Abstract
The cleft nasal deformity is a complex challenge in plastic surgery involving the skin, cartilage, mucosa, and skeletal platform. Ever since Blair and Brown first described the intricacies of the cleft pathology in 1931, the appropriate approach has been extensively debated in the literature with respect to timing, technique, and extent of surgical intervention. In this article, the authors review the literature and summarize the various modalities for achieving a successful rhinoplasty in the patient with a cleft nasal deformity.
Keywords: cleft nasal deformity, cleft nose, unilateral cleft nose, bilateral cleft nose, rhinoplasty
The cleft nasal deformity involves the skin, cartilage, mucosa, and skeletal platform. Theories regarding the origination of the cleft nasal deformity have been discussed extensively and continue to be debated today. The anatomic abnormalities have been measured and documented. An appreciation of the pathologic anatomy in unilateral and bilateral cleft noses is essential in achieving satisfactory aesthetic and functional results.
Background
Blair and Brown first described the cleft nose in 1931, critically identifying the nuances of the pathology.1 The relationship between clinical presentation and embryologic development is an essential step in appreciating the factors involved in surgical correction of the cleft lip and nose. Deformational abnormalities are attributable to a combination of intrinsic and extrinsic factors, such as mesenchymal migration and mechanical stresses.2 A cleft lip forms from improper fusion of the medial and lateral nasal prominences with the maxillary prominence during embryologic development. Studies have shown that the medial nasal process remains centralized and fails to fuse with the maxillary process in cleft patients.3 As embryogenesis continues, the unopposed forces, created by the development of the discontinuous orbicularis musculature, further define the aberrant clinical features of the cleft nose.2,4
Unilateral Cleft Nasal Deformity
The unilateral cleft nasal deformity involves the structural framework of the nose as well as the soft tissue envelope. The aberrant orbicularis muscle insertion results in an imbalance that is further compounded by the maxillary skeletal hypoplasia.2 Rather than a horizontal insertion and continuous decussation with the contralateral orbicularis oris seen in the normal lip, the orbicularis oris inserts in a discontinuous manner into the columella on the noncleft side. This creates an unopposed force that pulls the columella and caudal nasal septum to the noncleft side.4 On the cleft side, the orbicularis inserts into the nasal base, retracting it laterally and inferiorly. Additionally, due to poor maxillary skeletal support at the alar base, the ala is further displaced posteriorly (Fig. 1).4
Fig. 1.

Unilateral cleft nose deformity. Figures 1 and 5 depict the same patient throughout the entirety of his treatment course.
The asymmetric nasal tip results from the irregularly formed lower lateral cartilage on the cleft side. Although not ubiquitously accepted, the length of the lower lateral cartilage on the cleft side is considered equal to the noncleft side, primarily differing in shape and position.5,6,7,8 On the cleft side, the medial crus is shorter and the lateral crus longer, with a less defined and wider dome.9 This results in a poorly defined nasal tip with less projection.
Deviation of the nasal septum is seen both in the cleft and noncleft nostril. Due to the unopposed pull of the orbicularis oris muscle and the premaxillary ligament, the caudal nasal septum is deviated to the noncleft-side nostril. This force affects only the caudal septum, allowing for septal bowing in the cleft side nasal airway. Whether alone or in conjunction with hypertrophied nasal turbinates, the aperture of the nasal airway is decreased, resulting in nasal airway obstruction.10
Furthermore, nasal obstruction at the external nasal valve from the introverted lower lateral cartilage is common in cleft patients. The cephalic edge of the lower lateral cartilage introverts into the vestibule in a posterior inferior direction resulting in a visibly thickened and hooded ala.11 Attachment of the lateral nasal sidewall to the depressed cleft-side piriform results in a vestibular webbing that is visible through the cleft side nares.
