Abstract
The bilateral cleft lip and nasal deformity presents a complex challenge for repair. Surgical techniques continue to evolve and are focused on primary anatomic realignment of the tissues. This can be accomplished in a single-stage or two-stage repair early in infancy to provide a foundation for future growth of the lip and nasal tissue. Most cleft surgeons currently perform a single-stage repair for simplifying patient care. Certain institutions utilize presurgical orthopedics for alignment of the maxillary segments and nasal shaping. Methods for the bilateral cleft lip repair are combined with various open and closed rhinoplasty techniques to achieve improved correction of the primary nasal deformity. There is recent focus on shaping the nose for columellar and tip support, as well as alar contour and alar base position. The authors will present a new technique for closure of the nasal floor to prevent the alveolar cleft fistula. Although the alveolar fistula is closed, alveolar bone grafting is still required at the usual time in dental development to fuse the maxilla. It is paramount to try and minimize the stigmata of secondary deformities that historically have been characteristic of the repaired bilateral cleft lip. A properly planned and executed repair reduces the number of revisions and can spare a child from living with secondary deformities.
Keywords: bilateral cleft lip, bilateral cleft lip and palate, cleft nasal deformity, primary bilateral cleft lip repair, primary cleft rhinoplasty
The bilateral cleft lip and nasal deformity presents a complex and often frustrating challenge for surgical repair. The bilateral cleft lip and nasal deformity has a wide degree of variability in regards to the severity of the cleft (incomplete vs complete). There is also the complex three-dimensional dynamics and position of the prolabium and lateral maxillary segments that challenge the surgeon. The deformity is characterized by a protruding maxilla, a prolabium lacking muscle fibers with a blunted white roll, vertically long lateral lip elements widely spaced due to discontinuity of the orbicularis oris, short columella, flattened nose, and abnormally positioned alar cartilages. The goals of surgical repair include (1) proper orbicularis oris muscle repair, (2) a symmetric Cupid's bow with full tubercle, (3) balanced upper lip without horizontal tightness, (4) nasal alar symmetry and tip support, and (5) minimal secondary deformities.
Multiple secondary deformities may arise leading to poor results. These include wide philtrums, tight upper lip, wide scars, flattened nose, wide nasal base, and whistle deformities, just to highlight a few. Multiple techniques have evolved that allow us to focus on one primary lip and nasal repair that will set the stage for future balanced growth as well as hopefully minimize the need for lip revisions.
Cleft surgeons may opt to deal with the secondary deformities in planned revisions. However, multiple revisions will result in increased scarring and contracture. The excess scar tissue and abnormal blood supply not only makes further revision more difficult, but can add to the increased connective tissue deposition in the already abnormal cleft muscle fibers.1 Multiple dissections increase the risk of muscle denervation, further decreasing the functional capability of the cleft patient's muscle.1 Therefore, a single-stage bilateral cleft lip and nose repair to correct the deformity and allow for proper growth is believed to be better for future appearance and function.
We must stress that there is no universally accepted surgical technique. All cleft results are subjectively reviewed. There are inherent surgeon biases regarding the quality of outcomes and need for revisions that cannot be resolved. There are also too many biologic variables in the anatomy as well as healing process that make comparison of results impossible. This article is intended to be a review of key perspectives in managing a child with a bilateral cleft lip deformity preoperatively and with the primary repair. We will highlight components of the markings and techniques that we feel are beneficial for the repair. It is not possible to review all surgical techniques for the bilateral cleft lip deformity within the scope of such a single review article.
The authors introduce what we believe to be a novel technique for closure of the nasal floor across the primary palate/alveolar gap during the primary repair. This technique was devised by the senior author (JSG). To our knowledge, this technique has not yet been published in the literature. It was developed by the senior author after dissatisfaction with traditional maneuvers to attempt nasal floor closure. We feel this primary anatomic closure of the nasal floor improves alar base advancement, lower lateral cartilage position and support, as well as facilitates future alveolar bone grafting and definitive rhinoplasty.
Historical Perspective
Millard believed that there is inadequate white roll and dry vermilion in the central prolabial segment.2,3 His traditional repair recruits the vermilion border from the lateral lip element, which can create a tight upper lip.2,3 Manchester, however, believed that the there is adequate vermilion in the prolabium.4 His repair describes joining the vermilion and white roll to those elements that already exist on the prolabium, which avoids lateral lip sacrifice.4 This technique however, has a propensity for formation of a whistle deformity. Byrd subsequently developed a technique that modifies the traditional Millard and Manchester techniques that minimizes lateral lip sacrifice and augments the tubercle.5
The Millard and Manchester techniques did not address the cleft nasal deformity during the primary lip reconstruction. Several authors have advocated primary nasal repair during the bilateral cleft lip surgery. Trott and Mohan introduced an open rhinoplasty exposure with interdomal suturing for a primary single-stage bilateral lip and nasal repair.6 Grayson et al introduced presurgical nasoalveolar molding (NAM) to shape the nose prior to surgical repair.7 Cutting combined the presurgical NAM with variation of an open rhinoplasty technique for domal unification.8 Mulliken also describes a primary rhinoplasty method with interdomal sutures and soft triangle skin excisions during the primary repair.9,10 These above-mentioned recent techniques have all been subjectively reported to yield improved results with regard to the nasal correction.
