Abstract
Non-proliferating oocytes within avascular regions of the ovary are exquisitely susceptible to chemotherapy. Early menopause and sterility are unintended consequences of chemotherapy, and efforts to understand the oocyte apoptotic pathway may provide new targets for mitigating this outcome. Recently, the c-Abl kinase inhibitor imatinib mesylate (imatinib) has become the focus of research as a fertoprotective drug against cisplatin. However, the mechanism by which imatinib protects oocytes is not fully understood, and reports of the drug's efficacy have been contradictory. Using in vitro culture and subrenal grafting of mouse ovaries, we demonstrated that imatinib inhibits the cisplatin-induced apoptosis of oocytes within primordial follicles. We found that, before apoptosis, cisplatin induces c-Abl and TAp73 expression in the oocyte. Oocytes undergoing apoptosis showed downregulation of TAp63 and upregulation of Bax. While imatinib was unable to block cisplatin-induced DNA damage and damage response, such as the upregulation of p53, imatinib inhibited the cisplatin-induced nuclear accumulation of c-Abl/TAp73 and the subsequent downregulation of TAp63 and upregulation of Bax, thereby abrogating oocyte cell death. Surprisingly, the conditional deletion of Trp63, but not ΔNp63, in oocytes inhibited apoptosis, as well as the accumulation of c-Abl and TAp73 caused by cisplatin. These data suggest that TAp63 is the master regulator of cisplatin-induced oocyte death. The expression kinetics of TAp63, c-Abl and TAp73 suggest that cisplatin activates TAp63-dependent expression of c-Abl and TAp73 and, in turn, the activation of TAp73 by c-Abl-induced BAX expression. Our findings indicate that imatinib protects oocytes from cisplatin-induced cell death by inhibiting c-Abl kinase, which would otherwise activate TAp73-BAX-mediated apoptosis. Thus, imatinib and other c-Abl kinase inhibitors provide an intriguing new way to halt cisplatin-induced oocyte death in early follicles and perhaps conserve the endocrine function of the ovary against chemotherapy.
Keywords: ovarian follicles, cisplatin, imatinib, c-Abl, TAp63, TAp73
Earlier detection of cancer coupled with improved treatment options has increased the number of cancer survivors. As the number of cancer survivors increases, so do concerns regarding their post-treatment quality-of-life. One of the most serious consequences of radiation and chemotherapy is the off-target effects on germ cells.1, 2 In women, the ‘ovarian reserve' represents all available oocytes for the future fertility and endocrine health. As immature oocytes within ovarian reserve are highly sensitive to cancer therapies, radiation and chemotherapy with alkylating agents increase the likelihood of premature ovarian failure,3, 4 which has physical consequences such as hypoestrogenism and the long-term sequelae of sex steroid deficiency, as well as psychological consequences.5, 6 There is a significant need for preventive approaches that can protect the ovarian reserve against cancer therapy-induced premature ovarian failure, and preserve future fertility and endocrine function.2
One promising approach is the use of neoadjuvant fertoprotective agents that guard the ovarian reserve when administered concurrently with either radiation7 or chemotherapies.8 For example, sphingosine-1-phosphate was shown to protect small follicles and preserve fertility against radiation in primates, allowing them to give birth to healthy offspring.7 Similar results were obtained in mice treated with cisplatin using imatinib mesylate (imatinib), which protected immature follicles, presumably by inhibiting the function of tyrosine kinase c-Abl.8 Although the fertoprotective effect of imatinib and other treatments remains to be confirmed,9, 10 ‘neoadjuvant' therapies may still provide effective options to protect both fertility and endocrine function in women before and/or during cancer therapy.11 To develop safe and effective therapies, the mechanisms by which cancer therapies kill oocytes in immature follicles must be elucidated.
Apoptosis of damaged germ cells appears to be controlled by p53 orthologs throughout the animal kingdom.12, 13 In the starlet sea anemone, UV-induced germ cell death requires the function of the p53 ortholog nvp63.14 DNA damage-induced germ cell death in the nematode is also regulated by a p53 ortholog, cep-1.15, 16 In the fruit fly, a p53 ortholog is essential to eliminate unnecessary germ cells via apoptosis.17 The mammalian p53 family consists of three paralogs, p53, p63 and p73 (encoded by TP53/Trp53, TP63/Trp63 and TP73/Trp73 in human/mouse),18 and all three p53 family members appear to have a role in DNA damage-induced apoptosis of male germ cells. Stress/DNA damage-induced germ cell apoptosis is attenuated in the testis of Trp53-deficient19, 20 and Trp63-deficient mice.21 The c-Abl/p73 pathway appears to be activated in male germ cells during etoposide-induced apoptosis.22 Unlike in testis, there is evidence supporting a role for TAp63 but not p53 or TAp73 in oocyte apoptosis.23 In the mouse ovary, TAp63, the p63 isoform that contains a p53-like transactivation domain, is constitutively expressed in oocytes.24, 25, 26 Oocytes of TAp63-deficient mice were found to be insensitive to γ-irradiation-induced apoptosis, indicating an essential role for TAp63 in the ablation of damaged oocytes.25, 27 In contrast, p53 is dispensable for either doxorubicin- or radiation-induced apoptosis in oocytes.25, 28 In addition, TAp73 appears to prevent rather than to facilitate apoptosis in immature oocytes as ovaries of TAp73-deficient mice have a reduced number of primordial and primary follicles.29 On the basis of these observations, TAp63 has been proposed to regulate cisplatin-induced apoptosis in oocytes,8 although the necessity of TAp63 in this process has not yet been functionally demonstrated.
To study how imatinib can preserve immature follicles against cisplatin, we developed an assay system that consists of in vitro culture and subsequent subrenal grafting of ovaries from postnatal day 5 (P5) mice. Primordial and primary follicles, which are the predominant structure in P5 mouse ovaries, are highly sensitive to radiation and chemotherapies; thus, this age is an ideal time which to study the mechanism of immature follicle death induced by genotoxic cancer therapy. We confirmed the protective effect of imatinib against cisplatin-induced loss of ovarian reserve, and by generating an oocyte-specific Trp63 conditional knockout mice, we demonstrated – for the first time – that TAp63 is necessary for cisplatin-induced oocyte apoptosis. During apoptosis, oocytes express p53 and TAp73, as well as c-Abl in a Trp63-dependent manner, suggesting that cisplatin induces apoptosis of oocytes in primordial follicles by triggering a signaling network involving all three p53 family members, which is controlled by TAp63.
Results
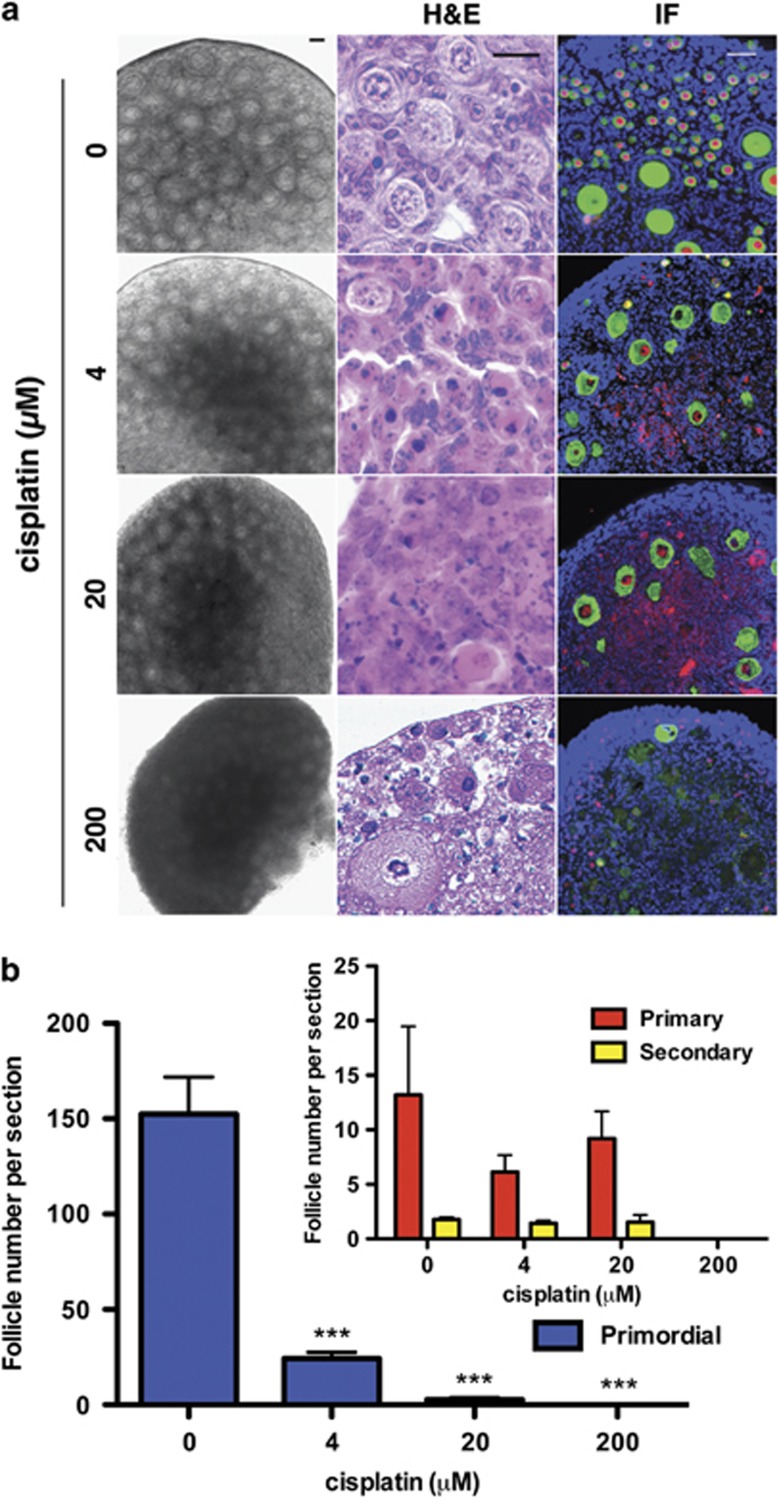
Dose-dependent effect of cisplatin on ovarian follicles in organ culture
P5 mouse ovaries were cultured with various doses of cisplatin (4–200 μℳ). After 4 days in culture, dose-dependent damage by cisplatin was observed as dark condensed areas in the centers of oocytes by phase contrast microscopy (Figure 1a). At 20 μℳ or higher, cisplatin killed most follicles, as well as stromal cells as seen in H&E-stained sections. In contrast, the damage caused by 4 μℳ cisplatin was mostly restricted to the primordial follicles (Figures 1a and b), and reduced the number of primordial follicles to ∼10% of that in control ovaries (Figure 1b). As 4 μℳ cisplatin is comparable to the plasma concentrations observed in patients receiving cisplatin,30 we used this concentration in subsequent experiments.
