.65 (0.69) | 0.35 | −2.8 (0.69) | <0.001 | −0.67 (0.045) | <0.001 | −0.19 (0.084) | 0.023 | −0.24 (0.085) | 0.005 |
| ADL disability | 0.58 (0.71) | 0.41 | 2.6 (0.72) | 0.003 | 1.1 (0.066) | <0.001 | 0.25 (0.12) | 0.042 | 0.61 (0.13) | <0.001 |
| Cantril scale of well-being | −0.021 (0.17) | 0.90 | 0.24 (0.17) | 0.15 | −0.20 (0.021) | <0.001 | 0.039 (0.041) | 0.35 | −0.045 (0.043) | 0.29 |
| Geriatric depression scale | 0.060 (0.31) | 0.85 | 0.033 (0.31) | 0.92 | 0.30 (0.035) | <0.001 | −0.023 (0.069) | 0.74 | 0.030 (0.070) | 0.66 |
Associations were assessed by linear mixed models adjusted for sex. Scale: MMSE, 0–30 points; ADL disability, 9–36 points; Cantril, 0–10 points; GDS of depressive symptoms, 0–15 points
CVD cardiovascular disease
aReference group: group with no CVD at baseline
Fig. 2.
Changes in cognitive function, disability, subjective well-being, and depressive symptoms over time as estimated from linear mixed models adjusted for sex. Data are presented as the means with standard errors. Triangles reference group with no history of CVD, squares minor CVD, diamonds major CVD
Sensitivity analyses
At 90 years of age, participants were recategorized with the updated clinical information from 85 to 90 years of age. Of the participants with complete data at 90 years of age (n = 296), 119 (40 %) had no history of CVD, 93 (31 %) had minor CVD, and 84 (28 %) had major CVD. In participants with minor CVD, the 5-year risk for cardiovascular mortality (up to 95 years of age) was not significantly increased (1.1; 95 % CI, 0.6–1.9), but participants with major CVD had a more than twofold increased risk (HR, 2.1; 95 % CI, 1.2–3.7). For all-cause mortality, the HRs were 1.1 (95 % CI, 0.79–1.5) and 2.1 (95 % CI, 1.5–3.0), respectively.
The second sensitivity analysis was done with different groups according to the site of their CVD. There were 25 participants (4.4 %) with peripheral CVD, 73 (12.8 %) with cerebrovascular CVD, 109 (19.1 %) with cardiac CVD, and 66 (11.6 %) with CVD on more than one site (Table 4). HRs were all calculated with the group with no CVD as reference group. The HR for fatal or nonfatal stroke was as high as 3.9 (95 % CI, 2.2–6.9) for those with previous TIA or stroke, and the HR for fatal or nonfatal MI was particularly high (3.4; 95 % CI, 1.9–6.4) in the group with CVD on multiple sites. The HR for cardiovascular mortality was highest in participants with peripheral CVD (3.8; 95 % CI, 1.7–8.5). In contrast with this high risk of cardiovascular mortality, the HRs for fatal or nonfatal MI and fatal or nonfatal stroke in participants with peripheral CVD were low, nearly equal to the group with no CVD (1.0; 95 % CI, 0.23–4.3 and 1.4; 95 % CI, 0.32–5.8, respectively). Except for the above-mentioned HRs, the groups did not differ materially.
Table 4.