McComb transformed our rationale regarding surgical reconstruction.11 He concluded that the prolabium is embryologically lip tissue, thus, should stay in the lip. He felt that multistaged procedures are not necessary to create a columella. The columella is shortened due to the lateral pull of the alar cartilages and alar base due to the malalignment of the prolabium and the lateral maxillary segments. This displaces the true soft triangle and columella, which flattens the nasal tip and shortens the columellar height.
The alar cartilages and nasal soft tissue envelope can be sculpted, which will rotate the skin of the alar rim medially and add length to the columella. This can be achieved by presurgical NAM or surgical maneuvers at the time of the primary repair. Secondary columellar lengthening procedures, such as banked fork flaps or nasal sill tissue flaps yield suboptimal aesthetic results, as the scar lines are highly visible. The advent of presurgical NAM and primary rhinoplasty techniques have made secondary columellar lengthening procedures obsolete.9 We agree that secondary columellar lengthening procedures are suboptimal and should be avoided.
Role of Nasoalveolar Molding
The term presurgical orthopedics has been clouded by debate between active and passive techniques. The goals of the original techniques were to exert control over the floating premaxilla and align the maxillary dental arch. This is believed to reduce the tension on the lip repair and simplifying future orthodontics.7,8,12,13 Initial passive techniques involved lip taping and/or alveolar molding plates, which gently pushed on the prolabial segment. The most common active device utilized is the Latham device. This includes a surgically placed plate and pin system that requires active movement to set back the premaxilla.9,12,13,14 The subsequent debates centered on the potential detrimental effects on future maxillary growth. The controversy evolved and the benefit of the dental alignment did not seem to achieve better outcomes relative to lip adhesion or even early muscle repair. Subsequently, the technique of NAM emerged as a passive method with new alterations to the nose that previous presurgical orthodontics had been unable to achieve.8
Presurgical orthopedics was originally employed to expand the bony collapse of the lateral alveolar segments and make room for the premaxilla to be retrolined into arch position.7,8 The gaps of the primary palate clefts were narrowed and tension across the nasal and lip repair was decreased. However, good retraction on the premaxilla was not accomplished until nasal extensions were added to an alveolar molding plate.8 The combination of anterior thrust on the nostrils with posterior pull on both the inferior portion of the premaxilla as well as on the lip–columella junction was able to retract the premaxilla into proper anatomic alignment. The anterior nasal spine was gently brought back to define a nasolabial angle. The nasal lining was stretched and the columella was lengthened. This set the stage for the lip–nose repair while defining the lip–columella angle without forcing the nasal tip upward.
NAM requires a coordinated effort between the child's parents, the orthodontist, and the surgeon. NAM molding should be initiated as early as possible, preferably within the first month of life, to take advantage of the early malleability of the nasal and maxillary components. The molding process can take 2 to 4 months to complete. It is a labor-intensive process for the orthodontist and parents. Unfortunately, most centers in North America do not have orthodontists experienced in NAM. In addition, socioeconomic factors and the logistics of repeated office visits are significant obstacles for many families that prevent the utilization of NAM.
Presurgical taping is an alternative for centers that do not have access to an orthodontist that is experienced with NAM and for families unable to meet the demands of the process. Presurgical taping, albeit less optimal, will partially push back the premaxilla prior to surgery and decrease the discrepancy between the premaxilla and lateral maxillary segments. It must be stressed that taping alone does not help with nasal shaping.
Even without presurgical treatment, restoration of the muscle continuity across the midline is critical during the repair and establishes forces that act on the protruding premaxilla.6 In addition, proper release of the abnormal lateral lip and nasal attachments results in a tension free lip repair.6 If presurgical NAM is not used, primary repair should be planned at ∼ 3 months of age, when the child is at a safe weight for an elective general anesthetic. If presurgical NAM is utilized, then surgical repair is planned for when the molding process is complete, which can be as early as 3 months of age.
Surgical Markings
We stress again that there is no universally accepted surgical technique for bilateral lip repair. A decision must then be made whether the vermillion border of the prolabium is acceptable. Millard chose to bring both the white roll and dry vermillion from the lateral segments, believing that these prolabial elements were inadequate to form a full tubercle.2,3 Manchester accepted the prolabial vermilion border and flat mucocutaneous junction to avoid a tight upper lip and an obvious scar above the white roll.4 Byrd combined these two techniques, accepting the prolabial white roll and dry vermillion, but bringing in additional red lip from the lateral elements.5 This avoids the visible scar along the white roll inset and augments the tubercle while limiting the sacrifice from the lateral segments to prevent a tight upper lip closure.5
We present the surgical markings that were described by Byrd et al5 with minor modifications that we feel are beneficial. The original markings by Byrd et al are a modification of the traditional Millard and Manchester techniques.5 The markings are illustrated in Figs. 1, 2, and 3. This technique accepts the white roll on the prolabium as Manchester does. A true white roll on the prolabium may be blunted. It is still utilized, under those circumstances.
