Abstract
Members of the Bcl-2 family have critical roles in regulating tissue homeostasis by modulating apoptosis. Anti-apoptotic molecules physically interact and restrain pro-apoptotic family members preventing the induction of cell death. However, the specificity of the functional interactions between pro- and anti-apoptotic Bcl-2 family members remains unclear. The pro-apoptotic Bcl-2 family member Bcl-2 interacting mediator of death (Bim) has a critical role in promoting the death of activated, effector T cells following viral infections. Although Bcl-2 is an important Bim antagonist in effector T cells, and Bcl-xL is not required for effector T-cell survival, the roles of other anti-apoptotic Bcl-2 family members remain unclear. Here, we investigated the role of myeloid cell leukemia sequence 1 (Mcl-1) in regulating effector T-cell responses in vivo. We found, at the peak of the response to lymphocytic choriomeningitis virus (LCMV) infection, that Mcl-1 expression was increased in activated CD4+ and CD8+ T cells. Retroviral overexpression of Mcl-1-protected activated T cells from death, whereas deletion of Mcl-1 during the course of infection led to a massive loss of LCMV-specific CD4+ and CD8+ T cells. Interestingly, the co-deletion of Bim failed to prevent the loss of Mcl-1-deficient T cells. Furthermore, lck-driven overexpression of a Bcl-xL transgene only partially rescued Mcl-1-deficient effector T cells suggesting a lack of redundancy between the family members. In contrast, additional loss of Bax and Bak completely rescued Mcl-1-deficient effector T-cell number and function, without enhancing T-cell proliferation. These data suggest that Mcl-1 is critical for promoting effector T-cell responses, but does so by combating pro-apoptotic molecules beyond Bim.
Keywords: T cells, Mcl-1, Bim, Bax, Bak, Bcl-2
Bcl-2 family members have critical roles in immune system homeostasis. Indeed, genetic loss of the pro-apoptotic molecule Bcl-2-interacting mediator of death (Bim) or loss of both Bax and Bak results in lymphadenopathy.1, 2 Conversely, genetic loss of the anti-apoptotic molecules Bcl-2 or myeloid cell leukemia sequence 1 (Mcl-1) results in profound depletion of hematopoietic cells as well as developing thymocytes and peripheral T cells.3, 4, 5, 6 However, the specific interactions between pro- and anti-apoptotic Bcl-2 family members and how these relationships control lymphocyte homeostasis remain unclear.
During infection, T cells engage foreign antigen resulting in a proliferative expansion of antigen-specific effector T cells. After antigen elimination, the majority of these effector T cells die by apoptosis, whereas some survive and become memory cells.7 This culling of activated T cells is critical for restoring T-cell homeostasis, preventing autoimmunity, and promoting protective immune responses. Although initial work suggested a role for the death receptor pathway, more recent work has shown a dominant role of the mitochondrial pathway of apoptosis, governed by Bcl-2 family members, in regulating the death of activated T cells.7, 8 Indeed, the BH3-only molecule Bim, acting through Bax/Bak, is required for the apoptosis of most effector T cells.2, 9, 10, 11, 12, 13 Genetic ablation of Bim prevents the loss of effector CD4+ and CD8+ T cells and enhances protective immunity.12, 14 However, the molecular mechanism(s) by which Bim is normally antagonized to promote effector T-cell survival remains unclear.
The expression of Bcl-2 family members is dynamically regulated in activated T cells. During T-cell activation, the levels of Bcl-2 are decreased, whereas Bcl-xL expression is increased.13, 15, 16 However, despite the normal induction of Bcl-xL, T cell-specific genetic deletion of Bcl-xL did not exacerbate the contraction of CD4+ or CD8+ T cell responses,17 suggesting that either Bcl-xL is not required for effector T-cell survival or that it is redundant with other anti-apoptotic Bcl-2 family members. In the context of effector CD8+ T-cell subpopulations, KLRG-1hi cells have low expression of Bcl-2, whereas KLRG-1low effector cells have high expression of Bcl-2.13 This high level of Bcl-2 expression in KLRG-1low cells is critical for their resistance to Bim-mediated death and their survival into the memory compartment.13 Bcl-2 levels in activated T cells are controlled by IL-7 and IL-15 signaling through STAT5, a molecule essential for effector CD8+ T-cell survival.18 However, the role of other anti-apoptotic Bcl-2 family members in effector T-cell apoptosis remains unclear.
Mcl-1 is another Bcl-2 family member that is highly expressed in T cells.6, 19 Mcl-1 is critical for naive T-cell survival and Mcl-1 can efficiently bind to Bim in vitro and in vivo.6 A recent report suggested that, at least in vitro, Mcl-1 may be an important antagonist of Bim in naive T cells.20 Here, we investigated the role of Mcl-1 in maintaining activated T cells following lymphocytic choriomeningitis virus (LCMV) infection in mice. The loss of Mcl-1 during viral infection led to a massive loss of antigen-specific CD4+ and CD8+ T cells. Notably, the loss of effector T cells in Mcl-1-deleted mice was restored by the additional loss of Bax and Bak and was only partially restored by Bcl-xL overexpression, but was not restored by the additional loss of Bim. Together with our previous work on Bcl-2 being a major antagonist for Bim,13, 21 these data show a complex specificity between anti- and pro-apoptotic Bcl-2 family members in controlling T-cell fate.
Results
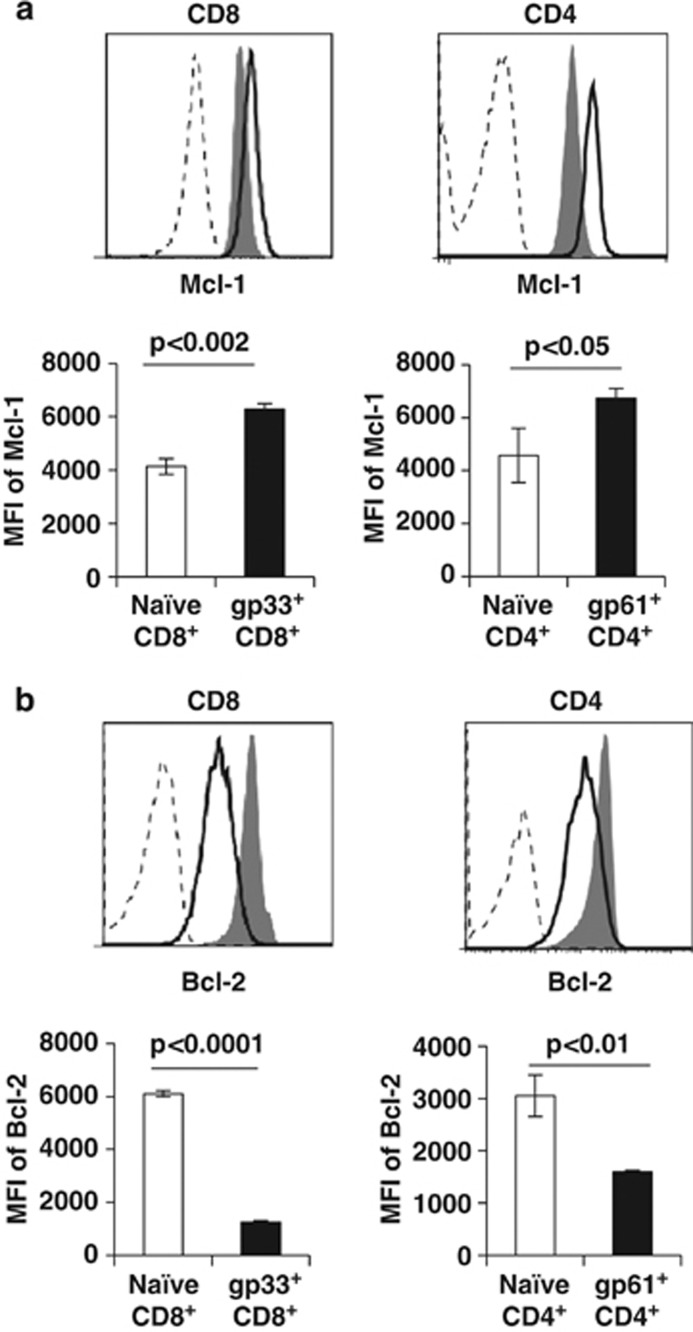
Divergent expression of Mcl-1 and Bcl-2 in effector CD4+ and CD8+ T cells
During T-cell activation, Bcl-2 levels are decreased in both CD4+ and CD8+ T cells, whereas Bcl-xL levels are increased.10, 19, 22, 23 A recent report showed that Mcl-1 levels are increased following in vitro T-cell activation,24 although whether or not Mcl-1 levels are changed in T cells activated in vivo remains unclear. We examined expression of Mcl-1 within antigen-specific CD4+ and CD8+ T cells after infection with LCMV. At 8 days after infection, Mcl-1 levels were increased within LCMV-sp. CD4+ and CD8+ T cells, as assessed by intracellular flow cytometric analysis of MHC-tetramer+ cells (Figure 1a). In contrast, Bcl-2 levels were decreased in both LCMV-sp. CD4+ and CD8+ T cells (Figure 1b). Together, these data suggest that Mcl-1 could be a survival factor for activated T cells, particularly when Bcl-2 levels are low.