Five-year hazard ratios for cardiovascular morbidity and mortality for participants, depending on specific site of cardiovascular history adjusted for sex (n = 570)
| CVD history | ||||||
|---|---|---|---|---|---|---|
| None (n = 297) | Cardiac (n = 109) | Cerebrovascular (n = 73) | Peripheral (n = 25) | Multiple sites (n = 66) | ||
| Morbidity | Fatal and nonfatal MI | 1 | 2.0 (1.1–3.7) | 1.9 (0.96–3.9) | 1.0 (0.23–4.3) | 3.4 (1.9–6.4) |
| Fatal and nonfatal stroke | 1 | 2.3 (1.3–4.2) | 3.9 (2.2–6.9) | 1.4 (0.32–5.8) | 1.6 (0.68–3.7) | |
| CV events or CV mortalitya | 1 | 2.0 (1.4–3.0) | 2.3 (1.5–3.5) | 1.9 (0.93–3.8) | 2.5 (1.6–3.9) | |
| Mortality | Cardiovascular | 1 | 2.8 (1.7–4.6) | 3.0 (1.7–5.3) | 3.8 (1.7–8.5) | 3.1 (1.7–5.5) |
| Noncardiovascular | 1 | 1.4 (0.90–2.1) | 1.5 (0.95–2.4) | 1.6 (0.76–3.3) | 1.6 (1.0–2.6) | |
| All-cause | 1 | 1.8 (1.3–2.5) | 2.0 (1.4–2.8) | 2.2 (1.3–3.8) | 2.0 (1.4–3.0) | |
Data are presented as HR with corresponding 95 % CIs
CVD cardiovascular disease, Cardiac angina or MI, Cerebrovascular TIA or stroke, Peripheral claudication or operation for noncoronary arterial disease, Multiple sites CVD on more than one of cardiac, cerebrovascular, or peripheral sites
aComposite endpoint: fatal and nonfatal MI, fatal and nonfatal stroke, and cardiovascular mortality
Discussion
In this cohort of oldest old from the general population, participants with a history of major CVD had a markedly increased risk of recurrent MI, stroke, and functional decline, as well as cardiovascular and all-cause mortality. Patients with a history of minor CVD had a relatively better prognosis: in nonagenarians, a history of minor CVD was not associated with mortality anymore. This implies that, within the group of very old patients who are eligible for secondary prevention, different risk groups can now be identified on the basis of clinical information only. Since the prevention of morbidity and subsequent loss of independency is increasingly important in the aging Western societies, cardiovascular prevention remains essential up to the highest age groups. Our findings underscore the importance of adequate secondary preventive measures in those with a history of major cardiovascular events, since these measures have been shown to be effective up to high ages (Andrawes et al. 2005; Alhusban and Fagan 2011; Castilla-Guerra et al. 2009; Asberg et al. 2010; Ray et al. 2006; Deedwania et al. 2007; Shepherd et al. 2002; Wenger and Lewis 2010; Thomas et al. 2010). On the other hand, our results suggest that the potential yield of secondary preventive measures in the oldest old might be less in older persons with a history of minor CVD.
Our study is the first to analyze prognosis based on a history of “minor” and “major” CVD in the general population of the oldest old. This distinction between minor and major CVD is based on the difference in risk of cardiovascular events and mortality after angina or TIA compared with the risk after an MI or stroke, which has been described in younger patients (Arima et al. 2006; Rosengren et al. 1998; Hjemdahl et al. 2006). Our study now also showed a significant difference in cardiovascular morbidity and mortality between groups with a history of minor and major CVD in participants aged 85 years and over.
Most other studies, performed in younger age groups, have evaluated risks after an event in a specific cardiovascular bed (cardiac, cerebral, or peripheral) (Migliaccio-Walle et al. 2010; Bhatt et al. 2009; Arima et al. 2006; Touze et al. 2005) or observed differences in risk between one or multiple CVD sites (Ferrieres et al. 2006; Migliaccio-Walle et al. 2010; Bhatt et al. 2009; Steg et al. 2007). The high risk of recurrent stroke in the group with a history of TIA or stroke that we observed is in line with previous studies (Steg et al. 2007; Arima et al. 2006; Ferrieres et al. 2006; Vickrey et al. 2002).
In keeping with earlier reports, in the present study, the risk of cardiovascular mortality was remarkably high in participants with peripheral artery disease, whereas cardiovascular morbidity risk in this group was relatively low (Ferrieres et al. 2006; Steg et al. 2007; Arima et al. 2006; Vickrey et al. 2002). In contrast with younger age groups, mortality risks in our study were not higher in participants with multiple-site CVD (Steg et al. 2007; Bhatt et al. 2009; Migliaccio-Walle et al. 2010; Ferrieres et al. 2006). In very old age, it seems that major CVD, rather than multiple CVD, is of prognostic value.