Bilateral Cleft Nasal Deformity
Although there are anatomic components of the bilateral cleft nose that resemble the unilateral deformity, there tends to be a greater level of symmetry in the bilateral deformity (Fig. 2). The columella is short or nearly absent due to decreased soft tissue and skin between the nasal tip and upper lip.12 The degree of columellar shortening is related to the extent of prolabial development, cephalic nasal tip rotation, and cleft severity. The lower lateral cartilages have an increased interdomal distance due to the aberrant muscular insertions, resulting in decreased projection and tip definition.11 The septum normally remains midline unless it is asymmetric. The less-severe side applies more force to the caudal septum, resulting in deviation to this side. A wide septum is not uncommon and may present as nasal obstruction.
Fig. 2.
Bilateral cleft nose deformity demonstrating relative symmetry of nose with wide ala and broad nasal dome.
Surgical Timing
Timing of cleft lip nasal surgery can be divided into primary, intermediate, and secondary repairs. Multiple studies have disproved the idea that early manipulation of the nasal cartilage interferes with growth.5 Originally based on experimental studies that showed large submucous resections of the nasal septum affected subsequent nasal and midface growth, studies by McComb and Coghlan overturned this philosophy by demonstrating that repositioning of the lower lateral cartilage without cartilage resection did not interfere with subsequent nasal and midfacial development.13,14
Because of these findings, primary cleft rhinoplasty occurs with the initial lip repair.15 The benefit of early intervention allows for an earlier restoration of nasal shape with the potential for more symmetric nasal growth. It is important to note that any surgery done at an early age will subsequently result in scar tissue and consequently affect future surgeries.
Primary Rhinoplasty
Primary rhinoplasty is defined as nasal surgery at the time of primary cleft lip repair. Although both the nose and lip are addressed simultaneously, the nasal correction should not be considered an adjunct to the lip, but should instead be a part of the overall cleft pathology. These two anatomic structures are connected and should be considered together when it comes to repair and reconstruction. The goal of primary rhinoplasty for both the unilateral and bilateral deformity is to provide better contour, symmetry, and projection of the nasal tip by releasing, undermining, and repositioning the lower lateral cartilages.16,17,18,19 In addition, in unilateral deformities, the caudal nasal septum can be placed back on the anterior nasal spine to allow for more symmetric growth.
There have been various techniques described to correct the unilateral cleft nose.15,18 Most techniques involve a dissection of the skin overlying the lower lateral cartilages through both medial and lateral tunnels within the cleft lip incisions (Fig. 3).20 This allows for a differential movement of nasal alae and lower lateral cartilage when it comes to positioning the nasal base and relocating the lower lateral cartilages. The vestibular skin is rarely dissected during the primary nasal surgery. The retropositioned nasal base can be brought more anterior by dissecting the lateral nasal sidewall from the piriform. By making a back-cut in the lateral nasal sidewall, the depressed nasal base on the cleft side can be positioned in a more symmetric position with the contralateral side. The muscular ring of the nasalis is reconstructed by securing it to the anterior nasal spine.9 It is important during this portion of the reconstruction to not overcorrect the position of the nasal ala and nostril base. If the length of the nostril sill is not preserved and the alar base is cinched too tight, the patient will heal with a micronostril, a problem extremely difficult to correct secondarily. Once the nasal base position has been set and the cleft lip repaired, the lower lateral cartilage can be resuspended to the contralateral side upper lateral cartilage with transnasal sutures.21 The goal of these sutures is to recreate the cleft-side nasal dome with better symmetry and projection. These sutures are brought into the nose, through the vestibular lining, through the lower lateral cartilages, and through the nasal skin. They are then repassed through the nasal skin, the upper lateral cartilage, and suture down within the nasal vestibule. They are reintroduced into the nose through the same needle hole they exited, to prevent any skin necrosis (Fig. 4).
Fig. 3.