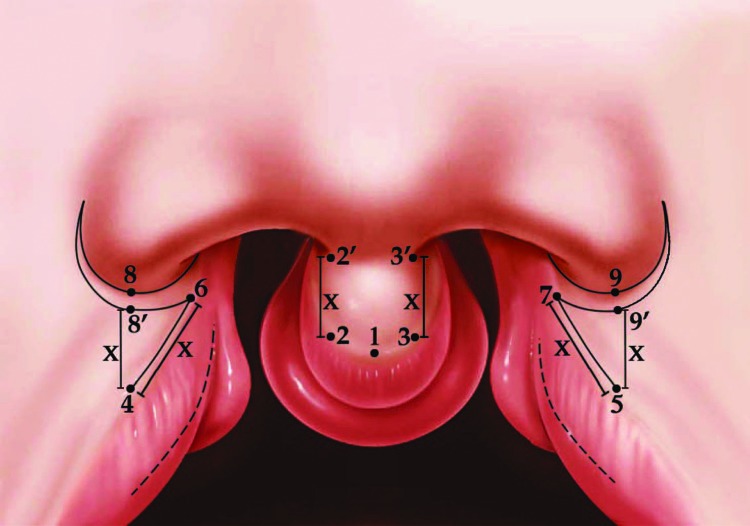
Fig. 1.
Critical points for the surgical markings (Byrd repair). X, Vertical height of the upper lip; 1, midline point on the vermilion border of the prolabium, corresponds to the trough of the Cupid's bow peak; 2 and 3, Cupid's bow peak points on the vermilion border of the prolabium; 2' and 3', columellar base points; 4 and 5, corresponding Cupid's bow peak points on the lateral lip element marked at the area of greatest fullness of the dry vermilion; 6 and 7, upper lip points on the lateral lip elements—these correspond to the columellar base points during closure; 8 and 9, alar base points; 8' and 9', new alar base points if there is excess vertical height on the lateral lip element—this necessitates a crescentic wedge excision of skin if encountered. (Reproduced with permission from Byrd HS, Ha RY, Khosla RK, Gosman AA. Bilateral cleft lip and nasal repair. Plast Reconstr Surg 2008; 122(4):1181–1190).
Fig. 2.
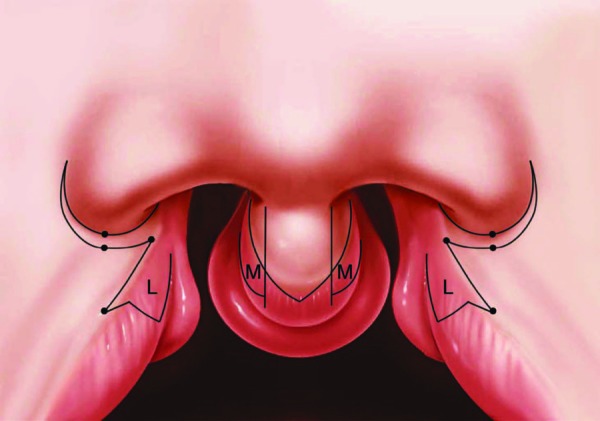
Skin incisions on the prolabial and lateral lip elements. M and L flaps marked. U-shaped prolabial skin flap demonstrated. The crescentic wedge excision performed if necessary for situations of excess vertical height on the lateral lip element. (Reproduced with permission from Byrd HS, Ha RY, Khosla RK, Gosman AA. Bilateral cleft lip and nasal repair. Plast Reconstr Surg 2008; 122(4):1181–1190).
Fig. 3.
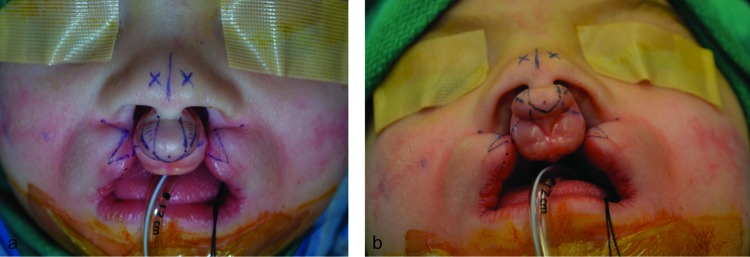
Photographs of the markings intraoperatively. Key features include the U-shaped prolabial skin flap and the triangular extension flaps on the lateral lip elements. (a) Anterior view. (b) Basal view.
An initial point is placed at the midline on the prolabium at the mucocutaneous junction of the white roll (Fig. 1). This establishes the central trough of the Cupid's bow peak. The columellar base points are marked and this sets the prolabial width. This width can be extrapolated to the vermilion border on the prolabium (Figs. 1, 2). A straight vertical line connects these points. This creates a straight-line closure for the reconstructed philtral columns (Figs. 1, 2). Some surgeons advocate widening the width of the prolabial at the vermilion border, which we think is also reasonable (Fig. 3). This modification allows for slightly oblique or biconcave incisions to give a “necktie” type design to the prolabial skin flap (Fig. 3). The vertical height of the upper lip (X) is predetermined by the vertical height of the prolabial segment (Fig. 1).