Previous studies have revealed a significant decline in physical functioning after stroke and MI in 70-year-olds (van Jaarsveld et al. 2001; Newman et al. 2009) and a negative impact on neurocognitive function (Waldstein and Wendell 2010; Newman et al. 2005, 2009). Our study confirmed these data in the very old.
Our study has several strengths. First, our results can be easily applied in day to day medical practice. The current electronic medical records provide clinicians a rapid overview of the cardiovascular history without any extra costs or effort. Secondly, our population-based study had a high participation rate (87 %) and no exclusion criteria, both allowing our conclusions to be generalized to the oldest old in the general population. Finally, we studied multiple relevant outcomes for an ageing population: mortality, morbidity, and functional status. A limitation might be that CVD history was based on the diagnosis of the primary care physicians, using variable diagnostic standards. However, this reflects clinical reality in primary care and previous research has shown the accuracy of data recorded in general practice to be very high (Hassey et al. 2001). In view of the fact that this study was the first to discriminate major and minor CVD in very old age, we recommend that this analysis be repeated in another cohort.
Evidence that medication for secondary cardiovascular prevention is recommendable up to the highest age groups is increasing (Andrawes et al. 2005; Alhusban and Fagan 2011; Castilla-Guerra et al. 2009; Asberg et al. 2010; Maroo et al. 2008; Ray et al. 2006; Deedwania et al. 2007; Shepherd et al. 2002; Wenger and Lewis 2010; Thomas et al. 2010). In this cohort, the use of secondary preventive medication was far from optimal, leaving room for improvement. From our results, it can be derived that distinct groups are discernible within those who should receive secondary prevention. This is an important finding, since at very old age, polypharmacy (Banerjee et al. 2011; Fleg et al. 2011), treatment adherence (Kvan et al. 2006), and the delicate balance between benefit and harm (Cardenas-Valladolid et al. 2010; Kvan et al. 2006; Fleg et al. 2011) raise a challenge for clinicians in day to day practice (Anthierens et al. 2010; Fried et al. 2011). The results of our study may help them to make appropriate treatment decisions, taking all relevant prognostic information into account.
In conclusion, in very old age, the CVD history is an easy tool for clinicians to identify patients who are at high risk for new cardiovascular events, functional decline, and cardiovascular mortality, as well as all-cause mortality. A history of major CVD nearly doubles the risk of a recurrent cardiovascular event or cardiovascular mortality compared with a history of minor CVD. Our results encourage both physicians and 85-year-olds with a history of major CVD to maximize their cardiovascular preventive efforts. However, when adverse effects or harmful interactions arise in a very old patient with minor CVD, the balance between benefit and harm could change and strict continuation of preventive medication might be reconsidered.
Acknowledgments
The Leiden 85-plus Study was partly funded by an unrestricted grant from the Dutch Ministry of Health, Welfare and Sports.
