Short abstract
While various factors have been assumed to affect knee joint biomechanics, few data have been reported on the function of the extensor mechanism in deep flexion of the knee. This study analyzed the patellofemoral joint contact kinematics and the ratio of the quadriceps and patellar tendon forces in living subjects when they performed a single leg lunge up to 150 deg of flexion. The data revealed that in the proximal-distal direction, the patellofemoral articular contact points were in the central one-third of the patellar cartilage. Beyond 90 deg of flexion, the contact points moved towards the medial-lateral edges of the patellar surface. At low flexion angles, the patellar tendon and quadriceps force ratio was approximately 1.0 but reduced to about 0.7 after 60 deg of knee flexion, implying that the patella tendon carries lower loads than the quadriceps. These data may be valuable for improvement of contemporary surgical treatments of diseased knees that are aimed to achieve deep knee flexion.
Keywords: patellofemoral contact, weight-bearing activity, patellar tendon force, quadriceps force, knee biomechanics
1. Introduction
Deep flexion is necessary for normal function of the knee during various daily activities [1]. Achieving deep flexion of the knee is also an objective of contemporary total knee arthroplasty (TKA) [2]. A recent literature review [3] indicated that patients implanted with contemporary TKAs, either conventional or high flexion designs, on average cannot flex their knees beyond 120 deg. Numerous studies have investigated the biomechanics of the knee in deep flexion in order to understand the biomechanical mechanisms that affect knee flexion capabilities. For example, Hefzy et al. [4] investigated deep knee flexion using plane X-rays; Most et al. [5] measured the knee kinematics before and after TKA from full extension to 150 deg of flexion using an in vitro robotic testing system; and Nagura et al. [6] investigated knee motion in deep squatting of normal subjects using a motion analysis method.
However, most previous studies have examined the tibiofemoral joint kinematics in deep flexion of the knee. The mechanisms that affect the deep flexion of the knee are still unclear. Li et al. [7] measured the in situ forces of the anterior cruciate ligament (ACL)/posterior cruciate ligament (PCL) at 150 deg of knee flexion using a cadaveric experimental setup in order to understand the intrinsic biomechanics of the knee in deep flexion. Most et al. [8] and Walker et al. [9] investigated the tibiofemoral joint contact patterns in deep knee flexion using cadaveric specimens. Recently, Kobayashi et al. [10] reported the patellofemoral and patellar tendon kinematics during deep flexion of the knee. While these studies have provided insights into the biomechanical function of the knee in deep flexion, little data has been reported on the function of the extensor mechanism of the knee (the quadriceps-patella-patellar tendon complex) [11]. A properly functioning extensor mechanism has been assumed to play a critical role in deep knee flexion [12].
The objectives of this study are to determine the extensor mechanism kinematics. Specifically, the interaction of the quadriceps, patellofemoral articular contact kinematics, and the patellar tendon was investigated during a single leg lunge up to maximal flexion of the knee in a group of normal human subjects and to quantitatively understand the biomechanics of the extensor mechanism in order to improve the contemporary TKA function.
2. Materials and Methods
Seven healthy human subjects (age, 23–49; five male and two female) with no history of knee injuries or chronic knee pain were recruited. Each subject signed a consent form approved by our institutional review board. One knee of each subject was imaged using a 3.0T magnetic resonance imaging (MRI) scanner (Siemens, Malvern, PA) with a fat suppressed 3D spoiled gradient recalled sequence. Sagittal images were captured in a 180 × 180 mm field of view with a 1 mm thickness and a resolution of 512 × 512 pixels. These images were used to create a 3D anatomical model of the knee using a solid modeling software (Rhinoceros, Robert McNeel & Assoc., Seattle, WA). Bony surfaces of the femur, tibia, and patella and their articular cartilage surfaces were segmented from the magnetic resonance (MR) images [13]. The patellar tendon insertion sites at the tibial tubercle and the distal patella were also segmented [14].
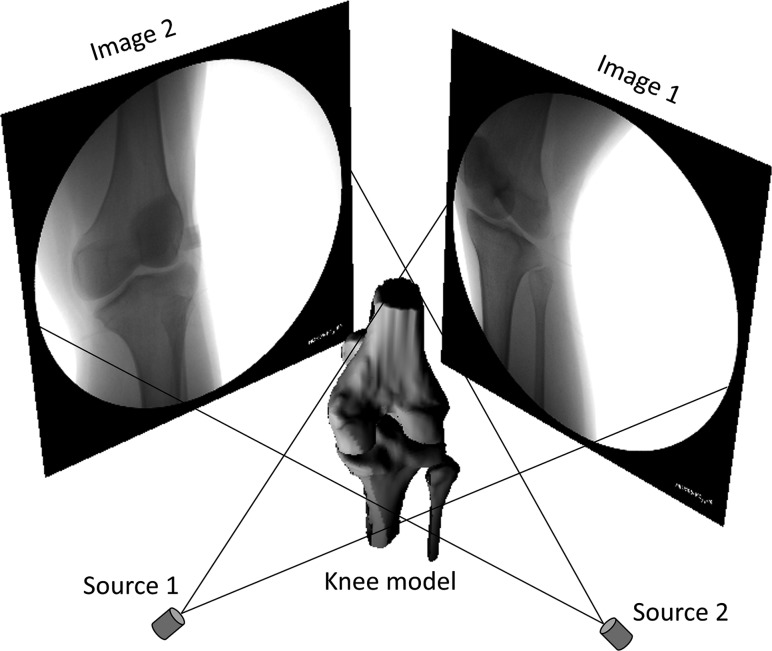
After MR image scanning, each subject performed a single leg bend up to maximum flexion in the field of view of two orthogonally positioned fluoroscopes (BV Pulsera; Philips, Bothell, WA). The subjects were instructed to hold the position for a second at each selected angle and allowed to use the contralateral leg and a handrail to keep body balance if the subject felt necessary. Flexion angles of the knee were monitored with a goniometer. The orthogonal fluoroscopic images and the 3D bony models of the femur, tibia, and patella were imported into a virtual system that replicated the orthogonal fluoroscopy system in the solid modeling software (Fig. 1) [13,15]. The outline of each bone was extracted from the fluoroscopic images. The projection of each 3D bony model was matched to its corresponding outlines on the fluoroscopic images to reproduce the 3D position of the model in space. This technique has been validated previously for the measurement of tibiofemoral joint kinematics [16] and for patellar tracking [17].
Fig. 1.
