Abstract
INTRODUCTION
This paper describes, for the first time, the outcomes of patients undergoing total hip replacement for acute fractured neck of femur (#NOF) as recorded by the National Joint Registry of England and Wales (NJR).
METHODS
In the NJR we identified 1,302 of 157,232 Hospital Episode Statistics linked patients who had been recorded as having a total hip replacement for acute #NOF between April 2003 and November 2008.
RESULTS
The revision rate at five years for fully uncemented components was 4.1% (95% confidence interval [Cl]: 2.2-7.3%), for hybrid it was 2.2% (95% Cl: 0.9%-5.3%) and for fully cemented components 0.9% (95% Cl: 0.4-2.0%). Five-year revision rates were increased for those whose operations were performed via a posterior versus a lateral approach. The Kaplan-Meier estimate of 30-day mortality was 1.4% (95% Cl: 1.0-2.4%), which is over double the 30-day mortality rate for total hip replacement identified by the Office for National Statistics. The mean length of stay was also increased for those undergoing total hip replacements for #NOF compared with non-emergency indications.
CONCLUSIONS
Our data suggest that total hip replacements for acute #NOF give comparable results with total hip replacements for other indications.
Keywords: Hip, Fracture, Total hip replacement, Arthroplasty, Registry
Displaced subcapital and intracapsular femoral neck fractures unsuitable for reduction and primary fixation are usually treated with an arthroplasty procedure.1 This may be cemented or uncemented hip hemiarthroplasty or total hip replacement. The rationale is that in the majority of patients who have suffered a subcapital fractured neck of femur (#NOF), the functional results of hemiarthroplasty are acceptable as a significant proportion of these patients are medically unfit and/or have a sedentary lifestyle.
The experience of the available surgeon may also not always be felt to be acceptable for total hip replacement whereas this is less of an issue for the less technically demanding hemiarthroplasty. This may be due in part to the increased inherent stability of the larger head of the hemiarthroplasty and the reduced need for a clear circumferential exposure of the acetabulum. Hemiarthroplasty also avoids lengthy operations and the perceived dangers of pressurised bone cement (depending on the type of implant and technique used).
There are reports of mixed outcomes when using total hip replacement for #NOF citing increased incidence of dislocation and further procedures compared with those undergoing the total hip replacement for osteoarthritis alone.2,3 The results of hip hemiarthroplasty have, however, been shown to be not as good as total hip replacement in competent, medically fitter (ASA [American Society of Anesthesiologists] grades 1-2), ‘high demand', active patients.4 Consequently, there is evidence for increasing use of total hip replacement (cemented or uncemented) for certain patients with displaced subcapital #NOF. A recent meta-analy-sis concluded that total hip replacement may lead to lower reoperation rates and better functional outcomes compared with hemiarthroplasty and this is supported by the recent update to guidance in Scotland.5,6
In 2009 the National Patient Safety Agency (NPSA) published a report commenting on the risks of using bone cement, citing 26 cement related deaths between 2003 and 2008.7 As a result, there has been a question as to whether British orthopaedic surgeons should use uncemented prostheses or modify the cement introduction techniques to minimise possible embolic phenomena and reactions. Those patients who have suffered a fragility fracture such as #NOF are perceived to be most at risk from these phenomena, usually to a general deterioration in health and physiological reserves.8
This paper describes, for the first time, the outcomes of patients undergoing a total hip replacement for acute #NOF as recorded by the National Joint Registry of England and Wales (NJR).
Methods
We identified 157,232 primary total hip replacements registered with the NJR between April 2003 and November 2008 and linked to a Hospital Episode Statistics (HES) episode. (See the NJR 2009 annual report for detailed methods.)9
Identification of patients with fractured neck of femur
The NJR database collects information regarding indication for surgery. We selected the subgroup of interest in the following way: for those patients entered in databases MDS1 (Minimum Dataset) and MDS2 we chose entries where the field ‘fractured neck of femur’ was selected and for the entries in MDS3 we chose those where the field ‘trauma-acute (neck of femur)’ was selected. Using information in HES, we then restricted the analysis group to those patients whose primary procedure was carried out in an emergency admission and for whom the ICD-10 (International Classification of Diseases) codes in the primary diagnosis field was ‘S72’ (ie fracture of femur). This was done to create the most homogenous group possible in terms of indication for surgery. Confirmation of the accuracy of the cohort was achieved by identifying the implant as being a total hip replacement.