Open Access
This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Abbreviations
- ADL
Activities of Daily Living
- BNP
Brain natriuretic peptide
- CABG
Coronary artery bypass grafting
- CAD
Coronary artery disease
- CI
Confidence interval
- CV
Cardiovascular
- CVD
Cardiovascular disease
- GDS
Geriatric Depression Scale
- HR
Hazard ratio
- ICD
International Classification of Diseases
- MI
Myocardial infarction
- MMSE
Mini-Mental State Examination
- PAD
Peripheral artery disease
- PTCA
Percutaneous transluminal coronary angioplasty
- SE
Standard error
- TIA
Transient ischemic attack
References
- Alhusban A, Fagan SC. Secondary prevention of stroke in the elderly: a review of the evidence. Am J Geriatr Pharmacother. 2011;9:143–152. doi: 10.1016/j.amjopharm.2011.04.002. [DOI] [PubMed] [Google Scholar]
- Andrawes WF, Bussy C, Belmin J. Prevention of cardiovascular events in elderly people. Drugs Aging. 2005;22:859–876. doi: 10.2165/00002512-200522100-00005. [DOI] [PubMed] [Google Scholar]
- Anthierens, S., Tansens, A., Petrovic, M., & Christiaens, T (2010) Qualitative insights into general practitioners views on polypharmacy. BMC.Fam.Pract., 11, 65 [DOI] [PMC free article] [PubMed]
- Arima H, Tzourio C, Butcher K, Anderson C, Bousser MG, Lees KR, Reid JL, Omae T, Woodward M, MacMahon S, Chalmers J. Prior events predict cerebrovascular and coronary outcomes in the PROGRESS trial. Stroke. 2006;37:1497–1502. doi: 10.1161/01.STR.0000221212.36860.c9. [DOI] [PubMed] [Google Scholar]
- Arnold SV, Spertus JA, Tang F, Krumholz HM, Borden WB, Farmer SA, Ting HH, Chan PS. Statin use in outpatients with obstructive coronary artery disease. Circulation. 2011;124:2405–2410. doi: 10.1161/CIRCULATIONAHA.111.038265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asberg S, Henriksson KM, Farahmand B, Asplund K, Norrving B, Appelros P, Stegmayr B, Asberg KH, Terent A. Ischemic stroke and secondary prevention in clinical practice: a cohort study of 14,529 patients in the Swedish Stroke Register. Stroke. 2010;41:1338–1342. doi: 10.1161/STROKEAHA.110.580209. [DOI] [PubMed] [Google Scholar]
- Banerjee A, Mbamalu D, Ebrahimi S, Khan AA, Chan TF. The prevalence of polypharmacy in elderly attenders to an emergency department—a problem with a need for an effective solution. Int J Emerg Med. 2011;4:22. doi: 10.1186/1865-1380-4-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhatt DL, Steg PG, Ohman EM, Hirsch AT, Ikeda Y, Mas JL, Goto S, Liau CS, Richard AJ, Rother J, Wilson PW. International prevalence, recognition, and treatment of cardiovascular risk factors in outpatients with atherothrombosis. JAMA: J Am Med Assoc. 2006;295:180–189. doi: 10.1001/jama.295.2.180. [DOI] [PubMed] [Google Scholar]
- Bhatt DL, Peterson ED, Harrington RA, Ou FS, Cannon CP, Gibson CM, Kleiman NS, Brindis RG, Peacock WF, Brener SJ, Menon V, Smith SC, Jr, Pollack CV, Jr, Gibler WB, Ohman EM, Roe MT. Prior polyvascular disease: risk factor for adverse ischaemic outcomes in acute coronary syndromes. Eur Heart J. 2009;30:1195–1202. doi: 10.1093/eurheartj/ehp099. [DOI] [PubMed] [Google Scholar]
- Bhatt DL, Eagle KA, Ohman EM, Hirsch AT, Goto S, Mahoney EM, Wilson PWF, Alberts MJ, D'Agostino R, Liau CS, Mas JL, Röther J, Smith SC, Salette GV, Contant CF, Massaro JM, Steg P. Comparative determinants of 4-year cardiovascular event rates in stable outpatients at risk of or with atherothrombosis. JAMA: J Am Med Assoc. 2010;304:1350–1357. doi: 10.1001/jama.2010.1322. [DOI] [PubMed] [Google Scholar]