The wet–dry junction (red line) of the prolabium is then marked. Curvilinear lines are made from the Cupid's bow peak points down to the midline of the red line (Fig. 2). This preserves a portion of the prolabial dry lip and forms a U-shaped distal end to the prolabial skin flap. This drops the resulting scar off the vermilion border, which is felt to be better camouflaged.5 The M-flaps are marked along the red line extending into the cleft (Fig. 2). The M-flaps are not used in our current modification described here and will be discarded during the dissection and closure.
The lateral lip markings are then planned (Figs. 1, 2, 3). The red lines of the lateral lip elements are marked with a dotted line as they extend into the cleft and eventually fade into the mucocutaneous junction. The alar base points are marked on both sides. We have found that it is unnecessary to extend an incision around the alar base beyond the alar base points. We have found that this extended incision is highly visible and blunts the alar cheek groove. Therefore, our current modification stops the incision at the alar base points (Fig. 3).
The corresponding points for the Cupid's bow peaks on the lateral lip elements are marked on the white roll at the point of maximal fullness of the dry vermilion (Figs. 1, 2, 3). The vertical height of the lip (X) is then extrapolated to the lateral lip elements (Fig. 1). Adequate vertical height is confirmed by measuring from the cupids bow peak points to the alar base points as well as medially as the vermilion border fades into the cleft. If there is inadequate skin to accommodate the vertical height (X) on the lateral lip elements, then the intended Cupid's bow peak points need to be moved laterally along the vermilion border until sufficient height is achieved. At times, the lateral lip element will be longer than the prolabial vertical height. If this is encountered then a small crescentic wedge of skin is excised adjacent to the alar base (Figs. 1, 2). If a crescentic wedge is removed, then the incision needs to extend only a couple of millimeters beyond the alar base point to accommodate a reduction in the vertical height. It is not necessary to incise completely around the alar base.
Triangular lateral vermillion advancement flaps are then drawn starting from the Cupid's bow peak points on the lateral lip into the dry vermilion (Figs. 1, 2, 3). This line is marked to correspond with the length of the U-shaped extension on the prolabial segment on each side. This modification recruits more tissue (including mucosa and muscle) from the lateral lip elements to fill in the tubercle and prevent a whistle deformity. The L-flaps are marked extending down to the sulcus on the lateral lip elements (Figs. 2, 4).
Fig. 4.
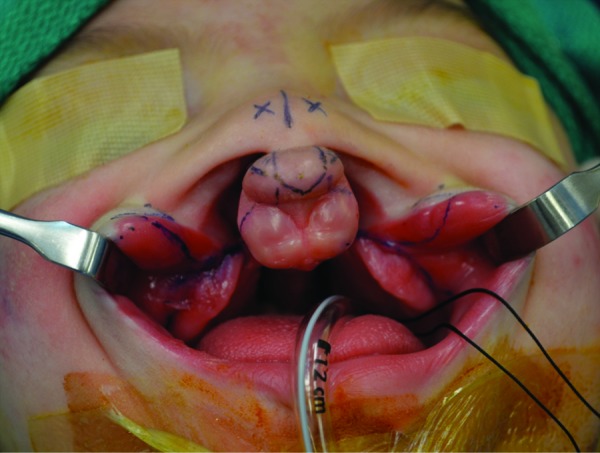
Intraoral markings demonstrating the L-flap incision taken down to the sulcus on the cleft margin. The sulcus incision is shown extending laterally with a back-cut in the buccal mucosa. The marking for the extended lateral nasal wall flap is shown extending posteriorly from the sulcus around the cleft margin.
Dissection of the Lip Elements
We begin the dissection with the skin incisions on the prolabial element (Figs. 2, 3). The U-shaped central prolabial flap is elevated in a deep subcutaneous plane to keep the flap thick to maintain reliable perfusion. This flap is elevated up to the columella–lip junction. The bilateral fork flaps are elevated. The fork flaps are not needed in the reconstruction and will be discarded. The remaining inferiorly based prolabial mucosal flap is advanced superiorly to create a sulcus if the anatomy has an ill-defined sulcus. This is trimmed at the distal end to create a triangular configuration. The mucosal flap is tacked down to the periosteum create a deep gingivolabial sulcus on the prolabium.
The M-flaps are then elevated. The M and L flaps historically have been used as part of the nasal floor closure. We believe that these diminutive and thin flaps are inadequate for the nasal floor closure. Therefore, the M-flaps are not used in our current technique and are discarded. The senior author (JSG) devised a novel nasal floor closure that will be described below in the section, Nasal Floor Repair.
The lateral cutaneous skin incisions are then made (Figs. 2, 3). The incisions along the alar base do not need to be taken further than the alar base points. We find that the lateral scar around the alar base is highly visible and blunts the alar cheek junction. In addition, appropriate soft tissue release can be accomplished purely with the subcutaneous dissection and soft tissue release. If the lateral lip elements are long, then a crescentic wedge of skin is excised as previously discussed.