Identification of revisions and revision rates
In patients with linked NJR-HES records of primary hip replacements, we identified revisions through longitudinal linkage in HES based on the unique patient identifier assigned to episodes of care in NHS hospitals and through longitudinal linkage in the NJR based on NHS number or patient surname, date of birth and postcode.
Co-morbidity
Using the HES episode history up to one year prior to the hip replacement, the presence of any co-morbid conditions of this subgroup was assessed using the method described by Armitage etal.10 The number of co-morbid conditions is presented using the Royal College of Surgeons Charlson score, defined as a score of 0, 1, 2, 3 or more.
Length of stay and 30-day mortality
We calculated the length of stay based on the discharge date in HES. Using the dates of death provided by the Office for National Statistics (ONS), we identified those who died within 30 days of the primary procedure.
Statistical analysis
Revision and mortality rates were estimated using Kaplan-Meier methods and compared using the logrank test. Mul-tivariate Cox regression was used to compare implant and patient survival while adjusting for confounding factors. The results of the Cox regression are reported as hazard ratios (HR) with 95% confidence intervals (CI). In the multivari-ate models, significance was assessed using the likelihood ratio test. Linear regression was used to compare length of stay for different patient and prosthesis characteristics. Results are expressed as mean differences with 95% CIs. Significance was assessed using the Wald test or the F-test as appropriate. Age, sex, physical status and prosthesis type were included in all three multivariate models. Incision approach was also included in the model for revision rates. A p-value of <0.05 was considered statistically significant and Stata® v10 (StataCorp, College Station, TX, US) was used for all analyses.
Results
Patients and procedures
A total of 2,105 patients (1.3%) of the 157,232 primary HES-linked total hip replacements in the NJR had #NOF as the indication for surgery. However, 620 of these were coded as elective procedures and therefore we suspect they were more likely to be procedures for the complications of #NOF rather than primary surgery. A further 183 did not have the appropriate ICD-10 code in the primary diagnosis field in HES. This left 1,302 patients in the analysis group. The mean age was 71 years (range: 29-96 years) and there were 966 women (76%). A total of 710 patients (54%) had a cemented prosthesis, 350 (27%) an uncemented and 242 (19%) a hybrid total hip replacement.
The type of prosthesis implanted varied by age in this selected group; older patients were more likely to receive a cemented prosthesis than younger patients. In the youngest age group (<65 years) 36% received a cemented prosthesis whereas 60% and 62% of those in the older groups received a cemented prosthesis. Uncemented prostheses (including hybrids) were implanted in 43% of the under 65s and in 21% of older patients.
The type of prosthesis implanted did not vary by physical status: between 54% and 59% of the patients in each of the three ASA grade groups (P1, P2, P3+) received a cemented prosthesis. There was some variation in the proportions of procedures in which a posterior approach was used. A higher proportion of hybrid (39%) and uncemented (36%) prosthesis were implanted using a posterior approach than for cemented prosthesis (27%).
We looked at the seniority of the surgeon listed as having undertaken the index procedure. Over two-thirds of the operations were recorded as having a consultant as the primary surgeon (Fig 1).
Figure 1.
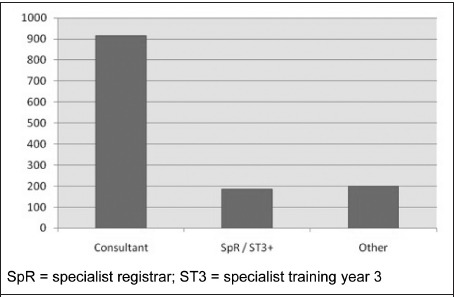
Grade of primary operating surgeon Revision rates
The most popular cemented stem was the Exeter™ V40™ (Howmedica, Newbury, UK) (n=520, 58%) with all other brands being used in fewer than 100 procedures. The most popular uncemented stem was the Corail® (DePuy, Warsaw, IN, US) (n=165, 46%) with all other brands being used in fewer than 100 procedures. The most popular cemented cups were the Contemporary (Howmedica) (n=143, 21%) and the Elite Plus™ Ogee® (DePuy) (n=124, 19%). The most popular uncemented cups were the Pinnacle® (DePuy) (n=139, 25%) and the Trident (Howmedica) (n=103, 19%).
Revision rates
The overall cumulative revision rate following total hip replacement for femoral neck fracture was 1.5% (95% CI: 0.9-2.4%) at one year, 2.0% (95% CI: 1.3-3.1%) at three years and 2.0% (95% CI: 1.3-3.1%) at five years. Revision rates (Table 1) varied according to prosthesis type (p=0.02), with those receiving an uncemented prosthesis having the highest revision rate at three years (4.1% [95% CI: 2.2-7.3%]).
