Abstract
In this report, we conducted a secondary analysis of the Treatment of SSRI-Resistant Depression in Adolescents (TORDIA) study to explore the impact of specific cognitive–behavioral therapy (CBT) treatment components on outcome. In TORDIA, 334 youths (ages 12 to 18 years) with major depressive disorder who had failed to respond to an adequate course of selective serotonin reuptake inhibitor (SSRI) medication were randomized to a medication switch (either to an alternative SSRI or venlafaxine) with or without 12 weeks of adjunctive CBT. Participants who had more than 9 CBT sessions were 2.5 times more likely to have adequate treatment response than those who had 9 or fewer sessions. CBT participants who received problem-solving and social skills treatment components, controlling for number of sessions and other confounding variables, were 2.3 and 2.6 times, respectively, more likely to have a positive response. These preliminary findings underscore the importance of receiving an adequate number of sessions to attain an adequate clinical response. Finally, social skills and problem solving may be active elements in CBT for adolescent depression and should be considered in treatment by those working with seriously depressed youths.
Keywords: cognitive–behavioral therapy, adolescent depression, treatment components
Cognitive–behavioral therapy (CBT) is an established treatment for adolescent depression (Birmaher et al., 2007; Weisz, McCarty, & Valeri, 2006). However, CBT as a psychotherapy is composed of many heterogeneous treatment components. Common components, such as cognitive restructuring, behavioral activation, social skills training, and problem solving, are often included in these interventions, but the emphasis, specifics of delivery, intensity, and frequency varies (McCarty & Weisz, 2007; Weersing, Rozenman, & Gonzalez, 2009). Currently, little is known about which specific components of CBT contribute the most to positive treatment outcomes in depressed youths. Additionally, few studies have addressed CBT dosing (i.e., frequency and number of sessions) in relation to treatment outcome. Consequently, the National Institute of Mental Health has noted that research is needed to identify effective components of treatments for depressed youths to inform future adaptations that are more “potent” and more “efficient and transportable” (National Institute of Mental Health, 2006).
Little is known about the relationship between CBT dosing and treatment outcome. Craske et al. (2006) evaluated the relationship between CBT intensity and anxiety outcomes in panic disorder, concluding that a greater number of CBT sessions was related to fewer anxiety symptoms. In a study of CBT for insomnia, Edinger, Wohlgemuth, Radtke, Coffman, and Carney (2007) examined dose–response effects of one-session, two-session, four-session, and eight-session CBT. Edinger et al. found that four biweekly sessions resulted in “optimal dosing” (p. 210), with 58.3% of participants in this group meeting criteria for clinically significant improvement, as compared with 43.8% in one-session CBT, 22.2% in two-session CBT, and 35.3% in eight-session CBT.
In the adult depression literature, randomized component analysis studies have found that behavioral activation is more effective than cognitive strategies in acute treatment (Dimidjian et al., 2006), whereas both components appear equally efficacious in relation to longer term outcomes (Dobson et al., 2008). Such studies do not yet exist in the youth depression literature, although recent investigations and meta-analyses suggest promising directions for treatment component research. For example, Asarnow, Scott, and Mintz (2002) found that preadolescent children reported finding behavioral components of a group CBT for depression (e.g., pleasant activities/behavioral activation, problem solving, social skills) to be more helpful than cognitive components. In CBT treatment of pediatric anxiety, Kendall et al. (1997) examined the necessity of an exposure intervention in a study of anxiety disorders in children (ages 9 to 13 years). These researchers compared the response to the first half of treatment, which included a cognitive–educational training intervention, with the response at the completion of treatment, which included the cognitive–educational training plus exposure, and found that the exposure component was necessary to achieve improvement.
Weersing et al. (2009) coded the content of three, prominent manualized CBT interventions for youths with major depressive disorder. These three interventions—namely, the Coping with Depression for Adolescents Course (CWD-A; Lewinsohn, Clarke, Hops, & Andrews, 1990), the Cognitive Therapy Manual from the Pittsburgh CBT trial (Brent & Poling, 1997; Brent et al., 1997), and the modular CBT manual of the Treatment for Adolescents With Depression Study (TADS; Curry et al., 2000; Wells & Curry, 2000)—varied widely in CBT technique content and emphasis. For example, both the Coping With Depression for Adolescents (CWD-A) and Pittsburgh Cognitive Therapy manuals included a significant number of sessions devoted to cognitive restructuring, whereas the TADS CBT manual included a wider range of core skills. Given the less potent acute effects of monotherapy CBT in TADS compared with other CBT investigations (Treatment for Adolescents With Depresssion Study (TADS) Team, 2004), Weersing et al. speculated, in their review on effective components of CBT in the literature (2009), that there might be a “dose × technique minimum threshold” (p. 30) for core components of CBT, such as cognitive restructuring and behavioral activation. In a similar fashion, McCarty and Weisz (2007) examined common components of several efficacious CBT studies, conducting a meta-analysis of nine studies of pediatric major depressive disorder with an effect size of 0.5 or greater. The most frequent components (i.e., those found in six or more studies) of these successful CBT studies included achieving measurable goals or increasing competence, child psychoeducation, self-monitoring, relationship skills, communication training, cognitive restructuring, problem solving, and behavioral activation. Because many of these components are combined in these studies, we still do not know which of these specific components is having a direct impact on outcome, nor the most effective dose of treatment components. Although the most accurate way to determine which components are most effective is experimentally by a dismantling study (Jacobson et al., 1996), no studies of this kind currently exist in the child CBT literature.
Whereas strides have been made in testing manualized, evidence-based interventions for children and adolescents with depression, researchers and clinicians have relatively little information regarding the active ingredients of these effective treatments. The need for dissemination of these treatments has been noted (Chambers et al., 2005); however, it would be helpful to know which components are most efficacious in order to generate the most efficient program to facilitate dissemination.