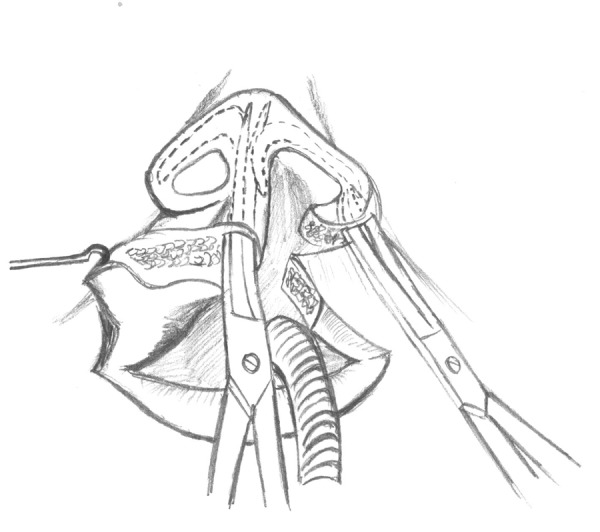
Dissection for access to crura.
Fig. 4.
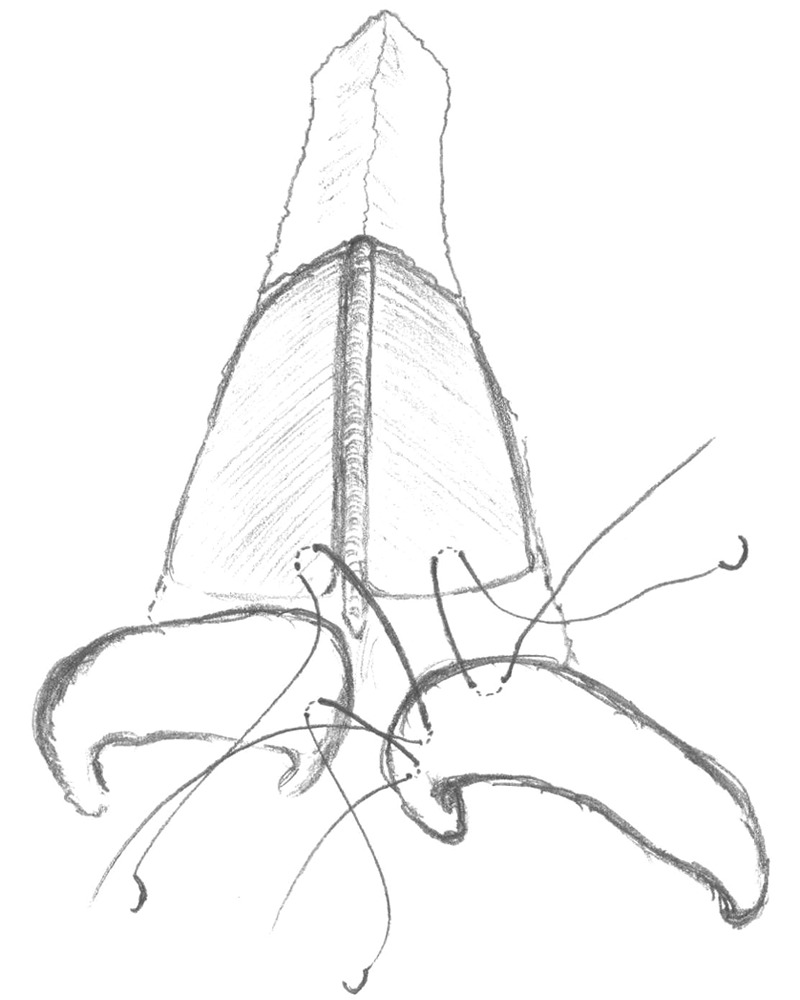
Transnasal sutures recreate the cleft-side nasal dome for better symmetry and projection. The sutures pass through the nose, vestibular lining, the lower lateral cartilages, and through the nasal skin before being repassed through the nasal skin, upper lateral cartilage, and sutured down within the nasal vestibule.
Correction of the bilateral cleft nasal deformity is usually limited to repositioning the alar bases and reconstructing the nasal muscular ring, as done in the unilateral technique. The nasalis muscle is secured to the nasal septum bilaterally to help correctly position the retrodisplaced alar base. This is done in conjunction with release of the lateral nasal lining, as done in the unilateral repair. Nasal tip surgery is reserved for the intermediate stage for bilateral patients.