Figure 1.
Cisplatin damages cultured ovaries in a dose-dependent manner. (a) Analysis of ovarian follicles. The damaging effect of cisplatin was observed in the ovary as dark, condensed areas in the phase contrast bright field image. In H&E-stained sections, severe damage of somatic (both granulosa and stromal) cells and secondary follicles was observed at 20 μℳ and 200 μℳ cisplatin, whereas damage was specific to primordial and primary follicles at 4 μℳ cisplatin. Loss of follicles was clearly demonstrated by immunofluorescence assays for oocyte markers TAp63 (nucleus, red) and MSY2 (cytoplasm, green). Nuclear TAp63, which marks oocytes within immature follicles, was significantly reduced in cisplatin-treated groups. Loss of secondary follicles, indicated by the loss of MSY2 staining, was prominent in the 200 μℳ cisplatin group. Scale bars=25 μm. Blue=DAPI. (b) Quantification of follicle loss. Follicle numbers at 4 days are shown as the average number of follicles per section (n=4). Bars indicate average number±S.D.. The number of primordial follicles (blue bars) was significantly reduced in all cisplatin-treated groups. There was no statistically significant difference in the number of primary (red bars) and secondary (yellow bars) follicles with 0, 4 and 20 μℳ cisplatin, most likely due to the small population of these follicle types at this age. However, both primary and secondary follicles completely disappeared with 200 μℳ cisplatin. ***P<0.001 compared with the untreated control group
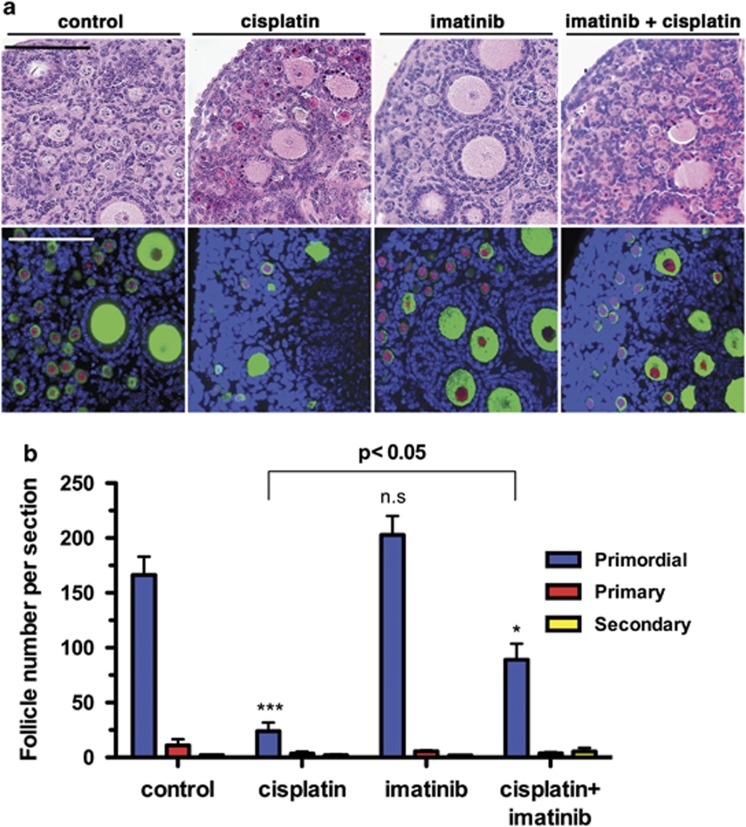
Imatinib prevents cisplatin-induced loss of primordial follicles in organ culture
Next, the effect of imatinib was tested between 1–100 μℳ concentrations to reflect the range of plasma concentrations observed in patients receiving imatinib treatment.31 As imatinib was toxic at higher concentrations (Supplementary Figure S1), 5 μℳ imatinib was used in subsequent experiments. In cisplatin-treated ovaries, oocyte death in primordial follicles was prominent in H&E-stained sections and was effectively repressed by cotreatment with 5 μℳ imatinib (Figure 2a). The protective effect of imatinib on primordial follicles was better visualized with immunofluorescent detection of MSY2 (green) and TAp63 (red) in the oocyte cytoplasm and nuclei, respectively (Figure 2a). Coadministration of imatinib with cisplatin resulted in significant retention of primordial follicles. While ∼10% of primordial follicles remained after 4 days of treatment in the cisplatin group, ∼50% of primordial follicles survived in the cisplatin+imatinib group (Figure 2b).
Figure 2.
Imatinib prevents cisplatin-induced loss of follicles in the ovarian reserve. (a) The protective effect of imatinib against cisplatin was tested in ovarian organ culture. A volume of 5 μℳ imatinib was not toxic to the ovary (see Supplementary Figure S1 for dose response). In H&E-stained sections, cisplatin-treated ovaries contained a high number of damaged follicles with dark pink cytoplasm and condensed nuclei, whereas most primordial follicles in the cisplatin+imatinib-treated ovaries appeared healthy. The fertoprotective effect of imatinib on immature follicles was clearly observed by the significant increase in TAp63-positive (red) and MSY2-positive (green) follicles present in cisplatin+imatinib-treated ovaries relative to cisplatin-treated ovaries. Scale bar=100 μm. Blue=DAPI. (b) Average follicle number per section (four ovaries/group) was reported as mean±S.D. (n=3). There was no significant difference between the number of primordial follicles in the control and imatinib groups (n.s.). There was a significant difference in the number of primordial follicles between the control, cisplatin and cisplatin+imatinib-treated groups. *P<0.05, ***P<0.001 compared with the untreated control group
Although primordial follicles survived for 4 days in vitro with cisplatin+imatinib, it is possible that the oocytes in these follicles would have eventually undergone apoptosis because of irreparable DNA damage. To examine the long-term effect of cisplatin with or without imatinib on ovarian follicles, after 4 days in culture, mouse ovaries were transplanted under the kidney capsule of a syngenic female host mouse and were grown for an additional 14 days in vivo. To allow oocytes to repair DNA damage before grafting, ovaries were cultured with cisplatin for 24 h, after which they were cultured in control or imatinib-containing medium for an additional 3 days (Supplementary Figure S2). Although follicles were visible under the bright field microscope before grafting, no tissue was present after 14 days of in vivo growth in the cisplatin-only treatment group. This result indicates that the damaging effect of cisplatin persisted within the ovary even after removal of the drug. In contrast, ovaries containing primordial, primary and secondary follicles were recovered after 14 days of in vivo growth from each of the other groups (n=4, per treatment; Figure 3). Although the overall size of ovarian tissues in the cisplatin+imatinib group was observably smaller than those of the control and imatinib groups, all tissues contained primordial follicles (n=4, Figure 3 inset, yellow arrow). These findings support the fertoprotective efficacy of imatinib against acute and chronic effects of cisplatin.
Figure 3.