In this report, we describe a secondary exploratory analysis of a large randomized clinical trial of adolescent depression in order to examine the relationship between the use of various types of therapy modules and therapeutic outcome. The Treatment of SSRI-Resistant Depression in Adolescents Study (TORDIA) enrolled youths with major depression who had failed to respond to an initial, adequate course of selective serotonin reuptake inhibitor (SSRI) medication. These youths were randomized to a medication switch (either to an alternative SSRI or to venlafaxine) with or without adjunctive CBT. This randomized, controlled trial has been well described in a previous report, and overall results supported the efficacy of the CBT and medication combination treatment over a medication switch alone (Brent et al., 2008). In this secondary analysis, we evaluate those participants who received 12 weeks of acute CBT and medication treatment to determine whether the use of specific CBT treatment components is associated with depression response in this seriously depressed sample of adolescents. Specific aims included the following: (a) to evaluate whether the receipt of more sessions (i.e., higher dose) relates to better outcomes and (b) to identify CBT components associated with overall treatment response.
On the basis of the existing literature, our primary hypothesis was that the receipt of more CBT sessions would result in greater rates of response and that cognitive restructuring, problem solving, and behavioral activation components of treatment would be associated with positive outcomes. Furthermore, as this was a treatment-resistant population, we predicted that emotion regulation would be associated with better response rates.
Method
A detailed description of the study design, inclusion and exclusion criteria, Consolidated Standards of Reporting Trials (CONSORT) diagram, and 12-week outcome are presented elsewhere (Brent et al., 2008). Key study features are reviewed briefly here, to the extent that they influence the aims of this secondary analysis.
Participants
All participants had clinically significant depression at enrollment—defined as a total score of ≥40 on the Children’s Depression Rating Scale—Revised (CDRS-R; Poznanski & Mokros, 1996) and a score of ≥4 on the Clinical Global Impression—Severity scale (CGI-S; Guy, 1976) in addition to meeting criteria from the Diagnostic and Statistical Manual for Mental Disorders (4th ed. [DSM–IV]; American Psychiatric Association, 1994) for major depressive disorder as measured by the Schedule for Affective Disorders and Schizophrenia for School-Age Children–Present and Lifetime Version (Kaufman et al., 1997). Enrolled youths had been nonresponsive to an adequate treatment with an SSRI for at least 6 weeks (defined as a dosage the equivalent of 20 mg of fluoxetine) and a final 2 weeks at a dosage equivalent to 40 mg of fluoxetine, unless this dose could not be tolerated. Exclusion criteria were the following: completing ≥2 adequate SSRI trials; history of nonresponse to an adequate trial of venlafaxine; prior trial of ≥7 sessions of CBT; or prescribed medications with psychoactive properties but permitting some study medications, which included medications in the stimulant, hypnotic (trazadone, zolpidem, zaleplon), and antianxiety (clonazepam, lorazepam) classes at stable doses (≥12 weeks duration). In addition, those youths with diagnoses of Bipolar I or II, psychosis, autism, eating disorders, substance abuse or dependence; hypertension (diastolic blood pressure of ≥90); and female adolescents who were pregnant, breast-feeding, or not reliably using contraception were excluded from study participation. The study was approved by each site’s local Institutional Review Board (IRB); all participants gave informed assent (and informed consent after turning 18 years of age), and parents gave informed consent in accordance with local IRB regulations.
Participants were randomly assigned to one of four treatments: (a) change to second SSRI; (b) change to venlafaxine; (c) change to a second SSRI combined with CBT; or (d) change to venlafaxine combined with CBT. Randomization was balanced both within and across sites on incoming treatment medication, comorbid anxiety, chronic depression (duration of ≥24 months), and suicidal ideation (Beck Depression Inventory–II [BDI-II]; Beck, Steer, & Brown, 1996; a score of ≥2 on Item 9). In the primary investigation (Brent et al., 2008), no differences were found in outcomes following a medication switch to venlafaxine versus a second SSRI; thus, we combined the CBT cells for this secondary analysis. Therefore, all 166 participants were receiving both CBT and antidepressant medication treatment.
Cognitive–Behavioral Therapy
Content and adherence
The CBT treatment administered in the TORDIA study was based on several treatment manuals, including the TADS manual (Curry et al., 2000; Wells & Curry, 2000), the Coping With Depression for Adolescents Course (CWD-A; Lewinsohn, Clarke, Hops, & Andrews, 1990), and the Cognitive Therapy Manual for Depressed and Suicidal Youth (Brent & Poling, 1997). The TORDIA CBT manual emphasized cognitive restructuring, behavioral activation, emotion regulation, social skills, and problem-solving components for the individual patient, along with family sessions, with a focus on decreasing family conflict and criticism and improving family communication and problem solving. The treatment modules were flexibly applied on the basis of the individual and clinical needs of the participant and family. This was a necessary and important adaptation, as these participants were by definition treatment resistant and had failed prior medication treatment for their depressive illness. The TORDIA CBT manual included guidance for the therapist on how to balance adherence to the protocol with the flexibility required to address the youth’s individual needs through the selection of specific modules. Therapists were of master’s level or above, had prior experience in conducting CBT, and were supervised by a site supervisor as well as an external supervisor who reviewed case formulations and treatment progress on a conference call held every other week. The CBT protocol called for 12 sessions (of 60 to 90 min each) during the first 12 weeks of treatment, of which 3 to 6 could be family sessions.
Therapists attended a 2-day training meeting at the beginning of the study and again at the midpoint of the study. On-site and off-site supervisors audiotaped and rated CBT sessions using the Cognitive Therapy Rating Scale (CTRS; Vallis, Shaw, & Dobson, 1986), with 94% of sessions rated as acceptable (CTRS score of ≥39; Brent et al., 2008). On-site ratings were completed by site supervisors (277 tapes), whereas off-site review consisted of ratings by two CBT supervisors at the coordinating site in Pittsburgh, Pennsylvania (351 tapes) and ratings by an external consultant affiliated with the Beck Cognitive Therapy Center, Philadelphia, Pennsylvania (49 tapes). The first two sessions for each therapist (a total of six tapes) were reviewed. If these were rated as satisfactory (CTRS score of ≥39) by both the on-site reviewer and the Pittsburgh reviewer, additional tapes for review were selected at random.