Intermediate Rhinoplasty
Intermediate rhinoplasty is usually performed before the cleft patient enters school, between 4 and 6 years of age.20 This allows the surgeon the ability to perform any minor lip revisions if necessary, as well as achieve better nasal tip symmetry. Additionally, if there is any lateral vestibular webbing, this can be corrected to prevent external nasal valve obstruction. The major goal of surgery is to correct the aberrant position of the cleft-side lower lateral cartilage so that future nasal growth will not exacerbate the cleft nasal deformity. This will achieve a more symmetric appearing nose after surgery, but also make the correction of any nasal asymmetries easier after facial growth is complete. Septal surgery should be deferred until postadolescence so as not to prevent further nasal growth.11
In unilateral deformities, the intermediate rhinoplasty addresses the position of the cleft side of the lower lateral cartilage as well as the lateral vestibular webbing. An open rhinoplasty approach can be performed to expose the lower lateral cartilages bilateral and directly observe the geometric differences. Once they are appreciated, correction with suture techniques can be performed. Cartilage grafting is not performed at this young age, given the residual growth potential of the nose. Once the shape of the tip is corrected, the nose is closed along its columellar incision.22 If there is lateral vestibular webbing present through the incision, a V-Y type incision or back-cut can used to lengthen the lateral nasal sidewall, and advance the lower lateral cartilage forward.20
In bilateral cases, the intermediate rhinoplasty addresses the depressed lower lateral cartilages and lengthens the shortened columella.19,20 This is done via an open rhinoplasty technique as well. The lower lateral cartilages are exposed through transcolumellar and infracartilaginous incisions. The lower lateral cartilages are sutured together via a transdomal suture to decrease their angle of divergence and put them in a more projected orientation.19 Soft tissue that is commonly found between the lower lateral cartilages can be thinned to help achieve a better lower lateral cartilage position. The incisions are then closed with plain gut in the vestibule and permanent suture on the columella.
Secondary Rhinoplasty
Secondary rhinoplasty occurs after facial growth is completed. This is around 14 to 16 years old in female patients and 16 to 18 years old in male patients.23,24 Surgical techniques rely on well-accepted rhinoplasty principles and are applied for unilateral or bilateral cleft nasal deformities.25,26,27 The open approach is preferred for better exposure and visualization of the nasal elements. Placement of cartilage grafts for support and reinforcement is a major component of the cleft rhinoplasty operation. Use of the cartilage grafts reinforces the structural support of the nose, allowing for improved tip definition, and preventing wound contracture and collapse.
Evaluation
All patients should be thoroughly addressed and evaluated with a history and physical exam before proceeding with the rhinoplasty operation. Previous surgeries should be specifically discussed to prepare for possible findings intraoperatively. Patient concerns as relates to their nasal airway, nose, and lip symmetry should be addressed. Preoperative photographs should be taken to document the deformities. These photographs are also helpful when consulting the patient regarding operative goals.
Physical exam of the nose should be done in relation to its position on the facial skeleton. Preoperative photographs are helpful when examining these relationships. Furthermore, cephalometric analysis should be considered to evaluate the jaw position and the affect it has on the patient's nose. Maxillary position should be evaluated to see if orthognathic surgery is necessary to help with overall facial harmony. Chin position is another important landmark that must be evaluated. These issues should be discussed with the patient and family. If they are not interested in orthognathic surgery, and are happy with the overall facial appearance, an exam centered on nasal shape and symmetry can be performed.