A virtual dual fluoroscopic image system
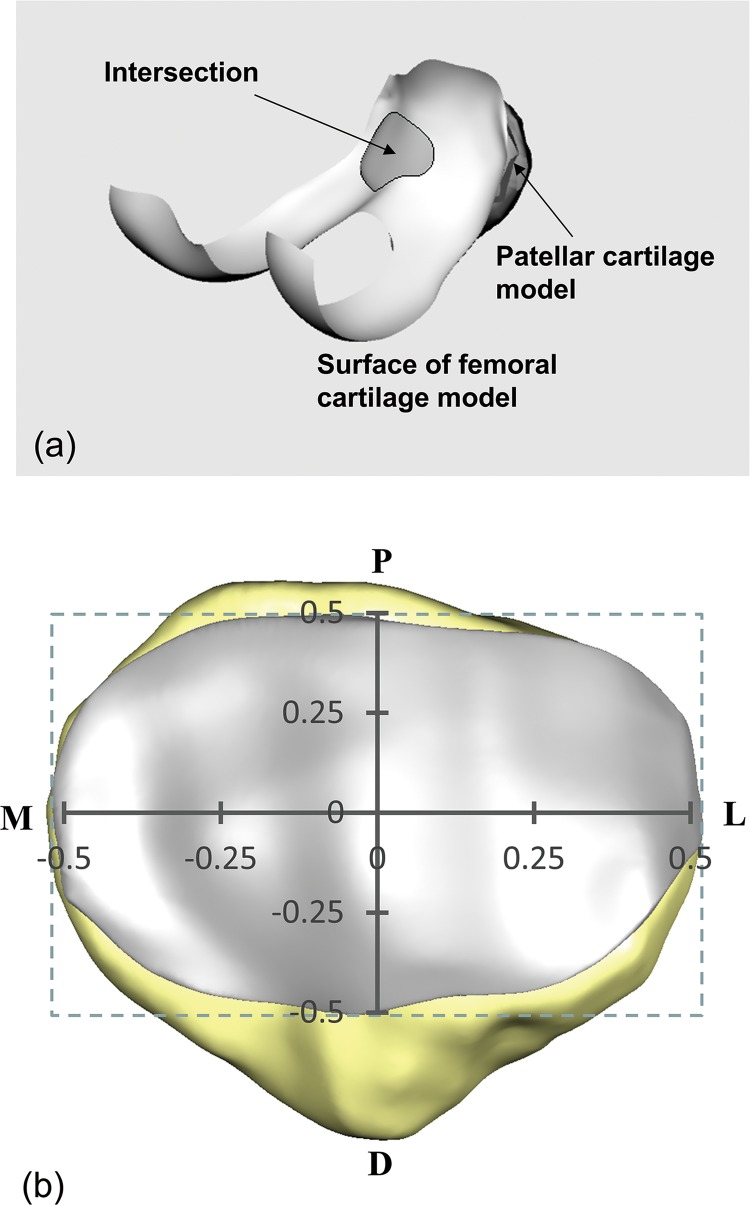
From the series of models used to reproduce knee motion, the relative positions of the cartilage layers on the femur and patella were determined [18]. The overlap of the two cartilage layers was used to approximate the cartilage contact area (Fig. 2(a)). The centroid of this contact area was defined as the contact point. To describe the motion of the contact point on the patella, a coordinate system was created by fitting a rectangle to the patellar cartilage (Fig. 2(b)). The center of the rectangle was the origin of the coordinate system. The vertical axis corresponded the proximal-distal direction and the horizontal axis the medial-lateral direction. A contact point was positive if it was on the proximal side and on the lateral side. Absolute coordinate values of the contact point positions were normalized to the length of corresponding face of fitted rectangular and reported in percentage (%). A previous validation study showed an accuracy of 14% when this technique was used to measure the cartilage contact area [19].
Fig. 2.
(a) Intersection of the patellar and femoral cartilage models. (b) The coordinate system on the patellar articular surface to determine the patellofemoral contact locations.
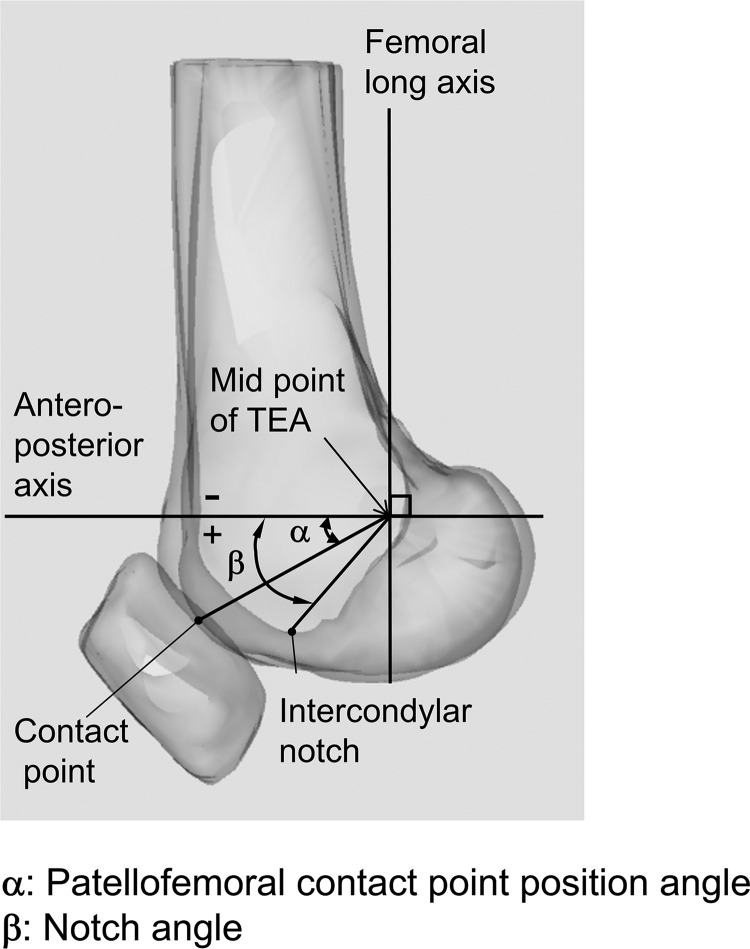
The extensor mechanism during deep knee bend was analyzed on the femoral or patellar sagittal plane by tracking the contact point location as well as the orientation changes in the quadriceps and patellar tendon (Fig. 3). When there are two patellofemoral contact points in a deep knee flexion angle, the point between the projections of these two points on the femoral or patellar sagittal plane was defined as the sagittal plane patellofemoral contact point at this flexion angle. To describe the motion of the contact points on the surface of the femur, a line connecting the middle point of the transepicondylar axis (TEA) and the contact point was projected on the sagittal plane of the femur. The angle between the projected line and the anteroposterior axis, which was perpendicular to the femoral long axis, was defined as the contact position angle (α, Fig. 4). A positive angle indicated that the contact point was below the anteroposterior axis, and a negative angle meant that the contact point was above the anteroposterior axis. The notch angle was defined as an angle formed by the anteroposterior axis and the projection of the line connecting the middle point of the TEA and the intercondylar notch (β, Fig. 4).
Fig. 3.
