Abstract
Anecdotal and biographical reports have long suggested that bipolar disorder is more common in people with exceptional cognitive or creative ability. Epidemiological evidence for such a link is sparse. We investigated the relationship between intelligence and subsequent risk of hospitalisation for bipolar disorder in a prospective cohort study of 1,049,607 Swedish men. Intelligence was measured on conscription for military service at a mean age of 18.3 years and data on psychiatric hospital admissions over a mean follow-up period of 22.6 years was obtained from national records. Risk of hospitalization with any form of bipolar disorder fell in a stepwise manner as intelligence increased (p for linear trend <0.0001). However, when we restricted analyses to men with no psychiatric comorbidity, there was a ‘reversed-J’ shaped association: men with the lowest intelligence had the greatest risk of being admitted with pure bipolar disorder, but risk was also elevated among men with the highest intelligence (p for quadratic trend = 0.03), primarily in those with the highest verbal (p for quadratic trend=0.009) or technical ability (p for quadratic trend <0.0001). At least in men, high intelligence may indeed be a risk factor for bipolar disorder, but only in the minority of cases who have the disorder in a pure form with no psychiatric comorbidity.
Introduction
The idea that genius and madness are linked dates back at least as far as the Ancient Greeks. Anecdotal and biographical reports suggest that the extreme mood swings of elation and despair characteristic of bipolar disorder (previously known as manic depression) are more common in individuals with exceptional cognitive and creative ability.1,2 Epidemiological evidence for this link is sparse. One study found that children with high IQ scores were more likely to be diagnosed with mania in adulthood than less bright peers, but there were only eight cases of mania, too few to be certain of the accuracy of this finding.3 Another indication that exceptionally bright people may be at risk of bipolar disorder comes from findings that boys with very high or very low school grades were both more likely than those with average performance to be hospitalised with bipolar disorder as adults; 4 whether these associations are driven primarily by intelligence or by other factors that influence educational attainment is unclear. No association was found between intelligence and subsequent hospitalisation with bipolar disorder in a study of 50,000 men, but the study may have lacked the statistical power to detect an association.5
Bipolar disorder is uncommon in the general population, as is very high intelligence, so studying very large numbers of people is necessary for reliable detection of any association between the two. We used data on over a million Swedish men to investigate the relationship between intelligence and subsequent hospitalisation for bipolar disorder. People with higher intelligence have a lower risk of some mental disorders, including schizophrenia, non-affective psychoses, major depression, neurotic and substance use disorders.6,7 We hypothesised that, if men with exceptional intelligence do have an increased risk of bipolar disorder, it will be bipolar disorder in its pure form with no psychiatric comorbidity.
Methods
Study participants and record-linkage of registers
The record linkage methods used to generate this cohort study have been reported previously.8 In brief, the cohort comprises all non-adopted men born in Sweden from 1950 to 1976 for whom both biological parents could be identified in the Multi-Generation Register. Using unique personal identification numbers we linked the Multi-Generation Register with the Military Service Conscription Register, Population and Housing Censuses records, the Cause of Death Register, and the National Hospital Discharge Register. Study approval was obtained from the Regional Ethics Committee, Stockholm.