Nasal examination is always performed in a very systematic and repeatable fashion. Gunter diagrams are very helpful for preoperative planning purposes. The cleft nasal deformities in the adult are related to what is found during the primary repair, but will be altered by any previous surgery that has been performed. It is important to understand these changes, as it may affect the planned operation. Frequently the nasal root is wide and deviated away from the cleft (Fig. 5A). The midvault tends to be straight and follow the nasal root. There can be significant nasal tip asymmetry, with distorted cleft-side lower lateral cartilages. This cartilage is hypoplastic and has either lost or never had most of its structural integrity. The nasal dome on the cleft side is depressed and nasal ala is in an extended and flattened orientation when compared with the opposite side. The nasal septum is deviated into the cleft nostril, whereas the caudal septum is deviated into the opposite nostril. The nostril sill can be short due to overcorrection, and the cleft side nares can have a smaller circumference than its counterpart. Nasal tip support will be weak because of the hypoplastic cleft-side lower lateral cartilage. Lateral vestibular webbing in the cleft-side nostril is frequently present if the nasal sidewall dissection is not performed at the time of the original cleft repair.
Fig. 5.

(A) Preoperative evaluation prior to the secondary rhinoplasty demonstrates a wide nasal root deviated away from the cleft with distorted cleft-side lower lateral cartilages. (B) Secondary rhinoplasty postoperative photos demonstrating corrected nasal tip projection and ala repositioning.
Alar base support is essential for attaining definitive repair and relies on the skeletal foundation of the face. Varying degrees of unilateral or bilateral maxillary hypoplasia are typically present in the cleft patient. Bridging the cleft with alveolar bone graft should be performed prior to eruption of the canine teeth, between the ages of 9 to 11 years.4,28,29 This serves to support, augment, and reposition the alar base. When inadequate support is encountered, secondary augmentation using bone, cartilage, and alloplastic implants may be applied. In severe maxillary hypoplasia where more-significant augmentation is necessary, LeFort I maxillary osteotomy and advancement reconstruct the anteroposterior dimensions of the face. Advancement should be completed prior to definitive rhinoplasty.22
Incision
Performing the cleft rhinoplasty operation via an open approach allows for direct visualization of nasal structures as well as anatomic reconstruction of abnormal components. Transcolumellar and infracartilaginous incisions are most frequently employed to visualize the lower lateral cartilages as well as the nasal septum. Care should be taken when elevating the columella not to injure the medial crura of the lower lateral cartilages. These cartilages lie directly under the skin adjacent to the lateral portions of the columella. Superficial dissection should proceed in these areas to prevent injuring these structures. Once the nasal skin has been elevated, the nasal structures can be examined for deformities.
The Septum
The nasal septum can be approached by splitting the lower lateral cartilages between the medial crura. The caudal septum is found between these two cartilages and a subperichondrial dissection can be started from this point. It is important to ensure that the dissection is in the proper plain, which can be validated by the blue appearance of the cartilage once it has been encountered. A portion of the septum is harvested to obtain cartilage for grafting as well as to correct septal deviation causing nasal airway obstruction. A 1-cm dorsal and caudal strut should remain to avoid nasal collapse. Any displacement of the caudal septum should be corrected at this time by release from the maxillary crest and resecured to the anterior nasal spine. In complete clefts, there is often a bony septal spur that needs removal to help achieve a patent nasal airway. This can be addressed during the septal cartilage harvest and repositioning.
The Nasal Tip
The nasal tip is buttressed using a columellar strut graft, placed in between the medial crura and sutured in place. The lower lateral cartilage is then advanced and secured to the graft using mattress sutures to obtain appropriate tip projection.30 It is important to place the columellar strut behind the medial crura, so as not to increase the columella width.31 When the lower lateral cartilages are wide, the nose may appear asymmetric and may benefit from cephalic trimming. Typically, projection remains inadequate on the cleft side. Batten grafting with onlay septal cartilage grafts on the cleft-side lower lateral cartilage can provide for better support and shape.30 The cartilages are then sutured together to reconstitute the dome into a more cephalic position. Onlay shield grafts can help give better definition to the ill-defined nasal tip.31
Bilateral cleft deformities require repositioning of both lower lateral cartilages with tip suture techniques. If the cartilages are not strong enough to allow for appropriate projection, septal grafts as columellar struts as well as in the onlay position can be beneficial.31 Cephalic trimming of large lower lateral cartilages is helpful in reducing the large nasal tip commonly seen in bilateral cleft patients. The goal for the bilateral deformity is to decrease the angle of divergence between the domal points of the lower lateral cartilages, create a more defined nasal tip, and provide a strong nasal framework for better tip projection.