Cognitive–behavioral therapy taxonomy
A total of 22 separate CBT modules were included in the TORDIA manual; however, many of these modules were based on similar theoretical principles. For example, the Assertiveness module and the Communication and Compromise module were both elements of a broader behavioral social skills approach. We explored empirical methods of creating metacategories for the 22 different CBT modules. A Jaccard proximity score was calculated for each possible pair of modules, and we examined the probability of receiving both modules given that the patient had received either one of them (Aldenderfer & Blashfield, 1984). Out of the 253 possible pairs, only six had a probability score of greater than 0.65 indicating that, for most of these clusters, we were unable to find significant indications of frequent co-delivery of modules within a given metadomain. In retrospect this is not surprising, given that this CBT approach was intentionally multimodal and that therapists were encouraged to take a breadth approach to exposing youths to skills across several domains. This therapeutic strategy would not lead to a pattern of high co-delivery of modules within each meta-category. Given that empirical methods did not create clear clusters by therapist use, we returned to theory and categorized modules on the basis of their underlying purpose. Our final categorization of nine core components (see Table 1) closely conforms to the coding systems used in previous studies of CBT manual content (McCarty & Weisz, 2007; Weersing et al., 2009). Note that we chose to cluster individual and family versions of the same core skill together rather than classifying modules by whether they were family or individual sessions.
Table 1.
Cognitive–Behavioral Therapy Taxonomy of Treatment of SSRI-Resistant Depression in Adolescents (TORDIA) Modules
| TORDIA module | Description of module | Treatment component |
|---|---|---|
| Psychoeducation | Defining depression; causes; benefits of treatment | General therapy processes |
| Taking stock | Identifying helpful skills, progress made, work still to be done | |
| Mood monitoring | Self-rating of daily mood; evaluating progress over time | |
| Automatic thoughts and cognitive distortions | Identifying unrealistic thoughts and underlying beliefs; examining evidence for and against; testing reality of beliefs | Cognitive restructuring |
| Realistic counter-thoughts | Creating and implementing realistic alternatives to unrealistic thoughts and beliefs | |
| Increasing pleasant activities | Selecting target activities; establishing baseline; setting small, incremental goals; self-reward for meeting goals | Behavioral activation |
| Reengagement | Overcoming inertia and avoidance; reengagement in reinforcing activities | |
| Emotion regulation | Interrupting chain of events leading to distressing emotions; self-soothing | Emotion regulation |
| Relaxation | Progressive muscle relaxation, deep breathing, imagery to reduce tension | |
| Family emotion regulation | Introducing emotion regulation skills to the family | |
| Assertion | Avoiding passivity and aggressiveness; “I” statements | Social skills |
| Communication and compromise | Active listening and reflecting; negotiation and conflict resolution | |
| Social interaction | Starting conversations, joining groups, listening | |
| Family communication | Reducing blame, clearly identifying objective problems/goals without name calling, increasing trust, active listening, and reflecting | |
| Problem solving | Operationalizing problems/goals; brainstorming solutions; seeking compromise; evaluating | Problem solving |
| Family problem solving | Introducing problem-solving skills to the family | |
| Family high expectations and positive reinforcement | Managing high expectations; strategies for positive reinforcement | Family-oriented components |
| Family contingency management | Introducing behavioral contracting between the child and family | |
| Family attachment and commitment | Helping parents identify strengths and positive attributes of the child; planning positive interactions | |
| Motivational interviewing | Pros/cons of alternative choices; readiness for change | Motivational interviewing |
| Relapse prevention | Self-monitoring, action plan for relapse | Relapse prevention |
| Family relapse prevention | Involving family in relapse prevention planning |
Note. SSRI = selective serotonin reuptake inhibitor.
Measures
Baseline inclusion
All participants were diagnosed by structured interview with the Schedule for Affective Disorders and Schizophrenia for School-Age Children—Present and Lifetime Version (Kaufman et al., 1997). At baseline, family demographic characteristics, adolescent self-report of symptoms, and parent reports of their own symptoms were assessed as well (see original TORDIA report for details).
Treatment response
The primary outcome of treatment response was based jointly on the Children’s Depression Rating Scale—Revised (CDRS-R; Poznanski & Mokros, 1996) and the Clinical Global Impressions—Improvement (CGI-I; Guy, 1976). The CDRS-R, a measure of depression symptom severity based on separate interviews of the child and parent, was completed by the independent evaluator, who was uninformed of the treatment assignment. This is a 17-item scale, which results in total scores ranging from 17 to 113, with a total score of 40 or greater indicating significant depression (Poznanski & Mokros, 1996). The CGI-I is a measure of clinical improvement, as rated by the independent evaluator on a scale of 1 (very much improved) to 7 (very much worse; Guy, 1976). “Adequate clinical response” at Week 12, was defined as a 50% reduction in CDRS score and a CGI-I score of 2 or less. Responses were evaluated by an independent evaluator.
Implementation delivery covariates
We also planned to statistically control for several potentially important covariates: number of CBT treatment sessions and site.
Analytic Plan
We used the Statistical Package for Social Sciences (SPSS 14.0) and STATA 9.2 to conduct all statistical analyses. For hypothesis generation value, alpha level was set at .05.
Intervention delivery
As a first step, we began by examining descriptive statistics on intervention delivery, including the frequency of use of each of the nine CBT core components. In this analysis, we also sought to identify sample-wide covariates of intervention delivery and treatment response in order to adjust analyses appropriately in later stages.
Treatment response
We conducted a Pearson chi-square analysis, using a median split, to examine whether number of session, was associated with response to treatment. Next, baseline differences between youths who received numbers of sessions above and below the median were examined with Pearson chi-square analysis and independent sample t test. Subsequently, we calculated the odds ratio (OR) for response, adjusting for these baseline differences and site.