Conscription examination
The military service conscription examination involves a structured, standard medical assessment of physical and mental health, and intelligence. During the years covered by this study, the law required this examination; only men of foreign citizenship or those with severe disability were excused. This dataset covers examinations from 15 September 1969 to 31 December 1994, after which testing procedures used to assess intelligence changed. Intelligence was measured at a mean age of 18.3 years using four written subtests of verbal, logical, spatial, and technical ability.9,10 Due to military secrecy, a detailed description of the tests is not available to persons outside the Swedish conscription board, however, the subtests can be described in general terms. The logical test measures the capacity to understand written instructions and apply them to solving a problem. Items from the spatial test depicted a plan drawing of an object in its pre-assembled, two-dimensional state. Respondents were required to identify, from a series of drawings of fully-assembled, three-dimensional objects, which it represented. The verbal test measures the knowledge of synonyms. The subject is required to determine which out of four alternatives is the synonym of a given word. The technical comprehension test measures technical and mechanical aptitude and also knowledge of chemistry and physics; it implies a component of general knowledge. Correlations between the test scores range between 0.47 and 0.69. All test scores - including a global IQ score derived from a summation of the four subtests results - were standardized to give a Gaussian distributed score between 1 and 9 (a ‘standard nine’ or ‘Stanine’ score), with higher values indicating greater intellectual capacity. In a population where IQ has a mean of 100 and a standard deviation of 15, a Stanine score of 1 is equivalent to an IQ of 75 or less and a Stanine score of 9 is equivalent to an IQ of least 125. In our study sample which excludes men who were judged unsuitable for conscription due to mental retardation, it is possible that these values will be higher.”
Men underwent a medical examination, including a structured interview by a psychologist. A psychiatrist assessed men who reported or showed psychiatric symptoms. Diagnoses were made according to the Swedish version of the International Classification of Disease (ICD) versions 8 or 9.
Inpatient episodes
The Swedish National Hospital Discharge Register has covered virtually all in-patient care for psychiatric disorders (including hospital admissions at forensic psychiatric clinics) since 1973, with the exception of admissions in a few counties during some of the early years of data collection.11 The validity of a discharge diagnosis of bipolar disorder has recently been investigated and found to be high, with 92% agreement between register diagnoses of bipolar disorder and diagnoses based on two psychiatrists’ assessment of medical records.12 Nearly all other studies on the validity of the psychiatric diagnoses in the Swedish National Hospital Discharge Register have examined schizophrenia.13 For this disorder too, the number of false-positive diagnoses in the Register appears to be low.14,15 We extracted data from the Register on psychiatric admissions from 1968 to December 31st 2004.
Men were followed up for psychiatric hospital admission for a mean of 22.6 years. Diagnoses (both primary and secondary) were coded according to the Swedish version of the International Classification of Disease versions 8, 9 or 10. Cases of bipolar disorder were defined from version 8 using codes 296.0, 296.1, 296.3, 296.88, 296.99, from version 9 using codes 296A, 296C, 296D, 296E, 296W, 296X, and from version 10 using codes F30-31. This combination of codes was shown by Sellgren and colleagues’ validity study to be optimal in terms of sensitivity and specificity.12 Adopting a hierarchy-free approach to the data on diagnoses, we classified men as having bipolar disorder if they were assigned a hospital discharge diagnosis of bipolar disorder on one or more occasions during the follow-up period. We considered men to have a comorbid form of bipolar disorder if they were also assigned a hospital discharge diagnosis of one or more other mental disorders at any point during the follow-up period (either before their bipolar disorder diagnosis, concurrently or sequentially); the exception to this was men with a diagnosis of bipolar disorder whose sole comorbid diagnosis was a depressive disorder; these men, together with those who had no comorbid diagnoses, were considered to have pure bipolar disorder.
Statistical analysis
We used Cox proportional hazards regression to calculate risks of hospital admission for bipolar disorder category according to IQ categories. Survival time in days was calculated from date of conscription to date of first hospital admission, date of death, date of emigration, or 31st December 2004, whichever occurred first. 90.1% of the participants were followed up to 31st December 2004. We adjusted for age at conscription, conscription testing centre, year of conscription, parental age and parental socioeconomic status which was based on the highest occupation of either parent from the 1960/1970 Population and Housing Censuses classified in 5 categories: non-manual (high/intermediate), non-manual (low), skilled, unskilled, and other. (As the presence of severe mental disorder may affect educational attainment and adult socioeconomic status, we did not adjust for these factors.) As prior psychiatric disorder might have affected performance on the IQ test, we excluded men diagnosed with psychiatric disorder at conscription or admitted to hospital with a psychiatric disorder before conscription (n=88,385). Analyses are based on the remaining 1,049,607 men. We carried out a receiver operator curve analysis to investigate the overall performance of IQ as a method of classifying individuals according to subsequent hospitalization with bipolar disorder
Results
Table 1 shows the distribution of the 1,049,607 men in the study according to the 9-point total IQ scale, and the association of IQ with the main covariates. Men with higher IQ scores were less likely to have parents in unskilled occupations. Higher IQ was also associated with older age at conscription and with older maternal and paternal age at birth.