Nasal Vestibule
Nasal vestibule contracture, resulting from either the primary repair or revisions, is a difficult and common problem encountered during secondary rhinoplasty. Scaring can lead to nostril stenosis and collapse of the external nasal valve. Local tissue rearrangement with healthy tissue can help reconstruct this and disrupt the constrictive forces in the external nasal valve.16 Redundant skin may be used to line a stenotic nasal vestibule.32 A laterally or medially based sliding chondrocutaneous flap, harvested using the previous cleft lip scar, can be critical for lining vestibular deficits due to its healthy blood supply.32
If there is significant constriction of the nostril and loss of tissue along the nostril sill, the nasal alae should be repositioned. Micronostril is a very difficult problem to correct, and the creation of this deformity during primary repair should be recognized and avoided at all costs. One of the more reliable ways to correct this problem is by introducing new skin into the nasal sill with a perialar nasolabial flap. This can increase the relative size of the nostril, reposition the medially displaced alar base, and increase the length of the nostril sill to more accurately match the opposite side.
Lateral vestibular webbing is a common problem seen in secondary rhinoplasty. This can prevent the lower lateral cartilage from advancing into a more anatomic position. Advancing this tissue with a V-Y–type tissue rearrangement will provide some freedom for this cartilage to move into a more anatomic position. This issue can be corrected during the primary lip repair by releasing the lateral nasal sidewall from the piriform and advancing the alar base to its correct position.
Nasal Dorsum
The root of the nasal dorsum is usually directed toward the side of the cleft, resulting in the tip of the nose deviating away from the cleft. Dorsal humps are usually not a significant issue for cleft patients, but if they are present, they should be addressed after the nasal skin has been elevated in the standard fashion. The nasal bones are commonly thick and wide, therefore low to high osteotomies can be performed to reposition the nasal shoot in a more midline orientation and narrow the nasal base width.31 If this does not adequately narrow the dorsum, a central segment can be removed to create an open roof via paramedian osteotomies, the nasal bones can be in-fractured to achieve adequate narrowing. If this is done, spreader grafts may be necessary to reconstruct the internal nasal valve. Nasal bone osteotomies are either performed percutaneous with a 2-mm osteotome or transnasally.
In bilateral cleft noses, the nasal dorsum is usually wide and straight. Treatment consists of narrowing the dorsum with ostomies via a transcutaneous, transnasal, or gingival buccal sulcus approach.
Nasal Alae
Addressing the malpositioned nasal alae is often one of the final stages of secondary rhinoplasty. Although often lateral and inferiorly malpositioned, the ala can potentially be in any orientation. Using a full-thickness perialar incision, the ala is brought into a position that mirrors the contralateral side (Fig. 5B). The lateral ala is medialized using a V-to-Y advancement along the alar facial groove. Conversely, lateralization of the ala requires transposition of a lateral skin flap into the nasal floor to accommodate the tissue loss. Superiorly positioned alae are dropped by excision of superior lip skin. Skin from the cheek is advanced superiorly to push the inferiorly positioned ala into a more symmetric position. The depressed alae can be augmented with piriform rim augmentation. This is commonly done with alloplastic implants. Fat grafting has also been used in this area to correct the deficiency.
Conclusion
The cleft nasal deformity is a common problem that has both consistent and reliable findings, as well as distinctive nuances. The deformed soft tissue and skeletal foundation are further complicated by the long-term effects of anatomic growth and surgical scarring. The goals of primary rhinoplasty are to restore symmetry and reposition the nasal structures such that further growth will not exacerbate deformities. Intermediate rhinoplasty, although not always indicated, can be utilized before school age to help achieve greater symmetry and help alleviate future growth deformities. Secondary rhinoplasty is best approached after nasal growth has concluded and done via an open technique to fully visualize the nasal structure. Cleft nasal deformity is a complicated problem that should be addressed during multiple stages of the patient's life.