Similarly, we conducted Pearson chi-square analyses to examine whether receipt of each of the nine components was significantly associated with the primary outcome (i.e., response to treatment). Using Pearson chi-square analysis and independent sample t test, we investigated baseline differences between youths who did and did not receive each of the nine components. Subsequently, these baseline differences, in addition to site and total number of CBT sessions were used in multivariate logistic regression models to calculate the adjusted OR for response associated with the use of each of the nine components. We controlled for those variables that were significantly associated with certain components to ensure that an association between the outcome and response, if it existed, was due to the component itself rather than confounding factors. Finally, to examine dose effect, responders and nonresponders were compared, using an independent sample t test, on the number of times they received each component.
Results
Details regarding the 166 participants are outlined in Table 2. As can be seen in the table, the majority of the sample was White and female and their average age was 16 years. The mean baseline CDRS, CGI-S, and CGAS scores indicated significant impairment. The average age of onset of major depressive disorder was 12.9 years (SD = 2.4), and the duration of the current major depressive episode averaged almost 2 years. At Week 12, the response rate was 54.8, the average CDRS score was 38.12 (SD = 14.51), and the average CGI-I score was 2.51 (SD = 1.13).
Table 2.
Baseline Characteristics
| Characteristic | Cognitive–behavioral therapy (n = 166) |
|---|---|
| Demographic characteristics | |
| Age in years: M (SD) | 16.0 (1.5) |
| Racial background: n (%) | |
| Asian | 4 (2.4) |
| Black | 6 (3.6) |
| Biracial | 3 (1.8) |
| Hispanic | 11 (6.6) |
| White | 141 (84.9) |
| Other | 1 (0.6) |
| Female sex: n (%) | 116 (69.9) |
| Income in U.S. dollars: n (%) | |
| 0–10,000 | 4 (2.8) |
| 10,001–20,000 | 4 (2.8) |
| 20,001–30,000 | 13 (9.1) |
| 30,001–40,000 | 21 (14.7) |
| 40,001–50,000 | 23 (16.1) |
| 50,001–60,000 | 10 (7.0) |
| 60,001–70,000 | 10 (7.0) |
| 70,001–80,000 | 18 (12.6) |
| 80,001–90,000 | 9 (6.3) |
| 90,001–100,000 | 7 (4.9) |
| 100,000+ | 24 (16.8) |
| Parent/guardian education: n (%) | |
| Junior high | 4 (2.5) |
| Some high school | 8 (5.1) |
| High school graduate | 27 (17.2) |
| Some college | 42 (26.8) |
| College degree | 34 (21.7) |
| Graduate/professional training | 42 (26.8) |
|
| |
| Clinical characteristics | |
| Children’s Depression Rating Scale—Revised: M (SD) | 59.2 (11.0) |
| Clinical Global Impressions—Severity: M (SD) | 4.5 (0.7) |
| Children’s Global Assessment Scale: M (SD) | 50.6 (7.7) |
| Beck Depression Inventory: M (SD) | 21.4 (12.6) |
| Comorbidity: n (%) | |
| Anxiety (excluding posttraumatic stress disorder) | 53 (33.1) |
| Posttraumatic stress disorder | 9 (5.5) |
| Attention deficit hyperactivity disorder | 29 (17.7) |
| Oppositional defiant disorder/conduct disorder | 15 (9.2) |
| Dysthymia | 47 (28.7) |
|
| |
| Clinical history | |
| First episode of depression: n (%) | 119 (74.4) |
| Duration current major depressive episode in months: M (SD) | 22.3 (19.4) |
| Age at onset of major depressive disorder symptoms in years: M (SD) | 12.9 (2.4) |
| History of suicide attempts: n (%) | 35 (21.1) |
Intervention Delivery
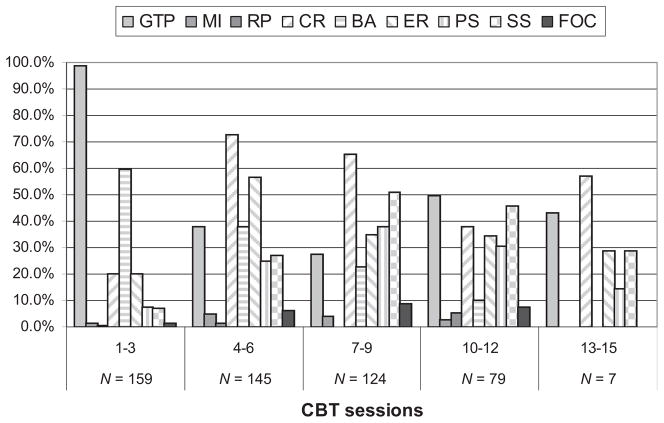
We began by exploring receipt of CBT components over treatment and examining important covariates of intervention delivery. Twelve planned CBT sessions were to be delivered over a 12-week period, three to six of which were to include parents. Up to three additional sessions were available to address emergent clinical needs. A mean of 8.3 sessions was actually delivered (SD = 3.6; Mdn = 9; range = 0–15), with no difference by medication group (Brent et al., 2008). The mean number of family sessions was 1 (range = 0–7). Table 3 presents the treatment components delivered across these sessions and the frequencies of the participants who received them. The most frequently delivered group of modules was general therapy processes (95.2%), followed by cognitive restructuring (78.9%), behavioral activation (72.3%) and emotion regulation (66.9%). Very few participants received motivational interviewing (8.4%) or relapse prevention (4.2%); therefore, these components were not included in the remaining analyses. With regard to the timing of CBT sessions, within the first three sessions, 98.7% of the participants received general therapy process modules and 60% received the behavioral activation component (Figure 1). In Sessions 4 through 6, the majority of participants received cognitive restructuring (72%) and emotion regulation (56.6%) components. Cognitive restructuring was used frequently in Sessions 7 through 9 (65% of the participants) along with social skills (50.8%), problem solving (37.9%), and emotion regulation (34.7%) components. In the last three sessions (10–12), the most commonly administered modules were general therapy process and social skills (49.4% and 45.6%, respectively). Seven participants needed an extra one to three sessions to address emergent clinical issues, in which general therapy process and cognitive restructuring were the most used components.