Figure 1.
Divergent expression of Mcl-1 and Bcl-2 in effector T cells. C57BL/6 mice (N=3/group) were infected with LCMV (2 × 105 p.f.u. i.p.) and killed 8 days later. Single spleen cell suspensions were generated and 2 million cells were stained with antibodies directed against CD4 and CD8, with MHC tetramers and intracellulary with antibodies against Bcl-2 and Mcl-1. Results show the mean fluorescence intensity of (a) Mcl-1 versus (b) Bcl-2 staining in Dbgp33-sp. and I-Ab-gp61-sp. T cells ±S.E.M. Histograms display gated CD4+ or CD8+ events from either naive (filled histogram) or tetramer+ events from LCMV-infected mice (dark line, open histogram). Isotype controls for Mcl-1 and Bcl-2 are shown by dashed lines. Results are representative of six independent experiments with similar results
Mcl-1 is critical for survival of activated T cells in vivo
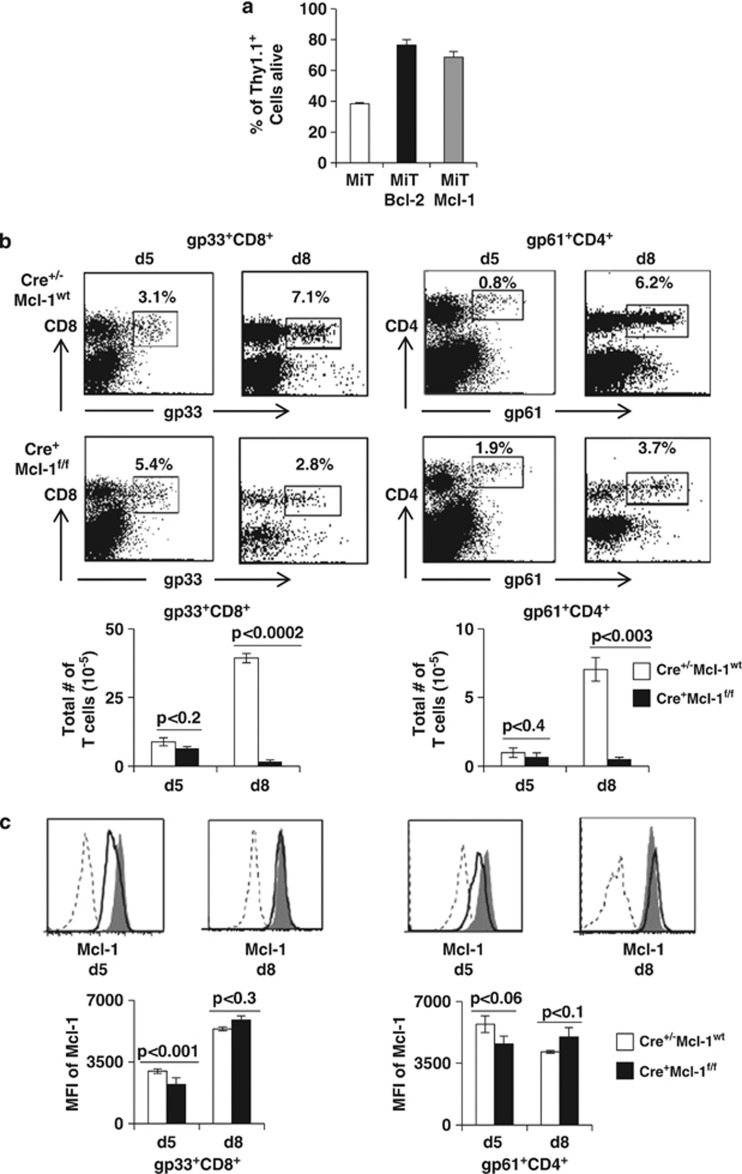
As Mcl-1 levels were increased in activated T cells, we next determined whether sustained Mcl-1 overexpression can promote effector T-cell survival. To obtain a large population of in vivo activated T cells for retroviral transduction, we injected Vβ8.2 TCR Tg (VβDO) mice with staphylococcal enterotoxin B (SEB) and 24 h later, transduced purified lymph node T cells with either empty retrovirus or retroviruses overexpressing Bcl-2 or Mcl-1 and tracked the survival of transduced (Thy1.1+), SEB-reactive, Vβ8-bearing T cells. Similar to overexpression of Bcl-2, retroviral overexpression of Mcl-1 afforded significant protection of activated T cells after 24 h culture in vitro (Figure 2a).
Figure 2.
Mcl-1 is critical for promoting effector T-cell responses. (a) VβDO mice were injected i.p. with 100 μg staphylococcal enterotoxin B and 24 h later purified splenic T cells were retrovirally transduced with either empty vector or with vectors encoding mBcl-2 or mMcl-1 cDNA and placed in culture (N=3/group). Twenty-four hours later, cells were stained with antibodies against CD4, CD8, and Thy1.1 and cell death assessed by live/dead gating as described previously.10, 23 Results show the percent of Thy1.1 cells alive after 24 h±S.E.M. (b and c) Groups of Mcl-1f/f and Mx1cre-Mcl-1f/f mice (N=4/group) were infected i.p. with LCMV, killed at either 5 or 8 days after infection (in separate experiments) and LCMV-sp. cells enumerated by MHC tetramer staining and flow cytometric analysis. (b) Results show the frequency of CD8+ cells that are gp33-sp. (left dot plots), CD4+ cells that are gp61-sp. (right dot plots) and the total numbers of CD8+ gp33-sp. and CD4+ gp61-sp.T cells. (c) Histograms show Mcl-1 staining in LCMV-sp. T cells from either Mcl-1f/f (shaded histogram) or Mx1cre-Mcl-1f/f (dark line) mice on either day 5 or day 8 after infection. Isotype control staining for Mcl-1 is depicted by the dashed line. Bar graphs show the mean fluorescence intensity of either Mcl-1 staining within LCMV-sp. CD4+ or CD8+ T cells on days 5 or 8 after infection ±S.E.M. Results are representative of four independent experiments with similar results
We next determined whether Mcl-1 was required for the generation of an effector T-cell response. Conventional Mcl-1-deficient embryos suffer from maturation defects at the blastomere stage along with defects in blastocyst peri-implantation.25 Further, T-cell-specific deletion of Mcl-1 results in massive lymphopenia due to reduced survival of thymocytes and peripheral naive T cells.6 To avoid these issues, we used a system in which Cre expression is controlled by the αIFN-inducible Mx1-promoter, to inducibly delete Mcl-1 during LCMV infection, as we have previously done to investigate the role of STAT5 in effector T-cell survival.18 Mx1Cre-Mcl-1f/f and Mcl-1f/f mice were infected with LCMV and their T-cell response assessed using class I and class II MHC tetramers. At day 5 after infection, although the frequency of tetramer+ CD4+ and CD8+ T cells in Mx1Cre-Mcl-1f/f mice were slightly increased, the total numbers of tetramer+ T cells in Mx1Cre-Mcl-1f/f mice were slightly decreased when compared with control mice (Figure 2b). This difference is likely due to a loss of total CD4+ and CD8+ T cells upon Mcl-1 deletion (Supplementary Figure 1). By day 8, both the frequency and total numbers of LCMV-sp CD4+ and CD8+ T cells in Mx1Cre-Mcl-1f/f mice was significantly reduced when compared with control mice (Figure 2b). We next examined the deletion of Mcl-1 in Mx1Cre-Mcl-1f/f mice by intracellular flow cytometry. Although Mcl-1 levels were decreased on day 5 after infection, by day 8 Mcl-1 levels in LCMV-sp. T cells were similar between Mx1Cre-Mcl-1f/f mice and controls (Figure 2c). We considered that the Mcl-1-induced loss of T cells may prevent control of viral infection and drive T-cell exhaustion, so we assessed viral load by plaque assay. On day 5 after infection, viral load was slightly higher in Mx1Cre-Mcl-1f/f mice, but by day 8, the virus was undetectable in the livers of both Mx1cre-Mcl-1f/f and Mcl-1f/f mice (Supplementary Figure 2). Thus, Mx1Cre-induced deletion of Mcl-1 led to massive loss of LCMV-sp. T cells, and selection for Mcl-1-expressing cells (that failed to delete Mcl-1) that were able to clear the infection.