References
- 1.Blair V, Brown J B. Nasal abnormalities, fancied and real surgery. Gynecol Obstet. 1931;53:797–819. [Google Scholar]
- 2.Rifley W, Thaller S R. The residual cleft lip nasal deformity. An anatomic approach. Clin Plast Surg. 1996;23(1):81–92. [PubMed] [Google Scholar]
- 3.Johnston M C, Millicovsky G. Normal and abnormal development of the lip and palate. Clin Plast Surg. 1985;12(4):521–532. [PubMed] [Google Scholar]
- 4.Fisher D M, Sommerlad B C. Cleft lip, cleft palate, and velopharyngeal insufficiency. Plast Reconstr Surg. 2011;128(4):342e–360e. doi: 10.1097/PRS.0b013e3182268e1b. [DOI] [PubMed] [Google Scholar]
- 5.McComb H. Primary correction of unilateral cleft lip nasal deformity: a 10-year review. Plast Reconstr Surg. 1985;75(6):791–799. doi: 10.1097/00006534-198506000-00003. [DOI] [PubMed] [Google Scholar]
- 6.McComb H. Primary repair of unilateral cleft lip nasal deformity. Oper Tech Plast Reconstr Surg. 1995;2:200–205. [Google Scholar]
- 7.Wolfe S A. A pastiche for the cleft lip nose. Plast Reconstr Surg. 2004;114(1):1–9. doi: 10.1097/01.prs.0000130416.86351.24. [DOI] [PubMed] [Google Scholar]
- 8.Li A Q, Sun Y G, Wang G H, Zhong Z K, Cutting C. Anatomy of the nasal cartilages of the unilateral complete cleft lip nose. Plast Reconstr Surg. 2002;109(6):1835–1838. doi: 10.1097/00006534-200205000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Byrd H S, El-Musa K A, Yazdani A. Definitive repair of the unilateral cleft lip nasal deformity. Plast Reconstr Surg. 2007;120(5):1348–1356. doi: 10.1097/01.prs.0000279497.95331.1e. [DOI] [PubMed] [Google Scholar]
- 10.Latham R A. The pathogenesis of the skeletal deformity associated with unilateral cleft lip and palate. Cleft Palate J. 1969;6:404–414. [PubMed] [Google Scholar]
- 11.Fisher D M, Mann R J. A model for the cleft lip nasal deformity. Plast Reconstr Surg. 1998;101(6):1448–1456. doi: 10.1097/00006534-199805000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Penfold C, Dominguez-Gonzalez S. Bilateral cleft lip and nose repair. Br J Oral Maxillofac Surg. 2011;49(3):165–171. doi: 10.1016/j.bjoms.2010.01.017. [DOI] [PubMed] [Google Scholar]
- 13.McComb H K Coghlan B A Primary repair of the unilateral cleft lip nose: completion of a longitudinal study Cleft Palate Craniofac J 199633123–30., discussion 30–31 [DOI] [PubMed] [Google Scholar]
- 14.Bernstein L. Early submucous resection of nasal septal cartilage. A pilot study in canine pups. Arch Otolaryngol. 1973;97(3):273–278. doi: 10.1001/archotol.1973.00780010281012. [DOI] [PubMed] [Google Scholar]
- 15.Morovic C G Cutting C Combining the Cutting and Mulliken methods for primary repair of the bilateral cleft lip nose Plast Reconstr Surg 200511661613–1619., discussion 1620–1622 [DOI] [PubMed] [Google Scholar]
- 16.Sykes J M Jang Y J Cleft lip rhinoplasty Facial Plast Surg Clin North Am 2009171133–144., vii [DOI] [PubMed] [Google Scholar]
- 17.Salyer K E, Genecov E R, Genecov D G. Unilateral cleft lip-nose repair—long-term outcome. Clin Plast Surg. 2004;31(2):191–208. doi: 10.1016/S0094-1298(03)00128-7. [DOI] [PubMed] [Google Scholar]