Table 1.
Revision rates at three years after total hip replacement following a femoral neck fracture
| Patients | Revision rate* (95% CI) | Hazard ratio** (95% CI) | |
| Age | |||
| <65 years | 326(25%) | 3.2% (1.7-6.1%) | 1 |
| 65-74 years | 510(39%) | 1.2% (0.5-3.0%) | 0.6(0.3-1.5) |
| >75 years | 466(36%) | 2.1% (1.0-4.2%) | 0.7(0.3-1.6) |
| Sex | |||
| Female | 336(74%) | 1.8% (1.1-3.1%) | 1 |
| Male | 966(26%) | 2.5% (1.2-5.4%) | 0.7(0.3-1.8) |
| Physical status | |||
| PI (fit and healthy) | 184(14%) | 1.1% (0.3-4.3%) | 1 |
| P2 (mild disease) | 768(59%) | 1.6% (0.8-2.9%) | 1.3(0.3-6.1) |
| P3 (incapacitating disease) | 350(27%) | 3.7% (2.0-6.8%) | 2.7(0.6-12.3) |
| Prosthesis type | |||
| Cemented | 710(55%) | 0.9% (0.4-2.0%) | 1 |
| Uncemented | 350(27%) | 4.1% (2.2-7.3%) | 2.9(1.0-8.1) |
| Hybrid | 242(19%) | 2.2% (0.9-5.3%) | 2.1(0.6-7.6) |
| Incision approach | |||
| Posterior | 416(32%) | 3.5% (2.0-6.3%) | 2.2(1.0-5.3) |
| Other | 886(68%) | 1.3% (0.7-2.5%) | 1 |
unadjusted
adjusted for all other variables in the table
The revision rate at three years for patients receiving either a cemented or hybrid prosthesis was 0.9% (95% CI: 0.4-2.0%) and 2.2% (95% CI: 0.9-5.3%) respectively. The three-year revision rate for procedures in which a posterior incision approach was used was significantly higher than in cases where another approach was used (3.5% vs 1.3%, p=0.02). The youngest patients (under 65 years) had the highest revision rates at three years: 3.2% (95% CI: 1.7-6.1%) compared with 1.2% (95% CI: 0.5-3.0%) for patients aged 65-74 years and 2.1% (95% CI: 1.0-4.2%) in those aged 75 and over.
On average, men had a slightly higher revision rate than women (2.5% vs 1.8%). The revision rates at three years increased with poorer physical status (according to ASA grade): 3.7% (95% CI: 2.0-6.8%) for P3+, 1.6% (95% CI: 0.8-2.9%) for P2 and 1.1% (95% CI: 0.3-4.3%) for P1. The differences in revision rates by age, sex and physical status were not statistically significant (p=0.16,p=0.5 and p=0.11 respectively).
A multivariate analysis was carried out to investigate the association between prosthesis type and revision rates while adjusting for age, sex, physical status and approach. After adjustment, the risk of revision within three years for patients receiving an uncemented prosthesis was about three times that of someone who received a cemented prosthesis (HR: 2.9, 95% CI: 1.0-8.1, p=0.11). Important differences in the risk of revision by physical status and approach remained after adjustment but were not statistically significant (p=0.11 and p=0.06 respectively).
Length of hospital stay
The mean length of stay in hospital was 16 days. Length of stay varied significantly by age and physical status (both p<0.001). Length of stay was highest in those patients in the oldest age group and those with poorer physical status as described by ASA grade. On average, women stayed two days longer in hospital than men (p=0.02).
A multivariate analysis was carried out to investigate the association between prosthesis type and patient characteristics with length of stay. Table 2 shows the adjusted mean difference in length of stay. The effect of age and physical status on length of stay remained significant after adjustment for the other factors in the multivariate model (both p<0.0001). The effect of sex on length of stay also remained significant (p=0.04).
Table 2.