The triangular lateral vermilion advancement flap is incised as part of the lateral lip element to be advanced over to the prolabium. The orbicularis oris has two distinct muscle sections, the pars peripheralis and the pars marginalis. The pars marginalis along the red lip must be preserved along the lateral lip element and triangular extension. This additional muscle and mucosal tissue augments the tubercle in the reconstruction. The L-flaps are elevated as a mucosal only flap to preserve all muscle fibers in the lateral lip element for transposition across the cleft. The L-flaps are dissected down to the gingivobuccal sulcus and kept posteriorly based. Our current modification for the nasal floor reconstruction does not utilize the L-flaps for nasal floor closure. The L-flaps can be used for lateral vestibular nasal lining if needed, which will be described below. If the L-flaps are not needed for lateral vestibular lining then they are discarded.
A relaxing incision is made along the gingivobuccal sulcus. A small cuff of mucosa is maintained along the gingival side to sew to. This is extended with a back-cut well in front of the parotid duct. The back-cut allows additional release of the buccal mucosa. The closure of the back-cut down to the sulcus is performed to advance the mucosa from a lateral to medial direction. This maneuver allows for recruitment of additional mucosa to cross the cleft up to the prolabial segment and allow for tension-free mucosal closure of the sulcus.
The alar base remains tethered to the pyriform rim by fibrous attachments of the accessory chain of the lateral crus of the lower lateral cartilages. The anterior maxillary soft tissues are aggressively released. This is dissected in the preperiosteal plane up to the level of the infraorbital nerve and medially to the pyriform rim and nasal bones. This soft tissue release is very important to adequately release the alar base from the pyriform rim and allow it to advance anteriorly into a more normal anatomic position.
The orbicularis oris muscle in a bilateral cleft lip is incorrectly oriented in an oblique direction in the lateral lip elements with abnormal attachments to the pyriform aperture and alar base. These attachments must be released to reposition the muscle in its proper horizontal orientation across the prolabium. The prolabium has an absence of muscle fibers in the complete bilateral cleft and a deficiency in the incomplete cleft.15 Thus, in either deformity, the muscle from the lateral lip elements must be brought together in the midline, underneath the prolabial skin flap during the repair. The pars peripheralis and pars marginalis should be approximated to give a visual distinction of the muscle underlying the cutaneous lip from those fibers, which are aligned under the red lip. Proper orbicularis repair is critical as this creates the oral sphincter and is the strength of the lip repair and takes tension off the skin closure.
Nasal Floor Repair
The authors present what we believe to be a novel technique for anatomic nasal floor closure through the alveolar clefts in patients with complete clefts of the primary palate. To our knowledge, this technique has yet to be described in the literature. This current technique was devised by Joseph S. Gruss, MD, out of frustration with unreliable nasal floor closures using prior techniques with M and L flaps. We feel the M and L flaps do not provide suitable tissue for nasal floor closure. The majority of these prior patients had open alveolar clefts after both the lip and palate repairs. This demonstrated the inadequacy of M and L flaps for nasal floor closure across the alveolar cleft. This new technique for nasal floor closure was initially presented at the American Cleft Palate Association Annual meeting by Patrick K. Kelley, MD, and named the extended lateral nasal wall flap for nasal floor closure.16 We currently utilize this technique in the reconstruction of both complete unilateral lip and complete bilateral lip deformities.
The nasal floor is anatomically closed with the extended lateral nasal wall flap and an extended medial nasal lining flap. The lateral flap is dissected from the base of the L-flap at the gingivobuccal sulcus along the cleft margin (Fig. 4). An incision is extended from the lateral sulcus headed posteriorly along the cleft margin. The lining release is performed in the subperiosteal plane and extended as posteriorly as possible. This elevates a large sheet of lining mucosa that will easily swing across the cleft. The L-flap can be maintained based off this lateral wall nasal lining flap if needed (Fig. 5). This maneuver helps release all the tethering forces on the mucosa from the pyriform rim. At times, the lateral nasal lining is still tight, as is the situation with severe lateral maxillary segment collapse. Thus, the alar base may not elevate sufficiently in the anterior direction. If this is encountered, then preservation of the L-flap should be considered. A back-cut can then be made in the lateral vestibular lining to allow for inset of the L-flap to augment the lateral vestibular nasal lining (Fig. 5).
Fig. 5.
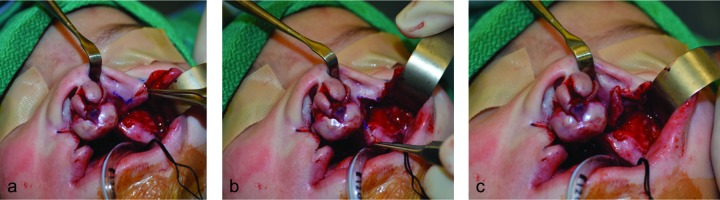
Lateral nasal vestibular lining release. The L-flap is posteriorly based off the lateral nasal wall flap. (a) Marking for the lateral vestibular lining release. Forceps is holding the L-flap laterally. (b) Lateral vestibular lining release with donor defect. Forceps is holding the L-flap inferiorly. (c) Transposition of the L-flap into the lateral nasal lining defect.
The medial nasal lining flap is started along the gingivo–mucosal border of the premaxilla. The incision is extended posteriorly around the premaxilla and onto the vomer along the midline. Flaps are elevated bilaterally in the subperiosteal plane posteriorly as possible. This flap requires minimal elevation along the vomer and septum to create an edge to close the lateral nasal lining flap to. The majority of the movement across the cleft comes from the lateral flap. The lateral flap is advanced across the cleft and repaired to the medial lining flap. This closes the nasal floor as posteriorly as possible, at least across the primary palate (Fig. 6).