- 18.Haddock N T, McRae M H, Cutting C B. Long-term effect of primary cleft rhinoplasty on secondary cleft rhinoplasty in patients with unilateral cleft lip-cleft palate. Plast Reconstr Surg. 2012;129(3):740–748. doi: 10.1097/PRS.0b013e3182402e8e. [DOI] [PubMed] [Google Scholar]
- 19.Mulliken J B Primary repair of bilateral cleft lip and nasal deformity Plast Reconstr Surg 20011081181–194., 195–196 [DOI] [PubMed] [Google Scholar]
- 20.Shih C W, Sykes J M. Correction of the cleft-lip nasal deformity. Facial Plast Surg. 2002;18(4):253–262. doi: 10.1055/s-2002-36493. [DOI] [PubMed] [Google Scholar]
- 21.Tajima S. Follow-up results of the unilateral primary cleft lip operation with special reference to primary nasal correction by the author's method. Facial Plast Surg. 1990;7(2):97–104. doi: 10.1055/s-2008-1064669. [DOI] [PubMed] [Google Scholar]
- 22.Byrd H S, Salomon J. Primary correction of the unilateral cleft nasal deformity. Plast Reconstr Surg. 2000;106(6):1276–1286. doi: 10.1097/00006534-200011000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Kohout M P, Aljaro L M, Farkas L G, Mulliken J B. Photogrammetric comparison of two methods for synchronous repair of bilateral cleft lip and nasal deformity. Plast Reconstr Surg. 1998;102(5):1339–1349. doi: 10.1097/00006534-199810000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Mulliken J B, Burvin R, Farkas L G. Repair of bilateral complete cleft lip: intraoperative nasolabial anthropometry. Plast Reconstr Surg. 2001;107(2):307–314. doi: 10.1097/00006534-200102000-00001. [DOI] [PubMed] [Google Scholar]
- 25.Stal S, Brown R H, Higuera S. et al. Fifty years of the Millard rotation-advancement: looking back and moving forward. Plast Reconstr Surg. 2009;123(4):1364–1377. doi: 10.1097/PRS.0b013e31819e26a5. [DOI] [PubMed] [Google Scholar]
- 26.Mulliken J B. Principles and techniques of bilateral complete cleft lip repair. Plast Reconstr Surg. 1985;75(4):477–487. doi: 10.1097/00006534-198504000-00003. [DOI] [PubMed] [Google Scholar]
- 27.Cutting C B. Secondary cleft lip nasal reconstruction: state of the art. Cleft Palate Craniofac J. 2000;37(6):538–541. doi: 10.1597/1545-1569_2000_037_0538_sclnrs_2.0.co_2. [DOI] [PubMed] [Google Scholar]
- 28.Kane A A, Pilgram T K, Moshiri M, Marsh J L. Long-term outcome of cleft lip nasal reconstruction in childhood. Plast Reconstr Surg. 2000;105(5):1600–1608. doi: 10.1097/00006534-200004050-00002. [DOI] [PubMed] [Google Scholar]
- 29.Boyne P J, Sands N R. Secondary bone grafting of residual alveolar and palatal clefts. J Oral Surg. 1972;30(2):87–92. [PubMed] [Google Scholar]
- 30.Guyuron B, Ghavami A, Wishnek S M. Components of the short nostril. Plast Reconstr Surg. 2005;116(5):1517–1524. doi: 10.1097/01.prs.0000182590.01431.3d. [DOI] [PubMed] [Google Scholar]
- 31.Guyuron B. MOC-PS(SM) CME article: late cleft lip nasal deformity. Plast Reconstr Surg. 2008;121(4, Suppl):1–11. doi: 10.1097/01.prs.0000305955.67554.40. [DOI] [PubMed] [Google Scholar]
- 32.Madorsky S J, Wang T D. Unilateral cleft rhinoplasty: a review. Otolaryngol Clin North Am. 1999;32(4):669–682. doi: 10.1016/s0030-6665(05)70163-8. [DOI] [PubMed] [Google Scholar]