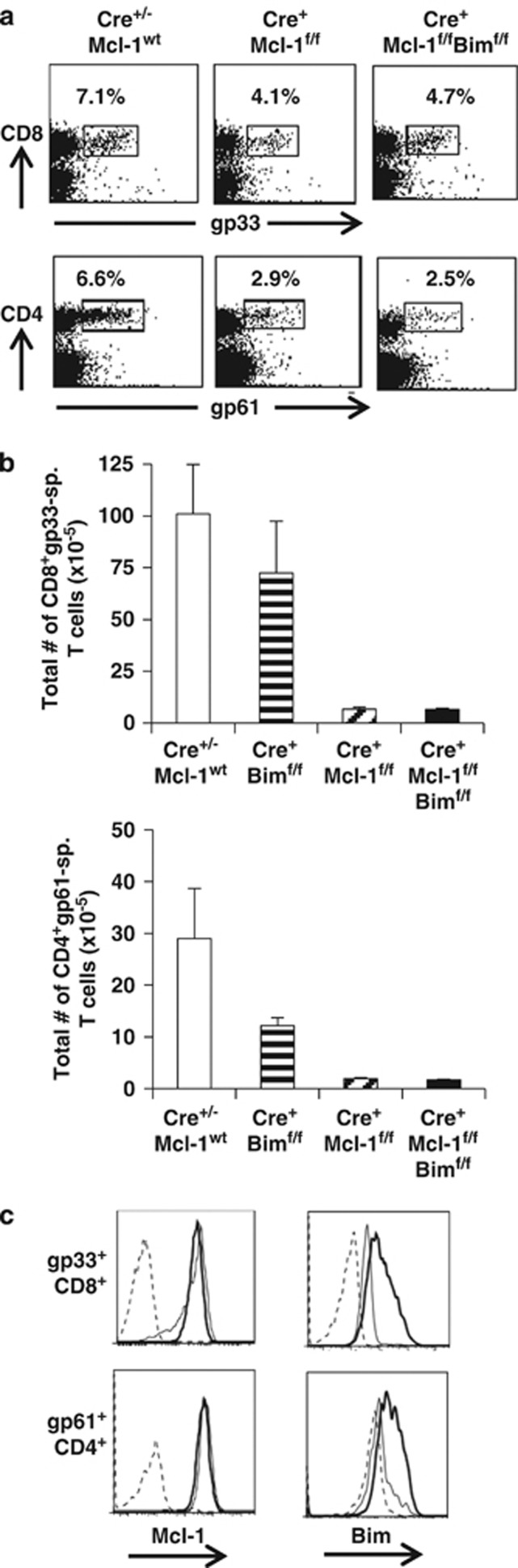
Concomitant loss of Bim does not rescue Mcl-1-deficient LCMV-sp. T cells
Mcl-1 can physically associate with Bim6 and has been shown to antagonize Bim in T cells activated in vitro.20 To test whether additional loss of Bim could promote survival of Mcl-1-deficient cells, we bred Mcl-1-deficient mice to Bimf/f mice.26 First, we administered polyI:C to groups of naive control, Mx1Cre-Mcl1f/f, and Mx1Cre-Mcl-1f/fBimf/f mice. PolyI:C induced a significant loss of CD4+ and CD8+ T cells in Mx1Cre-Mcl1f/f mice and the additional loss of Bim failed to rescue this T-cell loss (Supplementary Figure 3). We next examined whether Mcl-1-antagonized Bim in effector T cells by infecting the same groups of mice with LCMV. On day 8 after LCMV infection, the frequency and total numbers of CD4+ gp61-sp. and CD8+ gp33-sp.T cells were again decreased in Mx1Cre-Mcl-1f/f mice and the additional loss of Bim was unable to restore LCMV-sp T-cell responses (Figures 3a and b). In Mx1Cre-Bimf/f mice, the numbers and frequency of LCMV-sp. CD4+ and CD8+ T cells were similar to controls, consistent with our and others previous data showing that the total deletion of Bim does not increase LCMV-sp. T cells at the peak of the response.11, 12 We again failed to detect a significant loss of Mcl-1 staining in LCMV-sp. CD4+ or CD8+ T cells in Mx1Cre-Mcl-1f/f mice (Figure 3c). To assess Bim deletion, we measured Bim expression within tetramer+ T cells by intracellular flow cytometry using a Bim-specific antibody.27 Notably, we found substantial loss of Bim in CD4+gp61-sp and CD8+ gp33-sp T cells from Mx1Cre-Mcl-1f/f Bimf/f mice (Figure 3c). Thus, despite efficient deletion, this additional loss of Bim failed to restore either naive or LCMV-sp. CD4+ and CD8+ T-cell responses in mice that had inducibly deleted Mcl-1, suggesting that Mcl-1 antagonizes additional pro-apoptotic molecules in T cells.
Figure 3.
Additional loss of Bim is unable to promote Mcl-1-deficient T-cell responses. Groups of control Mcl-1f/f or Mx1Cre+Mcl-1wt, Mx1Cre-Bimf/f Mx1cre-Mcl-1f/f, and Mx1cre-Mcl-1f/fBimf/f mice (N=7 mice/group, pooled from two independent experiments with similar results) were infected with LCMV and 8 days later were killed and single spleen cell suspensions were stained with Dbgp33-41 and I-Abgp61-80 tetramers. Results show the (a) frequencies and (b) total numbers of LCMV-sp. CD4+ and CD8+ T cells in control Mcl-1f/f or Mx1Cre+Mcl-1wt, Mx1Cre-Bimf/f Mx1cre-Mcl-1f/f, and Mx1cre-Mcl-1f/f Bimf/f mice. (c) Results show the mean fluorescence intensity of either Mcl-1 staining or Bim staining from either Mcl-1wt animals (dark line) or from Mx1Cre-Mcl-1f/fBimf/f (light line) within LCMV-sp. CD4+ or CD8+ T cells. Isotype control staining is depicted by the dashed line
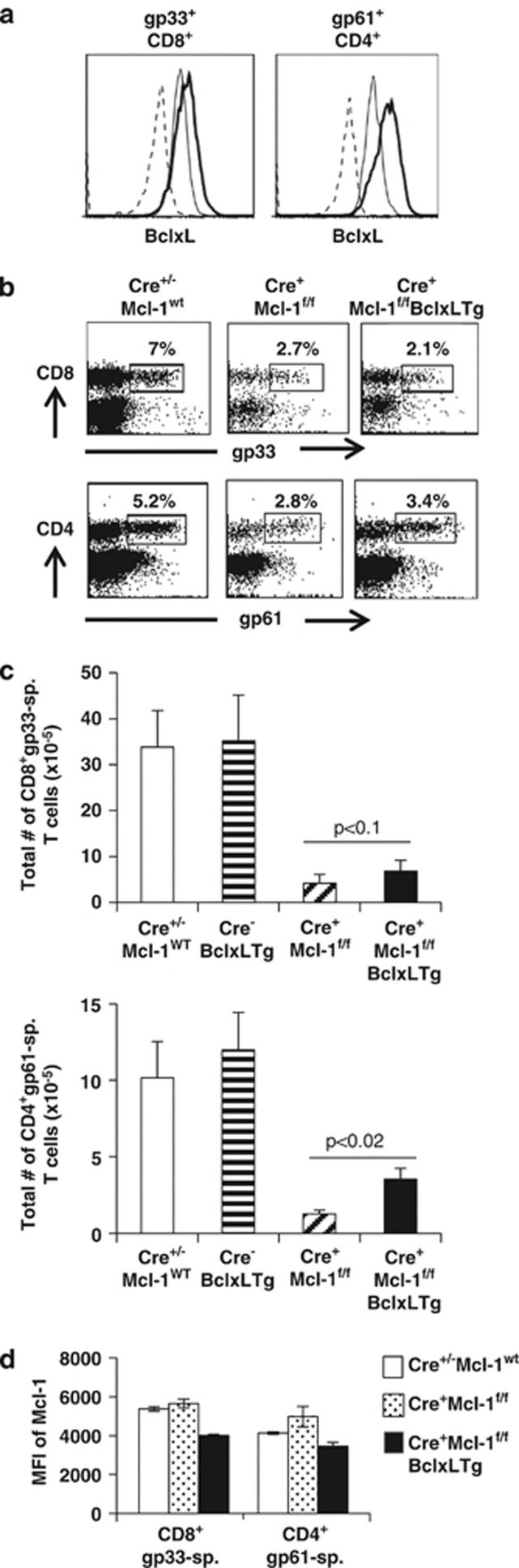
Bcl-xL overexpression partially restores CD4+, but not CD8+ T cells in inducible Mcl-1-deleted mice
To assess whether overexpression of Bcl-xL could substitute for Mcl-1 deletion and rescue LCMV-sp. T-cell responses, we bred lck-Bcl-xL Tg mice to Mx1Cre-Mcl-1f/f mice, infected them with LCMV, and assessed their T-cell responses on day 8 after infection. Bcl-xL levels, as assessed by intracellular flow cytometry were increased in both LCMV-sp. CD4+ and CD8+ T cells, although the increase was greater in CD4+gp61-sp. T cells (Figure 4a). Surprisingly, the frequency and total numbers of CD8+ gp33-sp. T cells in Mx1Cre-Mcl-1f/f mice were not restored by expression of ectopic Bcl-xL (Figures 4b and c). However, the frequency and total numbers of CD4+ gp61-sp. T cells were partially restored by Bcl-xL overexpression, but not back to control levels (Figures 4b and c). We observed a subtle (<20%) decrease in Mcl-1 levels in LCMV-sp. CD4+ and CD8+ T cells from lck-Bcl-xLMx1Cre-Mcl-1f/f mice (data not shown). Thus, even the overexpression of Bcl-xL is unable to compensate for the Mcl-1 deletion in activated CD8+ T cells and only partially compensates in CD4+ T cells in vivo.