Imatinib protects ovaries against detrimental effects of cisplatin. Subrenal grafting assay to assess the long-term effects of cisplatin and imatinib on the ovary. Ovaries were cultured in vitro for 4 days and then grafted under the subrenal capsule of prepubertal (3-week-old) ovariectomized female C57BL/6j mice (four ovaries/group) (see Supplementary Figure S2 for treatment schedule). Before grafting, ovaries from the cisplatin and cisplatin+imatinib groups were smaller compared with those of other groups, though bright field microscopy revealed the presence of follicles in all groups. Two weeks after grafting, ovarian transplants significantly increased in size in all groups except the cisplatin-treated group. Although traces of degraded tissue were observed in the cisplatin-treated group, no ovarian tissue was recovered. H&E staining showed that all ovarian transplants in control, imatinib and cisplatin+imatinib groups contained primordial, primary, secondary and antral follicles (four ovaries/group). High power images of primordial follicles in the cisplatin+imatinib group are shown in the inset (Scale bar=25 μm). For bright field and H&E images, scale bar=100 μm; for kidney images, scale bar=2 mm
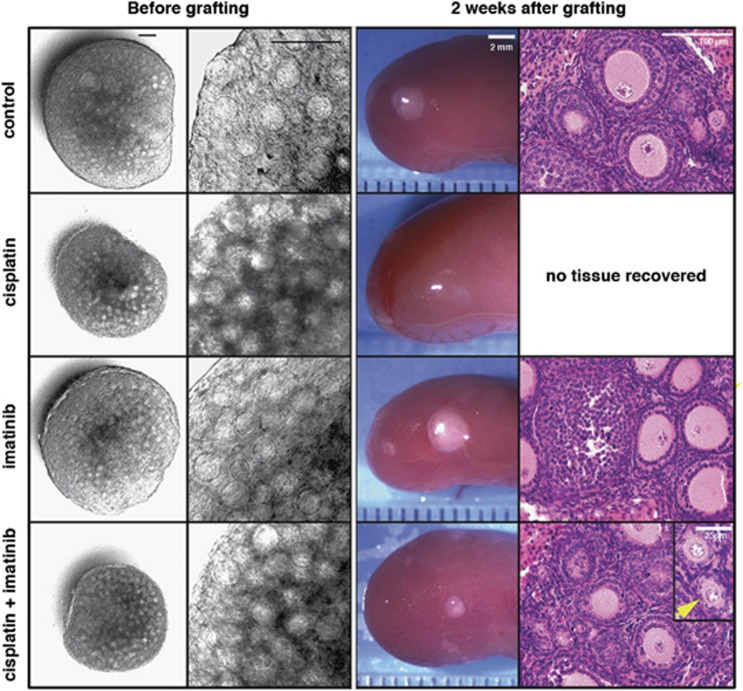
Imatinib does not prevent platinum (Pt)-DNA adducts and DNA damage in oocytes
To elucidate the signaling pathways involved in cisplatin-induced follicle depletion and its prevention by imatinib, immunofluorescence analyses were performed on ovaries cultured for 48 h, the time point at which ovaries cultured with cisplatin still contain a substantial number of primordial follicles (Figure 4). Cisplatin-activated apoptotic signaling in oocytes was detected by the presence of known mediators of apoptosis, Bax,28 active caspase-332 and cleaved PARP33, 34 (Figure 4a). Cotreatment with imatinib, attenuated the expression of these cisplatin-induced apoptotic signaling proteins (Figure 4a). Thus, cisplatin causes primordial follicle loss through the apoptosis of oocytes and imatinib protects the ovarian reserve by inhibiting the activation of cisplatin-induced apoptosis.
Figure 4.
Imatinib blocks the apoptotic signaling pathway without affecting the DNA damage response. (a) Immunofluorescent staining of Bax, caspase-3 (active form), and PARP (cleaved form) (green) in control, cisplatin and cisplatin+imatinib-treated groups after culturing for 48 h in vitro. All three proteins were present in the cisplatin group, and their levels were reduced with imatinib treatment. Inserts indicate small follicles including primordial follicles observed at 60x. (b) Immunofluorescent staining of PtCG, pATM/ATR substrate and γH2AX (green) in the control, cisplatin, and cisplatin+imatinib-treated groups after culturing for 48 h in vitro. PtCG and γH2AX show punctate signals in oocyte nuclei. Imatinib did not change the expression patterns of these two proteins or the expression of pATM/ATR substrate. Scale bar=25 μm. Blue=DAPI
Immunofluorescence was performed to detect the platinum-DNA adduct cis-Pt(NH3)2d(pCpG) [Pt(CG)]35 and DNA damage response proteins. The signal for Pt(CG) showed equal intensity in the oocyte nuclei of the large follicles remaining in the cisplatin group and the primordial follicles in the cisplatin+imatinib group, but not in the control group (Figure 4b). Likewise, markers for the DNA damage response (γH2AX and phosphorylated ATM/ATR substrate) were detected at equal levels in the cisplatin and cisplatin+imatinib groups but not in the control group (Figure 4b). Thus, while imatinib protects the primordial follicles of the ovarian reserve from apoptosis, it does not inhibit DNA double-stranded breaks or damage response mechanisms.
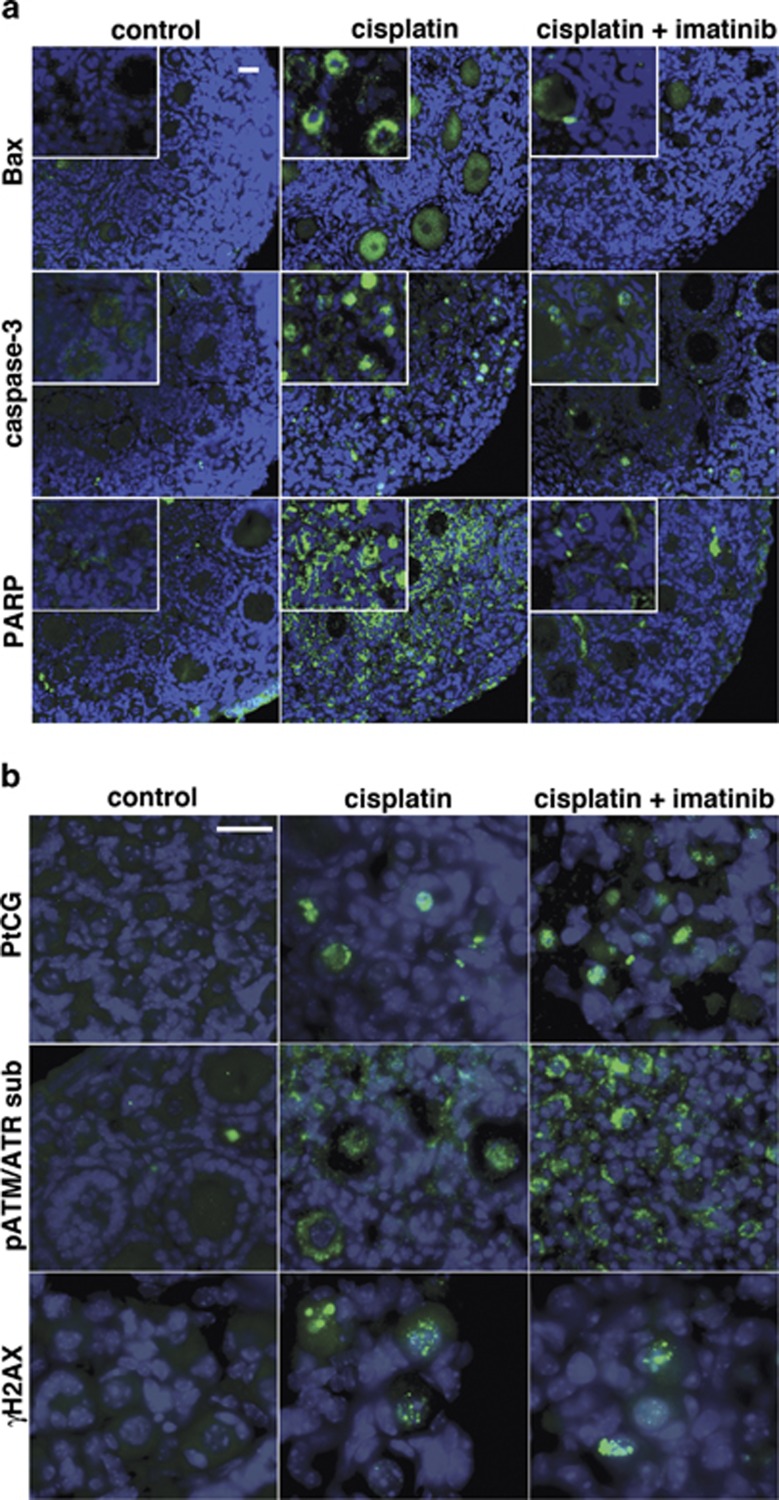
Upregulation of p53 family proteins and c-Abl by cisplatin and its inhibition by imatinib
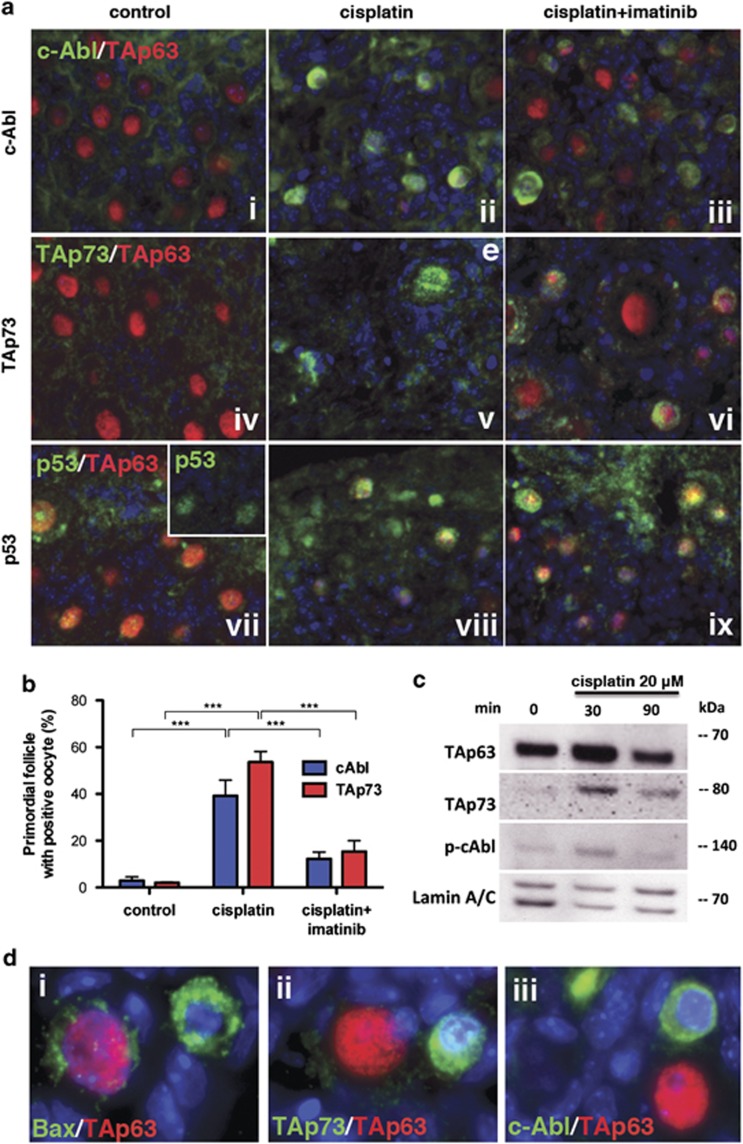
To identify mediators of cisplatin-induced apoptosis in oocytes, expression of p53 family members (p53, p63 and p73) and their putative activator, c-Abl, were examined. Oocytes constitutively express TAp63 (Figure 5ai, iv and vii) in the nucleus in primordial to early secondary follicles; TAp73 is only expressed in the nucleus of these follicles upon cisplatin treatment (Figure 5av and vi). ΔNp63 and ΔNp73 were not detected in P5 mouse ovaries in situ or in culture regardless of the treatment (Supplementary Figure S4xi and iv, respectively). While p53 was weakly detected (Figure 5avii inset), and the signals for c-Abl and TAp73 were almost undetectable (Figure 5ai and iv) in the control group, 48 h of cisplatin treatment induced high expression of c-Abl, TAp73 and p53 in both the cytoplasm and nuclei of oocytes within primordial and primary follicles (Figure 5aii, v and viii, respectively). Expression of TAp73 and c-Abl was detected in ∼50% of oocytes of primordial follicles (Figure 5b). This cisplatin-induced upregulation of c-Abl and TAp73 was significantly attenuated by imatinib (Figure 5aiii and vi, respectively); oocytes positive for TAp73 and c-Abl declined to ∼15% (Figure 5b). Short-term treatment of ovaries with 20 μℳ cisplatin showed nuclear accumulation by 30 min and subsequent downregulation of nuclear TAp63, TAp73 and c-Abl by 90 min (Figure 5c). Oocyte nuclear TAp63 was downregulated 48 h after treatment with 4 μℳ cisplatin, whereas TAp73 and c-Abl remained (Figure 5aiii, vi, and d ii and iii). Bax was detected primarily in the oocytes devoid of nuclear TAp63 (Figure 5di). The exclusive expression pattern of TAp63 versus TAp73/c-Abl/Bax suggests that TAp63 induces Bax via activation of TAp73 and c-Abl. Imatinib treatment inhibited both cisplatin-induced oocyte death and the downregulation of TAp63 (Figure 5aiii, vi and ix), suggesting that degradation of TAp63 is regulated by the kinase activity of c-Abl.