Fig. 6.
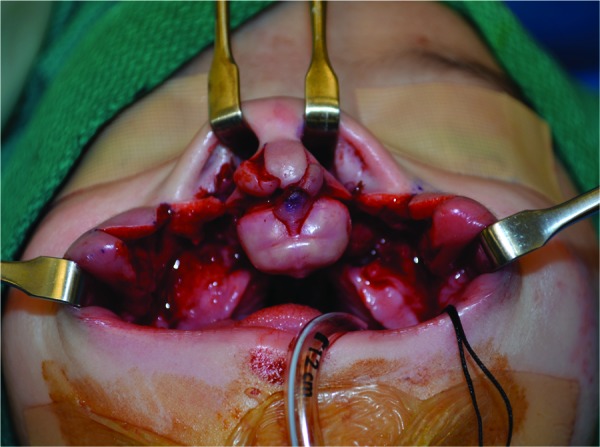
Basal view of the anatomic nasal floor closure. The extended lateral nasal wall flap is sutured to the extended medial nasal lining flap. This creates an internal sling for lateral nasal support.
This is a powerful technique to reconstruct the nasal floor with anatomically appropriate and robust mucosal tissue. We feel that this has several advantages. The dissection allows for more anterior movement of the alar base on each side bringing the lateral nose into appropriate anatomic position relative to the premaxilla. The nasal floor repair creates a strong internal sling that further supports the nasal reconstruction, alar base position, and alar shape.
The undersurface of the one layer repair fills in with scar tissue and mucosalizes across the alveolar cleft on the oral side. This effectively closes off the oronasal communication along the alveolar cleft. This also makes the palate repair easier as the anterior-most aspect of the nasal lining is already closed. Once the palate is repaired, patients do not experience years of nasal regurgitation awaiting bone grafting, as the alveolar cleft is filled with scar tissue. In addition, this nasal floor closure makes future alveolar bone grafting procedure easier as the nasal floor is already closed across the alveolar cleft.
Primary Rhinoplasty
The premaxilla lacks proper definition of the anterior nasal spine, thus the medial footplates fall away from each other, unzipping the cartilage and destroying the tip support that should be given by the columella. The maxillary segments and pyriform apertures have fallen laterally and posteriorly, pulling and rotating the lateral crura with them. Therefore, the skin envelope of the nose has no defining framework and the columella appears short and wide.
Several single-stage lip and primary rhinoplasty techniques with various approaches to access the nasal cartilage for reshaping have been developed. Trott and Mohan introduced a single-stage bilateral cleft lip and nasal repair of wide clefts for patients in a socioeconomic situation where presurgical molding was not possible.6 They described their extension of bilateral Tajima-style “reverse-U” nasal incisions inferiorly around the prolabium in an open-tip rhinoplasty approach. The nasal lining and alar bases are completely detached from the pyriform margins to decrease the tension across the nose. The columella–prolabium skin complex was elevated anteriorly off the cartilage and retracted over the dorsum of the nose. Their open technique provided the advantage of complete cartilage visualization for precise intercartilaginous suturing and excision of the fibroadipose tissue separating the domes. The disadvantage of fibroadipose excision and wide elevation of the skin flap was poor vascularity to the prolabial skin, necessitating a design of a wider philtrum.
McComb introduced a method of cleft lip-nasal repair that avoided nasal lining incisions and instead used an external cutaneous “flying bird” incision along both nostril rims and across the nasal tip.11 He described wide undermining and elevation of a triangular skin flap to expose the cartilages and excise the fibroadipose tissue separating the domes. Interdomal sutures are placed, a v-y skin closure narrows the nasal tip and lengthens the columella. He started this method as a single-stage repair, but encountered compromised blood supply to the columella–prolabium skin. Thereafter, he reserved the single-stage repair for older patients. A two-stage approach was planned for infants, starting with the nasal repair while leaving the prolabium attached to the premaxilla and finishing with a lip repair once the columella had healed. The disadvantage is the necessity for two stages and an external nasal scar.
Mulliken used similar bilateral nostril rim incisions without an extension across the columella for adequate exposure of the nasal cartilage.9,10 This maintained better vascular supply for the distal skin of the columella–prolabial complex and allowed for a narrow philtral design. In addition, any excess soft triangle tissue is excised before closure of the rim incisions thus helping narrow the nasal tip and lengthen the columella. This has the advantage of precise cartilage shaping and consistent vascular supply to the narrow prolabial skin tip, but sacrifices dorsal skin length, which can result in an up-turned nose.
In patients who have been successfully treated with NAM, Cutting developed a retrograde approach to the cartilage dissection to preserve the columella–prolabium blood supply.8 Transfixion incisions are used and the medial crura and columella–prolabial skin complex are elevated off the nasal septum and retracted back over the nasal dorsum. Starting with the undersurface of the cartilage exposed, dissection is performed between the tip cartilages, elevating the fibroadipose tissue with the dorsal nasal skin, thereby preserving blood supply to the prolabial skin flap. The intercartilaginous sutures are then placed from behind. Direct visualization for placement of domal sutures is not as critical because the presurgical NAM has already partially shaped the infantile cartilage, requiring more subtle remodeling.