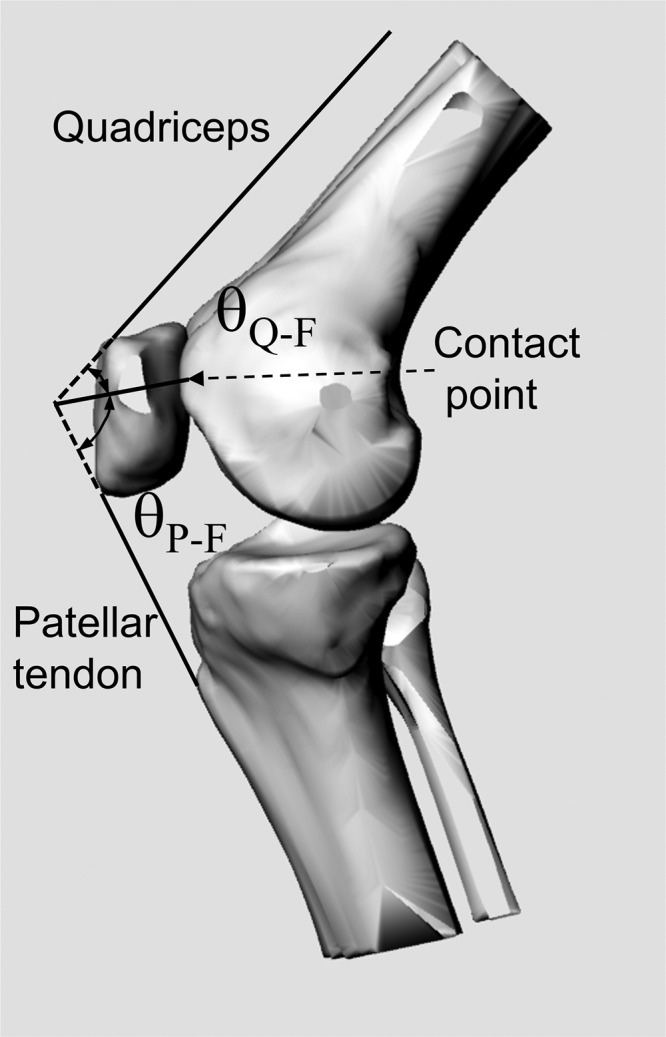
Definitions of the angle between the quadriceps and the direction of the patellofemoral joint reaction force (θQ − F) and the angle between the patellar tendon and the direction of the patellofemoral joint reaction force (θP − F)
Fig. 4.
Definitions of the contact position angle (α) and the notch angle (β)
The attachment sites of the patellar tendon on the patella and tibial tubercle were represented by their corresponding centroids. The line connecting the two attachment sites was used to represent the patellar tendon direction (Fig. 3). If the line intersected with the tibial bony surface, a line tangential to the intersected tibial bony surface was drawn from each attachment site to represent the effect of the tendon wrapping on the bone [10].
The orientation of the quadriceps was assumed to be parallel to the femoral shaft since the MRI could not capture the entire quadriceps from their origins to insertions. The quadriceps were represented using a straight line starting from the centroid of the attachment site on the patella and running parallel to the femoral shaft. If this line contacted with the distal femoral articular surface at deep flexion angles, the line was redrawn from the attachment site on the patella to the contact point on the femoral articular surface. The projection of the quadriceps line on the patellar sagittal plane was extended distally, and the projection of the patellar tendon line was extended proximally. The intersection of the quadriceps and the patellar tendon lines was, thus, determined in the sagittal plane (Fig. 3). A line connecting this intersection and the contact point was considered as the direction of the joint reaction force [11,20,21]. An angle between the quadriceps and the direction of the patellofemoral joint reaction force was defined as the quadriceps angle (θQ − F), and that between the patellar tendon and the direction of the patellofemoral joint reaction force was defined as the patellar tendon angle (θP − F). We assumed that muscle forces are along a vector parallel to the geometric angles defined for each muscle in sagittal plane, i.e., the quadriceps force vector is applied parallel to quadriceps angle (θQ−F), the patellar tendon force vector is parallel to its corresponding angle, etc. For patellofemoral contact force, the assumption was that the force is perpendicular to the frontal cartilage surface at the contact point. The ratio of the patellar tendon force (Pf) and the quadriceps force (Qf) was calculated using the theorem of sines, Pf/Qf = sin(θQ − F)/sin(θP − F).
A repeated measures analysis of variance (ANOVA) was used to detect the effect of knee flexion angles on patellofemoral contact kinematics. The Student–Newman–Keuls post hoc test was used to isolate significant differences among the groups. Differences were considered statistically significant when p < 0.05.
3. Results
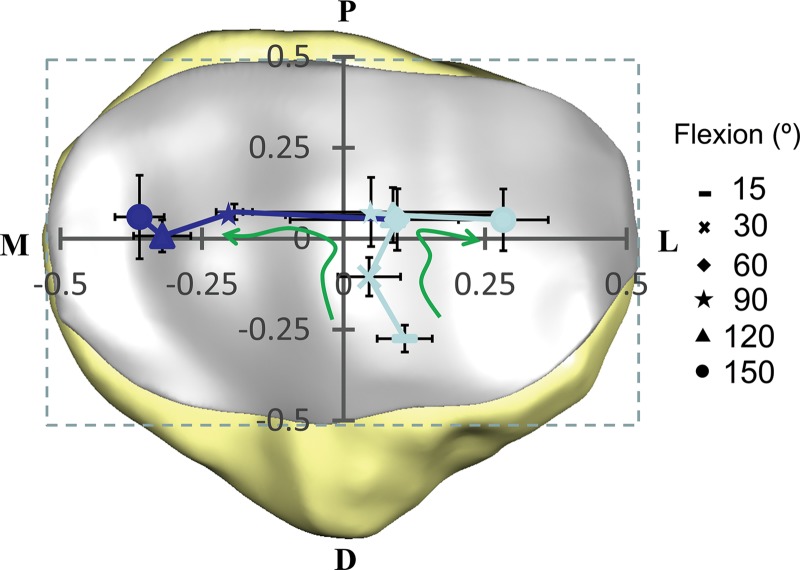
We observed femoral and patellar articular cartilage contact in only three subjects at 15 deg of the knee flexion. Thereafter, we observed the articular contact in all subjects. The patellofemoral contact point on the patella located distolaterally and moved proximally as the flexion angle increased to 90 deg (Fig. 5). The location of the contact point was at −27.5 ± 3.7% in the proximal-distal direction and 10.8 ± 4.9% in the medial-lateral direction at 15 deg of the knee flexion. Beyond 60 deg, separation of the contact was observed in two knees at 90 deg and 120 deg of the knee flexion, and six knees at 150 deg of the knee flexion. The lateral contact point moved laterally and the medial contact point moved medially as the knee flexed to 150 deg, where the lateral contact point was at 5.2 ± 8.5% in the proximal-distal direction and 27.0 ± 7.7% in the medial-lateral direction and the medial contact point was at 6.0 ± 11.5% in the proximal-distal direction and −36.0 ± 4.3% in the medial-lateral direction. The coordinate values of the contact point location at each flexion angle are shown in Table 1. The demography and contact area data of the individual subjects at different flexion angles are shown in the supplementary Appendix.