Figure 4.
Transgenic overexpression of Bcl-xL partially rescues LCMV-sp. CD4+ but not CD8+ T-cell responses in inducible Mcl-1-deficient mice. Groups of control Mcl-1f/f or Mx1Cre+Mcl-1wt, lck-BclxLTg, Mx1cre-Mcl-1f/f, and lck-BclxLTg Mx1cre-Mcl-1f/f mice (N=4/group) were infected with LCMV and 8 days later were killed and single spleen cell suspensions were stained with Dbgp33-41 and I-Abgp61-80 tetramers. (a) Results show the mean fluorescence intensity of Bcl-xL staining from either Mcl-1wt animals (light line) or from Mx1Cre-Mcl-1f/fBcl-xLTg (dark line) within LCMV-sp. CD4+ or CD8+ T cells. Isotype control staining is depicted by the dashed line. Results show the (b) frequencies and (c) total numbers of LCMV-sp. CD4+ and CD8+ T cells in control Mcl-1f/f or Mx1Cre+Mcl-1wt, lck-BclxLTg, Mx1cre-Mcl-1f/f, and lck-BclxLTg Mx1cre-Mcl-1f/f mice
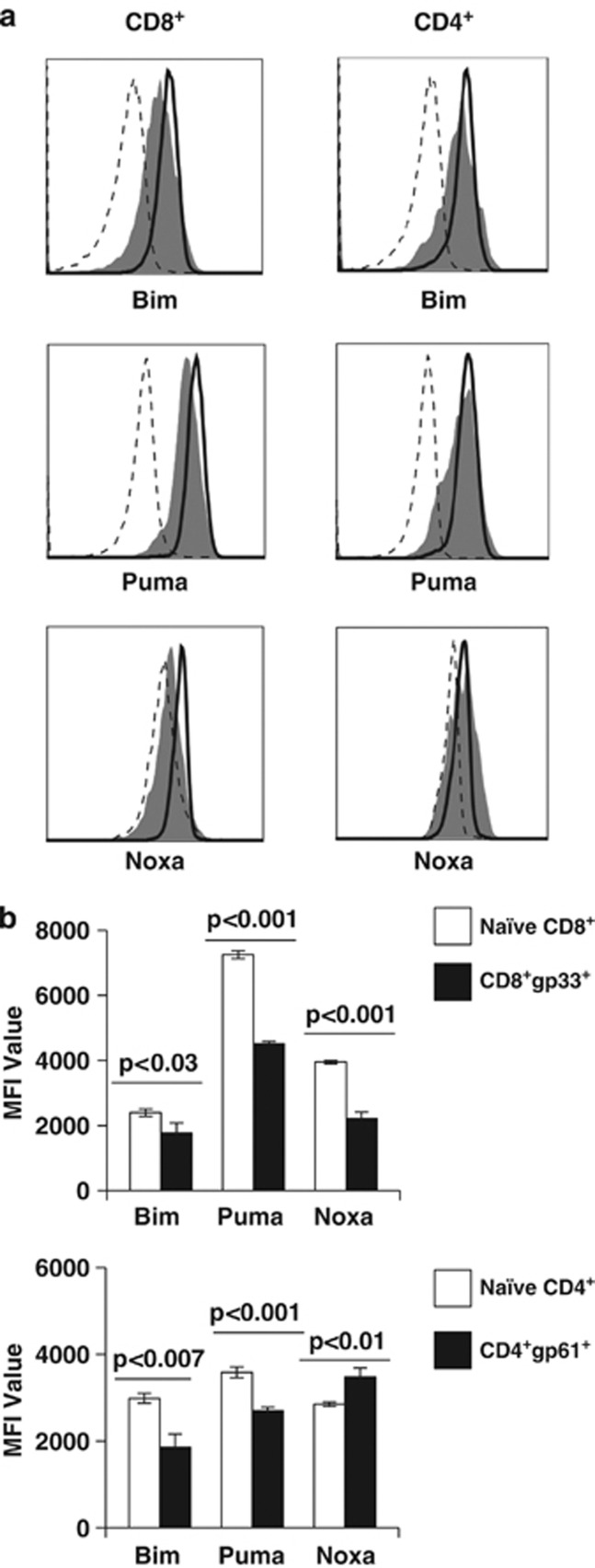
Levels of Puma, Bim, and Noxa are increased in LCMV-sp. effector T cells from Mx1Cre-Mcl1f/f mice
As concomitant loss of Bim was unable to restore LCMV-sp. T cells in Mx1Cre-Mcl-1f/f mice, we considered the possibility that Mcl-1 may antagonize multiple BH3-only molecules. We found that the levels of Bim, Puma, and Noxa were all expressed in naive CD4+ and CD8+ T cells (Figure 5). Specificity of the Puma antibody was confirmed on Puma-deficient mice (Supplementary Figure 4). Following LCMV infection, the levels of Bim and Puma were slightly decreased within effector CD4+ and CD8+ T cells (Figure 5), whereas Noxa was increased in LCMV-sp. CD4+, but not CD8+, T cells (Figure 5). Nonetheless, activated T cells express several BH3-only molecules, and the loss of Bim alone is not sufficient to restore T cells in Mcl-1-deficient mice.
Figure 5.
Expression of Puma, Bim, Noxa within naive and LCMV-sp. effector CD4+ and CD8+ T cells. Groups of C57BL/6 mice (N=4/group) were either left uninfected or were infected with LCMV and 8 days later were killed and single spleen cell suspensions were stained with Dbgp33-41 and I-Abgp61-80 tetramers and intracellularly with antibodies against either Bim, Puma, or Noxa (all from Cell Signaling Technologies). Stained cells were analyzed on an LSRII flow cytometer. (a) Results show the levels of either Bim, Puma, or Noxa within either naive (dark line) LCMV-sp. or CD8+ gp33+ cells (filled histogram, left panels) or CD4+ gp61+ T cells (filled histogram, right panels). Isotype control staining is depicted by the dashed lines. (b) Data are presented as the mean fluorescence intensity of the Bim, Puma, or Noxa stains within either naive or LCMV-sp. CD4+ or CD8+ T cells ±S.E.M.
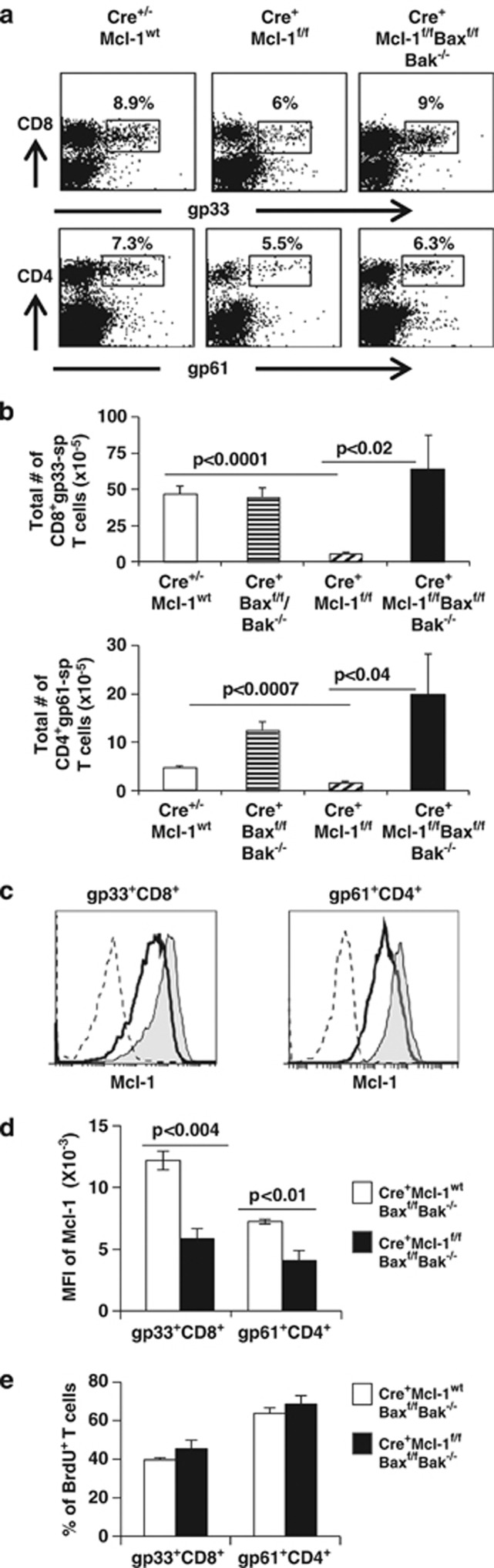
Concomitant loss of Bax and Bak restores Mcl-1-deficient effector T cells
Neither the single additional loss of Bim nor the overexpression of Bcl-xL, substantially restored effector T-cell responses in Mcl-1-deleted mice, suggesting that Mcl-1 may target multiple BH3-only molecules in a manner independent of Bcl-xL or that Mcl-1 targets the downstream apoptotic effectors Bax and Bak. Alternatively, we recently showed that an isoform of Mcl-1 contributes to mitochondrial respiration and ATP generation,28 raising the possibility that Mcl-1 may function in a non-apoptotic manner to control T-cell responses. To distinguish between these possibilities, we generated mice lacking Bak that were also conditionally deficient in Bax and Mcl-1. The additional loss of Bax and Bak would prevent the induction of apoptosis upon loss of Mcl-1, but would not rescue mitochondrial function. Mx1Cre-Mcl-1f/f and Mx1Cre-Mcl-1f/fBaxf/fBak−/− mice (along with the respective controls) were infected with LCMV, killed at day 8 of infection and the numbers of LCMV-sp. T cells were assessed with MHC tetramers. Inducible deletion of Mcl-1 resulted again in decreased CD4+ gp61-sp. and CD8+ gp33-sp. T-cell responses; however, in Mx1Cre-Mcl-1f/fBaxf/fBak−/− mice, the frequency and total numbers of LCMV-sp. CD4+ and CD8+ T cells were restored (Figures 6a and b). Further, the loss of both Bax and Bak allowed the survival and persistence effector T cells with decreased Mcl-1 expression indicating that the deletion of both pro-apoptotic effectors relieves the need of Mcl-1 (Figure 6c).