If NAM is not used or is unsuccessful, Cutting recommends a combination of his retrograde dissection with a modification of Mulliken's anterior dissection done using the reverse-U Tajima incision.8,17 The sutures are placed as Mulliken described, but no skin is sacrificed because the incisions are closed with the excess tissue folded over the rim to create a soft triangle. Closure is completely inside the nostril rim.
It is still unclear whether any primary open rhinoplasty approach performed during infancy prevents the need for future definitive rhinoplasty. Any aggressive open technique in the nose during primary reconstruction has a higher risk of skin necrosis to the columella and prolabium. Thus, the authors prefer a closed rhinoplasty technique primarily to accomplish nasal tip and alar shaping, along with lateral soft tissue release and anatomic nasal floor closure for alar base support.
Our best results in terms of nasal shaping are seen with successful preoperative NAM; however, this is not always possible given logistical constraints described previously. We feel that adequate soft tissue release of the nasal attachments to the pyriform and anatomic nasal floor closure are critical to alar shaping. All lateral attachments of the nose to the pyriform rim are released by the lateral dissection described during the dissection of the lateral lip elements. Access into the nose is obtained from the lateral exposure created at the alar bases with the dissection of the lateral lip elements. The soft tissues along the alar rim are released from the alar base up to the tip complex using blunt dissection both in the subcutaneous plane and submucosal plane. This releases the fibroadipose tissue along the alar rim and allows it to slide internally when the alar base is rotated into position. Central dissection into the nose is avoided to preserve circulation into the prolabial skin flap. Transnasal sutures are then used to shape the cartilage once the skin envelope is elevated. These include transmucosal mattress sutures that are placed under the tip complex to unify the domes. Transdermal modified Tajima-style sutures are placed to elevate the lower lateral cartilage (LLC) to the contralateral upper lateral cartilage (ULC).5,17,18 These mattress sutures start in the intranasal side and are passed through the external skin overlying the ULC. The suture is then passed through the same hole in the skin and brought back into the same nostril and tied down. Additional transnasal sutures are added to lateralize the vestibular webs and create the alar groove, further supporting the lateral position of the LLC. The alar shape is also held into its newly reconstructed position with nasal stents for ∼ 6 weeks.
Despite these primary rhinoplasty maneuvers employed, we understand that there are too many variables in the future growth and development of the nose to control primarily. It is unrealistic to expect that we can control for and expect proper future growth and development. Therefore, we believe that these patients will still benefit from a definitive rhinoplasty procedure during the late teenage years.
Discussion
The bilateral cleft lip deformity is one of the most challenging entities in cleft and craniofacial surgery. Multiple surgical techniques have been described for management of the deformity. There is no universally accepted consensus among cleft surgeons as to the optimal markings, flap designs, and primary rhinoplasty techniques. Results are entirely subjective and there are too many variables in the anatomy, healing processes, and future growth and development to control for. Many modifications of the traditional repairs have been described that offer subjective improvements in nasal shape and lip aesthetics.
Proper dissection of the prolabial lip element, lateral lip elements and nose are critical for release of the soft tissues. Anatomic repair of the nasal floor as presented here with the extended lateral nasal wall flap and medial nasal lining flap have provided significant benefits in the reconstruction. After the dissection is complete, the sequence of the closure is best performed from inside out. The L-flap is trimmed and inset into the lateral vestibular lining back-cut if needed for additional anterior alar base movement (Fig. 5). The nasal floor is closed, as exposure to this region is best when the lip is wide open (Fig. 6). The sulcus mucosa is subsequently closed, advancing the mucosa across the cleft with medial repair to the prolabial mucosal lining to establish a deep central sulcus. The raw undersurface of the nasal floor and sulcus closure across the alveolar clefts will fill in secondarily and mucosalize.
The orbicularis muscle fibers are carefully repaired thus bearing the tension of the repair and augmenting the tubercle. An alar cinch suture is placed to shape the alar contour and hold the alar bases in the best symmetric position as possible. The triangular advancement flaps are closed to the dry lip of the prolabial skin flap over the muscle repair to further augment the tubercle. The skin is carefully closed to align the vermilion border and columellar base followed by the nasal sill closure. The transnasal shaping sutures and nasal stents are performed last.
A typical case example using our current technique is shown in Fig. 7. This is a child with a complete bilateral cleft lip and palate deformity. The on table preoperative picture demonstrates severe collapse of the lateral maxillary segments and twisted prolabium. The result shown is 20 months postoperative. There is appropriate balance to the upper lip without tightness, good symmetry, and fullness in the tubercle, without a whistle deformity. The central lip scar is well hidden in the red lip of the vermilion border. There is appropriate maintenance of the alar base position bilaterally with symmetry of the alar contour.
Fig. 7.

Case example with pre- and postoperative photographs of a complete bilateral cleft lip and palate deformity. (a) Anterior view, preoperative. (b) Anterior view, 20 months postoperative.