Fig. 5.
Average locations of the contact points of the seven subjects on the surface of the patellar cartilage at different flexion angles. The data of each subject were normalized to the proximal-distal and medial-lateral dimensions of its patella. The contact started to separate on medial-lateral facets beyond 90 deg of knee flexion.
Table 1.
The locations of the contact points on patella cartilage at different flexion angles (absolute)
|
|
|
Separated |
||
|---|---|---|---|---|
| Flexion angle (deg) | M/L L+ (mm) | P/D P+ (mm) | M/L L+ (mm) | P/D P+ (mm) |
| 15 | 4.5 | −9.0 | ||
| 30 | 1.9 | −3.7 | ||
| 60 | 1.1 | 1.9 | ||
| 90 | 1.9 | 2.7 | −8.9 | 2.2 |
| 120 | 4.4 | 2.2 | −14.1 | 0.0 |
| 150 | 11.7 | 1.8 | −15.7 | 2.1 |
Note: M: medial, L: lateral, P: proximal, D: distal.
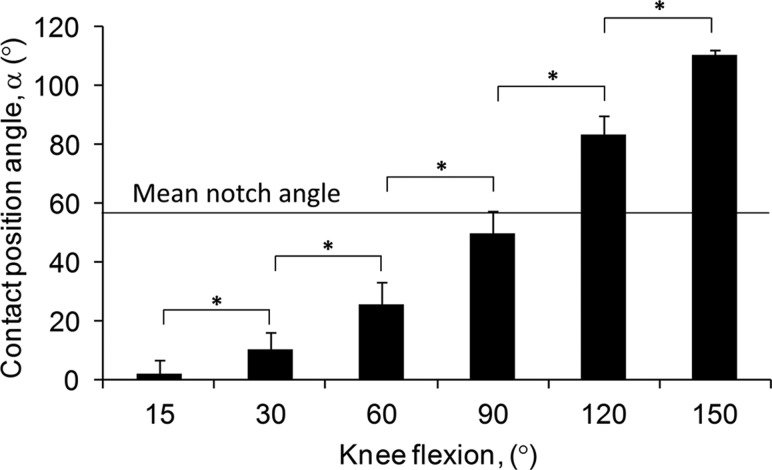
The contact position angle increased (contact point moved distally) consistently with flexion of the knee (p < 0.05, Fig. 6). At 15 deg of knee flexion, the contact point was at 2.1 ± 4.9 deg. The notch angle was 57.2 ± 7.8 deg. At 150 deg of knee flexion, the contact point was at 110.4 ± 2.0 deg. The contact position angle was lower than the knee flexion angle along the flexion path of the knee.
Fig. 6.
The contact position angle and the notch angle. The contact position angle monotonically increased as the knee flexed.
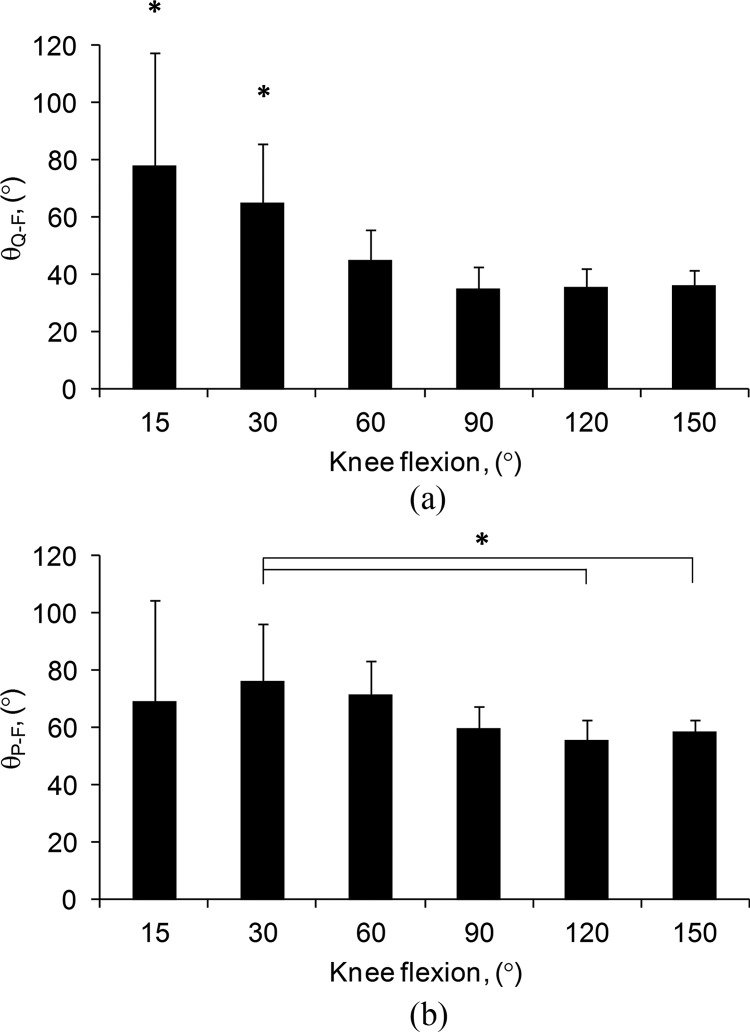
At 15 deg of knee flexion, the sagittal plane angle between the quadriceps and the patellofemoral joint reaction force (θQ − F) was 77.9 ± 39.6 deg (Fig. 7(a)). It decreased to 35.3 ± 7.6 deg as the knee flexed to 90 deg (p < 0.05). Beyond 90 deg, only a slight increase in quadriceps force angle was observed. The sagittal plane angle between the patellar tendon and patellofemoral joint reaction force (θP − F) at 15 deg of knee flexion was 69.5 ± 34.8 deg (Fig. 7(b)). It increased to 76.5 ± 20.1 deg at 30 deg then demonstrated a consistently decrease to 56.0 ± 6.7 deg as the knee flexion angle increased to 120 deg, followed by a slight increase to 58.7 ± 4.1 deg at 150 deg flexion of the knee.
Fig. 7.
(a) The angle between the quadriceps and the direction of the patellofemoral joint reaction force. (b) The angle between the patellar tendon and the direction of the patellofemoral joint reaction force.