Figure 6.
Concomitant loss of Bax and Bak restores LCMV-sp. CD4+ and CD8+ T-cell responses in inducible Mcl-1-deficient mice. Groups of control Mcl-1f/f or Mx1Cre-Mcl-1wt, Mx1cre-Baxf/f Bak−/−, Mx1cre-Mcl-1f/f, and Mx1cre-Mcl-1f/f Baxf/f Bak−/− mice (N=4/group, pooled from two independent experiments) were infected with LCMV and 8 days later were killed and single spleen cell suspensions were stained with Dbgp33-41 and I-Abgp61-80 tetramers. Results show the (a) frequencies and (b) total numbers of LCMV-sp. CD4+ and CD8+ T cells in control Mcl-1f/f or Mx1Cre+Mcl-1wt, Mx1cre-Baxf/f Bak−/−, Mx1cre-Mcl-1f/f, and Mx1cre-Mcl-1f/f Baxf/f Bak−/− mice. (c, d) Results show the mean fluorescence intensity of Mcl-1 staining within LCMV-sp. CD4+ or CD8+ T cells ±S.E.M. from either Mx1Cre-Mcl-1f/f animals (shaded histogram) or from Mx1cre-Mcl-1f/f Baxf/f Bak−/− mice (dark line). Isotype control staining is depicted by the dashed line. Results are pooled from two independent experiments with similar results. (e) Mice were injected with BrdU on day 6 and 7 after infection, killed on day 8 and splenic single cell suspensions were stained with MHC tetramers and intracellularly with anti-BrdU antibodies. Results show the percent of either CD8+gp33-sp. or CD4+gp61-sp. T cells that are BrdU+ from either Mx1cre-Baxf/f Bak−/− or Mx1cre-Mcl-1f/f Baxf/f Bak−/−±S.E.M.
To determine whether the restoration of Mcl-1-deleted effector T cells by the additional loss of Bax and Bak was due to increased proliferation of these cells, we injected the mice with BrdU and assessed BrdU incorporation in tetramer+ T cells. The frequency of LCMV-sp. CD4+ and CD8+ T cells that were BrdU+ was higher in Mx1Cre-Mcl-1f/fBaxf/fBak−/− mice compared with Mx1Cre-Baxf/fBak−/− mice (Figure 6d). However, the 2–4% difference in the percentage of BrdU+ T cells is insufficient to account for the three- to sixfold increase in T cells rescued by the combined absence of Bax and Bak. Importantly, the effector T cells retained functionality, as similar frequencies of IFN-γ/TNF-α-producing T cells were observed in mice that had or had not inducibly deleted all three genes (Supplementary Figure 5). Further, virus was undetectable in the livers of mice with deletions of Mcl-1, Bax, and Bak on day 8 after infection (data not shown). Thus, the absence of both Bax and Bak promoted the survival and functionality of effector CD4+ and CD8+ effector T cells following inducible Mcl-1 deletion.
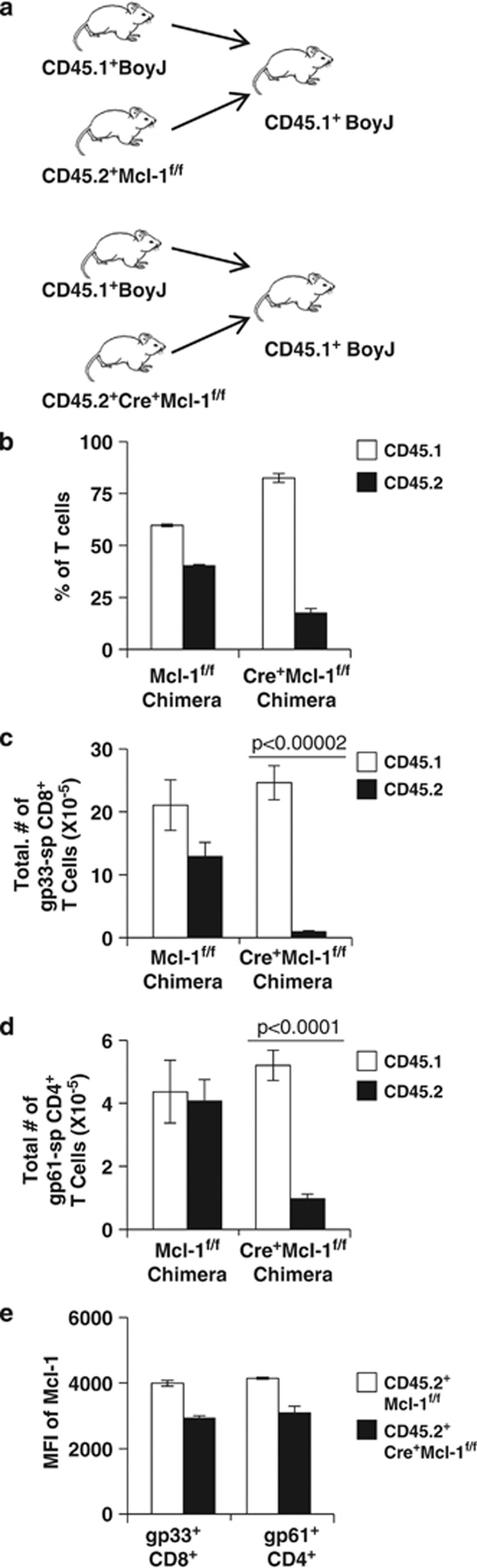
Mixed bone marrow (BM) chimeras reveal a cell intrinsic effect of Mcl-1 on T-cell survival
One caveat of the Mx1Cre-system is that during the course of the response, Mcl-1 is being deleted in multiple type I interferon responsive tissues and not just in T cells.5 To circumvent this issue, we generated mixed BM chimeras using BM from CD45.1+ B6.SJL-Ptprca Pepcb/BoyJ (referred to as CD45.1 congenics) and CD45.2+ Mx1Cre-Mcl-1f/f mice or from CD45.1 congenics and Mcl-1f/f as controls at a 50 : 50 ratio into lethally irradiated CD45.1 congenic recipients (Figure 7a). Before infection, there was a reduced engraftment of Mx1Cre-Mcl1f/f cells in the peripheral blood of mixed BM chimeras (Figure 7b). Nine weeks after reconstitution, mice were infected with LCMV and the numbers of control CD45.1 cells versus Mx1Cre-Mcl-1f/f CD45.2, LCMV-sp. CD4+ and CD8+ T cells were enumerated on day 8 after infection. In control mice, the numbers of CD8+ gp33-sp. and CD4+ GP61-sp. T cells derived from CD45.2 Mcl-1f/f mice were slightly decreased compared with those derived from CD45.1 congenics (Figure 7c), likely because of the slightly lower CD45.2 chimerism observed in these animals (Figure 7b). In contrast, the numbers of CD8+ gp33-sp. and CD4+ gp61-sp. derived from CD45.2 Mx1Cre-Mcl-1f/f BM were decreased when compared the same cells derived from CD45.1 congenics (Figures 7c and d). Although the chimerism was lower in this group (Figure 7b), there was a significant loss of both CD8+ gp33-sp. and CD4+ gp61-sp. derived from CD45.2 Mx1Cre-Mcl-1f/f BM compared with their CD45.1 congenic controls (Figures 7c and d). The few tetramer+ cells emerging from the CD45.2 Mx1Cre-Mcl-1f/f BM exhibited a slight decrease in Mcl-1 levels compared with controls (Figure 7e). Together, these data demonstrate that Mcl-1 is required in a cell intrinsic manner for generation of LCMV-sp. CD4+ and CD8+ T-cell responses.
Figure 7.