- Cantril H. The pattern of human concerns. New Brunswick: Rutgers University Press; 1965. [Google Scholar]
- Cardenas-Valladolid J, Martin-Madrazo C, Salinero-Fort MA, Carrillo de-Santa PE, Abanades-Herranz JC, de Burgos-Lunar C. Prevalence of adherence to treatment in homebound elderly people in primary health care: a descriptive, cross-sectional, multicentre study. Drugs Aging. 2010;27:641–651. doi: 10.2165/11537320-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Castilla-Guerra L, Fernandez-Moreno MC, Alvarez-Suero J. Secondary stroke prevention in the elderly: new evidence in hypertension and hyperlipidemia. Eur J Intern Med. 2009;20:586–590. doi: 10.1016/j.ejim.2009.06.005. [DOI] [PubMed] [Google Scholar]
- de Craen AJ, Heeren TJ, Gussekloo J. Accuracy of the 15-item geriatric depression scale (GDS-15) in a community sample of the oldest old. Int J Geriatr Psychiatry. 2003;18:63–66. doi: 10.1002/gps.773. [DOI] [PubMed] [Google Scholar]
- Deedwania P, Stone PH, Bairey Merz CN, Cosin-Aguilar J, Koylan N, Luo D, Ouyang P, Piotrowicz R, Schenck-Gustafsson K, Sellier P, Stein JH, Thompson PL, Tzivoni D. Effects of intensive versus moderate lipid-lowering therapy on myocardial ischemia in older patients with coronary heart disease: results of the Study Assessing Goals in the Elderly (SAGE) Circulation. 2007;115:700–707. doi: 10.1161/CIRCULATIONAHA.106.654756. [DOI] [PubMed] [Google Scholar]
- der Wiel AB, van Exel E, de Craen AJ, Gussekloo J, Lagaay AM, Knook DL, Westendorp RG. A high response is not essential to prevent selection bias: results from the Leiden 85-plus study. J Clin Epidemiol. 2002;55:1119–1125. doi: 10.1016/S0895-4356(02)00505-X. [DOI] [PubMed] [Google Scholar]
- Dornbrook-Lavender KA, Pieper JA, Roth MT. Primary prevention of coronary heart disease in the elderly. Ann Pharmacother. 2003;37:1654–1663. doi: 10.1345/aph.1D025. [DOI] [PubMed] [Google Scholar]
- Ferrieres J, Cambou JP, Gayet JL, Herrmann MA, Leizorovicz A. Prognosis of patients with atherothrombotic disease: a prospective survey in a non-hospital setting. Int J Cardiol. 2006;112:302–307. doi: 10.1016/j.ijcard.2005.09.024. [DOI] [PubMed] [Google Scholar]
- Fleg JL, Aronow WS, Frishman WH. Cardiovascular drug therapy in the elderly: benefits and challenges. Nat Rev Cardiol. 2011;8:13–28. doi: 10.1038/nrcardio.2010.162. [DOI] [PubMed] [Google Scholar]
- Fried TR, Tinetti ME, Towle V, O'Leary JR, Iannone L. Effects of benefits and harms on older persons' willingness to take medication for primary cardiovascular prevention. Arch Intern Med. 2011;171:923–928. doi: 10.1001/archinternmed.2011.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham, I., Atar, D., Borch-Johnsen, K. et al. (2007). European guidelines on cardiovascular disease prevention in clinical practice: full text. Fourth Joint Task Force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts). Eur.J.Cardiovasc.Prev.Rehabil., 14 Suppl 2, S1-113. [DOI] [PubMed]
- Hassey A, Gerrett D, Wilson A. A survey of validity and utility of electronic patient records in a general practice. BMJ. 2001;322:1401–1405. doi: 10.1136/bmj.322.7299.1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hjemdahl P, Eriksson SV, Held C, Forslund L, Nasman P, Rehnqvist N. Favourable long term prognosis in stable angina pectoris: an extended follow up of the angina prognosis study in Stockholm (APSIS) Heart. 2006;92:177–182. doi: 10.1136/hrt.2004.057703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kempen GI, Miedema I, Ormel J, Molenaar W. The assessment of disability with the Groningen Activity Restriction Scale. Conceptual framework and psychometric properties. Soc Sci Med. 1996;43:1601–1610. doi: 10.1016/S0277-9536(96)00057-3. [DOI] [PubMed] [Google Scholar]