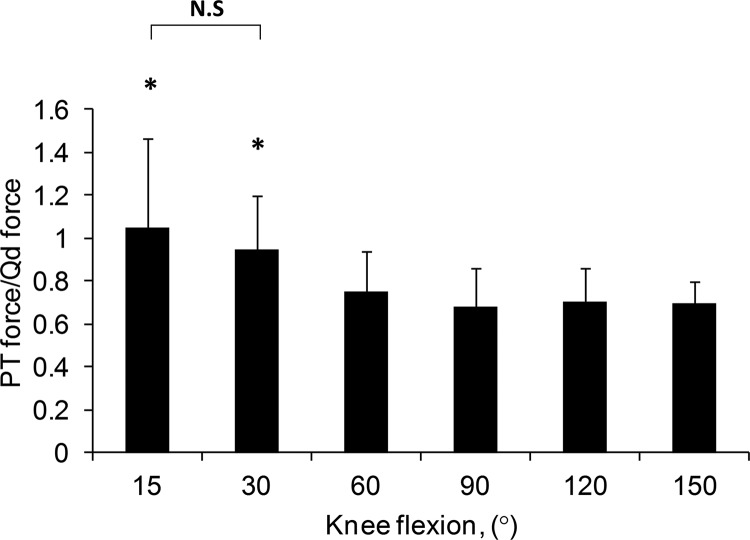
The ratio of the patellar tendon and the quadriceps forces at 15 deg of knee flexion was 1.05 ± 0.41 (Fig. 8). It decreased monotonically to 0.68 ± 0.18 at 90 deg then increased slightly at 120 deg and kept almost constant when the knee flexed to 150 deg.
Fig. 8.
The ratio of the patellar tendon and the quadriceps forces. At 15 deg of knee flexion, the patellar tendon and quadriceps have similar forces. Beyond 60 deg, the patellar tendon carries about 70% of the forces of that in the quadriceps.
4. Discussion
While various factors, such as the shapes of the articulating surfaces and the constraint due to the posterior soft tissues, have been assumed to affect the knee joint biomechanics in deep flexion angle [5,7,9,22], little is known about the function of the extensor mechanism. This study analyzed the patellofemoral joint contact kinematics and the ratio of the quadriceps and patellar tendon forces in living subjects when they performed a single leg lunge to 150 deg of flexion. The data revealed that the patellofemoral articular contact points were in the central one-third of the patellar cartilage in the proximal-distal direction. In general, the patellofemoral contact started to separate on medial-lateral facets beyond 90 deg of knee flexion. At low flexion angles, the patellar tendon and quadriceps have similar forces. However, beyond 60 deg, the patellar tendon carries about 70% of the forces in the quadriceps.
Many studies have reported on the patellofemoral contact locations of the knee in various range of flexion and under various loading conditions [12,23–29]. In general, the contact points of the patellofemoral joint were shown to move proximately from full extension to about 60 deg of flexion and little change in contact locations were observed in proximal-distal direction with further knee flexion. In general, the data of present study are consistent with those published in the literature.
However, our data indicated that beyond 90 deg of flexion, the patellofemoral contact started to separate in the medial and lateral portions. The higher the flexion angles are, the more the contact points tend to move towards the medial and lateral edge of the patellar cartilage surface. In cadaveric experiment setups, Goodfellow et al. [24] showed that the contact area is separated into the medial-lateral zones at 135 deg of flexion; Yildirim et al. [28] and Huberti and Hayes [30] showed that the contact areas are still arcuated bands at 120 deg and more. In an MRI investigation of deep flexion of the knee, Nakagawa et al. [26] showed similar contact location patterns on the patellar surface as to those observed in our study. It should be noted that the patellofemoral cartilage contact pattern is affected by the applied quadriceps load. The differences in the patellofemoral cartilage contact patterns among the reported data may be explained by the differences in quadriceps loads among these studies (including the magnitudes and directions of the loads). The usage of external sensors for measurement of contact area in in vitro studies may also cause alteration in the data measurement [30].
Our previous study showed that in general, the patella shifted laterally and tilted laterally along the flexion path of the knee [10]. After 60 deg of flexion, the patellar shift and tilt were almost constant while the patellar tilted medially at 150 deg. Since our current results showed that the relation between the contact area and the flexion angle varied among the subjects, the correlation between the contact area and the patellar kinematic parameters should be further investigated with force data applied across the patellofemoral joint.
Investigation of in vivo function of the extensor mechanisms is a challenging problem in biomedical engineering. This study analyzed the geometric relationship of the quadriceps-patellar tendon-patella complex in the sagittal plane [11]. At low flexion angles, the contact point was low on the patellar surface, which corresponds to the similar loading levels of the quadriceps and patellar tendon as the patellar tendon and quadriceps force ratio approaches approximately 1.0. As the contact point moved proximally on the patellar cartilage surface, the patellar tendon and quadriceps force ratio decreased and approached approximately 0.7. This information may provide useful implications for investigation of contemporary TKA biomechanics. In contemporary TKA components, while the patellofemoral contact locations have been measured using various techniques [31,32], the effect of the TKA on the function of the quadriceps-patellar tendon-patella complex has not been reported. Further, the patellofemoral contact biomechanics of the knee were not reproduced by the TKAs during flexion [20,33–35]. It is unknown if a physiological quadriceps and patellar tendon ratio could be reproduced in the knee after a TKA implantation. Therefore, it is necessary to quantitatively understand the biomechanics of the extensor mechanism of the knee after TKA in order to improve the contemporary TKA function.
Several limitations in the current study need to be pointed out. The knee was studied in a quasi-static single leg lunge activity. Future study should examine the extensor mechanism function during dynamic deep knee flexion. The function of the quadriceps-patella-patellar tendon complex was analyzed in the sagittal plane of the knee since we could not determine the 3D orientation of the quadriceps force as well as the differences of the contact forces on the medial and lateral patellar facets. Therefore, the contribution of other tissues such as medial-lateral patellar tendon, 3D quadriceps structures, etc. was not considered. In addition, the effects of wraparound of the quadriceps at the distal femur, thigh-calf contact as well as the posterior soft tissues on knee kinematics in deep flexion [26,36,37] were not studied. Despite these limitations, this study provided new data on the extensor mechanism function in deep flexion of the knee in vivo.
In summary, this study investigated the in vivo kinematics of the extensor mechanism of the knee during a single leg lunge activity. The data indicated that the patellofemoral contact point moved proximally with knee flexion up to 60 deg of knee flexion. Thereafter the contact point stays rather constant as flexion angle increases, but beyond 90 deg of flexion, the contact points moved towards the medial-lateral edges of the patellar surface. At low flexion angles, the patellar tendon and quadriceps force ratio was approximately 1.0 but reduced to about 0.7 after 60 deg of knee flexion. These data may be valuable for understanding the intrinsic biomechanics of the knee at deep flexion and providing baseline information for improvement of surgical treatments of diseased knees to achieve postoperative deep knee flexion.
Acknowledgment
This work was supported by a National Institutes of Health Grant R01AR055612 and a Grant-in-Aid for Scientific Research C22560074 by the Japan Society for the Promotion of Science.
Appendix
Table 2.