Table 3.
Frequency of Delivery of Cognitive–Behavioral Therapy (CBT) Components
| CBT component | No. participants receiving component | % Participants in trial receiving component | No. sessions that included the component M (SD) | No. times the component was useda M (SD) |
|---|---|---|---|---|
| General therapy process | 158 | 95.2 | 3.0 (1.7) | 3.5 (2.1) |
| Cognitive restructuring | 131 | 78.9 | 2.4 (2.1) | 2.9 (2.8) |
| Behavioral activation | 120 | 72.3 | 1.5 (1.4) | 1.5 (1.5) |
| Emotion regulation | 111 | 66.9 | 1.6 (1.8) | 1.7 (2.1) |
| Social skills | 90 | 54.2 | 1.3 (1.7) | 1.5 (2.5) |
| Problem solving | 86 | 51.8 | 0.9 (1.3) | 1.0 (1.5) |
| Family-oriented component | 20 | 12.0 | 0.2 (0.6) | 0.2 (0.7) |
| Motivational interviewing | 14 | 8.4 | 0.1 (0.5) | 0.1 (0.5) |
| Relapse prevention | 7 | 4.2 | 0.0 (0.2) | 0.0 (0.2) |
More than one module of the same component could have been used in the same session.
Figure 1.
Distribution of cognitive–behavioral therapy components by session number. GTP = general therapy process; MI = motivational interviewing; RP = relapse prevention; CR = cognitive restructuring; BA = behavioral activation; ER = emotion regulation; PS = problem solving; SS = social skills; FOC = family-oriented component.
Number of Sessions and Response to Treatment
Using a median split (9 sessions), we found that attending more than 9 CBT sessions was significantly associated with treatment response (OR = 2.6, 95% confidence interval [CI] = 1.4–4.9, p = .01), site, χ2(1) = 11.1, p = .05, and parental BDI score at baseline: M = 10.8, SD = 10.5, for 0–9 sessions vs. M = 7.9, SD = 7.6, for >9 sessions, t(145.60) = 1.96, p = .05. Number of CBT sessions was not associated with any other baseline demographic or clinical characteristics. Controlling for parental BDI score and site, we found that participants who had completed more than nine sessions were 2.5 times more likely to have adequate response as compared with those who had nine or fewer sessions (95% CI = 1.2–5.0).
Cognitive–Behavioral Therapy Components and Response to Treatment
In an unadjusted analysis, receipt of general therapy process, behavioral activation, emotion regulation, or the family-oriented component was not associated with response to treatment (Table 4). On the other hand, cognitive restructuring, problem solving, and social skills components were significantly positively associated with response to treatment. Further analyses were conducted that adjusted for the site, total number of CBT sessions, and baseline differences in clinical characteristics between those who received a specific CBT component and those who did not. As in the unadjusted analyses, the general therapy process, behavioral activation, emotion regulation, and family-oriented components remained unassociated with adequate response after adjusting for baseline differences between groups. Moreover, the effects for cognitive restructuring were no longer significant after controlling for baseline nonsuicidal self-injury, which differed between groups who did and did not receive cognitive restructuring. In contrast, the adjusted odds of response given receipt of social skills was 2.6 (95% CI = 1.1–6.5) after controlling for baseline differences in gender, race, attention deficit hyperactivity disorder, and nonsuicidal self-injury. The effect of problem solving on response also remained significant (OR = 2.3, 95% CI = 1.1–5.0) after controlling for number of sessions and site. As there were no baseline differences between participants who received and who did not receive the problem-solving module, we did not control for any participant characteristics. Moreover, there was no significant interaction between number of sessions and any of the above-mentioned components on treatment response. Therefore, there was no evidence of a “dose × technique” effect, as there was no relationship between the number of times a participant received a particular module and outcome (ps = .17–.96).
Table 4.
Response Rates Associated With Cognitive–Behavioral Therapy (CBT) Components Received
| CBT component | Not receiving corresponding component n (%) | Receiving corresponding component n (%) | p | Adjusted OR (95% CI, p) |
|---|---|---|---|---|
| General therapy process | 2 (25.0) | 89 (56.3) | .14 | 0.7 (0.1–5.3, .73)a |
| Cognitive restructuring | 13 (37.1) | 78 (59.5) | .02 | 0.6 (0.2–2.2, .50)b |
| Behavioral activation | 23 (50.0) | 68 (56.7) | .48 | 0.5 (0.2–1.2, .13)c |
| Emotion regulation | 33 (60.0) | 58 (52.3) | .34 | 0.5 (0.2–1.2, .12)d |
| Social skills | 34 (44.7) | 57 (63.3) | .02 | 2.6 (1.1–6.5, .04)e |
| Problem solving | 34 (42.5) | 57 (66.3) | <.01 | 2.3 (1.1–5.0, .03) |
| Family-oriented component | 78 (53.4) | 13 (65.0) | .33 | 0.6 (0.2–2.0, .37)f |
Note. The odds ratios (ORs) are adjusted for site, total number of CBT sessions, and baseline differences.
Age and nonsuicidal self-injury.
Nonsuicidal self-injury.
Gender and history of suicide attempt.
Drug Use Screening Inventory (Kirisci, Mezzich, & Tarter, 1995), anxiety, and parents’ education.
Gender, race, attention deficit hyperactivity disorder, and nonsuicidal self-injury.
Age, gender, the Conflict Behavior Questionnaire—Adolescent (Robin & Foster, 1989), the Beck Depression Inventory (Beck et al., 1996), the Beck Hopelessness Scale (Beck & Steer, 1988), nonsuicidal self-injury, and duration of current episode.