Cell intrinsic requirement for Mcl-1 in promoting CD4+ and CD8+ T-cell responses. (a) Generation of mixed bone marrow chimeras. Groups of BoyJ, Mcl-1f/f, and Mx1Cre-Mcl-1f/f mice (N=4/group) were killed and bone marrow removed and mixed 50/50 in the combinations shown and injected i.v. into irradiated Boy/J recipient mice. (b) Results show the percent chimerism (% of T cells that are either CD45.1+ or CD45.2+) in peripheral blood cells from either the control chimeras (Boy/J:Mcl-1f/f) or Mx1Cre-Mcl-1f/f chimeras (Boy/J:Mx1Cre-Mcl-1f/f) at 6 weeks after transplant. Nine weeks after bone marrow transplant, mixed bone marrow chimeric mice were injected with LCMV, killed 8 days later and numbers of gp33-sp and gp61-sp. T cells enumerated in the spleen by staining with MHC class I and class II tetramers and flow cytometry. (c and d) Results show the total numbers of CD8+ gp33-sp. (c) versus CD4+ gp61-sp. (d) T cells in CD45.1 cells (white bars) versus CD45.2 cells (black bars) from either control chimeras (Boy/J:Mcl-1f/f, left side) or Mx1Cre-Mcl-1f/f chimeras (Boy/J:Mx1Cre-Mcl-1f/f, right side). (e) Results show the levels of Mcl-1 within CD45.2 cells from either the control chimeras (Boy/J:Mcl-1f/f) or Mx1Cre-Mcl-1f/f chimeras (Boy/J:Mx1Cre-Mcl-1f/f)
Discussion
T cells express multiple pro- and anti-apoptotic Bcl-2 family members, however, the interactions between individual Bcl-2 family members and their specific roles in maintaining T-cell homeostasis has remained unclear. Initial work, using BH3 peptides from BH3-only pro-apoptotic Bcl-2 family members indicated that Bim and Puma could bind to nearly all anti-apoptotic molecules, whereas Noxa and Bad were more selective, Bad bound to Bcl-2, Bcl-xL, and Bcl-w but not A1 or Mcl-1 and Noxa had a higher affinity for Mcl-1 and A1 but not for Bcl-2, Bcl-xL, or Bcl-w.29 These data are consistent with the function of ABT-737, a BH3-mimetic based on the BH3 domain of Bad, which targets Bcl-2, Bcl-xL, and Bcl-w, but not A1 or Mcl-1.30 We previously showed that that Mcl-1 is a critical survival molecule for promoting naive T-cell survival in vivo6 and others have found that Mcl-1 is critical for activated and memory T-cell survival in vitro.24 Mcl-1 also possesses another function, to ensure appropriate mitochondrial respiration,28 and it was possible that this function of Mcl-1 contributed to T-cell homeostasis. However, our ability to rescue T-cell responses by the additional loss of Bax and Bak demonstrates that the anti-apoptotic function of Mcl-1 contributes significantly to its ability to maintain T-cell homeostasis. Both biochemical and genetic experiments have suggested an interaction between Bim and Mcl-1 in naive T cells6, 20 and other cells,31, 32 although the in vivo functionality of this interaction has not been assessed. Our data show that the in vivo deletion of Bim fails to rescue Mcl-1-deficient cells, whereas the loss of Bax and Bak is sufficient to rescue CD4+ and CD8+ T-cell responses in Mcl-1-deleted mice.
We envision three possible models by which Mcl-1 protects activated T cells from death. First, Mcl-1 may act downstream of Bim, targeting the pro-apoptotic molecules Bax and/or Bak. In support of this model, it has been shown that Mcl-1 can antagonize Bak on the mitochondria.33, 34 Furthermore, the additional loss of Bak restored most cells when Mcl-1 was deleted in vitro, but only when IL-7 is present.20 However, we have failed to observe rescue of Mcl-1-deleted hematopoietic cells by the loss of Bak alone (data not shown). Nonetheless, it is possible that loss of Mcl-1 can directly lead to the spontaneous activation of both Bax and Bak in T cells. Second, it is possible that Mcl-1 inhibits a pro-apoptotic BH3-only member that functions independently of Bim. Indeed, our data show that activated T cells express Puma and Noxa in addition to Bim; therefore, it is possible that with the loss of Mcl-1, Puma, Noxa, and Bim can all facilitate the activation of Bax and Bak.29, 35 The third possibility is that Mcl-1 acts as to ‘tune' Bim-mediated death. In this scenario, Bim is largely inhibited by another anti-apoptotic Bcl-2 family member, such as Bcl-2, and Mcl-1 buffers excess Bim that is not antagonized by Bcl-2. Thus, in activated T cells, increased Mcl-1 expression may enhance resistance to death at a time when it is critical to balance pathogen clearance with immunopathology. Consistent with this concept, it has been shown that GSK-3β inhibitors can maintain Mcl-1 levels and prolong activated T-cell survival.36
The loss of Bim failed to restore Mcl-1-deficient cells, so what normally restrains Bim in T cells? We recently showed that the loss of naive, effector, and memory CD8+ T cells in Bcl-2-deficient or ABT-737-treated mice are largely rescued by additional Bim deficiency.13, 21 A critical component to the sparing of effector CD8+ T cells is the action of the cytokines IL-7 and IL-15 that act to drive STAT5-dependent expression of Bcl-2.18 IL-4, IL-7, and IL-15 can induce an increase in Mcl-1 protein levels in activated T cells20 and Mcl-1 levels are largely controlled post-translationally,37 one possibility is that cytokines regulate Mcl-1's stability. However, when we cultured T cells with cycloheximide, neither IL-7 nor IL-15 significantly stabilized Mcl-1 levels within effector CD8+ T cells (data not shown). Further, IL-7 can increase the survival of Mcl-1-deleted T cells to a similar extent as Bcl-2 overexpression and IL-7 failed to further improve survival of Bcl-2 Tg/Mcl-1-deficient effector T cells.20 Together, these data suggest that a major survival function of cytokines is to promote the transcriptional upregulation of Bcl-2 rather than to modulate the turnover of Mcl-1.
In summary, these data suggest that critical and specific interactions between Bcl-2 family members control T-cell homeostasis. This is important because of the potential development of Bcl-2 antagonists being developed as therapeutics. As these drugs are developed for combating tumors, understanding the specificity of their interactions is crucial. One such drug, ABT-737 specifically antagonizes Bcl-2, Bcl-xL, and Bcl-w, but not A1 or Mcl-1 and is effective at tumors that express high levels of Bcl-2 or Bcl-xL, but it is ineffective against tumors expressing high levels of Mcl-1.30, 38, 39 In tumors that do not express high levels of Bcl-2, Bcl-xL, or Bcl-w, other Bcl-2 family member antagonists may be more beneficial. However, a possible complication to these inhibitors is that they may cause lymphopenia.21 Therefore, these inhibitors may also be exploited to target specific populations of T cells (activated effector cells) when these cells are wreaking havoc (e.g., autoimmunity). Indeed, recent studies have exploited their use in mouse models of autoimmunity with substantial benefit.40, 41 For such therapeutics to have maximal efficiency with minimal off-target effects, gaining knowledge of the specific interactions between Bcl-2 family members in specific populations of cells is essential. Despite a large amount of literature showing biochemical interactions between Bim and Mcl-1, we clearly show that, in vivo, the additional loss of Bim fails to rescue the loss of cells imposed by Mcl-1 deficiency. These data highlight the need to more carefully define the specific and antagonistic interactions between Bcl-2 family members that are operative in vivo.
Materials and Methods
Mice
Conditional Mcl-1f/f mice6 were crossed to Mx1Cre mice (Jackson Laboratory, Bar Harbor, ME, USA); to Lck-human Bcl-xL Tg mice (Jackson Laboratory); to Baxf/fBak−/− mice;26 and to Bimf/f mice26 (a kind gift from the late S. Korsmeyer). Puma-deficient mice were purchased from Jackson Laboratory. VβDO mice express the TCRβ chain from the DO11.10 TCR in a B10.D2 background.10, 42 B6.SJL-Ptprca Pepcb/BoyJ (BoyJ) were purchased from Jackson Laboratory. All animal protocols were reviewed and approved by our institutional animal care and use committees.
Virus
The Armstrong-3 strain of LCMV, described previously,43 was grown in BHK-21 cells; the number of plaque-forming units (p.f.u.) was assayed on Vero cells as described.43 Mice were injected intraperitoneally (i.p.) with 0.25 ml of LCMV (2 × 105 p.f.u.) diluted in balanced salt solution. Determination of liver viral load was determined by plaque assay on Vero cells as described.43
Molecular biology
Mouse Mcl-1 cDNA was purchased from Addgene (Cambridge, MA, USA) and subcloned into the retroviral plasmid MiT.44 MiT-Bcl-2 was generated as described.10 Retroviruses were generated by cotransfection of HEK293 with pCLEco and the MiT plasmid of interest by using calcium phosphate as described.10 After transduction, cells were stained with various fluorescently labeled antibodies and live and dead cells were distinguished by their forward side scatter properties using a flow cytometer as described.10
MHC tetramers
Class II MHC tetrameric staining reagents were created as described.45, 46 The methodology for preparation of MHC class I tetramers was modified from the protocol described by Altman and co-workers47 and were created as described previously.12, 48 For some experiments, I-Abgp66-77 tetramers were obtained from the NIH Tetramer Core Facility. We have observed no significant difference in tracking the LCMV-sp. CD4+ T-cell response using homemade versus NIH-generated LCMV-sp. class II tetramers.