The demography of the individual subjects
| Subject | Gender | Age, year | Height, m | Weight, kg | Condylar width, mm |
|---|---|---|---|---|---|
| 1 | M | 25 | 1.83 | 68 | 88.1 |
| 2 | M | 23 | 1.73 | 71 | 78.1 |
| 3 | M | 25 | 1.78 | 73 | 84.7 |
| 4 | F | 24 | 1.58 | 49 | 76.1 |
| 5 | F | 29 | 1.80 | 95 | 79.1 |
| 6 | M | 49 | 1.65 | 73 | 81.3 |
| 7 | M | 49 | 1.65 | 73 | 80.3 |
Table 3.
The contact area of the individual subjects at different flexion angles of the knee
|
Subject #1 |
Subject #2 |
|||
|---|---|---|---|---|
| Flexion angle (deg) | Lateral (mm2) | Medial (mm2) | Lateral (mm2) | Medial (mm2) |
| 15 | ||||
| 30 | 236.4 | |||
| 60 | 232.6 | 120.6 | ||
| 90 | 392.5 | 114.4 | 149.5 | |
| 120 | 276.6 | 259.1 | 55.2 | |
| 150 | 95.3 | 81.8 | ||
|
Subject #3 |
Subject #4 |
|||
|---|---|---|---|---|
| Flexion angle (deg) | Lateral (mm2) | Medial (mm2) | Lateral (mm2) | Medial (mm2) |
| 15 | 116.3 | |||
| 30 | 502.6 | 233.0 | ||
| 60 | 709.3 | 134.3 | ||
| 90 | 334.8 | 47.4 | 114.8 | |
| 120 | 579.7 | 187.4 | 85.3 | |
| 150 | 310.9 | 166.4 | 256.5 | 176.8 |
|
Subject #5 |
Subject #6 |
|||
|---|---|---|---|---|
| Flexion angle (deg) | Lateral (mm2) | Medial (mm2) | Lateral (mm2) | Medial (mm2) |
| 15 | 163.2 | 154.8 | ||
| 30 | 377.6 | 281.9 | ||
| 60 | 333.5 | 470.5 | ||
| 90 | 191.2 | 557.0 | ||
| 120 | 359.7 | 178.9 | 277.1 | |
| 150 | 231.0 | 177.9 | 105.0 | 319.0 |
|
Subject #7 |
||
|---|---|---|
| Flexion angle (deg) | Lateral (mm2) | Medial (mm2) |
| 15 | ||
| 30 | 127.7 | |
| 60 | 323.5 | |
| 90 | 461.4 | |
| 120 | 498.0 | |
| 150 | 295.2 | 50.6 |
Table 4.
The location of the contact points of the individual subjects at different flexion angles of the knee
|
Subject #1 | ||||
|---|---|---|---|---|
|
|
|
Separated |
||
| Flexion angle (deg) | M/L L+ (mm) | P/D P+ (mm) | M/L L+ (mm) | P/D P+ (mm) |
| 15 | ||||
| 30 | ||||
| 60 | −3.5 | 3.1 | ||
| 90 | −1.0 | 6.9 | ||
| 120 | −4.6 | 4.6 | ||
| 150 | 15.8 | 0.4 | −13.1 | 9.8 |
|
Subject #2 | ||||
|---|---|---|---|---|
|
|
|
Separated |
||
| Flexion angle (deg) | M/L L+ (mm) | P/D P+ (mm) | M/L L+ (mm) | P/D P+ (mm) |
| 15 | ||||
| 30 | 2.5 | −0.1 | ||
| 60 | −6.3 | 4.2 | ||
| 90 | 13.2 | 4.4 | −8.8 | 2.7 |
| 120 | 10.3 | 4.8 | −15.4 | 1.4 |
| 150 | ||||
|
Subject #3 | ||||
|---|---|---|---|---|
|
|
|
Separated |
||
| Flexion angle (deg) | M/L L+ (mm) | P/D P+ (mm) | M/L L+ (mm) | P/D P+ (mm) |
| 15 | ||||
| 30 | 2.0 | −4.1 | ||
| 60 | 3.0 | 3.8 | ||
| 90 | −0.4 | 2.9 | ||
| 120 | 5.2 | 0.2 | ||
| 150 | 14.8 | −0.5 | −17.2 | −1.2 |
|
Subject #4 | ||||
|---|---|---|---|---|
|
|
|
Separated |
||
| Flexion angle (deg) | M/L L+ (mm) | P/D P+ (mm) | M/L L+ (mm) | P/D P+ (mm) |
| 15 | 6.3 | −8.2 | ||
| 30 | 5.1 | −4.6 | ||
| 60 | 11.6 | −1.0 | ||
| 90 | 15.3 | −0.4 | −9.0 | 1.7 |
| 120 | 13.0 | −1.9 | −13.8 | −1.4 |
| 150 | 12.7 | −1.9 | −16.0 | −1.6 |
|
Subject #5 | ||||
|---|---|---|---|---|
|
Separated |
||||
| Flexion angle (deg) | M/L L+ (mm) | P/D P+ (mm) | M/L L+ (mm) | P/D P+ (mm) |
| 15 | 4.9 | −9.7 | ||
| 30 | 2.2 | −4.6 | ||
| 60 | −6.6 | −3.1 | ||
| 90 | −10.8 | −2.7 | ||
| 120 | −9.0 | 2.2 | ||
| 150 | 8.5 | 2.4 | −13.8 | 2.7 |
|
Subject #6 | ||||
|---|---|---|---|---|
|
|
Separated |
|||
| Flexion angle (deg) | M/L L+ (mm) | P/D P+ (mm) | M/L L+ (mm) | P/D P+ (mm) |
| 15 | 2.4 | −9.1 | ||
| 30 | −2.2 | −4.7 | ||
| 60 | 1.0 | 2.4 | ||
| 90 | −6.4 | 3.0 | ||
| 120 | 9.2 | 0.4 | −13.2 | 0.0 |
| 150 | 7.7 | 4.2 | −14.4 | 2.3 |
|
Subject #7 | ||||
|---|---|---|---|---|
|
|
Separated |
|||
| Flexion angle (deg) | M/L L+ (mm) | P/D P+ (mm) | M/L L+ (mm) | P/D P+ (mm) |
| 15 | ||||
| 30 | 2.0 | −3.8 | ||
| 60 | 8.8 | 3.6 | ||
| 90 | 3.6 | 4.9 | ||
| 120 | 6.6 | 4.8 | ||
| 150 | 10.8 | 6.1 | −19.5 | 0.3 |
Note: M: medial, L: lateral, P: proximal, D: distal.
Contributor Information
Koichi Kobayashi, Bioengineering Lab, Department of Orthopedic Surgery, Harvard Medical School/Massachusetts, General Hospital, Boston, MA 02114; Department of Health Sciences, Niigata University School of Medicine, Niigata, Japan.
Ali Hosseini, Bioengineering Lab, Department of Orthopedic Surgery, Harvard Medical School/Massachusetts, General Hospital, Boston, MA 02114.