Figure 5.
Regulation of c-Abl and p53 family members by cisplatin and imatinib. (a) In the control group (i, iv, vii), most oocytes expressed only nuclear TAp63 (red) with some p53 staining (green, inset in vii). Cisplatin treatment (ii, v, viii) induced c-Abl, TAp73 and p53 signals in oocytes (green), with c-Abl and TAp73 present in the oocyte nuclei. With cisplatin treatment, the level of nuclear TAp63 was lower than in controls (red). In the cisplatin+imatinib group (iii, vi, ix), TAp63 levels were maintained in the nuclei of oocytes (red) and TAp73 signal was attenuated and limited to the cytoplasm. DAPI (blue), c-Abl, TAp73 and p53 (green), TAp63 (red), and overlay (yellow). (b) Percentage of primordial follicles with oocytes stained for c-Abl and TAp73 at 48 h was determined by counting positive- and negative- oocytes on DAB-stained sections (three ovaries/group). Both c-Abl and TAp73 were essentially undetectable in the untreated control group. In the cisplatin-treated group, >50% of primordial follicles were positive for c-Abl and TAp73; <20% were positive in the cisplatin+imatinib-treated group. Bars indicate average number±S.D. (n=3). ***P<0.001 for the comparisons indicated by the brackets. (c) Immunoblot analysis of nuclear TAp63, TAp73 and phosphpo-c-Abl levels. The expression of TAp63 in ovarian nuclear extract was upregulated within 30 min after treatment with 20 μℳ cisplatin and then downregulated at 90 min. TAp73 and p-c-Abl showed similar expression patterns as TAp63. Lamin A/C was used as a loading control. (d) Differential expression of TAp63 (red) versus Bax, TAp73, and c-Abl (green) in the oocyte nucleus when the ovaries were cultured for 48 h with cisplatin in vitro. Oocytes undergoing apoptosis (positive for Bax, i) were negative for TAp63 but retained expression of TAp73 (ii) and c-Abl (iii), as indicated by the lack of yellow color in the overlay
TAp63 is the master regulator of cisplatin-induced oocyte death
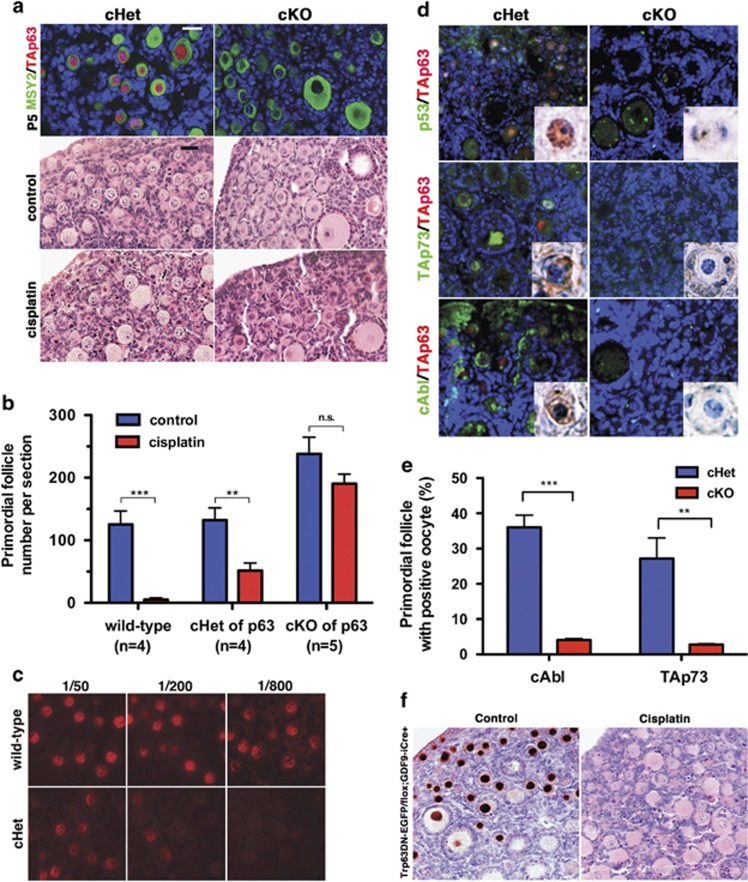
To determine the function of TAp63 in cisplatin-induced follicle loss, p63 cKO (conditional knockout) mice were generated using GDF9-iCre mice (Supplementary Figure S3). At P5, TAp63 protein was absent in the oocytes of p63 cKO (Trp63floxN/floxN; GDF9-iCre) mice, while MSY2 (Figure 6a) was present in the cytoplasm of oocytes in both p63 cKO and cHet (conditional heterozygotes, Trp63wt/floxN; GDF9-iCre) ovaries (Figure 6a). The sensitivity to cisplatin-induced oocyte death was compared between wild-type control (Trp63wt/wt; GDF9-iCre), p63 cHet and p63 cKO ovaries. After 4 days in culture, cisplatin destroyed 95% of primordial follicles in the wild-type ovaries. In contrast, the number of primordial follicles was no different in the control and cisplatin-treated p63 cKO ovaries (Figure 6b). p63 cHet ovaries demonstrated an intermediate phenotype; the number of primordial follicles in cisplatin-treated p63 cHet ovaries was significantly higher than wild-type ovaries (P<0.05) and lower than p63 cKO ovaries (P<0.001; Figure 6b). These data provide the first functional evidence for an essential role of TAp63 in the cisplatin-induced loss of immature follicles. Interestingly, p63 cKO ovaries contained significantly higher numbers of follicles than those of wild-type and cHet ovaries in the untreated control group (P<0.001), suggesting that TAp63 may also control the selective loss of oocytes that occurs in the postnatal period (Figure 6b).36 While immunofluorescence is difficult to quantitate, serial dilution immunofluorescence analysis indicated that the level of TAp63 in oocytes was significantly lower in p63 cHet compared with that of wild-type ovaries (Figure 6c). The degree of oocyte loss correlated with the copy number of the Trp63 gene and the expression level of TAp63, suggesting that the level of TAp63 determines the sensitivity of oocytes to DNA damage-induced apoptosis.
Figure 6.