- Kerr AJ, Broad J, Wells S, Riddell T, Jackson R. Should the first priority in cardiovascular risk management be those with prior cardiovascular disease? Heart. 2009;95:125–129. doi: 10.1136/hrt.2007.140905. [DOI] [PubMed] [Google Scholar]
- Kvan E, Pettersen KI, Landmark K, Reikvam A. Treatment with statins after acute myocardial infarction in patients > or = 80 years: underuse despite general acceptance of drug therapy for secondary prevention. Pharmacoepidemiol Drug Saf. 2006;15:261–267. doi: 10.1002/pds.1172. [DOI] [PubMed] [Google Scholar]
- Macfarlane PW, Latif S. Automated serial ECG comparison based on the Minnesota code. J Electrocardiol. 1996;29(Suppl):29–34. doi: 10.1016/S0022-0736(96)80016-1. [DOI] [PubMed] [Google Scholar]
- Maroo BP, Lavie CJ, Milani RV. Secondary prevention of coronary heart disease in elderly patients following myocardial infarction: are all HMG-CoA reductase inhibitors alike? Drugs Aging. 2008;25:649–664. doi: 10.2165/00002512-200825080-00003. [DOI] [PubMed] [Google Scholar]
- McDermott MM. The international pandemic of chronic cardiovascular disease. JAMA: J Am Med Assoc. 2007;297:1253–1255. doi: 10.1001/jama.297.11.1253. [DOI] [PubMed] [Google Scholar]
- Migliaccio-Walle, K., Stokes, M., Proskorovsky, I., Popovici-Toma, D., & El-Hadi, W. (2010). Evaluation of the consequences associated with diffuse vascular disease history in patients diagnosed with peripheral arterial disease: estimates from Saskatchewan health data. BMC.Cardiovasc.Disord., 10, 40. [DOI] [PMC free article] [PubMed]
- Newman AB, Fitzpatrick AL, Lopez O, Jackson S, Lyketsos C, Jagust W, Ives D, Dekosky ST, Kuller LH. Dementia and Alzheimer's disease incidence in relationship to cardiovascular disease in the Cardiovascular Health Study cohort. J Am Geriatr Soc. 2005;53:1101–1107. doi: 10.1111/j.1532-5415.2005.53360.x. [DOI] [PubMed] [Google Scholar]
- Newman AB, Arnold AM, Sachs MC, Ives DG, Cushman M, Strotmeyer ES, Ding J, Kritchevsky SB, Chaves PH, Fried LP, Robbins J. Long-term function in an older cohort—the cardiovascular health study all stars study. J Am Geriatr Soc. 2009;57:432–440. doi: 10.1111/j.1532-5415.2008.02152.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray KK, Bach RG, Cannon CP, Cairns R, Kirtane AJ, Wiviott SD, McCabe CH, Braunwald E, Gibson CM. Benefits of achieving the NCEP optional LDL-C goal among elderly patients with ACS. Eur Heart J. 2006;27:2310–2316. doi: 10.1093/eurheartj/ehl180. [DOI] [PubMed] [Google Scholar]
- Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation. 2011;123:e18–e209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosengren A, Wilhelmsen L, Hagman M, Wedel H. Natural history of myocardial infarction and angina pectoris in a general population sample of middle-aged men: a 16-year follow-up of the Primary Prevention Study, Goteborg. Sweden J Intern Med. 1998;244:495–505. doi: 10.1111/j.1365-2796.1998.00394.x. [DOI] [PubMed] [Google Scholar]
- Shepherd J, Blauw GJ, Murphy MB, Bollen EL, Buckley BM, Cobbe SM, Ford I, Gaw A, Hyland M, Jukema JW, Kamper AM, Macfarlane PW, Meinders AE, Norrie J, Packard CJ, Perry IJ, Stott DJ, Sweeney BJ, Twomey C, Westendorp RG. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet. 2002;360:1623–1630. doi: 10.1016/S0140-6736(02)11600-X. [DOI] [PubMed] [Google Scholar]