Makoto Sakamoto, Department of Health Sciences, Niigata University School of Medicine, Niigata, Japan.
Guoan Li, e-mail: gli1@partners.org, Bioengineering Lab, Department of Orthopedic Surgery, Harvard Medical School/Massachusetts, General Hospital, Boston, MA 02114.
References
- [1]. Mulholland, S. J. , and Wyss, U. P. , 2001, “Activities of Daily Living in Non-Western Cultures: Range of Motion Requirements for Hip and Knee Joint Implants,” Int. J. Rehabil. Res., 24, pp. 191–198. 10.1097/00004356-200109000-00004 [DOI] [PubMed] [Google Scholar]
- [2]. Weiss, J. M. , Noble, P. C. , Conditt, M. A. , Kohl, H. W. , Roberts, S. , Cook, K. F. , Gordon, M. J. , and Mathis, K. B. , 2002, “What Functional Activities Are Important to Patients With Knee Replacements?,” Clin. Orthop. Relat. Res., 404, pp. 172–188. 10.1097/00003086-200211000-00030 [DOI] [PubMed] [Google Scholar]
- [3]. Sumino, T. , Gadikota, H. R. , Varadarajan, K. M. , Kwon, Y. M. , Rubash, H. E. , and Li, G. , 2011, “Do High Flexion Posterior Stabilised Total Knee Arthroplasty Designs Increase Knee Flexion? A Meta Analysis,” Int. Orthop., 35, pp. 1309–1319. 10.1007/s00264-011-1228-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4]. Hefzy, M. S. , Kelly, B. P. , and Cooke, T. D. , 1998, “Kinematics of the Knee Joint in Deep Flexion: A Radiographic Assessment,” Med. Eng. Phys., 20, pp. 302–307. 10.1016/S1350-4533(98)00024-1 [DOI] [PubMed] [Google Scholar]
- [5]. Most, E. , Li, G. , Sultan, P. G. , Park, S. E. , and Rubash, H. E. , 2005, “Kinematic Analysis of Conventional and High-Flexion Cruciate-Retaining Total Knee Arthroplasties: An in Vitro Investigation,” J. Arthroplasty, 20, pp. 529–535. 10.1016/j.arth.2004.09.034 [DOI] [PubMed] [Google Scholar]
- [6]. Nagura, T. , Dyrby, C. O. , Alexander, E. J. , and Andriacchi, T. P. , 2002, “Mechanical Loads at the Knee Joint During Deep Flexion,” J. Orthop. Res., 20, pp. 881–886. 10.1016/S0736-0266(01)00178-4 [DOI] [PubMed] [Google Scholar]
- [7]. Li, G. , Zayontz, S. , Most, E. , DeFrate, L. E. , Suggs, J. F. , and Rubash, H. E. , 2004, “ In Situ Forces of the Anterior and Posterior Cruciate Ligaments in High Knee Flexion: An in Vitro Investigation,” J. Orthop. Res., 22, pp. 293–297. 10.1016/S0736-0266(03)00179-7 [DOI] [PubMed] [Google Scholar]
- [8]. Most, E. , Sultan, P. G. , Park, S. E. , Papannagari, R. , and Li, G. , 2006, “Tibiofemoral Contact Behavior is Improved in High-Flexion Cruciate Retaining TKA,” Clin. Orthop. Relat. Res., 452, pp. 59–64. 10.1097/01.blo.0000238843.11176.42 [DOI] [PubMed] [Google Scholar]
- [9]. Walker, P. S. , Yildirim, G. , Sussman-Fort, J. , and Klein, G. R. , 2006, “Relative Positions of the Contacts on the Cartilage Surfaces of the Knee Joint,” Knee, 13, pp. 382–388. 10.1016/j.knee.2006.04.011 [DOI] [PubMed] [Google Scholar]
- [10]. Kobayashi, K. , Sakamoto, M. , Hosseini, A. , Rubash, H. E. , and Li, G. , 2012, “In-Vivo Patellar Tendon Kinematics During Weight-Bearing Deep Knee Flexion,” J. Orthop. Res., 30, pp. 1596–1603. 10.1002/jor.22126 [DOI] [PubMed] [Google Scholar]
- [11]. Miller, R. K. , Goodfellow, J. W. , Murray, D. W. , and O'Connor, J. J. , 1998, “In Vitro Measurement of Patellofemoral Force After Three Types of Knee Replacement,” J. Bone Joint Surg. Br., 80, pp. 900–906. 10.1302/0301-620X.80B5.8460 [DOI] [PubMed] [Google Scholar]
- [12]. Hehne, H. J. , 1990, “Biomechanics of the Patellofemoral Joint and Its Clinical Relevance,” Clin. Orthop. Relat. Res., 258, pp. 73–85. [PubMed] [Google Scholar]
- [13]. DeFrate, L. E. , Sun, H. , Gill, T. J. , Rubash, H. E. , and Li, G. , 2004, “In Vivo Tibiofemoral Contact Analysis Using 3D MRI-Based Knee Models,” J. Biomech., 37, pp. 1499–1504. 10.1016/j.jbiomech.2004.01.012 [DOI] [PubMed] [Google Scholar]
- [14]. Defrate, L. E. , Nha, K. W. , Papannagari, R. , Moses, J. M. , Gill, T. J. , and Li, G. , 2007, “The Biomechanical Function of the Patellar Tendon During In-Vivo Weight-Bearing Flexion,” J. Biomech., 40, pp. 1716–1722. 10.1016/j.jbiomech.2006.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15]. Li, G. , DeFrate, L. E. , Sun, H. , and Gill, T. J. , 2004, “In Vivo Elongation of the Anterior Cruciate Ligament and Posterior Cruciate Ligament During Knee Flexion,” Am. J. Sports Med., 32, pp. 1415–1420. 10.1177/0363546503262175 [DOI] [PubMed] [Google Scholar]
- [16]. Li, G. , Wuerz, T. H. , and DeFrate, L. E. , 2004, “Feasibility of Using Orthogonal Fluoroscopic Images to Measure in Vivo Joint Kinematics,” ASME, J. Biomech. Eng., 126, pp. 314–318. 10.1115/1.1691448 [DOI] [PubMed] [Google Scholar]