Discussion
The TORDIA randomized controlled trial demonstrated favorable outcomes for depressed adolescents who received CBT in combination with medication compared with youths who received medication switch alone (Brent et al., 2008). A detailed presentation of specific clinical outcomes by treatment group is presented in the main outcome article (Brent et al., 2008). In this secondary analysis of participants receiving the combination of medication management and CBT, we found evidence that both CBT dose and specific components of the CBT treatment were associated with a more favorable treatment response. Youths receiving an adequate treatment dose (defined as >9 CBT sessions) had better outcomes, as did youths who received the social skills and problem-solving modules.
The TORDIA CBT treatment was designed to be tailored to the clinical needs of the participant. The majority of the participants received the cognitive restructuring, behavioral activation, and emotional regulation components in addition to the general treatment components of psychoeducation and mood monitoring. Interestingly, the most effective components, problem solving and social skills, were delivered to only 50% of these participants, predominantly in the later sessions (7 through 9) of treatment. We adjusted for the number of sessions in our outcome analyses, but it appears that those participants who remained in treatment longer were more likely to receive the more effective components of this treatment. This association may be accounted for, at least in part, by participants who withdrew from CBT early on because of poor response or decompensation and thus also had low rates of problem solving and social skills exposure.
Our finding that a greater number of CBT sessions was associated with a greater likelihood of response underscores the importance of receiving an adequate number of sessions in order to attain an adequate clinical response. Lower doses of psychotherapy have been associated with poorer outcomes in community mental health settings (Weersing & Weisz, 2002). In this study, response and number of sessions are confounded, insofar as those who worsened or experienced serious adverse events were often removed from the study, although they were still followed and may have continued to receive CBT. On the other hand, we were unable to demonstrate a dose effect for each specific module (i.e., a dose × technique effect), which may be due to the restricted range of the number of sessions. Thus, although we have conjectured that receipt of fewer numbers of modules in greater dose may be more efficacious than receiving brief encounters with multiple skill approaches (Weersing et al., 2009), it may be that it is not only the dose but that certain modules, such as problem solving and social skills, may be more likely to result in response.
Overall, our findings support the value of problem solving and social skills training for depressed adolescents. Although, these two classes of treatment modules are often used across a range of child and adolescent disorders (e.g. conduct disorders, attention deficit hyperactivity disorder), our data support their value in treating adolescent depression. Moreover, these treatment elements are common to interpersonal psychotherapy, another efficacious intervention of adolescent depression (Mufson, Weissman, Moreau, & Garfinkel, 1999) as well as other successful CBT protocols, such as the CWD-A course (Lewinsohn et al., 1990). Of note, the specific type of CBT used in the major adult chronic depression trial that had significant positive results had a heavy emphasis on interpersonal problem solving, thus social problem solving may be an essential component of effective treatment (Keller et al., 2000). Other treatment studies of adult depression have yielded similar positive effects for problem-solving approaches (Mynors-Wallis, Gath, Day, & Baker, 2000; Nezu, 1986). As previously noted, in the TORDIA study, only 51.8% of participants received the problem-solving component and 54.2% of participants received the social skills component. Whereas CBT had a favorable impact on treatment outcome in the overall study, one wonders if the CBT response rates would have been even higher if more participants had received problem solving and social skills training.
There are several limitations of this study. First, modules were not assigned randomly but instead were selected on the basis of patient and family characteristics, and adolescent (substance use, nonsuicidal self injury) and family (CBQ-A) variables associated with use of the family, emotion regulation, and motivational interviewing modules were also related to poor outcome (Asarnow et al., 2009a). The impact of specific modules is confounded by dose and order effects. CBT dose (number of sessions) as well as specific module exposure are associated with treatment outcomes, and we cannot separate dose from receipt of module. Similarly, the infrequency of certain components (e.g., motivational interviewing, relapse prevention) precludes our ability to draw conclusions about the effectiveness or ineffectiveness of receiving these interventions. Moreover, whereas we have ratings of overall quality of treatment, we do not have module-specific ratings of quality. In addition, the TORDIA represents a subset of depressed adolescents (i.e., those with chronic, treatment-resistant depression) and thus may not be generalizable to depressed adolescents as a whole. In addition, all participants who were receiving CBT were also receiving medication; the results may have been different if this were a monotherapy CBT trial. We believe that these findings generate tangible hypotheses that can be tested in future experimental design.
Finally, recent years have witnessed increased emphasis on disseminating and exporting evidence-based treatments to community practice settings. This trend has been stimulated by observations of a quality gap between research-based treatment and treatments delivered in community practice settings, with poorer outcomes for youths receiving routine community care (Weersing & Weisz, 2002). It is important to adapt research-based treatments to the needs of community practice settings, which treat a more diverse group of participants than those typically enrolled in clinical trials (Asarnow, McKowen, & Jaycox, 2009b). Given the apparent preference for psychosocial treatment versus medication (Asarnow et al., 2005; Jaycox et al., 2006) and the emphasis on evidence-based psychosocial treatment as a first-step treatment for most youths struggling with depression (Birmaher et al., 2007), there is a critical need to identify the key components of effective CBT and the conditions that lead to effective versus ineffective CBT delivery. Given that the TORDIA CBT manual is based on three prominent manuals in the adolescent depression literature—the CWD-A, Pittsburgh cognitive therapy, and the TADS CBT manual—results of this investigation may shed useful light on the broader CBT literature reporting on these common treatment programs. However, more research is needed to further clarify optimal CBT strategies for depressed adolescents, the “active” CBT components, and how to best personalize such approaches and match individual adolescents to the most beneficial CBT strategies. In addition, the strong relationship between dose of psychotherapy and outcome highlights the need to engage adolescents in treatment to increase attendance and continued participation in therapy, whether in research or community settings. Future research is needed to clarify the degree to which the findings in this report are specific to our more treatment-resistant population, characteristics of TORDIA CBT, or other factors.