Flow cytometry
Spleens were harvested and 106 cells were stained with fluorochrome-labeled antibodies (anti-CD4, anti-CD8, anti-CD44, anti-IL-7R and anti-KLRG-1) or intracellularly with antibodies against Bcl-xL (BD Transduction Labs, San Jose, CA, USA); Mcl-1 (Rockland Immunochemical, Gilbertsville, PA, USA); Bcl-2 (made in house from hybridoma 3F11); and Bim (Cell Signaling, Danvers, MA, USA), and data acquired using an LSRII flow cytometer (BD Biosciences, San Jose, CA, USA). Data were analyzed with FacsDIVA software (BD Biosciences). Antigen-specific CD4+ T cells were identified by staining 2 × 106 spleen cells with I-Abgp61-80 tetrameric staining reagents for 2 h at 37 °C, gating away from CD16/32+ cells as described.12 LCMV-sp. CD8+ T cells were detected by staining 2 × 106 cells/well with either Dbgp33 tetrameric staining reagents for 90 min at 4 °C followed by cell surface marker staining as described.12
Intracellular cytokine staining was performed as described.12 Briefly, spleen cells from mice were cultured at 37 °C for 4–5 h with or without various LCMV peptides (GP61-80 10 μg/ml; GP33-41, at 1 μg/ml) and BrefeldinA at 10 μg/ml. After culture, cells were stained for cell surface markers (CD4, CD8, CD44, antibodies from BD Pharmingen, San Jose, CA, USA) for 45 min at 4 °C. Cells were then washed, fixed, and permeabilized with 0.03% saponin and stained intracellularly with PE-labeled anti-IFN-γ or anti-IL-2 antibody (BD Pharmingen). A minimum of 5 × 105 events were acquired on a FacsCalibur flow cytometer and analyzed using CellQuest software (BD Biosciences).
Mixed bone marrow chimeras
BM from Mcl-1f/f Mx1Cre mice (CD45.2+) was mixed 1 : 1 with BM from B6.SJL-Ptprca Pepcb/BoyJ (CD45.1+) and 5 × 106 cells injected intravenously into lethally irradiated (1100 Rads) BoyJ recipients and allowed to engraft for 8 weeks at which time peripheral blood analyses indicated stable engraftment of both CD45.1 and CD45.2 cell surface-positive cells at a 3 : 1 ratio. The chimeric mice were then infected as described.
Statistical analyses
Statistical analyses were performed using a Student's two-sample t-test with Minitab for Windows Software (Release 14), State College, PA, USA.
Acknowledgments
We thank the Hildeman and Opferman labs for helpful suggestions and comments. This work was supported by Public Health Service Grants AI057753 and DK081175 (to DAH) and HL102175, the American Cancer Society 119130-RSG-10-255-01-LIB, a Cancer Center Support Grant P30CA021765, and the American Lebanese Syrian Associated Charities of St. Judes Children's Research Hospital (to JTO).
Author Contributions
JTO and DAH designed the research; PT and BK performed the research; DAH, JTO, BK, and PT analyzed and interpreted the data; PT performed the statistical analysis; and JTO and DAH wrote the manuscript.
Glossary
- Bim
Bcl-2-interacting mediator of death
- BM
bone marrow
- LCMV
lymphocytic choriomeningitis virus
- Mcl-1
myeloid cell leukemia sequence 1
- p.f.u.
plaque forming units
- SEB
staphylococcal enterotoxin B
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies this paper on Cell Death and Differentiation website (http://www.nature.com/cdd)
Edited by C Borner
Supplementary Material
References
- Bouillet P, Metcalf D, Huang DC, Tarlinton DM, Kay TW, Kontgen F, et al. Proapoptotic Bcl-2 relative Bim required for certain apoptotic responses, leukocyte homeostasis, and to preclude autoimmunity. Science. 1999;286:1735–1738. doi: 10.1126/science.286.5445.1735. [DOI] [PubMed] [Google Scholar]
- Rathmell JC, Lindsten T, Zong WX, Cinalli RM, Thompson CB. Deficiency in Bak and Bax perturbs thymic selection and lymphoid homeostasis. Nat Immunol. 2002;3:932–939. doi: 10.1038/ni834. [DOI] [PubMed] [Google Scholar]
- Nakayama K, Nakayama K, Negishi I, Kuida K, Shinkai Y, Louie MC, et al. Disappearance of the lymphoid system in Bcl-2 homozygous mutant chimeric mice. Science. 1993;261:1584–1588. doi: 10.1126/science.8372353. [DOI] [PubMed] [Google Scholar]
- Veis DJ, Sorenson CM, Shutter JR, Korsmeyer SJ. Bcl-2-deficient mice demonstrate fulminant lymphoid apoptosis, polycystic kidneys, and hypopigmented hair. Cell. 1993;75:229–240. doi: 10.1016/0092-8674(93)80065-m. [DOI] [PubMed] [Google Scholar]
- Opferman JT, Iwasaki H, Ong CC, Suh H, Mizuno S, Akashi K, et al. Obligate role of anti-apoptotic MCL-1 in the survival of hematopoietic stem cells. Science. 2005;307:1101–1104. doi: 10.1126/science.1106114. [DOI] [PubMed] [Google Scholar]
- Opferman JT, Letai A, Beard C, Sorcinelli MD, Ong CC, Korsmeyer SJ. Development and maintenance of B and T lymphocytes requires antiapoptotic MCL-1. Nature. 2003;426:671–676. doi: 10.1038/nature02067. [DOI] [PubMed] [Google Scholar]
- Kurtulus S, Tripathi P, Opferman JT, Hildeman DA. Contracting the 'mus cells'--does down-sizing suit us for diving into the memory pool. Immunol Rev. 2010;236:54–67. doi: 10.1111/j.1600-065X.2010.00920.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Cruz LM, Rubinstein MP, Goldrath AW. Surviving the crash: transitioning from effector to memory CD8+ T cell. Semin Immunol. 2009;21:92–98. doi: 10.1016/j.smim.2009.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grayson JM, Weant AE, Holbrook BC, Hildeman D. Role of Bim in Regulating CD8+ T-cell responses during chronic viral infection. J Virol. 2006;80:8627–8638. doi: 10.1128/JVI.00855-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hildeman DA, Zhu Y, Mitchell TC, Bouillet P, Strasser A, Kappler J, et al. Activated T cell death in vivo mediated by proapoptotic bcl-2 family member bim. Immunity. 2002;16:759–767. doi: 10.1016/s1074-7613(02)00322-9. [DOI] [PubMed] [Google Scholar]
- Prlic M, Bevan MJ. Exploring regulatory mechanisms of CD8+ T cell contraction. Proc Natl Acad Sci USA. 2008;105:16689–16694. doi: 10.1073/pnas.0808997105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wojciechowski S, Jordan MB, Zhu Y, White J, Zajac AJ, Hildeman DA. Bim mediates apoptosis of CD127(lo) effector T cells and limits T cell memory. Eur J Immunol. 2006;36:1694–1706. doi: 10.1002/eji.200635897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurtulus S, Tripathi P, Moreno-Fernandez ME, Sholl A, Katz JD, Grimes HL, et al. Bcl-2 allows effector and memory CD8+ T cells to tolerate higher expression of Bim. J Immunol. 2011;186:5729–5737. doi: 10.4049/jimmunol.1100102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reckling S, Divanovic S, Karp CL, Wojciechowski S, Belkaid Y, Hildeman D. Proapoptotic Bcl-2 family member Bim promotes persistent infection and limits protective immunity. Infect Immun. 2008;76:1179–1185. doi: 10.1128/IAI.01093-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaech SM, Tan JT, Wherry EJ, Konieczny BT, Surh CD, Ahmed R. Selective expression of the interleukin 7 receptor identifies effector CD8 T cells that give rise to long-lived memory cells. Nat Immunol. 2003;4:1191–1198. doi: 10.1038/ni1009. [DOI] [PubMed] [Google Scholar]
- Mitchell T, Kappler J, Marrack P. Bystander virus infection prolongs activated T cell survival. J Immunol. 1999;162:4527–4535. [PubMed] [Google Scholar]
- Zhang N, He YW. The antiapoptotic protein Bcl-xL is dispensable for the development of effector and memory T lymphocytes. J Immunol. 2005;174:6967–6973. doi: 10.4049/jimmunol.174.11.6967. [DOI] [PubMed] [Google Scholar]