- [17]. Nha, K. W. , Papannagari, R. , Gill, T. J. , Van de Velde, S. K. , Freiberg, A. A. , Rubash, H. E. , and Li, G. , 2008, “In Vivo Patellar Tracking: Clinical Motions and Patellofemoral Indices,” J. Orthop. Res., 26, pp. 1067–1074. 10.1002/jor.20554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18]. Van de Velde, S. K. , Gill, T. J. , DeFrate, L. E. , Papannagari, R. , and Li, G. , 2008, “The Effect of Anterior Cruciate Ligament Deficiency and Reconstruction on the Patellofemoral Joint,” Am. J. Sports Med., 36, pp. 1150–1159. 10.1177/0363546508314404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19]. Bingham, J. T. , Papannagari, R. , Van de Velde, S. K. , Gross, C. , Gill, T. J. , Felson, D. T. , Rubash, H. E. , and Li, G. , 2008, “In Vivo Cartilage Contact Deformation in the Healthy Human Tibiofemoral Joint,” Rheumatology, 47, pp. 1622–1627. 10.1093/rheumatology/ken345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20]. Amis, A. A. , Senavongse, W. , and Darcy, P. , 2005, “Biomechanics of Patellofemoral Joint Prostheses,” Clin. Orthop. Relat. Res., 436, pp. 20–29. 10.1097/01.blo.0000171546.45718.03 [DOI] [PubMed] [Google Scholar]
- [21]. Li, G. , DeFrate, L. E. , Zayontz, S. , Park, S. E. , and Gill, T. J. , 2004, “The Effect of Tibiofemoral Joint Kinematics on Patellofemoral Contact Pressures Under Simulated Muscle Loads,” J. Orthop. Res., 22, pp. 801–806. 10.1016/j.orthres.2003.11.011 [DOI] [PubMed] [Google Scholar]
- [22]. Li, G. , Zayontz, S. , DeFrate, L. E. , Most, E. , Suggs, J. F. , and Rubash, H. E. , 2004, “Kinematics of the Knee at High Flexion Angles: An in Vitro Investigation,” J. Orthop. Res., 22, pp. 90–95. 10.1016/S0736-0266(03)00118-9 [DOI] [PubMed] [Google Scholar]
- [23]. Fujikawa, K. , Seedhom, B. B. , and Wright, V . , 1983, “Biomechanics of the Patello-Femoral Joint—Part I: A Study of the Contact and the Congruity of the Patello-Femoral Compartment and Movement of the Patella,” Eng. Med., 12, pp. 3–11. 10.1243/EMED_JOUR_1983_012_004_02 [DOI] [PubMed] [Google Scholar]
- [24]. Goodfellow, J. , Hungerford, D. S. , and Zindel, M. , 1976, “Patello-Femoral Joint Mechanics and Pathology. 1. Functional Anatomy of the Patello-Femoral Joint,” J. Bone Joint Surg. Br., 58, pp. 287–290. [DOI] [PubMed] [Google Scholar]
- [25]. Heegaard, J. , Leyvraz, P. F. , Van Kampen, A. , Rakotomanana, L. , Rubin, P. J. , and Blankevoort, L. , 1994, “Influence of Soft Structures on Patellar Three-Dimensional Tracking,” Clin. Orthop. Relat. Res., 299, pp. 235–243. [PubMed] [Google Scholar]
- [26]. Nakagawa, S. , Kadoya, Y. , Kobayashi, A. , Tatsumi, I . , Nishida, N. , and Yamano, Y. , 2003, “Kinematics of the Patella in Deep Flexion. Analysis With Magnetic Resonance Imaging,” J. Bone Joint Surg. Am., 85-A, pp. 1238–1242. [DOI] [PubMed] [Google Scholar]
- [27]. Singerman, R. , Davy, D. T. , and Goldberg, V . M. , 1994, “Effects of Patella Alta and Patella Infera on Patellofemoral Contact Forces,” J. Biomech., 27, pp. 1059–1065. 10.1016/0021-9290(94)90222-4 [DOI] [PubMed] [Google Scholar]
- [28]. Yildirim, G. , Walker, P. S. , Sussman-Fort, J. , Aggarwal, G. , White, B. , and Klein, G. R. , 2007, “The Contact Locations in the Knee During High Flexion,” Knee, 14, pp. 379–384. 10.1016/j.knee.2007.06.007 [DOI] [PubMed] [Google Scholar]
- [29]. Matsuda, S. , Ishinishi, T. , White, S. E. , and Whiteside, L. A. , 1997, “Patellofemoral Joint After Total Knee Arthroplasty. Effect on Contact Area and Contact Stress,” J. Arthroplasty, 12, pp. 790–797. 10.1016/S0883-5403(97)90010-3 [DOI] [PubMed] [Google Scholar]
- [30]. Huberti, H. H. , and Hayes, W. C. , 1984, “Patellofemoral Contact Pressures. The Influence of Q-Angle and Tendofemoral Contact,” J. Bone Joint Surg. Am., 66, pp. 715–724. [PubMed] [Google Scholar]
- [31]. Hsu, H. C. , Luo, Z. P. , Rand, J. A. , and An, K. N. , 1996, “Influence of Patellar Thickness on Patellar Tracking and Patellofemoral Contact Characteristics After Total Knee Arthroplasty,” J. Arthroplasty, 11, pp. 69–80. 10.1016/S0883-5403(96)80163-X [DOI] [PubMed] [Google Scholar]
- [32]. Johanson, N. A. , Cerynik, D. L. , and Pasquale, M. , 2011, “Measuring Patellofemoral Forces and Pressures in a Simulated Operating Room Environment,” J. Arthroplasty, 26, pp. 137–143. 10.1016/j.arth.2009.09.004 [DOI] [PubMed] [Google Scholar]
- [33]. Omori, G. , Koga, Y. , Bechtold, J. E. , Gustilo, R. B. , Nakabe, N. , Sasagawa, K. , Hara, T. , and Takahashi, H. E. , 1997, “Contact Pressure and Three-Dimensional Tracking of Unresurfaced Patella in Total Knee Arthroplasty,” Knee, 4, pp. 15–24. 10.1016/S0968-0160(96)00230-X [DOI] [Google Scholar]
- [34]. Matsuda, S. , Whiteside, L. A. , and Ishinishi, T. , 1998, “Effect of Patellar Meniscus on Patellofemoral Contact Stress in Total Knee Arthroplasty,” J. Arthroplasty, 13, pp. 722–727. 10.1016/S0883-5403(98)80020-X [DOI] [PubMed] [Google Scholar]
- [35]. Xu, C. , Chu, X. , and Wu, H. , 2007, “Effects of Patellar Resurfacing on Contact Area and Contact Stress in Total Knee Arthroplasty,” Knee, 14, pp. 183–187. 10.1016/j.knee.2007.01.005 [DOI] [PubMed] [Google Scholar]
- [36]. Li, G. , Most, E. , Sultan, P. G. , Schule, S. , Zayontz, S. , Park, S. E. , and Rubash, H. E. , 2004, “Knee Kinematics With a High-Flexion Posterior Stabilized Total Knee Prosthesis: An in Vitro Robotic Experimental Investigation,” J. Bone Joint Surg., 86-A, pp. 1721–1729. [DOI] [PubMed] [Google Scholar]
- [37]. Zelle, J., Barink, M., De Waal Malefijt, M. , and Verdonschot, N., 2009, “Thigh–Calf Contact: Does It Affect the Loading of the Knee in the High-Flexion Range?,” J. Biomech., 42, pp. 587–593. 10.1016/j.jbiomech.2008.12.015 [DOI] [PubMed] [Google Scholar]