Table 1. Distribution of IQ scores at conscription and their relation with the main study covariates.
| Covariates | IQ score category | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
| No of men | 23,018 | 63,539 | 102,304 | 152,097 | 238,608 | 188,101 | 143,360 | 89,385 | 49,195 |
| Parent in unskilled occupation, no (%) |
9,270 (40.3) | 23,293 (36.7) | 34,803 (34.0) |
46,620 (30.7) |
62,985 (26.4) |
42,229 (22.5) |
26,905 (18.8) |
13,542 (15.2) |
5,934 (12.1) |
| Maternal age, mean (SD) | 26.9 (6.1) | 26.7 (6.0) | 26.8 (5.9) | 27.0 (5.9) | 27.1 (5.7) | 27.5 (5.6) | 27.7 (5.5) | 28.0 (5.3) | 28.2) (5.1) |
| Paternal age, mean (SD) | 30.7 (7.3) | 30.3 (7.0) | 30.2 (6.9) | 30.3 (6.8) | 30.2 (6.6) | 30.6 (6.5) | 30.8 (6.4) | 31.0 (6.3) | 31.1 (6.2) |
| Age at conscription, mean (SD) | 18.2 (0.5) | 18.2 (0.5) | 18.2 (0.5) | 18.3 (0.5) | 18.3 (0.5) | 18.3 (0.5) | 18.4 (0.5) | 18.4 (0.5) | 18.4 (0.5) |
In total, 3174 men (0.3%) were hospitalized with bipolar disorder during the follow-up period. Of these 3174 men, 2357 (74%) had also been diagnosed with other mental disorders. Of these, the most common comorbid disorders were mood disorders (31.4%), other non-affective psychoses (28.2%), schizophrenia (24.7%),.neuroses or adjustment disorders (22.2%), and alcohol-related disorders (20.2%). In total, 1079 (34%) of the men hospitalized with bipolar disorder had it in a pure form (defined here as either a diagnosis of bipolar disorder alone (n=817) or a diagnosis of bipolar disorder comorbid with mood disorder alone (n=262)).
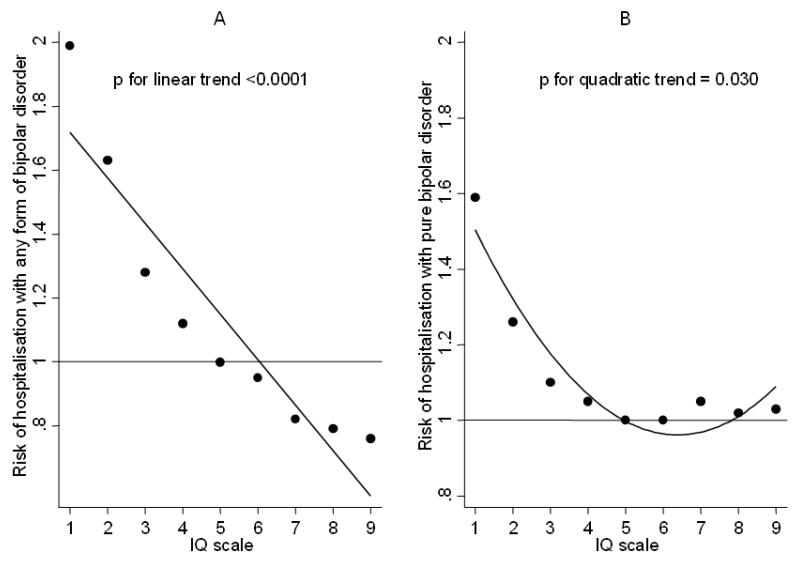
In unadjusted analyses, risk of hospitalization with any form of bipolar disorder fell in a stepwise manner as intelligence increased (p for linear trend <0.0001). Compared to men with average intelligence (IQ category=5), men with lower intelligence had an increased risk of hospitalisation with any form of bipolar disorder, while men with higher intelligence had a lower risk. Adjustment for age, year of conscription, conscription testing centre, parental age and parental social class had little effect on this association (Figure 1, A). We next excluded men with comorbid forms of the disorder (except those where mood disorder was the only comorbidity) in order to examine the link between intelligence and risk of being admitted with pure bipolar disorder. Compared to men with average intelligence, men with lower intelligence had an increased risk of hospitalisation with pure bipolar disorder, while men with higher intelligence had a similar or even slightly increased risk (p for quadratic trend = 0.03) (Figure 1, B). Confidence intervals around these estimates are wide because of the small number of cases within each IQ score band (Table 2).