TAp63 is essential for cisplatin-induced oocyte death. (a) Immunofluorescence assay for oocyte markers MSY2 (cytoplasm, green) and TAp63 (nucleus, red) confirmed the loss of TAp63 protein in oocytes in conditional knockout (cKO) ovaries at P5 when ovaries were cultured for 96 h. Blue=DAPI. In H&E-stained sections, small follicles were mostly intact in p63 cKO ovaries, whereas substantial numbers of dead follicles were detected in p63 cHet ovaries treated with cisplatin. Scale bars=25 μm. (b) The average number of primordial follicles per section was determined in p63 wild-type (n=4), cHet (n=4) and cKO (n=5) ovaries cultured with/without cisplatin. p63 cKO ovaries contained significantly higher numbers of primordial follicles compared with those of wild-type and cHet ovaries in the control groups. The survival rate of primordial follicles (average follicle number of the cisplatin group divided by that of the control group) was significantly higher in the following order: cKO (93.14%±37.72) >cHet (28.11%±19.10) >wt (5.98%±9.75). Bars indicate average number±S.D.. **P<0.01, ***P<0.001, n.s.=not significant for the comparisons indicated by the brackets. (c) Expression of TAp63 in wild-type and p63 cHet mice. Immunofluorescence staining was performed to assess the expression level of TAp63 (red) by Trp63 copy number, using different concentrations of anti-p63 antibody (4A4) from 1 : 50 to 1 : 800. While oocytes of wild-type (RosaTE/+; GDF9-iCre) mice showed a positive signal for TAp63 at 1 : 800, the signal for TAp63 was undetectable at the same antibody concentration in cHet oocytes, indicating a lower expression level. (d) Induction of p53, TAp73 and c-Abl (green) by cisplatin is TAp63-dependent. All panels show ovaries that were treated with cisplatin for 48 h. The induction of p53, TAp73 and c-Abl by cisplatin was notably reduced in p63 cKO ovaries compared with in those of cHet ovaries, indicating that TAp63 function is essential for induction of p53, TAp73 and c-Abl in response to cisplatin. All inserts are representative images of primordial follicles with DAB staining for each protein. (e) Percentage of primordial follicles with oocytes stained for c-Abl and TAp73 at 48 h was determined by counting positive and negative oocytes in cisplatin-treated ovaries on DAB-stained sections (three ovaries/group). p63 cKO showed positive signals for TAp73 and c-Abl in fewer than 5% of primordial follicles, whereas p63 cHet showed positive signals in ∼30% of primordial follicles. Bars indicate average number±S.D.. **P<0.01, ***P<0.001 for the comparisons indicated by the brackets. (f) Dispensability of ΔNp63 in cisplatin-induced oocyte death. ΔNp63 cKO ovaries were strongly positive for TAp63 (left panel; DAB staining with TAp63 on the control group), and sensitive for cisplatin-induced cell death of oocytes in primordial follicles (right panel; H&E staining on the cisplatin group). Thus, ΔNp63 is not required for cisplatin-induced oocyte death
Induction of p53, TAp73 and c-Abl by cisplatin was attenuated in the p63 cKO ovaries compared with wild-type and p63 cHet ovaries (Figures 6d and e, and inserts). In the cisplatin-treated group, the percentage of primordial follicle oocytes that were positive for TAp73 and c-Abl was significantly lower in cKO than cHet ovaries (P<0.01 and P<0.001, respectively). Although ΔNp63 was never detected (Supplementary Figure S4 xi), we examined whether ΔNp63 was required for apoptosis of oocytes by generating mice, in which ΔNp63 was specifically inactivated in oocytes. The ΔNp63 cKO carried a floxed allele and a ΔNp63-enhanced green fluorescent protein (EGFP) knock-in allele, in which the first exon of ΔNp63 was replaced by EGFP, and thus, only the TA isoform could be transcribed from this allele37 (Supplementary Figure S3). Cisplatin-induced apoptosis of oocytes in ΔNp63 cKO ovaries (Figure 6f), indicating that ΔNp63 is dispensable for cisplatin-induced oocyte death. Together, these observations demonstrate that the apoptosis of oocytes is regulated by a signaling network involving all three p53 family members and c-Abl, in which TAp63 acts as the master regulator (Figure 7).
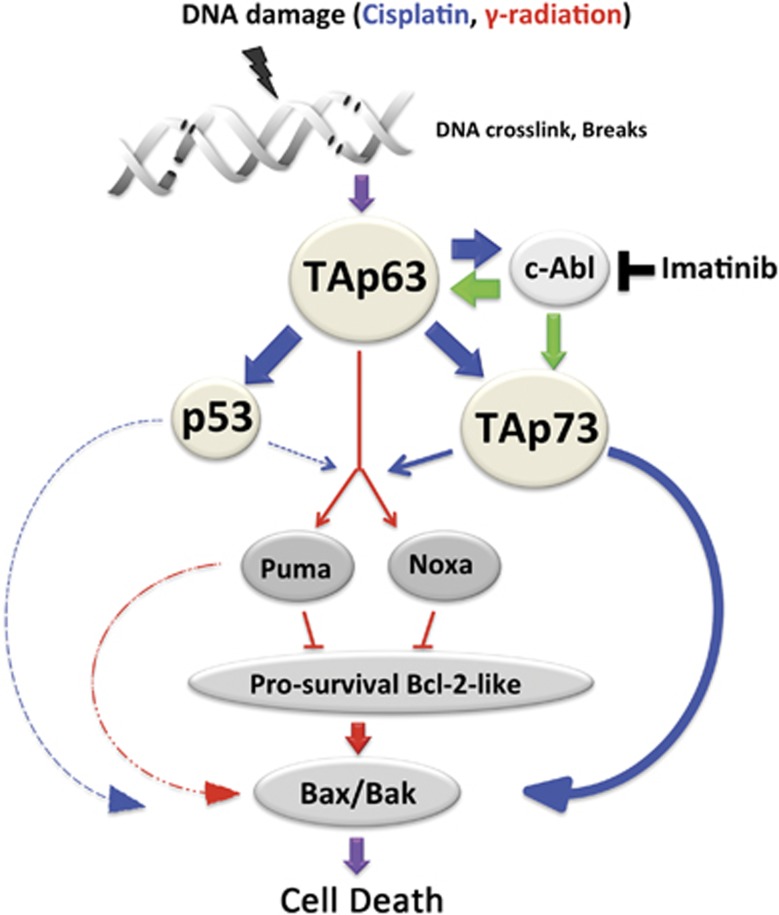
Figure 7.
Model for oocyte death regulated by p53 family members. All three p53 family members are involved in the apoptotic pathway in primordial follicle oocytes, with TAp63 playing a central role. DNA damage by γ-radiation activates signaling pathways through TAp63, resulting in the induction of Puma and Noxa and subsequent binding of PUMA and NOXA proteins to BAX/BAK as described in the recent report by Kerr et al. (red lines).23 DNA damage by cisplatin also activates TAp63, which results in upregulation of c-Abl. The kinase activity of c-Abl (green), which can be inhibited by imatinib, induces TAp63-dependent expression of TAp73 and subsequent degradation of TAp63. c-Abl may also activate TAp73 via phosphorylation; phospho-TAp73 then activates the apoptosis signaling pathway. p53 may have a minor or non-essential role in the activation of the apoptosis signaling pathway in response to cisplatin (shown as dotted line). The sequence of this signaling pathway and the consequences on primordial oocyte survival is profound and provides new insights into targets that may mitigate fertility loss in the cancer setting
Discussion
Previously, Gonfloni et al.8 reported that cotreatment with imatinib protects primordial follicles from cisplatin in P5 mice. On the basis of their finding of a strong correlation between the phosphorylation of TAp63 and the apoptosis of oocytes, it was proposed that DNA damage-induced apoptosis of oocytes via activation/phosphorylation of TAp63 by c-Abl and that imatinib blocked apoptosis via inhibition of c-Abl. However, the fertoprotective effect of imatinib against cisplatin was questioned in another study by Kerr et al., and remains controversial.9, 10 We recognize that there are subtle differences in study designs including in vitro versus in vivo treatment regiments, that platinum drugs and their activation of the DNA repair pathways in the oocyte may differ from pathways activated after treatment with doxorubicin or cyclophosphamide or other agents. Our studies are focused narrowly on the p63 pathway to specifically interrogate a linear gene effector pathway involved in oocyte loss in response to platinum adduct damage. This study, in partnership with the others that have been published, create a new paradigm, in which our twin goals of understanding oocyte biology and mitigating iatrogenic damage, can be more effectively studied.
In the current study, we have confirmed the fertoprotective effect of imatinib against cisplatin in primordial follicles, utilizing a novel system of in vitro organ culture and subrenal grafting. Through the conditional deletion of Trp63 in oocytes, we also established an essential role for TAp63 in the apoptosis of oocytes induced by cisplatin. Surprisingly, and perhaps important to the current controversy and future studies, loss of TAp63 function attenuated the upregulation of p53 and TAp73, as well as c-Abl, by cisplatin. This result demonstrates the role of TAp63 as a master regulator of the p53 family members in cisplatin-induced oocyte death (Figure 7). In addition, we found that the gene dose of Trp63 correlates with the expression level of TAp63 and the sensitivity of oocytes to cisplatin (Figure 6b). Therefore, the high and constitutive expression of TAp63 in oocytes within dormant primordial follicles may explain why these follicles are particularly sensitive to genotoxic insult. The expression patterns of TAp73 and Bax suggest that TAp73 is the immediate regulator of apoptotic signaling and that TAp63 activates apoptosis via TAp73 upregulation. In this model, TAp63 is degraded after transactivation of its target genes. While p53 is also upregulated by cisplatin in a TAp63-dependent manner, its role in cisplatin-induced apoptosis remains unclear. One possibility is that p53 and TAp73 redundantly activate transcription of Bax, which is a well-established transcriptional target of p5338 (Figure 7).
Although all three p53 family members are known substrates of c-Abl kinase, it is not clear whether TAp73 and TAp63 are direct targets of c-Abl, and whether c-Abl activity is important for localization or stability of these proteins. Imatinib-rescue of primordial follicles from cisplatin-induced death also inhibited the upregulation of TAp73 and downregulation of TAp63 seen with cisplatin treatment, suggesting that these events are regulated by c-Abl activity (Figure 7). Meanwhile, imatinib failed to block the upregulation of p53 by cisplatin, which requires the function of TAp63. Thus, we propose that TAp63 induces p53 independent of c-Abl, whereas the upregulation/activation of TAp73 depends on c-Abl kinase activity.