Length of hospital stay (LOS) for patients receiving a total hip replacement following a femoral neck fracture
| Patients | Mean LOS (days)* Mean (95% CI | Difference in mean LOS (days)** Mean (95% CD | |
| Age | |||
| <55 years | 325 (25%) | 14.9 (13.4-15.5) | 0 |
| 65-74 years | 510 (39%) | 12.9(11.9-13.9) | -1.9 (-3.9-0.1) |
| >75 years | 466 (36%) | 18.7 (17.2-20.2) | 3.4 (1.4-5.4) |
| Sex | |||
| Female | 336 (74%) | 17.0(15.2-18.9) | 0 |
| Male | 966 (26%) | 15.0(14.2-15.8) | -1.8 (-3.6— 0.1) |
| Physical status | |||
| PI (fit and healthy) | 184(14%) | 13.1 (11.2-15.1) | 0 |
| P2 (mild disease) | 768 (59%) | 14.1 (13.3-15.1) | 0.8 (-1.5-3.0) |
| P3 (incapacitating disease) | 350 (27%) | 19.7(17.9-21.5) | 5.7 (3.2-8.2) |
| Prosthesis type | |||
| Cemented | 710 (55%) | 15.4(14.5-16.4) | 0 |
| Uncemented | 350 (27%) | 16.0 (14.2-17.8 | 0.6 (-1.2-2.4) |
| Hybrid | 242 (19%) | 15.1 (13.3-16.8) | -0.2 (-2.2-1.9) |
unadjusted
adjusted for all other variables in the table
Co-morbidity
Of the 1,302 patients in this group, 475 (36%) had at least one co-morbid condition. There were twenty patients (2%) who had three or four co-morbid conditions. There were 350 patients (27%) in the poorest physical status group as recorded by ASA grade.
Mortality
Twenty patients died within thirty days of their procedure. The Kaplan-Meier estimate of 30-day mortality was 1.4% (95% CI: 1.0-2.4%), which is over twice the 30-day mortality rate for all 157,232 primary HES-linked total hip procedure patients identified by the ONS (0.6%). Of the 20 who died, 13 had received a cemented prosthesis. The 30-day mortality rate in the cemented group was the highest (1.8%, 95% CI: 1.1-3.2%) although the differences according to prosthesis types were not significant (p=0.45).
Mortality rates were significantly higher in older patients and those with poor physical status (both p<0.001). After adjustment for age, sex and prosthesis type, those patients with mild or incapacitating disease were over four times more likely die within thirty days than those who were fit and healthy (HR: 4.5, 95% CI: 1.8-11.2, p=0.002). Similarly, after adjustment for sex, prosthesis type and physical status, patients over 65 were about three times more likely to die within 30 days compared with the under 65s (p=0.01) (Table 3).
Table 3.
Thirty-day mortality rate after total hip replacement following a femoral neck fracture
| Patients | 30-day mortality* (95% CI | Hazard ratio** (95% CI | |
| Age | |||
| <65 years | 326 (25%) | 0.7% (0.3-1.6%) | 1 |
| ≥65 years | 976 (75%) | 3.0% (1.8-5.0%) | 3.4 (1.3-8.9) |
| Sex | |||
| Male | 336 (74%) | 2.1% (1.0-4.3%) | 1 |
| Female | 966 (26%) | 1.4% (0.8-2.3%) | 0.7 (0.3-1.7) |
| Physical status | |||
| P1 (fit and healthy) | 184 (14%) | 0.7% (0.4-1.5%) | 1 |
| P2 or P3 (mild or incapacitating disease) | 1,118(86)% | 3.7% (2.2-6.3%) | 4.5(1.8-11.2) |
| Prosthesis type | |||
| Cemented | 710 (55%) | 1.8% (1.1-3.2%) | 1 |
| Uncemented | 350 (27%) | 0.9% (0.3-2.6%) | 0.5 (0.2-1.9) |
| Hybrid | 242 (19%) | 1.7% (0.5-4.4%) | 1.0(0.3-3.1) |
unadjusted
adjusted for all other variables in the table
Discussion
Of the 157,232 NJR-HES linked primary hip replacement procedures, we identified 1,302 patients who had an emergency admission for a #NOF. The mean length of stay in hospital was 16 days, with older patients and those in the poorest health staying significantly longer. This is nearly double the national average length of stay following elective total hip replacement (8.8 days).9 Length of hospital stay did not vary with type of total hip replacement implanted. The overall 30-day mortality rate was 1.4%, with the over 65s and those patients with mild disease or worse having the highest mortality rates. This may be explained in part by 27% of patients from the database being recorded as ASA grade 3. This is almost double the proportion found in all the primary HES-linked procedures reported in the NJR 2009 annual report (15%).9
The overall three and five-year revision rate was 2.0%, with those patients receiving an uncemented prosthesis having the highest revision rate (4.1%). Overall, the revision rates were similar to those reported for all NJR-HES linked primary procedures in the 2009 annual report.9 However, the revision rate for uncemented procedures in this group of patients was higher than for all uncemented procedures described in the annual report (4.1% vs 2.8%).