Figure 1.
Hazard ratios for hospitalisation for any form of bipolar disorder (A) or pure bipolar disorder (B) in relation to IQ at conscription. Estimates have been adjusted for age, year of conscription, conscription testing centre, parental age and parental social class. Men in the average IQ group (IQ =5) are the reference group. Each graph shows the line that best fitted the data.
Table 2. Hazard ratios (95% confidence intervals) for admission to hospital with any form of bipolar disorder or with pure bipolar disorder during the follow-up period in relation to IQ at conscription.
| Any form of bipolar disorder | Pure bipolar disorder | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| IQ scale | Number | Number (%) admitted |
Hazard ratio (95% CI), adjusted for age, year of conscription, conscription testing centre, parental age and parental socioeconomic status |
Number | Number (%) admitted |
Hazard ratio (95% CI), adjusted for age, year of conscription, conscription testing centre, parental age and parental socioeconomic status |
| 1 | 23,018 | 125 (0.54) | 1.99 (1.65, 2.42) | 22,925 | 32 (0.14) | 1.59 (1.12, 2.38) |
| 2 | 63,539 | 288 (0.45) | 1.63 (1.42, 1.88) | 63,324 | 73(0.12) | 1.26 (0.97, 1.64)) |
| 3 | 102,304 | 374 (0.37) | 1.28 (1.13, 1.45) | 102,035 | 105 (0.10) | 1.10 (0.87, 1.38) |
| 4 | 152,097 | 501 (0.33) | 1.12 (1.00, 1.26) | 151,756 | 160 (0.11) | 1.05 (0.86, 1.29) |
| 5 | 238,608 | 659 (0.28) | 1.0 (Reference) | 238,170 | 221 (0.09) | 1.0 (Reference) |
| 6 | 188,101 | 532 (0.28) | 0.95 (0.85, 1.07) | 187,756 | 187 (0.10) | 1.00 (0.82, 1.21) |
| 7 | 143,360 | 359 (0.25) | 0.82 (0.72, 0.93) | 143,155 | 154 (0.11) | 1.05 (0.85, 1.29) |
| 8 | 89,385 | 220 (0.25) | 0.79 (0.68, 0.92) | 89,260 | 95 (0.11) | 1.02 (0.80, 1.30) |
| 9 | 49,103 | 116 (0.24) | 0.76 (0.62, 0.92) | 49,131 | 52 (0.11) | 1.03 (0.76, 1.38) |
|
| ||||||
| Total n | 1,049,607 | 3,174 (0.30) | 1,047,512 | 1,079 (0.10) | ||