Recently, Kerr et al.23 reported that γ-irradiation leads to apoptosis of primordial follicles through the transcriptional induction of Puma and Noxa by TAp63, and subsequent activation of NOXA-BAX/BAK. Mice lacking Puma or both Puma and Noxa were resistant to γ-irradiation-induced oocyte death, and produced healthy offspring. Furthermore, Puma was a direct transcriptional target of TAp63. Thus, they concluded that a signaling pathway of TAp63-Puma/Noxa-Bax/Bak was involved in oocyte death after DNA damage. Here, our report extends this molecular mechanism and suggests that TAp73 is a mediator of this pathway between TAp63 and Bax/Bak (Figure 7). In this context, TAp73 may directly regulate transcription of Bax or indirectly activate BAX/BAK through the activation of PUMA/NOXA or transcription of Puma/Noxa. The signaling pathways involved in DNA damage-induced oocyte apoptosis are emerging. Additional studies will clarify the timing of events that can be manipulated to protect the primordial follicle pool from genotoxic insult.
The three members of the mammalian p53 family evolved from a common ancestral protein as a result of two gene duplication events.39 This gene duplication allowed the mammalian p53 family members to gain novel functions. For example, ΔNp63, which is one of the isoforms encoded by the Trp63 gene, is essential for development of a squamous epithelial barrier.37, 40, 41, 42 Germ cell apoptosis, which was originally regulated by a single ancestral p53 family protein, appears to involve three paralogs in mammals. Interestingly, the levels of p53 and TAp73 were significantly reduced in p63 cKO oocytes, indicating a signaling network that links all three p53 family members within oocytes. Due to this mutual regulation, the function of TAp63 cannot be studied independently from those of p53 and TAp73. Prior works have shown that p53 is dispensable for doxorubicin- and radiation-induced apoptosis in oocytes.25, 28 In our study, p53 was coexpressed with either TAp63 or TAp73 in cisplatin-treated oocytes. Therefore, the dispensability of p53 in previous studies may result from compensation by the other p53 family members. In contrast, the mutually exclusive expression patterns of TAp63 and TAp73 suggest that the two proteins have unique roles in oocyte death.
Although the critical role for TAp63 in cisplatin-induced oocyte apoptosis has been established, neither the functional link between TAp63 and c-Abl in cisplatin-induced oocyte death, nor the role of imatinib and c-Abl inhibition in preventing oocyte death has been elucidated. In this regard, reagent specificity is a concern because imatinib is a highly specific inhibitor of c-Kit, platelet-derived growth factor receptor, c-Abl and v-Abl/Abl2, all of which are expressed in primordial and primary follicles.43, 44, 45, 46 However, because c-Abl was induced by cisplatin in a TAp63-dependent manner, we hypothesize that c-Abl is the target of imatinib in its fertoprotective effects on primordial follicles (Figure 7). Further studies are needed to identify the precise mechanism, through which imatinib exerts its fertoprotective effect against cisplatin.
As demonstrated by kidney grafting experiments, oocytes exposed to cisplatin are able to clear Pt-DNA adducts when the apoptotic signal is transiently repressed by imatinib, suggesting the feasibility of medically-based fertoprotection. However, there are several hurdles to clear before moving this new therapeutic approach to clinics. The biggest concern is whether cotreatment with imatinib compromises the efficacy of cisplatin on cancer, because activation of p53 or p73 by c-Abl has been shown to have critical roles in apoptosis of some cancer cell lines.47, 48, 49, 50 Further insight into the molecular mechanism of cisplatin-induced apoptosis in oocytes and cancer cells will be required to address this issue. A second critical hurdle is whether imatinib preserves the quality of eggs exposed to cisplatin. Animal studies have suggested that chemotherapies are mutagenic to female oocytes.51, 52 Therefore, the health of children born to women after cancer treatment is a major concern. Nevertheless, women undergoing chemotherapy with adjuvant imatinib may still benefit from preservation of endocrine function, even if the full integrity of the oocyte genome is not maintained.53 To determine the efficacy and safety of imatinib as a fertoprotective therapeutic, further studies on the mechanisms underlying the effects of cisplatin and imatinib on the oocyte are essential. Consequently, this report is an important contribution to a new field of inquiry that examines mechanisms for protecting fertility and reproductive health from iatrogenic damage caused by cancer treatments.
Materials and Methods
Animals
CD-1 mice were purchased from Harlan Laboratories (Madison, WI, USA), and C57BL/6j, NSG, Rosatm4(ACTB-tdTomato,-EGFP)Luo/J,54 and GDF9-iCre55 mice were purchased from Jackson Laboratories (Bar Harbor, ME, USA). The conditional alleles for Trp63 (p63 floxN)56 and ΔNp63-EGFP knock-in mice37 have been described previously. Rosatm4(ACTB-tdTomato,-EGFP)Luo/J;GDF9-iCre+mice were used as a wild-type control for all conditional knockout experiments. All procedures involving mice were approved by the Northwestern University Animal Care and Use Committee. Mice were housed and bred in a barrier facility within Northwestern University's Center of Comparative Medicine (Chicago, IL, USA) and were provided with food and water ad libitum. Temperature, humidity, and photoperiod (14L : 10D) were kept constant.
For conditional knockout studies, oocyte-specific gene excision was monitored by expression of EGFP from the ROSATE (Rosatm4(ACTB-tdTomato,-EGFP)Luo ) allele at the time of ovary dissection (Supplementary Figure S3). The genotype was confirmed by PCR of tail tissue as follows: the wild-type allele was detected with F1 (5′-AAGTGGCAGTGAGCAGAAC-3′) and R1 (5′-ACAATTCCAGTCAAACATCAA-3′) primers as a 300-bp product, and the floxed allele was detected with F1 and R2 (5′-TGAAAGATCCGGAACCCTTAATATA-3′) primers as a 450-bp product after 40 cycles of 94 °C for 5 min, 94 °C for 15 s, 58 °C for 15 s, and 72 °C for 30 s.
Whole-ovary organ culture
The day of birth was counted as postnatal day 0 (P0), and ovaries were collected from P5 neonatal mice. Ovaries were rinsed in L15 medium containing penicillin-streptomycin and 10% FBS and placed on a 0.4 μm pore Millicell insert (PICM03050, EMD Millipore Co, Billerica, MA, USA) in a six-well plate with culture medium: αMEM medium supplemented with 1 mg/ml bovine fetuin (Sigma-Aldrich, St. Louis, MO, USA), 5 μg/ml insulin, 5 μg/ml transferrin, 5 ng/ml selenium (Sigma-Aldrich), 30 mg/10 ml Albumin bovine (103700, MP Biomedicals, LLC., Solon, OH, USA) and 10 mlU/ml rhFSH (Sigma-Aldrich). Cisplatin (P4394, Sigma-Aldrich) and imatinib (PD-180970, Sigma-Aldrich) were prepared fresh as concentrated 100 × stock in PBS and H2O, respectively, and added to the medium to the final concentration. The surface of the ovary was covered with a drop of the culture medium and then cultured at 37 °C under 5% CO2. The medium was changed every 48 h. Ovaries were harvested after culture for 48 h or 96 h and processed for histologic analysis.
Subrenal grafting
Subrenal grafting of mouse ovaries has been reported previously.24 In this study, the inbred C57BL/6j mouse strain was used for isogenic grafting. Ovaries in the cisplatin and cisplatin+imatinib groups were exposed to cisplatin-containing medium for the first 24 h and then either no drug or imatinib in order to allow repair the cisplatin-mediated DNA damage (Supplementary Figure S2). After 96 h of organ culture, the ovaries were rinsed twice with PBS and then transplanted under the subrenal capsule of a 3-week-old C57BL/6j female host. All hosts were ovariectomized (OVX) at the time of grafting to remove the effect of endogenous ovaries. One ovary from each of the four groups (control, cisplatin, imatinib, cisplatin+imatinib) was grafted into one host (two ovaries/kidney). Hosts were euthanized 14 days after grafting to collect ovarian transplants.
Immunoblot analysis
Nuclear and cytoplasmic extracts were prepared using NE-PER nuclear and cytoplasmic extraction reagents (Thermo Fisher Scientific Inc., Waltham, MA, USA) according to the manufacturer's instructions. P5 mouse ovaries were homogenized with a minipestle in ice-cold lysis buffer and loaded with equal amounts of nuclear extracts into NuPAGE 4–12% gradient Bis-Tris precast SDS-PAGE gel and transferred to a nitrocellulose membrane (Life Technologies, Carlsbad, CA, USA). Primary antibodies used for immunoblotting were as follows: TAp63 (4A4) (sc-8431, Santa Cruz, CA, USA); TAp73 (A300-126A, Bethyl Laboratories Inc., Montgomery, TX, USA); p-c-Abl (ab4717, Abcam, Cambridge, MA, USA); and Lamin A/C (no. 2032, Cell Signaling Technology, Danvers, MA, USA). ECL Prime (89168-782, GE Healthcare Biosciences, Pittsburgh, PA, USA) was used for immunoblotted protein detection by The FluorChem HD Imaging System (Alpha Innotech Co, Johannesberg, Gauteng, South Africa).