The concerns raised by the NPSA do not seem to be reflected in published data discussing cementing techniques.11–14 There is evidence showing no increased mortality and, in fact, decreased morbidity with cemented versus uncemented hemiarthroplasty.15 A review of the Cochrane database did not show increased morbidity or mortality with the use of cemented arthroplasty for #NOF.16 Reopera-tion rates are shown to be reduced with total hip replacement (cemented or uncemented) compared with hemiarthroplasty.17 A previously published paper reviewing 38,488 patients retrospectively quoted an intra-operative mortality rate during elective total hip replacement of 0.06%.18 However, this was increased to 0.18% in those undergoing total hip replacement for #NOF. Thirty-day mortality rates have been quoted as high as 2.4%, far higher than that reflected in our data.11 A meta-analysis published in 2010 did not show any difference in mortality or incidence of deep infection between cemented hemiarthroplasty and total hip replacement at one year.5
There is increasing evidence that total hip replacement gives superior results to hemiarthroplasty in selected groups of patients. The previously published increased risk of dislocation in this group is not borne out in the NJR data. However, the NJR data look as an indication for a revision procedure and do not necessarily take into account those who may have suffered a dislocation or infection that is not treated by implant exchange. Furthermore, the data do not include periprosthetic fractures treated by fixation methods other than revision. Despite this, the overall revision rate of total hip replacement for #NOF is broadly similar to the overall rate for total hip replacement quoted by the NJR at five years, suggesting that these issues may not be a significant problem.
The Norwegian Arthroplasty Register reports good functional outcomes using total hip replacement for #NOF although inferior to elective osteoarthritic (OA) patients.2 Their data suggested increased risk of dislocation (especially in the first two weeks), infection and periprosthetic fracture compared with OA patients but this was not statistically significant after six months. However, the published data from this series only included patients over 60 years.
According to our data, the lowest revision risk appears to be when surgery is carried out via a lateral versus a posterior approach and this is reflected in previous published data.9 There can be no argument that proper component positioning protects against dislocation and it is therefore potentially controversial to argue that surgeons should perform total hip replacement via the lateral approach if they are not familiar with doing so. One should bear in mind that the proportion of total hip replacements performed via the posterior approach has increased recently from 39% in 2004 to 54% in 2008 (NJR data). The dislocation rate of total hip replacements may still be reduced with increasing use of larger femoral heads.19
This study does have limitations. Both HES and the NJR do not guarantee the quality of recording of reasons for revision. There is also a limitation of linkage. The reasons for linkage are discussed in the NJR but there is also a need for the addition of length of stay and ONS dates of death. Another limitation is the quality of the indication for surgery in the NJR data. This led to 803 exclusions as we tried to ensure as homogenous a group as possible. However, this has given us a well defined group. This is the first time the NJR has been used in this way and it is the largest study in the UK so far.
Conclusions
The trend in the majority of published work is that total hip replacement for #NOF gives comparable results with other indications. In the future, data from both the National Hip Fracture Database and the NJR may help define the best treatment in this cohort of patients.