- Tripathi P, Kurtulus S, Wojciechowski S, Sholl A, Hoebe K, Morris SC, et al. STAT5 is critical to maintain effector CD8+ T cell responses. J Immunol. 2010;185:2116–2124. doi: 10.4049/jimmunol.1000842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hildeman D, Jorgensen T, Kappler J, Marrack P. Apoptosis and the homeostatic control of immune responses. Curr Opin Immunol. 2007;19:516–521. doi: 10.1016/j.coi.2007.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunkle A, Dzhagalov I, He YW. Cytokine-dependent and cytokine-independent roles for Mcl-1: genetic evidence for multiple mechanisms by which Mcl-1 promotes survival in primary T lymphocytes. Cell Death Dis. 2011;2:e214. doi: 10.1038/cddis.2011.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wojciechowski S, Tripathi P, Bourdeau T, Acero L, Grimes HL, Katz JD, et al. Bim/Bcl-2 balance is critical for maintaining naive and memory T cell homeostasis. J Exp Med. 2007;204:1665–1675. doi: 10.1084/jem.20070618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boise LH, Minn AJ, Noel PJ, June CH, Accavitti MA, Lindsten T, et al. CD28 costimulation can promote T cell survival by enhancing the expression of Bcl-XL. Immunity. 1995;3:87–98. doi: 10.1016/1074-7613(95)90161-2. [DOI] [PubMed] [Google Scholar]
- Hildeman DA, Mitchell T, Aronow B, Wojciechowski S, Kappler J, Marrack P. Control of Bcl-2 expression by reactive oxygen species. Proc Natl Acad Sci USA. 2003;100:15035–15040. doi: 10.1073/pnas.1936213100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dzhagalov I, Dunkle A, He YW. The anti-apoptotic Bcl-2 family member Mcl-1 promotes T lymphocyte survival at multiple stages. J Immunol. 2008;181:521–528. doi: 10.4049/jimmunol.181.1.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rinkenberger JL, Horning S, Klocke B, Roth K, Korsmeyer SJ. Mcl-1 deficiency results in peri-implantation embryonic lethality. Genes Dev. 2000;14:23–27. [PMC free article] [PubMed] [Google Scholar]
- Takeuchi O, Fisher J, Suh H, Harada H, Malynn BA, Korsmeyer SJ. Essential role of BAX,BAK in B cell homeostasis and prevention of autoimmune disease. Proc Natl Acad Sci USA. 2005;102:11272–11277. doi: 10.1073/pnas.0504783102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chougnet CA, Tripathi P, Lages CS, Raynor J, Sholl A, Fink P, et al. A major role for Bim in regulatory T cell homeostasis. J Immunol. 2011;186:156–163. doi: 10.4049/jimmunol.1001505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perciavalle RM, Stewart DP, Koss B, Lynch J, Milasta S, Bathina M, et al. Anti-apoptotic MCL-1 localizes to the mitochondrial matrix and couples mitochondrial fusion to respiration. Nat Cell Biol. 2012;14:575–583. doi: 10.1038/ncb2488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L, Willis SN, Wei A, Smith BJ, Fletcher JI, Hinds MG, et al. Differential targeting of prosurvival Bcl-2 proteins by their BH3-only ligands allows complementary apoptotic function. Mol Cell. 2005;17:393–403. doi: 10.1016/j.molcel.2004.12.030. [DOI] [PubMed] [Google Scholar]
- Oltersdorf T, Elmore SW, Shoemaker AR, Armstrong RC, Augeri DJ, Belli BA, et al. An inhibitor of Bcl-2 family proteins induces regression of solid tumours. Nature. 2005;435:677–681. doi: 10.1038/nature03579. [DOI] [PubMed] [Google Scholar]
- Han J, Goldstein LA, Gastman BR, Froelich CJ, Yin XM, Rabinowich H. Degradation of Mcl-1 by granzyme B: implications for Bim-mediated mitochondrial apoptotic events. J Biol Chem. 2004;279:22020–22029. doi: 10.1074/jbc.M313234200. [DOI] [PubMed] [Google Scholar]
- Jamil S, Wang SW, Bondy L, Mojtabavi S, Duronio V. Prevention of cytokine withdrawal-induced apoptosis by Mcl-1 requires interaction between Mcl-1 and Bim. Biochem Cell Biol. 2010;88:809–818. doi: 10.1139/o10-004. [DOI] [PubMed] [Google Scholar]
- Wei MC, Lindsten T, Mootha VK, Weiler S, Gross A, Ashiya M, et al. tBID, a membrane-targeted death ligand, oligomerizes BAK to release cytochrome c. Genes Dev. 2000;14:2060–2071. [PMC free article] [PubMed] [Google Scholar]
- Willis SN, Chen L, Dewson G, Wei A, Naik E, Fletcher JI, et al. Proapoptotic Bak is sequestered by Mcl-1 and Bcl-xL, but not Bcl-2, until displaced by BH3-only proteins. Genes Dev. 2005;19:1294–1305. doi: 10.1101/gad.1304105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong Q, Gao W, Du F, Wang X. Mule/ARF-BP1, a BH3-only E3 ubiquitin ligase, catalyzes the polyubiquitination of Mcl-1 and regulates apoptosis. Cell. 2005;121:1085–1095. doi: 10.1016/j.cell.2005.06.009. [DOI] [PubMed] [Google Scholar]
- Sengupta S, Jayaraman P, Chilton PM, Casella CR, Mitchell TC. Unrestrained glycogen synthase kinase-3 beta activity leads to activated T cell death and can be inhibited by natural adjuvant. J Immunol. 2007;178:6083–6091. doi: 10.4049/jimmunol.178.10.6083. [DOI] [PubMed] [Google Scholar]
- Stewart DP, Koss B, Bathina M, Perciavalle RM, Bisanz K, Opferman JT. Ubiquitin-independent degradation of antiapoptotic MCL-1. Mol Cell Biol. 2010;30:3099–3110. doi: 10.1128/MCB.01266-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konopleva M, Contractor R, Tsao T, Samudio I, Ruvolo PP, Kitada S, et al. Mechanisms of apoptosis sensitivity and resistance to the BH3 mimetic ABT-737 in acute myeloid leukemia. Cancer Cell. 2006;10:375–388. doi: 10.1016/j.ccr.2006.10.006. [DOI] [PubMed] [Google Scholar]
- van Delft MF, Wei AH, Mason KD, Vandenberg CJ, Chen L, Czabotar PE, et al. The BH3 mimetic ABT-737 targets selective Bcl-2 proteins and efficiently induces apoptosis via Bak/Bax if Mcl-1 is neutralized. Cancer Cell. 2006;10:389–399. doi: 10.1016/j.ccr.2006.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bardwell PD, Gu J, McCarthy D, Wallace C, Bryant S, Goess C, et al. The Bcl-2 family antagonist ABT-737 significantly inhibits multiple animal models of autoimmunity. J Immunol. 2009;182:7482–7489. doi: 10.4049/jimmunol.0802813. [DOI] [PubMed] [Google Scholar]
- Carrington EM, Vikstrom IB, Light A, Sutherland RM, Londrigan SL, Mason KD, et al. BH3 mimetics antagonizing restricted prosurvival Bcl-2 proteins represent another class of selective immune modulatory drugs. Proc Natl Acad Sci USA. 2010;107:10967–10971. doi: 10.1073/pnas.1005256107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenton RG, Marrack P, Kappler JW, Kanagawa O, Seidman JG. Isotypic exclusion of gamma delta T cell receptors in transgenic mice bearing a rearranged beta-chain gene. Science. 1988;241:1089–1092. doi: 10.1126/science.2970670. [DOI] [PubMed] [Google Scholar]
- Hildeman D, Yanez D, Pederson K, Havighurst T, Muller D. Vaccination against persistent viral infection exacerbates CD4+ T-cell-mediated immunopathological disease. J Virol. 1997;71:9672–9678. doi: 10.1128/jvi.71.12.9672-9678.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell TC, Hildeman D, Kedl RM, Teague TK, Schaefer BC, White J, et al. Immunological adjuvants promote activated T cell survival via induction of Bcl-3. Nat Immunol. 2001;2:397–402. doi: 10.1038/87692. [DOI] [PubMed] [Google Scholar]
- Crawford F, Kozono H, White J, Marrack P, Kappler J. Detection of antigen-specific T cells with multivalent soluble class II MHC covalent peptide complexes. Immunity. 1998;8:675–682. doi: 10.1016/s1074-7613(00)80572-5. [DOI] [PubMed] [Google Scholar]
- Rees W, Bender J, Teague TK, Kedl RM, Crawford F, Marrack P, et al. An inverse relationship between T cell receptor affinity and antigen dose during CD4(+) T cell responses in vivo and in vitro. Proc Natl Acad Sci USA. 1999;96:9781–9786. doi: 10.1073/pnas.96.17.9781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altman JD, Moss PA, Goulder PJ, Barouch DH, McHeyzer-Williams MG, Bell JI, et al. Phenotypic analysis of antigen-specific T lymphocytes. Science. 1996;274:94–96. [PubMed] [Google Scholar]
- Fuller MJ, Zajac AJ. Ablation of CD8 and CD4 T cell responses by high viral loads. J Immunol. 2003;170:477–486. doi: 10.4049/jimmunol.170.1.477. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.