Successful surgical treatment of the bilateral cleft lip deformity can only be accomplished with proper understanding of the anatomy and how the abnormal anatomy of the lip and nose can be manipulated. The surgical repair must focus on proper orbicularis oris muscle repair, upper lip aesthetics, nasal support, and symmetry to minimize secondary deformities. However, secondary deformities may occur, as it is impossible to control future facial growth and development. For example, no matter what primary rhinoplasty technique is performed, definitive rhinoplasty near skeletal maturity is still extremely beneficial for functional breathing issues and nasal aesthetic improvements.
Many advances have been made in surgery for the bilateral cleft deformity over the last few decades. We offer some new ideas here that produce reproducible and improved results. We anticipate that future advances in surgical technique as well as basic science will continue to improve outcomes for patients born with a bilateral cleft lip deformity.
References
- 1.Schendel S A, Pearl R M, De Armond S J. Pathophysiology of cleft lip muscles following the initial surgical repair. Plast Reconstr Surg. 1991;88(2):197–200. doi: 10.1097/00006534-199108000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Millard D R. Bilateral cleft lip and a primary forked flap: a preliminary report. Plast Reconstr Surg. 1967;39(1):59–65. doi: 10.1097/00006534-196701000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Millard D R Jr. Closure of bilateral cleft lip and elongation of columella by two operations in infancy. Plast Reconstr Surg. 1971;47(4):324–331. doi: 10.1097/00006534-197104000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Manchester W M. The repair of bilateral cleft lip and palate. Br J Surg. 1965;52(11):878–882. doi: 10.1002/bjs.1800521111. [DOI] [PubMed] [Google Scholar]
- 5.Byrd H S, Ha R Y, Khosla R K, Gosman A A. Bilateral cleft lip and nasal repair. Plast Reconstr Surg. 2008;122(4):1181–1190. doi: 10.1097/PRS.0b013e3181858f33. [DOI] [PubMed] [Google Scholar]
- 6.Trott J A, Mohan N A. A preliminary report on one stage open tip rhinoplasty at the time of lip repair in bilateral cleft lip and palate: the Alor Setar experience. Br J Plast Surg. 1993;46(3):215–222. doi: 10.1016/0007-1226(93)90171-7. [DOI] [PubMed] [Google Scholar]
- 7.Grayson B H, Cutting C B, Wood R. Preoperative columella lengthening in bilateral cleft lip and palate. Plast Reconstr Surg. 1993;92(7):1422–1423. [PubMed] [Google Scholar]
- 8.Cutting C, Grayson B, Brecht L, Santiago P, Wood R, Kwon S. Presurgical columellar elongation and primary retrograde nasal reconstruction in one-stage bilateral cleft lip and nose repair. Plast Reconstr Surg. 1998;101(3):630–639. doi: 10.1097/00006534-199803000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Mulliken J B Primary repair of bilateral cleft lip and nasal deformity Plast Reconstr Surg 20011081181–194., 195–196 [DOI] [PubMed] [Google Scholar]
- 10.Mulliken J B, Wu J K, Padwa B L. Repair of bilateral cleft lip: review, revisions, and reflections. J Craniofac Surg. 2003;14(5):609–620. doi: 10.1097/00001665-200309000-00003. [DOI] [PubMed] [Google Scholar]
- 11.McComb H Primary repair of the bilateral cleft lip nose: a 15-year review and a new treatment plan Plast Reconstr Surg 1990865882–889., discussion 890–893 [PubMed] [Google Scholar]
- 12.Georgiade N G, Latham R A. Maxillary arch alignment in the bilateral cleft lip and palate infant, using pinned coaxial screw appliance. Plast Reconstr Surg. 1975;56(1):52–60. doi: 10.1097/00006534-197507000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Georgiade N G, Mason R, Riefkohl R, Georgiade G, Barwick W. Preoperative positioning of the protruding premaxilla in the bilateral cleft lip patient. Plast Reconstr Surg. 1989;83(1):32–40. doi: 10.1097/00006534-198901000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Millard D R Jr, Latham R A. Improved primary surgical and dental treatment of clefts. Plast Reconstr Surg. 1990;86(5):856–871. doi: 10.1097/00006534-199011000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Mulliken J B Pensler J M Kozakewich H P The anatomy of Cupid's bow in normal and cleft lip Plast Reconstr Surg 1993923395–403., discussion 404 [PubMed] [Google Scholar]
- 16.Kelley P K Harshbarger R Da Silveira A Gruss J Use of the extended lateral nasal lining flap improves primary cleft lip results and eliminates long term nasal lining deficiency Paper presented at: American Cleft Palate-Craniofacial Association Annual Meeting; April 5–9, 2011; San Juan, Puerto Rico
- 17.Tajima S, Maruyama M. Reverse-U incision for secondary repair of cleft lip nose. Plast Reconstr Surg. 1977;60(2):256–261. doi: 10.1097/00006534-197708000-00013. [DOI] [PubMed] [Google Scholar]
- 18.Tajima S. Follow-up results of the unilateral primary cleft lip operation with special reference to primary nasal correction by the author's method. Facial Plast Surg. 1990;7(2):97–104. doi: 10.1055/s-2008-1064669. [DOI] [PubMed] [Google Scholar]