- Steg PG, Bhatt DL, Wilson PW, D'Agostino R, Sr, Ohman EM, Rother J, Liau CS, Hirsch AT, Mas JL, Ikeda Y, Pencina MJ, Goto S. One-year cardiovascular event rates in outpatients with atherothrombosis. JAMA: J Am Med Assoc. 2007;297:1197–1206. doi: 10.1001/jama.297.11.1197. [DOI] [PubMed] [Google Scholar]
- Thomas JE, Tershakovec AM, Jones-Burton C, Sayeed RA, Foody JM. Lipid lowering for secondary prevention of cardiovascular disease in older adults. Drugs Aging. 2010;27:959–972. doi: 10.2165/11539550-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Tombaugh TN, McIntyre NJ. The mini-mental state examination: a comprehensive review. J Am Geriatr Soc. 1992;40:922–935. doi: 10.1111/j.1532-5415.1992.tb01992.x. [DOI] [PubMed] [Google Scholar]
- Touze E, Varenne O, Chatellier G, Peyrard S, Rothwell PM, Mas JL. Risk of myocardial infarction and vascular death after transient ischemic attack and ischemic stroke: a systematic review and meta-analysis. Stroke. 2005;36:2748–2755. doi: 10.1161/01.STR.0000190118.02275.33. [DOI] [PubMed] [Google Scholar]
- Vaartjes, I., van Dis, I, Grobbee, D. E., & Bots, M. L. (2010). The dynamics of mortality in follow-up time after an acute myocardial infarction, lower extremity arterial disease and ischemic stroke. BMC.Cardiovasc.Disord., 10, 57 [DOI] [PMC free article] [PubMed]
- van Exel E, Gussekloo J, Houx P, de Craen AJ, Macfarlane PW, Bootsma-van der Wiel A, Blauw GJ, Westendorp RG. Atherosclerosis and cognitive impairment are linked in the elderly. The Leiden 85-plus Study. Atherosclerosis. 2002;165:353–359. doi: 10.1016/S0021-9150(02)00253-8. [DOI] [PubMed] [Google Scholar]
- van Jaarsveld CH, Sanderman R, Miedema I, Ranchor AV, Kempen GI. Changes in health-related quality of life in older patients with acute myocardial infarction or congestive heart failure: a prospective study. J Am Geriatr Soc. 2001;49:1052–1058. doi: 10.1046/j.1532-5415.2001.49208.x. [DOI] [PubMed] [Google Scholar]
- van Wijk I, Kappelle LJ, van Gijn J, Koudstaal PJ, Franke CL, Vermeulen M, Gorter JW, Algra A. Long-term survival and vascular event risk after transient ischaemic attack or minor ischaemic stroke: a cohort study. Lancet. 2005;365:2098–2104. doi: 10.1016/S0140-6736(05)66734-7. [DOI] [PubMed] [Google Scholar]
- Vickrey BG, Rector TS, Wickstrom SL, Guzy PM, Sloss EM, Gorelick PB, Garber S, McCaffrey DF, Dake MD, Levin RA. Occurrence of secondary ischemic events among persons with atherosclerotic vascular disease. Stroke. 2002;33:901–906. doi: 10.1161/hs0402.105246. [DOI] [PubMed] [Google Scholar]
- Wald NJ, Simmonds M, Morris JK. Screening for future cardiovascular disease using age alone compared with multiple risk factors and age. PLoS One. 2011;6:e18742. doi: 10.1371/journal.pone.0018742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldstein SR, Wendell CR. Neurocognitive function and cardiovascular disease. J Alzheimers Dis. 2010;20:833–842. doi: 10.3233/JAD-2010-091591. [DOI] [PubMed] [Google Scholar]
- Wenger, N. K. & Lewis, S. J (2010) Use of statin therapy to reduce cardiovascular risk in older patients. Curr.Gerontol.Geriatr.Res., 915296 [DOI] [PMC free article] [PubMed]
- Wilson PW. Prediction of cardiovascular disease events. Cardiol Clin. 2011;29:1–13. doi: 10.1016/j.ccl.2010.10.004. [DOI] [PubMed] [Google Scholar]
- Wilson PW, d'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847. doi: 10.1161/01.CIR.97.18.1837. [DOI] [PubMed] [Google Scholar]