|
| ||||||
| P for linear trend | <0.0001 | |||||
|
| ||||||
| P for quadratic trend | 0.030 | |||||
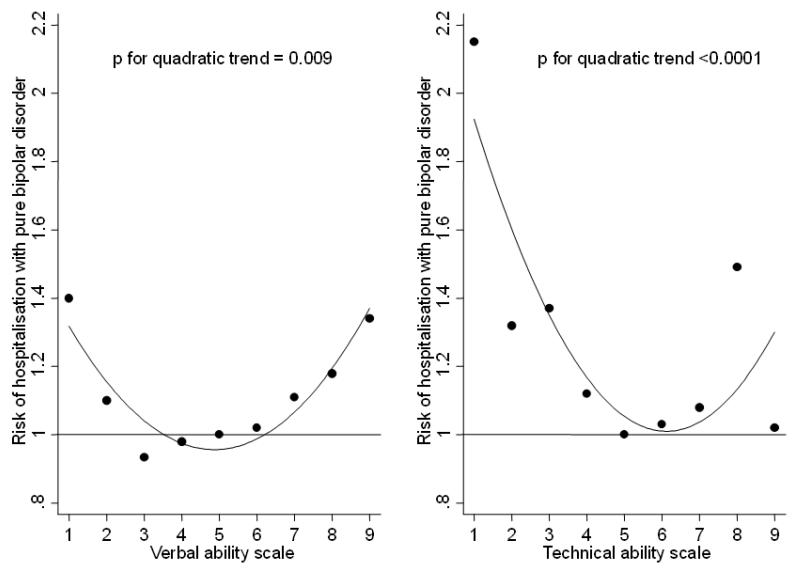
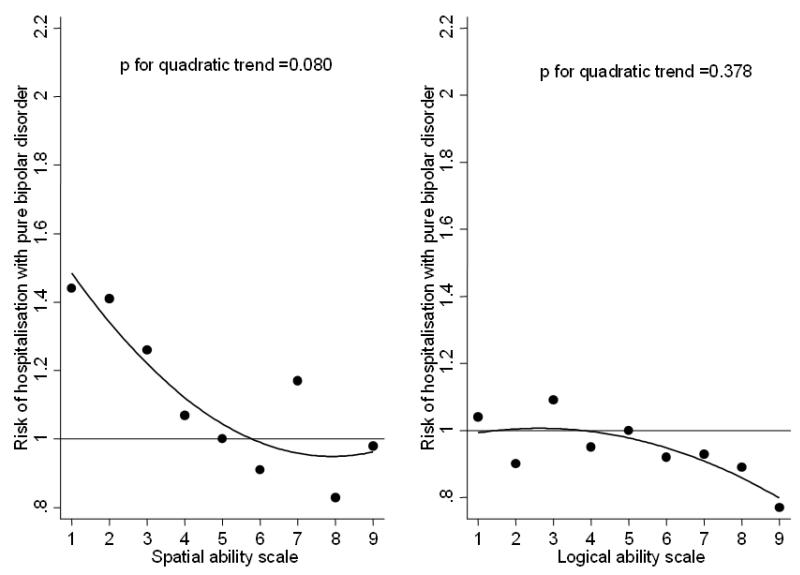
We examined the relation between scores on each of the four IQ subtests (verbal, logical, spatial, and technical) separately and risk of bipolar disorder. Linear associations between scores on each of the subtests and risk of any form of bipolar disorder were very similar to those found for total IQ (supplementary tables 1-4). However, there was more variability in the associations between scores on the subtests and risk of pure bipolar disorder (Figures 2 and 3, and supplementary tables 1-4). There were highly statistically significant quadratic trends between scores on the verbal and technical subtests and risk of hospitalization with pure bipolar disorder. There was a ‘U’-shaped association between verbal ability and risk of pure bipolar disorder (p for quadratic trend=0.009). Compared to men with average verbal ability, risk of hospitalization with pure bipolar disorder rose as verbal ability increased such that men with the highest verbal ability had a 41% increase in risk; men with the lowest verbal ability had an increase in risk of 34%. There was a ‘reversed-J’ shaped association between technical ability and risk of pure bipolar disorder (p for quadratic trend <0.0001). Men with the lowest technical ability had the greatest risk compared to those of average ability, but risk was also increased, to a lesser extent, in men of high technical ability, though it is worth noting that this increased risk was primarily in men in one ability group (technical ability scale=8). There was a weak quadratic trend between spatial ability and risk of pure bipolar disorder that was of borderline significance (p=0.080), and no clear trend between logical ability and risk of pure bipolar disorder.