Acknowledgments
Over the past 24 months, Graham J. Emslie has received research support from the BioBehavioral Diagnostic Company, Forest Laboratories, Shire Specialty Pharmaceuticals, Somerset, and Wyeth Pharmaceuticals and has served as a consultant for the BioBehavioral Diagnostic Company, Eli Lilly, Forest Laboratories, Pfizer Inc. (as a member of the Data Safety Monitoring Board), Shire Specialty Pharamaceuticals, Validus Pharmaceuticals, and Wyeth Pharmaceuticals. Karen D. Wagner has been a consultant and/or served on advisory boards for Forest Laboratories, GlaxoSmithKline, Pfizer, Eli Lilly, and Wyeth Pharmaceuticals. Joan Rosenbaum Asarnow has received unrestricted research funding from Phillip Morris and has consulted regarding cognitive– behavioral therapy and quality improvement.
Contributor Information
Betsy D. Kennard, Department of Psychiatry, University of Texas Southwestern Medical Center at Dallas
Greg N. Clarke, Kaiser Permanente Center for Health Research, Portland, Oregon
V. Robin Weersing, Joint Doctoral Program in Clinical Psychology, San Diego State University and University of California, San Diego.
Joan Rosenbaum Asarnow, Department of Psychiatry and Biobehavioral Sciences, Semel Institute for Neuroscience and Human Behavior, University of California, Los Angeles.
Wael Shamseddeen, Department of Psychiatry, Western Psychiatric Institute and Clinic, Pittsburgh, Pennsylvania, and University of Pittsburgh Medical Center.
Giovanna Porta, Department of Psychiatry, Western Psychiatric Institute and Clinic, Pittsburgh, Pennsylvania, and University of Pittsburgh Medical Center.
Michele Berk, Harbor–UCLA Medical Center and Department of Psychiatry and Biobehavioral Sciences, Semel Institute for Neuroscience and Human Behavior, University of California, Los Angeles.
Jennifer L. Hughes, Department of Psychiatry, University of Texas Southwestern Medical Center at Dallas
Anthony Spirito, Department of Psychiatry and Human Behavior, Brown University.
Graham J. Emslie, Department of Psychiatry, University of Texas Southwestern Medical Center at Dallas
Martin B. Keller, Department of Psychiatry and Human Behavior, Brown University, and Butler Hospital, Providence, Rhode Island
Karen D. Wagner, Department of Psychiatry, University of Texas Medical Branch at Galveston
David A. Brent, Department of Psychiatry, Western Psychiatric Institute and Clinic, Pittsburgh, Pennsylvania, and University of Pittsburgh Medical Center
References
- Aldenderfer MS, Blashfield RK. Cluster analysis. Newbury Park, CA: Sage; 1984. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual for mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- Asarnow JR, Emslie GJ, Clarke G, Wagner KD, Spirito A, Vitiello B, et al. Treatment of selective serotonin reuptake inhibitor–resistant depression in adolescents: Predictors and moderators of treatment response. Journal of the American Academy of Child and Adolescent Psychiatry. 2009a;48:330–339. doi: 10.1097/CHI.0b013e3181977476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asarnow JR, Jaycox LH, Duan N, LaBorde AP, Rea MM, Murray P, et al. Effectiveness of a quality improvement intervention for adolescent depression in primary care clinics: A randomized controlled trial. Journal of the American Medical Association. 2005;293:311–319. doi: 10.1001/jama.293.3.311. [DOI] [PubMed] [Google Scholar]
- Asarnow JR, McKowen J, Jaycox L. Improving care for depression: Integrating evidence-based depression treatment within primary care services. In: Essau CA, editor. Treatment of adolescent depression. London: Oxford University Press; 2009b. pp. xxx–xxx. [Google Scholar]
- Asarnow JR, Scott CV, Mintz J. A combined cognitive–behavioral family education intervention for depression in children: A treatment development study. Cognitive Therapy and Research. 2002;26:221–229. [Google Scholar]
- Beck AT, Steer RA. Manual for the Beck Hopelessness Scale. San Antonio, TX: Psychological Corporation; 1988. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory–II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Birmaher B, Brent D, Bernet W, Bukstein O, Walter H, Benson RS, et al. AACAP Work Group on Quality Issues. Practice parameter for the assessment and treatment of children and adolescents with depressive disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:1503–1526. doi: 10.1097/chi.0b013e318145ae1c. [DOI] [PubMed] [Google Scholar]
- Brent D, Emslie G, Clarke G, Wagner KD, Asarnow JR, Keller M, et al. Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression: The TORDIA randomized controlled trial. Journal of the American Medical Association. 2008;299:901–913. doi: 10.1001/jama.299.8.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent D, Poling K. Cognitive therapy treatment manual for depressed and suicidal youth. 1997. Unpublished manuscript. [Google Scholar]
- Brent DA, Holder D, Kolko D, Birmaher B, Baugher M, Roth C, et al. A clinical psychotherapy trial for adolescent depression comparing cognitive, family, and supportive therapy. Archives of General Psychiatry. 1997;54:877–885. doi: 10.1001/archpsyc.1997.01830210125017. [DOI] [PubMed] [Google Scholar]
- Chambers DA, Ringeisen H, Hickman EE. Federal, state, and foundation initiatives around evidence-based practices for child and adolescent mental health. Child and Adolescent Psychiatric Clinics of North America. 2005;14:307–327. doi: 10.1016/j.chc.2004.04.006. [DOI] [PubMed] [Google Scholar]
- Craske MG, Roy-Byrne P, Stein MB, Sullivan G, Hazlett-Stevens H, Bystritsky A, et al. CBT intensity and outcome for panic disorder in a primary care setting. Behavior Therapy. 2006;37:112–119. doi: 10.1016/j.beth.2005.05.003. [DOI] [PubMed] [Google Scholar]
- Curry J, Wells K, Brent D, Clarke G, Rodhe P, Albano AM, et al. Cognitive behavior therapy manual for TADS. 2000. Unpublished manuscript. [Google Scholar]