Histology
Mouse ovaries were fixed with Modified Davison's fixative (Electron Microscopy Science Inc.) for 24 h at 4 °C and then processed and embedded in paraffin. H&E staining was performed using standard methods. Immunofluorescence staining (IF) and 3,3′-Diaminobenzidine (DAB) staining were performed and visualized as previously described.36, 57 Primary antibodies used for IF or DAB staining were as follows: MSY2 (gift from R. Schultz, University of Pennsylvania); TAp63 (gift from Dr. Satrajit Sinha, the State University of New York at Buffalo),58 p63 (4A4) (sc-8431), p53 (sc-6243) and c-Abl (sc-131) from Santa Cruz Biotechnology Inc. (Santa Cruz); PtCG (MAB R-C18, ONCOLYZE, Germany); phospho-ATM/ATR substrate (no. 2851) and cPARP (no. 9544) from Cell signaling Technology; γH2AX (05-636), Bax (Ab-1, pc66) and ΔNp73 (OP-181)59 from EMD Millipore; active caspase-3 (557035, BD Biosciences, San Jose, CA, USA); and TAp73 (A300-126A, Bethyl Laboratories Inc., Montgomery, TX, USA).59 The specificity of IF signals was tested by the absence of signals in the negative control, in which the primary antibody was omitted. For IF detection of c-Abl, p53 and TAp73, signals were amplified using the TSA detection kit (Life Technologies). For DAB staining, the DAB Peroxidase Substrate Kit (SK-4100, Vector, Burlingame, CA, USA) was used.
Follicle counting and statistical analysis
The entire ovary was sectioned at 5 μm thickness, and follicles were counted in every 5th section as described previously.36 Positive oocytes from DAB staining with c-Abl and TAp73 antibodies were counted (n=3/treatment). All statistical analyses (two-way ANOVA) were performed using the software Prism 4.0 (GraphPad Software, San Diego, CA, USA). A difference was considered to be significant if the P-value was<0.05.
Acknowledgments
We thank Megan M Romero (the Northwestern University Ovarian Histology Core: P01HD021921) for sectioning all our samples and Jessina Thomas for counting follicles. This work was supported by SYK and TKW (RL1HD058295, UL1DE19587); TK, VAS, LMB (R01CA154358 and R01HD064402); SYK, TK, and TKW (U54 HD076188)
Glossary
- BAX
Bcl-2-associated X protein
- ATM
Ataxia telangiectasia mutated
- ATR
Atm and Rad3-related
- GDF9
Growth differentiation factor 9
- EGFP
Enhanced green fluorescent protein
- PUMA
p53 upregulated modulator of apoptosis
- BAK
Bcl-2 homologous antagonist killer
- NSG
NOD-scid gamma
- FSH
Follicle-stimulating hormone
- PARP
Poly-ADP ribose polymerase
- TSA
Tyramide Signaling Amplification
- DAB
3,3-diaminobenzidine
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies this paper on Cell Death and Differentiation website (http://www.nature.com/cdd)
Edited by G Melino
Supplementary Material
References
- Minton SE, Munster PN. Chemotherapy-induced amenorrhea and fertility in women undergoing adjuvant treatment for breast cancer. Cancer Control. 2002;9:466–472. doi: 10.1177/107327480200900603. [DOI] [PubMed] [Google Scholar]
- Jeruss JS, Woodruff TK. Preservation of fertility in patients with cancer. N Engl J Med. 2009;360:902–911. doi: 10.1056/NEJMra0801454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meirow D. Ovarian injury and modern options to preserve fertility in female cancer patients treated with high dose radio-chemotherapy for hemato-oncological neoplasias and other cancers. Leuk Lymphoma. 1999;33:65–76. doi: 10.3109/10428199909093726. [DOI] [PubMed] [Google Scholar]
- Kerr JB, Brogan L, Myers M, Hutt KJ, Mladenovska T, Ricardo S, et al. The primordial follicle reserve is not renewed after chemical or gamma-irradiation mediated depletion. Reproduction. 2012;143:469–476. doi: 10.1530/REP-11-0430. [DOI] [PubMed] [Google Scholar]
- Muscari Lin E, Aikin JL, Good BC. Premature menopause after cancer treatment. Cancer Pract. 1999;7:114–121. doi: 10.1046/j.1523-5394.1999.07306.x. [DOI] [PubMed] [Google Scholar]
- Woodruff TK. The Oncofertility Consortium—addressing fertility in young people with cancer. Nature reviews. Clin Oncol. 2010;7:466–475. doi: 10.1038/nrclinonc.2010.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zelinski MB, Murphy MK, Lawson MS, Jurisicova A, Pau KY, Toscano NP, et al. In vivo delivery of FTY720 prevents radiation-induced ovarian failure and infertility in adult female nonhuman primates Fertil Steril 2011951440–1445.e1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonfloni S, Di Tella L, Caldarola S, Cannata SM, Klinger FG, Di Bartolomeo C, et al. Inhibition of the c-Abl-TAp63 pathway protects mouse oocytes from chemotherapy-induced death. Nat Med. 2009;15:1179–1185. doi: 10.1038/nm.2033. [DOI] [PubMed] [Google Scholar]
- Kerr JB, Hutt KJ, Cook M, Speed TP, Strasser A, Findlay JK, et al. Cisplatin-induced primordial follicle oocyte killing and loss of fertility are not prevented by imatinib. Nat Med. 2012;18:1170–1172. doi: 10.1038/nm.2889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiani E, Di Bartolomeo C, Klinger FG, Cannata SM, Bernardini S, Chateauvieux S, et al. Reply to: cisplatin-induced primordial follicle oocyte killing and loss of fertility are not prevented by imatinib. Nat Med. 2012;18:1172–1174. doi: 10.1038/nm.2852. [DOI] [PubMed] [Google Scholar]
- Woodruff TK. Preserving fertility during cancer treatment. Nat Med. 2009;15:1124–1125. doi: 10.1038/nm1009-1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine AJ, Tomasini R, McKeon FD, Mak TW, Melino G. The p53 family: guardians of maternal reproduction. Nat Rev Mol Cell Biol. 2011;12:259–265. doi: 10.1038/nrm3086. [DOI] [PubMed] [Google Scholar]
- Coutandin D, Ou HD, Lohr F, Dotsch V. Tracing the protectors path from the germ line to the genome. Proc Natl Acad Sci USA. 2010;107:15318–15325. doi: 10.1073/pnas.1001069107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pankow S, Bamberger C. The p53 tumor suppressor-like protein nvp63 mediates selective germ cell death in the sea anemone Nematostella vectensis. PLoS One. 2007;2:e782. doi: 10.1371/journal.pone.0000782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schumacher B, Hofmann K, Boulton S, Gartner A. The C. elegans homolog of the p53 tumor suppressor is required for DNA damage-induced apoptosis. Curr Biol. 2001;11:1722–1727. doi: 10.1016/s0960-9822(01)00534-6. [DOI] [PubMed] [Google Scholar]
- Derry WB, Putzke AP, Rothman JH. Caenorhabditis elegans p53: role in apoptosis, meiosis, and stress resistance. Science. 2001;294:591–595. doi: 10.1126/science.1065486. [DOI] [PubMed] [Google Scholar]
- Yamada Y, Davis KD, Coffman CR. Programmed cell death of primordial germ cells in Drosophila is regulated by p53 and the Outsiders monocarboxylate transporter. Development. 2008;135:207–216. doi: 10.1242/dev.010389. [DOI] [PubMed] [Google Scholar]
- Lane DP, Madhumalar A, Lee AP, Tay BH, Verma C, Brenner S, et al. Conservation of all three p53 family members and Mdm2 and Mdm4 in the cartilaginous fish. Cell Cycle. 2011;10:4272–4279. doi: 10.4161/cc.10.24.18567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin Y, Stahl BC, DeWolf WC, Morgentaler A. p53-mediated germ cell quality control in spermatogenesis. Dev Biol. 1998;204:165–171. doi: 10.1006/dbio.1998.9074. [DOI] [PubMed] [Google Scholar]
- Chandrasekaran Y, Richburg JH. The p53 protein influences the sensitivity of testicular germ cells to mono-(2-ethylhexyl) phthalate-induced apoptosis by increasing the membrane levels of Fas and DR5 and decreasing the intracellular amount of c-FLIP. Biol Reprod. 2005;72:206–213. doi: 10.1095/biolreprod.104.030858. [DOI] [PubMed] [Google Scholar]
- Petre-Lazar B, Livera G, Moreno SG, Trautmann E, Duquenne C, Hanoux V, et al. The role of p63 in germ cell apoptosis in the developing testis. J Cell Physiol. 2007;210:87–98. doi: 10.1002/jcp.20829. [DOI] [PubMed] [Google Scholar]
- Codelia VA, Cisterna M, Alvarez AR, Moreno RD. p73 participates in male germ cells apoptosis induced by etoposide. Mol Hum Reprod. 2010;16:734–742. doi: 10.1093/molehr/gaq045. [DOI] [PubMed] [Google Scholar]
- Kerr JB, Hutt KJ, Michalak EM, Cook M, Vandenberg CJ, Liew SH, et al. DNA damage-induced primordial follicle oocyte apoptosis and loss of fertility require TAp63-mediated induction of Puma and Noxa. Mol Cell. 2012;48:343–352. doi: 10.1016/j.molcel.2012.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurita T, Cunha GR, Robboy SJ, Mills AA, Medina RT. Differential expression of p63 isoforms in female reproductive organs. Mech Dev. 2005;122:1043–1055. doi: 10.1016/j.mod.2005.04.008. [DOI] [PubMed] [Google Scholar]