Figure 2.
Hazard ratios for hospitalisation for pure bipolar disorder in relation to verbal or technical ability at conscription. Estimates have been adjusted for age, year of conscription, conscription testing centre, parental age and parental social class. Men in the average ability group (verbal or technical=5) are the reference group. Each graph shows the line that best fitted the data.
Figure 3.
Hazard ratios for hospitalisation for pure bipolar disorder in relation to spatial or logical ability at conscription. Estimates have been adjusted for age, year of conscription, conscription testing centre, parental age and parental social class. Men in the average ability group (spatial or logical=5) are the reference group. Each graph shows the line that best fitted the data.
In total, 24% of the men we classified as having pure bipolar disorder had also been diagnosed with a mood disorder at some stage during follow-up. These men differed from those whose sole diagnosis was bipolar disorder in that they had been admitted to hospital more often (median number of admissions 2 vs 1, p=0.002), suggesting that one explanation for their additional diagnosis might be that on average they tended to have more severe or complex illness. We had originally hypothesized that if men with exceptional intelligence do have an increased risk of bipolar disorder, it will be bipolar disorder in its pure form with no psychiatric comorbidity, in other words a form of the disorder that is likely to be less severe. As a further test of this we repeated our analyses of risk of pure bipolar disorder after excluding these 262 men. This exclusion strengthened the quadratic associations between total IQ and the verbal ability subtest and risk of pure bipolar disorder, such that the p values for quadratic trend changed from 0.03 to 0.003 and 0.009 to 0.004 respectively. After full adjustment for all the covariates, compared to men with average IQ, men with the lowest total IQ had a 56% increase in risk and men with highest IQ had a 24% increase in risk. Compared to men with average verbal ability, men with the lowest verbal ability had a 43% increase in risk, while men with high verbal ability had a 60% increase in risk. Quadratic associations between the technical ability and spatial ability subtests were only slightly strengthened by this exclusion
Discussion
These findings based on over a million men provide partial support for the belief that exceptional intelligence and a particular form of ‘madness’ are linked. Most men hospitalized with bipolar disorder were also diagnosed with other disorders. Comorbid forms of bipolar disorder occurred less frequently in highly intelligent men than in men of average or lower ability, consistent with findings that suggest that high intelligence may confer resilience to several forms of psychiatric comorbidity.6,7 Among those who had bipolar disorder in a pure form, we found that men with the highest intelligence, particularly as regards verbal and technical ability, were at increased risk compared to those of average ability. These associations with high intelligence were strengthened when we used a more restrictive definition of pure bipolar disorder, excluding cases who had been diagnosed with a mood disorder as well as bipolar disorder. It may be that genetic or environmental factors linked with having bipolar disorder in a pure form are also involved in high intelligence but we are unaware of any evidence on this. Pure bipolar disorder is rarely studied. Evidence from a family-based study showed that bipolar disorder as a whole is associated with poorer memory and processing speed and that these cognitive deficits are linked with genetic liability to the illness, but there was no examination of pure bipolar disorder.16
Examination of the four subtests of IQ showed that risk of being hospitalized with any form of bipolar disorder fell as scores for verbal, spatial, logical or technical ability increased, just as it did with global IQ score. However, for risk of hospitalization with pure bipolar disorder, the picture was slightly different in that not all abilities appeared to be equally associated with risk: the quadratic association seen between IQ and risk appeared to be due primarily to an increased risk of pure bipolar disorder in men with the highest verbal or technical abilities. This is in keeping with biographical reports linking bipolar disorder with exceptional literary or scientific creativity, 1,2 though it is perhaps surprising that high logical and spatial abilities were not similarly associated with increased risk. This difference may be a chance finding, but given that scores on all four subtests were linked with risk of hospitalisation with bipolar disorder overall, the fact that high ability in some cognitive domains appears to be particularly predictive of pure bipolar disorder is worthy of further investigation.