- Dimidjian S, Hollon SD, Dobson KS, Schmaling KB, Kohlenberg RJ, Addis ME, et al. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. Journal of Consulting and Clinical Psychology. 2006;74:658–670. doi: 10.1037/0022-006X.74.4.658. [DOI] [PubMed] [Google Scholar]
- Dobson KS, Hollon SD, Dimidjian S, Schmaling KB, Kohlenberg RJ, Gallop RJ. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the prevention of relapse and recurrence in major depression. Journal of Consulting & Clinical Psychology. 2008;76:468–477. doi: 10.1037/0022-006X.76.3.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edinger JD, Wohlgemuth WK, Radtke RA, Coffman CJ, Carney CE. Dose–response effects of cognitive–behavioral insomnia therapy: A randomized clinical trial. Sleep. 2007;30:203–212. doi: 10.1093/sleep/30.2.203. [DOI] [PubMed] [Google Scholar]
- Guy W, editor. DHEW Publication No ADM 76-388. 2. Washington, DC: U.S. Government Printing Office; 1976. ECDEU assessment manual for psychopharmacology. [Google Scholar]
- Jacobson NS, Dobson KS, Truax PA, Addis ME, Koerner K, Gollan JK, et al. A component analysis of cognitive-behavioral treatment for depression. Journal of Consulting and Clinical Psychology. 1996;64:295–304. doi: 10.1037//0022-006x.64.2.295. [DOI] [PubMed] [Google Scholar]
- Jaycox LH, Asarnow JR, Sherbourne CD, Rea MM, LaBorde AP, Wells K. Adolescent primary care patients’ preferences for depression treatment. Administration and Policy in Mental Health. 2006;33:198–207. doi: 10.1007/s10488-006-0033-7. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for Affective Disorders and Schizophrenia for School-Aged Children—Present and Lifetime Version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Keller MB, McCullough JP, Klein DN, Arnow B, Dunner DL, Gelenberg AJ, et al. A comparison of nefazodone, the cognitive behavioral-analysis system of psychotherapy, and their combination for the treatment of chronic depression. The New England Journal of Medicine. 2000;342:1462–1470. doi: 10.1056/NEJM200005183422001. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Flannery-Schroeder E, Panichelli-Mindel SM, Southam-Gerow M, Henin A, Warman M. Therapy for youths with anxiety disorders: A second randomized clinical trial. Journal of Consulting and Clinical Psychology. 1997;65:366–380. doi: 10.1037//0022-006x.65.3.366. [DOI] [PubMed] [Google Scholar]
- Kirisci L, Mezzich A, Tarter R. Norms and sensitivity of the adolescent version of the drug use screening inventory. Addictive Behaviors. 1995;20:149–157. doi: 10.1016/0306-4603(94)00058-1. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Clarke GN, Hops H, Andrews JA. Cognitive–behavioral treatment for depressed adolescents. Behavior Therapy. 1990;21:385–401. [Google Scholar]
- McCarty CA, Weisz JR. Effects of psychotherapy for depression in children and adolescents: What we can (and can’t) learn from meta-analysis and component profiling. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:879–886. doi: 10.1097/chi.0b013e31805467b3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mufson L, Weissman MM, Moreau D, Garfinkel R. Efficacy of interpersonal psychotherapy for depressed adolescents. Archives of General Psychiatry. 1999;56:573–579. doi: 10.1001/archpsyc.56.6.573. [DOI] [PubMed] [Google Scholar]
- Mynors-Wallis LM, Gath DH, Day A, Baker F. Randomised controlled trial of problem-solving treatment, antidepressant medication, and combined treatment for major depression in primary care. British Medical Journal. 2000;320:26–30. doi: 10.1136/bmj.320.7226.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute of Mental Health. Meeting summary: Benefits, limitations, and emerging research needs in treating youth with depression. 2006 Retrieved from http://www.nimh.nih.gov/research-funding/scientific-meetings/2006/benefits-limitations-and-emerging-research-needs-in-treating-youth-with-depression/summary.shtml.
- Nezu AM. Efficacy of a social problem-solving therapy approach for unipolar depression. Journal of Consulting and Clinical Psychology. 1986;54:196–202. doi: 10.1037//0022-006x.54.2.196. [DOI] [PubMed] [Google Scholar]
- Poznanski E, Mokros H. Children’s Depression Rating Scale—Revised. Los Angeles, CA: Western Psychological Services; 1996. [Google Scholar]
- Robin AL, Foster SL. Negotiating parent–adolescent conflict. New York: Guilford Press; 1989. [Google Scholar]
- Treatment for Adolescents With Depression Study (TADS) Team. Fluoxetine, cognitive–behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents with Depression Study (TADS) randomized controlled trial. Journal of the American Medical Association: Journal of the American Medical Association. 2004;292:807–820. doi: 10.1001/jama.292.7.807. [DOI] [PubMed] [Google Scholar]
- Vallis TM, Shaw BF, Dobson KS. The Cognitive Therapy Scale: Psychometric properties. Journal of Consulting and Clinical Psychology. 1986;54:381–385. doi: 10.1037//0022-006x.54.3.381. [DOI] [PubMed] [Google Scholar]
- Weersing VR, Rozenman M, Gonzalez A. Core components of therapy in youth: Do we know what to disseminate? Behavior Modification. 2009;33:24–47. doi: 10.1177/0145445508322629. [DOI] [PubMed] [Google Scholar]
- Weersing VR, Weisz JR. Community clinic treatment of depressed youth: Benchmarking usual care against CBT clinical trials. Journal of Consulting and Clinical Psychology. 2002;70:299–310. doi: 10.1037//0022-006x.70.2.299. [DOI] [PubMed] [Google Scholar]
- Weisz JR, McCarty CA, Valeri SM. Effects of psychotherapy for depression in children and adolescents: A meta-analysis. Psychological Bulletin. 2006;132:132–149. doi: 10.1037/0033-2909.132.1.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells KC, Curry JF. Cognitive behavior therapy manual for TADS: Parent and conjoint parent–adolescent sessions. 2000. Unpublished manuscript. [Google Scholar]