- Suh EK, Yang A, Kettenbach A, Bamberger C, Michaelis AH, Zhu Z, et al. p63 protects the female germ line during meiotic arrest. Nature. 2006;444:624–628. doi: 10.1038/nature05337. [DOI] [PubMed] [Google Scholar]
- Livera G, Petre-Lazar B, Guerquin MJ, Trautmann E, Coffigny H, Habert R. p63 null mutation protects mouse oocytes from radio-induced apoptosis. Reproduction. 2008;135:3–12. doi: 10.1530/REP-07-0054. [DOI] [PubMed] [Google Scholar]
- Deutsch GB, Zielonka EM, Coutandin D, Weber TA, Schafer B, Hannewald J, et al. DNA damage in oocytes induces a switch of the quality control factor TAp63alpha from dimer to tetramer. Cell. 2011;144:566–576. doi: 10.1016/j.cell.2011.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez GI, Knudson CM, Leykin L, Korsmeyer SJ, Tilly JL. Apoptosis-associated signaling pathways are required for chemotherapy-mediated female germ cell destruction. Nat Med. 1997;3:1228–1232. doi: 10.1038/nm1197-1228. [DOI] [PubMed] [Google Scholar]
- Tomasini R, Tsuchihara K, Wilhelm M, Fujitani M, Rufini A, Cheung CC, et al. TAp73 knockout shows genomic instability with infertility and tumor suppressor functions. Genes Dev. 2008;22:2677–2691. doi: 10.1101/gad.1695308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Hennik MB, van der Vijgh WJ, Klein I, Elferink F, Vermorken JB, Winograd B, et al. Comparative pharmacokinetics of cisplatin and three analogues in mice and humans. Cancer Res. 1987;47:6297–6301. [PubMed] [Google Scholar]
- Demetri GD, Wang Y, Wehrle E, Racine A, Nikolova Z, Blanke CD, et al. Imatinib plasma levels are correlated with clinical benefit in patients with unresectable/metastatic gastrointestinal stromal tumors. J Clin Oncol. 2009;27:3141–3147. doi: 10.1200/JCO.2008.20.4818. [DOI] [PubMed] [Google Scholar]
- Takai Y, Canning J, Perez GI, Pru JK, Schlezinger JJ, Sherr DH, et al. Bax, caspase-2, and caspase-3 are required for ovarian follicle loss caused by 4-vinylcyclohexene diepoxide exposure of female mice in vivo. Endocrinology. 2003;144:69–74. doi: 10.1210/en.2002-220814. [DOI] [PubMed] [Google Scholar]
- Ghafari F, Gutierrez CG, Hartshorne GM. Apoptosis in mouse fetal and neonatal oocytes during meiotic prophase one. BMC Dev Biol. 2007;7:87. doi: 10.1186/1471-213X-7-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang F, Baumann C, De La Fuente R. Persistence of histone H2AX phosphorylation after meiotic chromosome synapsis and abnormal centromere cohesion in poly (ADP-ribose) polymerase (Parp-1) null oocytes. Dev Biol. 2009;331:326–338. doi: 10.1016/j.ydbio.2009.05.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liedert B, Pluim D, Schellens J, Thomale J. Adduct-specific monoclonal antibodies for the measurement of cisplatin-induced DNA lesions in individual cell nuclei. Nucleic Acids Res. 2006;34:e47. doi: 10.1093/nar/gkl051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bristol-Gould SK, Kreeger PK, Selkirk CG, Kilen SM, Mayo KE, Shea LD, et al. Fate of the initial follicle pool: empirical and mathematical evidence supporting its sufficiency for adult fertility. Dev Biol. 2006;298:149–154. doi: 10.1016/j.ydbio.2006.06.023. [DOI] [PubMed] [Google Scholar]
- Romano RA, Smalley K, Magraw C, Serna VA, Kurita T, Raghavan S, et al. DeltaNp63 knockout mice reveal its indispensable role as a master regulator of epithelial development and differentiation. Development. 2012;139:772–782. doi: 10.1242/dev.071191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyashita T, Reed JC. Tumor suppressor p53 is a direct transcriptional activator of the human bax gene. Cell. 1995;80:293–299. doi: 10.1016/0092-8674(95)90412-3. [DOI] [PubMed] [Google Scholar]
- Belyi VA, Ak P, Markert E, Wang H, Hu W, Puzio-Kuter A, et al. The origins and evolution of the p53 family of genes. Cold Spring Harb Perspect Biol. 2010;2:a001198. doi: 10.1101/cshperspect.a001198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurita T, Mills AA, Cunha GR. Roles of p63 in the diethylstilbestrol-induced cervicovaginal adenosis. Development. 2004;131:1639–1649. doi: 10.1242/dev.01038. [DOI] [PubMed] [Google Scholar]
- Mills AA, Zheng B, Wang XJ, Vogel H, Roop DR, Bradley A. p63 is a p53 homologue required for limb and epidermal morphogenesis. Nature. 1999;398:708–713. doi: 10.1038/19531. [DOI] [PubMed] [Google Scholar]
- Yang A, Schweitzer R, Sun D, Kaghad M, Walker N, Bronson RT, et al. p63 is essential for regenerative proliferation in limb, craniofacial and epithelial development. Nature. 1999;398:714–718. doi: 10.1038/19539. [DOI] [PubMed] [Google Scholar]
- Hutt KJ, McLaughlin EA, Holland MK. KIT/KIT ligand in mammalian oogenesis and folliculogenesis: roles in rabbit and murine ovarian follicle activation and oocyte growth. Biol Reprod. 2006;75:421–433. doi: 10.1095/biolreprod.106.051516. [DOI] [PubMed] [Google Scholar]
- Herrera L, Ottolenghi C, Garcia-Ortiz JE, Pellegrini M, Manini F, Ko MS, et al. Mouse ovary developmental RNA and protein markers from gene expression profiling. Dev Biol. 2005;279:271–290. doi: 10.1016/j.ydbio.2004.11.029. [DOI] [PubMed] [Google Scholar]
- Yoon SJ, Kim KH, Chung HM, Choi DH, Lee WS, Cha KY, et al. Gene expression profiling of early follicular development in primordial, primary, and secondary follicles. Fertil Steril. 2006;85:193–203. doi: 10.1016/j.fertnstert.2005.07.1296. [DOI] [PubMed] [Google Scholar]
- Pan H, O'Brien MJ, Wigglesworth K, Eppig JJ, Schultz RM. Transcript profiling during mouse oocyte development and the effect of gonadotropin priming and development in vitro. Dev Biol. 2005;286:493–506. doi: 10.1016/j.ydbio.2005.08.023. [DOI] [PubMed] [Google Scholar]
- Gong JG, Costanzo A, Yang HQ, Melino G, Kaelin WG, Jr., Levrero M, et al. The tyrosine kinase c-Abl regulates p73 in apoptotic response to cisplatin-induced DNA damage. Nature. 1999;399:806–809. doi: 10.1038/21690. [DOI] [PubMed] [Google Scholar]
- Toh WH, Siddique MM, Boominathan L, Lin KW, Sabapathy K. c-Jun regulates the stability and activity of the p53 homologue, p73. J Biol Chem. 2004;279:44713–44722. doi: 10.1074/jbc.M407672200. [DOI] [PubMed] [Google Scholar]
- Sedletska Y, Giraud-Panis MJ, Malinge JM. Cisplatin is a DNA-damaging antitumour compound triggering multifactorial biochemical responses in cancer cells: importance of apoptotic pathways. Curr Med Chem Anticancer Agents. 2005;5:251–265. doi: 10.2174/1568011053765967. [DOI] [PubMed] [Google Scholar]
- Leong CO, Vidnovic N, DeYoung MP, Sgroi D, Ellisen LW. The p63/p73 network mediates chemosensitivity to cisplatin in a biologically defined subset of primary breast cancers. J Clin Invest. 2007;117:1370–1380. doi: 10.1172/JCI30866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meirow D, Schiff E. Appraisal of chemotherapy effects on reproductive outcome according to animal studies and clinical data. J Natl Cancer Inst Monogr. 2005;34:21–25. doi: 10.1093/jncimonographs/lgi025. [DOI] [PubMed] [Google Scholar]
- Katoh MA, Cain KT, Hughes LA, Foxworth LB, Bishop JB, Generoso WM. Female-specific dominant lethal effects in mice. Mutat Res. 1990;230:205–217. doi: 10.1016/0027-5107(90)90058-c. [DOI] [PubMed] [Google Scholar]
- Kong BY, Skory RM, Woodruff TK. Creating a continuum of care: integrating obstetricians and gynecologists in the care of young cancer patients. Clin Obstet Gynecol. 2011;54:619–632. doi: 10.1097/GRF.0b013e318236ea2c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muzumdar MD, Tasic B, Miyamichi K, Li L, Luo L. A global double-fluorescent Cre reporter mouse. Genesis. 2007;45:593–605. doi: 10.1002/dvg.20335. [DOI] [PubMed] [Google Scholar]
- Lan ZJ, Xu X, Cooney AJ. Differential oocyte-specific expression of Cre recombinase activity in GDF-9-iCre, Zp3cre, and Msx2Cre transgenic mice. Biol Reprod. 2004;71:1469–1474. doi: 10.1095/biolreprod.104.031757. [DOI] [PubMed] [Google Scholar]
- Mills AA, Qi Y, Bradley A. Conditional inactivation of p63 by Cre-mediated excision. Genesis. 2002;32:138–141. doi: 10.1002/gene.10067. [DOI] [PubMed] [Google Scholar]
- Kurita T. Developmental origin of vaginal epithelium. Differentiation. 2010;80:99–105. doi: 10.1016/j.diff.2010.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romano RA, Ortt K, Birkaya B, Smalley K, Sinha S. An active role of the DeltaN isoform of p63 in regulating basal keratin genes K5 and K14 and directing epidermal cell fate. PLoS One. 2009;4:e5623. doi: 10.1371/journal.pone.0005623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbluth JM, Johnson K, Tang L, Triplett T, Pietenpol JA. Evaluation of p63 and p73 antibodies for cross-reactivity. Cell Cycle. 2009;8:3702–3706. doi: 10.4161/cc.8.22.10036. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.