Our study shows that population variations in IQ at age 18 are predictive of risk of hospitalization with bipolar disorder many years later, but it is worth stressing that this does not imply that IQ is an effective discriminator of which individuals go on to have hospital treatment for this disorder. All the hazard ratios in our study were under 3. Hazard ratios relating a risk predictor to a subsequent disease outcome need to be of an order of magnitude that is rare in epidemiological studies if they are to be effective markers of whether an individual will develop a disease (Pepe et al 2004). We carried out a receiver operator curve analysis to investigate the overall performance of IQ as a method of classifying individuals according to subsequent hospitalization with bipolar disorder. As expected, this analysis showed that there was no optimal cut point in terms of sensitivity and specificity and the area under the curve was 0.57, suggesting that, based on these data, IQ does not provide an accurate marker of individual outcome.
The main strength of this study lies in its size. This, coupled with the length of follow-up, allowed us to examine the relation of pre-morbid intelligence with risk of a disorder that is uncommon in the general population. The study also has limitations. Firstly, cases of bipolar disorder during the follow-up period were defined on the basis of hospital admission. In Sweden, as in many other countries, inpatient care for mental disorders has become less common. The men identified as having bipolar disorder in our study are therefore likely to be predominantly those with more severe illness, and, perhaps, those whose coping skills or lack of support networks make them more liable to be offered inpatient treatment. The use of non-standardised diagnoses made by different clinicians is a further drawback of using data from national inpatient registers. In the absence of gold standard data on lifetime diagnosis made using structured interview we cannot be certain of the accuracy of our classification of pure bipolar disorder, or indeed of bipolar disorder as a whole, though it is worth pointing out that a validation study of the bipolar disorder diagnoses in the Swedish inpatient register suggests that the number of false-positive diagnoses is low.12 The second limitation of our study is that it is based on men only. Whether our findings can be extrapolated to women is uncertain. Finally, a subset of this cohort had been the subject of previous research into intelligence and bipolar disorder5. Although the present study uses the same conscription register, there is virtually no overlap between the two study populations: the earlier study was based on men born in 1949-1951 and represents around 2% of the present study population, who were born between 1950 and 1976.
Our results suggest that, at least in men, high intelligence may indeed be a risk factor for bipolar disorder, but only in the minority who have the disease in a pure form. The association with high intellect might also help to explain why this seriously debilitating condition has been maintained across populations and human history.
Supplementary Material
Acknowledgments
The University of Edinburgh Centre for Cognitive Ageing and Cognitive Epidemiology is supported by the Biotechnology and Biological Sciences Research Council, the Economic and Social Research Council, the Engineering and Physical Sciences Research Council and the Medical Research Council, as part of the Lifelong Health and Wellbeing Initiative (G0700704/84698). David Batty is a UK Wellcome Trust Fellow. Finn Rasmussen is supported by the Swedish Council for Working Life and Social Research. The study sponsors had no role in the study design, the collection of data, or in the preparation of this manuscript.
Footnotes
Conflicts of interest
None of the authors has any competing financial interest in relation to this work.