References
- 1.Parker ML, Pryor G, Gurusamy K. Cemented versus uncemented hemiarthroplasty for intracapsular hip fractures: a randomised controlled trial in 400 patients. J Bone Joint Surg Br. 2010;92:116–122. doi: 10.1302/0301-620X.92B1.22753. [DOI] [PubMed] [Google Scholar]
- 2.Gjertsen JE, Lie SA, Fevang JM, et al. Total hip replacement after femoral neck fractures in elderly patients: results of 8,577 fractures reported to the Norwegian Arthroplasty Register. Acta Orthop. 2007;78:491–497. doi: 10.1080/17453670710014130. [DOI] [PubMed] [Google Scholar]
- 3.Greenough CG, Jones JR. Primary total hip replacement for displaced subcapital fracture of the femur. J Bone Joint Surg Br. 1988;70:639–643. doi: 10.1302/0301-620X.70B4.3403615. [DOI] [PubMed] [Google Scholar]
- 4.Baker RP, Squires B, Gargan MF, Bannister GC. Total hip arthroplasty and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck. A randomized, controlled trial. J Bone Joint Surg Am. 2006;88:2,583–2,589. doi: 10.2106/JBJS.E.01373. [DOI] [PubMed] [Google Scholar]
- 5.Hopley C, Stengel D, Ekkernkamp A, Wich M. Primary total hip arthroplasty versus hemiarthroplasty for displaced intracapsular hip fractures in older patients: systematic review. BMJ. 2010;340:c2–332. doi: 10.1136/bmj.c2332. [DOI] [PubMed] [Google Scholar]
- 6.Scottish Intercollegiate Guidelines Network. Management of Hip Fracture in Older People. Edinburgh: SIGN; 2009. [Google Scholar]
- 7.National Patient Safety Agency. Rapid Response Report NPSA/2009/RRR001: Mitigating Surgical Risk in Patients Undergoing Hip Arthroplasty for Fractures of the Proximal Femur. London: NPSA; 2009. [DOI] [PubMed] [Google Scholar]
- 8.Lee BP, Berry DJ, Harmsen WS, Sim FH. Total hip arthroplasty for the treatment of an acute fracture of the femoral neck: long-term results. J Bone Joint Surg Am. 1998;80:70–75. [PubMed] [Google Scholar]
- 9.National Joint Registry for England and Wales. 6th Annual Report 2009. Hemel Hempstead: NJR; 2010. [Google Scholar]
- 10.Armitage JN, van der Meulen JH. Identifying co-morbidity in surgical patients using administrative data with the Royal College of Surgeons Charlson Score. Br J Surg. 2010;97:772–781. doi: 10.1002/bjs.6930. [DOI] [PubMed] [Google Scholar]
- 11.Parvizi J, Ereth MH, Lewallen DG. Thirty-day mortality following hip arthroplasty for acute fracture. J Bone Joint Surg Am. 2004;86:1,983–1,988. doi: 10.2106/00004623-200409000-00017. [DOI] [PubMed] [Google Scholar]
- 12.Foster AP, Thompson NW, Wong J, Charlwood AP. Periprosthetic femoral fractures - a comparison between cemented and uncemented hemiarthroplasties. Injury. 2001;36:424–429. doi: 10.1016/j.injury.2004.07.023. [DOI] [PubMed] [Google Scholar]
- 13.Khan RJ, Mac Dowell A, Crossman P, Keene GS. Cemented or uncemented hemiarthroplasty for displaced intracapsular fractures of the hip - a systematic review. lnjury. 2002;33:13–17. doi: 10.1016/s0020-1383(01)00101-2. [DOI] [PubMed] [Google Scholar]
- 14.Emery RJ, Broughton NS, Desai K, et al. Bipolar hemiarthroplasty for subcapital fracture of the femoral neck. A prospective randomised trial of cemented Thompson and uncemented Moore stems. J Bone Joint Surg Br. 1991;73:232–234. doi: 10.1302/0301-620X.73B2.2005165. [DOI] [PubMed] [Google Scholar]
- 15.Timperley AJ, Whitehouse SL. Mitigating surgical risk in patients undergoing hip arthroplasty for fractures of the proximal femur. J Bone Joint Surg Br. 2009;91:851–854. doi: 10.1302/0301-620X.91B7.22617. [DOI] [PubMed] [Google Scholar]
- 16.Parker MJ, Gurusamy K. Arthroplasties (with and without bone cement) for proximal femoral fractures in adults. Cochrane Database Syst. doi: 10.1002/14651858.CD001706.pub3. ffei/2006; 3: CD001706. [DOI] [PubMed] [Google Scholar]
- 17.Gebhard JS, Amstutz HC, Zinar DM, Dorey FJ. A comparison of total hip arthroplasty and hemiarthroplasty for treatment of acute fracture of the femoral neck. Clin Orthop Relat Res. 1992;282:123–131. [PubMed] [Google Scholar]
- 18.Parvizi J, Holiday AD, Ereth MH, Lewallen DG. The Frank Stinchfield Award. Sudden death during primary total hip arthroplasty. Clin Orthop Relat Res. 1999;369:39–48. doi: 10.1097/00003086-199912000-00005. [DOI] [PubMed] [Google Scholar]
- 19.Berry DJ, von Knoch M, Schleck CD, Harmsen WS. Effect of femoral head diameter and operative approach on risk of dislocation after primary total hip arthroplasty. J Bone Joint Surg Am. 2005;87:2,456–2,463. doi: 10.2106/JBJS.D.02860. [DOI] [PubMed] [Google Scholar]