References
- 1.Jamison KR. Manic-depressive illness and creativity. Sci Am. 1995;272:62–7. doi: 10.1038/scientificamerican0295-62. [DOI] [PubMed] [Google Scholar]
- 2.Nettle D. Strong imagination: Madness, creativity and human nature. Oxford University Press; Oxford: 2001. [Google Scholar]
- 3.Koenen KC, Moffitt TE, Roberts AL, Martin LT, Kubzansky L, Harrington H, et al. Childhood IQ and adult mental disorders: a test of the cognitive reserve hypothesis. Am J Psychiatry. 2009;166:50–7. doi: 10.1176/appi.ajp.2008.08030343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.MacCabe JH, Lambe MP, Cnattingius S, Sham PC, David AS, Reichenberg A, et al. Excellent school performance at age 16 and risk of adult bipolar disorder: national cohort study. Br J Psychiatry. 2010;196:109–15. doi: 10.1192/bjp.bp.108.060368. [DOI] [PubMed] [Google Scholar]
- 5.Zammit S, Allebeck P, David AS, Dalman C, Hemmingsson T, Lundberg I, et al. A longitudinal study of premorbid IQ Score and risk of developing schizophrenia, bipolar disorder, severe depression, and other nonaffective psychoses. Arch Gen Psychiatry. 2004;61:354–60. doi: 10.1001/archpsyc.61.4.354. [DOI] [PubMed] [Google Scholar]
- 6.Gale CR, Deary IJ, Boyle SH, Barefoot J, Mortensen LH, Batty GD. Cognitive ability in early adulthood and risk of 5 specific psychiatric disorders in middle age: the Vietnam experience study. Arch Gen Psychiatry. 2008;65:1410–8. doi: 10.1001/archpsyc.65.12.1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gale CR, Batty GD, Tynelius P, Deary IJ, Rasmussen F. Intelligence in early adulthood and subsequent hospitalization for mental disorders. Epidemiology. 2010;21:70–7. doi: 10.1097/EDE.0b013e3181c17da8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gunnell D, Magnusson PK, Rasmussen F. Low intelligence test scores in 18 year old men and risk of suicide: cohort study. BMJ. 2005;330:167. doi: 10.1136/bmj.38310.473565.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carlstedt B, Mardberg B. Construct-Validity of the Swedish Enlistment Battery. Scandinavian Journal of Psychology. 1993;34:353–62. doi: 10.1111/j.1467-9450.2005.00432.x. [DOI] [PubMed] [Google Scholar]
- 10.Carlstedt B. Cognitive abilities - aspects of structure, process and measurement. University of Gothenburg; 2000. [Google Scholar]
- 11.Epidemiologiskt Centrum S. Patientregistret. Utskrivningar från sluten vård 1964-2005. Kvalitet och innehåll. Socialstyrelsen; Stockholm: 2006. [Google Scholar]
- 12.Sellgren C, Landen M, Lichtenstein P, Hultman CM, Langstrom N. Validity of bipolar disorder hospital discharge diagnoses: file review and multiple register linkage in Sweden. Acta Psychiatr Scand. 2011;124:447–53. doi: 10.1111/j.1600-0447.2011.01747.x. [DOI] [PubMed] [Google Scholar]
- 13.Ludvigsson JF, Andersson E, Ekbom A, Feychting M, Kim JL, Reuterwall C, et al. External review and validation of the Swedish national inpatient register. BMC Public Health. 2011;11:450. doi: 10.1186/1471-2458-11-450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ekholm B, Ekholm A, Adolfsson R, Vares M, Osby U, Sedvall GC, et al. Evaluation of diagnostic procedures in Swedish patients with schizophrenia and related psychoses. Nord J Psychiatry. 2005;59:457–64. doi: 10.1080/08039480500360906. [DOI] [PubMed] [Google Scholar]
- 15.Dalman C, Broms J, Cullberg J, Allebeck P. Young cases of schizophrenia identified in a national inpatient register--are the diagnoses valid? Soc Psychiatry Psychiatr Epidemiol. 2002;37:527–31. doi: 10.1007/s00127-002-0582-3. [DOI] [PubMed] [Google Scholar]
- 16.Glahn DC, Almasy L, Barguil M, Hare E, Peralta JM, Kent JW, et al. Neurocognitive endophenotypes for bipolar disorder identified in multiplex multigenerational families. Arch Gen Psychiatry. 2010;67:168–77. doi: 10.1001/archgenpsychiatry.2009.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.